Abstract
Purpose of Review
To provide an overview of the mechanistic and epidemiologic evidence linking sleep-related exposures, such as short sleep duration, obstructive sleep apnea, shift work, and insomnia, with type 2 diabetes risk in adults.
Recent Findings
Both poor sleep habits and sleep disorders are highly prevalent among adults with type 2 diabetes. In observational studies, short sleep duration, obstructive sleep apnea, shift work, and insomnia are all associated with higher risk of incident type 2 diabetes and may predict worse outcomes in those with existing diabetes. However, interventional studies addressing sleep abnormalities in populations with or at high risk for type 2 diabetes are scarce.
Summary
Although common sleep abnormalities are associated with risk of incident type 2 diabetes and worse prognosis in those with established diabetes, there are few randomized trials evaluating the impact of sleep-focused interventions on diabetes, making it difficult to determine whether the relationship is causal.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Hobson JA. Sleep is of the brain, by the brain and for the brain. Nature. 2005;437(7063):1254–6. https://doi.org/10.1038/nature04283.
Everson CA, Bergmann BM, Rechtschaffen A. Sleep deprivation in the rat: III. Total sleep deprivation. Sleep. 1989;12(1):13–21.
Krueger JM, Frank MG, Wisor JP, Roy S. Sleep function: toward elucidating an enigma. Sleep Med Rev. 2016;28:46–54. https://doi.org/10.1016/j.smrv.2015.08.005.
Benington JH, Heller HC. Restoration of brain energy metabolism as the function of sleep. Prog Neurobiol. 1995;45(4):347–60.
Tononi G, Cirelli C. Sleep and the price of plasticity: from synaptic and cellular homeostasis to memory consolidation and integration. Neuron. 2014;81(1):12–34. https://doi.org/10.1016/j.neuron.2013.12.025.
Xie L, Kang H, Xu Q, Chen MJ, Liao Y, Thiyagarajan M, et al. Sleep drives metabolite clearance from the adult brain. Science. 2013;342(6156):373–7. https://doi.org/10.1126/science.1241224.
Spiegel K, Leproult R, Van Cauter E. Impact of sleep debt on metabolic and endocrine function. Lancet. 1999;354(9188):1435–9. https://doi.org/10.1016/S0140-6736(99)01376-8.
Buxton OM, Pavlova M, Reid EW, Wang W, Simonson DC, Adler GK. Sleep restriction for 1 week reduces insulin sensitivity in healthy men. Diabetes. 2010;59(9):2126–33. https://doi.org/10.2337/db09-0699.
Broussard JL, Ehrmann DA, Van Cauter E, Tasali E, Brady MJ. Impaired insulin signaling in human adipocytes after experimental sleep restriction: a randomized, crossover study. Ann Intern Med. 2012;157(8):549–57. https://doi.org/10.7326/0003-4819-157-8-201210160-00005.
Robertson MD, Russell-Jones D, Umpleby AM, Dijk DJ. Effects of three weeks of mild sleep restriction implemented in the home environment on multiple metabolic and endocrine markers in healthy young men. Metabolism. 2013;62(2):204–11. https://doi.org/10.1016/j.metabol.2012.07.016.
Leproult R, Deliens G, Gilson M, Peigneux P. Beneficial impact of sleep extension on fasting insulin sensitivity in adults with habitual sleep restriction. Sleep. 2015;38(5):707–15. https://doi.org/10.5665/sleep.4660.
Tasali E, Leproult R, Ehrmann DA, Van Cauter E. Slow-wave sleep and the risk of type 2 diabetes in humans. Proc Natl Acad Sci U S A. 2008;105(3):1044–9. https://doi.org/10.1073/pnas.0706446105.
Stamatakis KA, Punjabi NM. Effects of sleep fragmentation on glucose metabolism in normal subjects. Chest. 2010;137(1):95–101. https://doi.org/10.1378/chest.09-0791.
Louis M, Punjabi NM. Effects of acute intermittent hypoxia on glucose metabolism in awake healthy volunteers. J Appl Physiol (1985). 2009;106(5):1538–44. https://doi.org/10.1152/japplphysiol.91523.2008.
Iiyori N, Alonso LC, Li J, Sanders MH, Garcia-Ocana A, O'Doherty RM, et al. Intermittent hypoxia causes insulin resistance in lean mice independent of autonomic activity. Am J Respir Crit Care Med. 2007;175(8):851–7. https://doi.org/10.1164/rccm.200610-1527OC.
Punjabi NM, Shahar E, Redline S, Gottlieb DJ, Givelber R, Resnick HE, et al. Sleep-disordered breathing, glucose intolerance, and insulin resistance: the Sleep Heart Health Study. Am J Epidemiol. 2004;160(6):521–30. https://doi.org/10.1093/aje/kwh261.
Pamidi S, Wroblewski K, Broussard J, Day A, Hanlon EC, Abraham V, et al. Obstructive sleep apnea in young lean men: impact on insulin sensitivity and secretion. Diabetes Care. 2012;35(11):2384–9. https://doi.org/10.2337/dc12-0841.
Kent BD, Grote L, Bonsignore MR, Saaresranta T, Verbraecken J, Levy P, et al. Sleep apnoea severity independently predicts glycaemic health in nondiabetic subjects: the ESADA study. Eur Respir J. 2014;44(1):130–9. https://doi.org/10.1183/09031936.00162713.
Scheer FA, Hilton MF, Mantzoros CS, Shea SA. Adverse metabolic and cardiovascular consequences of circadian misalignment. Proc Natl Acad Sci U S A. 2009;106(11):4453–8. https://doi.org/10.1073/pnas.0808180106.
Beihl DA, Liese AD, Haffner SM. Sleep duration as a risk factor for incident type 2 diabetes in a multiethnic cohort. Ann Epidemiol. 2009;19(5):351–7. https://doi.org/10.1016/j.annepidem.2008.12.001.
Dionne KE, Colton CK, Yarmush ML. Effect of hypoxia on insulin secretion by isolated rat and canine islets of Langerhans. Diabetes. 1993;42(1):12–21.
Punjabi NM, Beamer BA. Alterations in glucose disposal in sleep-disordered breathing. Am J Respir Crit Care Med. 2009;179(3):235–40. https://doi.org/10.1164/rccm.200809-1392OC.
Somers VK, Dyken ME, Mark AL, Abboud FM. Sympathetic-nerve activity during sleep in normal subjects. N Engl J Med. 1993;328(5):303–7. https://doi.org/10.1056/NEJM199302043280502.
Irwin M, Thompson J, Miller C, Gillin JC, Ziegler M. Effects of sleep and sleep deprivation on catecholamine and interleukin-2 levels in humans: clinical implications. J Clin Endocrinol Metab. 1999;84(6):1979–85. https://doi.org/10.1210/jcem.84.6.5788.
Somers VK, Dyken ME, Clary MP, Abboud FM. Sympathetic neural mechanisms in obstructive sleep apnea. J Clin Invest. 1995;96(4):1897–904. https://doi.org/10.1172/JCI118235.
Leproult R, Copinschi G, Buxton O, Van Cauter E. Sleep loss results in an elevation of cortisol levels the next evening. Sleep. 1997;20(10):865–70.
Manenschijn L, van Kruysbergen RG, de Jong FH, Koper JW, van Rossum EF. Shift work at young age is associated with elevated long-term cortisol levels and body mass index. J Clin Endocrinol Metab. 2011;96(11):E1862–5. https://doi.org/10.1210/jc.2011-1551.
Irwin MR, Olmstead R, Carroll JE. Sleep disturbance, sleep duration, and inflammation: a systematic review and meta-analysis of cohort studies and experimental sleep deprivation. Biol Psychiatry. 2016;80(1):40–52. https://doi.org/10.1016/j.biopsych.2015.05.014.
Ryan S, Taylor CT, McNicholas WT. Predictors of elevated nuclear factor-kappaB-dependent genes in obstructive sleep apnea syndrome. Am J Respir Crit Care Med. 2006;174(7):824–30. https://doi.org/10.1164/rccm.200601-066OC.
Yokoe T, Minoguchi K, Matsuo H, Oda N, Minoguchi H, Yoshino G, et al. Elevated levels of C-reactive protein and interleukin-6 in patients with obstructive sleep apnea syndrome are decreased by nasal continuous positive airway pressure. Circulation. 2003;107(8):1129–34.
Gottlieb DJ, Punjabi NM, Mehra R, Patel SR, Quan SF, Babineau DC, et al. CPAP versus oxygen in obstructive sleep apnea. N Engl J Med. 2014;370(24):2276–85. https://doi.org/10.1056/NEJMoa1306766.
Leproult R, Holmback U, Van Cauter E. Circadian misalignment augments markers of insulin resistance and inflammation, independently of sleep loss. Diabetes. 2014;63(6):1860–9. https://doi.org/10.2337/db13-1546.
McMullan CJ, Schernhammer ES, Rimm EB, Hu FB, Forman JP. Melatonin secretion and the incidence of type 2 diabetes. JAMA. 2013;309(13):1388–96. https://doi.org/10.1001/jama.2013.2710.
Bouatia-Naji N, Bonnefond A, Cavalcanti-Proenca C, Sparso T, Holmkvist J, Marchand M, et al. A variant near MTNR1B is associated with increased fasting plasma glucose levels and type 2 diabetes risk. Nat Genet. 2009;41(1):89–94. https://doi.org/10.1038/ng.277.
Lyssenko V, Nagorny CL, Erdos MR, Wierup N, Jonsson A, Spegel P, et al. Common variant in MTNR1B associated with increased risk of type 2 diabetes and impaired early insulin secretion. Nat Genet. 2009;41(1):82–8. https://doi.org/10.1038/ng.288.
Garaulet M, Gomez-Abellan P, Rubio-Sastre P, Madrid JA, Saxena R, Scheer FA. Common type 2 diabetes risk variant in MTNR1B worsens the deleterious effect of melatonin on glucose tolerance in humans. Metabolism. 2015;64(12):1650–7. https://doi.org/10.1016/j.metabol.2015.08.003.
Consensus Conference Panel, Watson NF, Badr MS, Belenky G, Bliwise DL, Buxton OM, et al. Joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society on the recommended amount of sleep for a healthy adult: methodology and discussion. Sleep. 2015;38(8):1161–83. https://doi.org/10.5665/sleep.4886.
Centers for Disease Control and Prevention. Sleep and sleep disorders. https://www.cdc.gov/features/sleep/. https://www.cdc.gov/features/sleep/.
Hirshkowitz MWK, Albert SM, Alessi C, Bruni O, Don Carlos L, Hazen N, et al. National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health. 1(1):40–3.
Mukherjee S, Patel SR, Kales SN, Ayas NT, Strohl KP, Gozal D, et al. An official American Thoracic Society statement: the importance of healthy sleep. Recommendations and future priorities. Am J Respir Crit Care Med. 2015;191(12):1450–8. https://doi.org/10.1164/rccm.201504-0767ST.
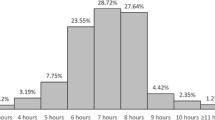
Liu Y, Wheaton AG, Chapman DP, Cunningham TJ, Lu H, Croft JB. Prevalence of healthy sleep duration among adults--United States, 2014. MMWR Morb Mortal Wkly Rep. 2016;65(6):137–41. https://doi.org/10.15585/mmwr.mm6506a1.
Ohayon MM, Carskadon MA, Guilleminault C, Vitiello MV. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep. 2004;27(7):1255–73.
Silva GE, Goodwin JL, Sherrill DL, Arnold JL, Bootzin RR, Smith T, et al. Relationship between reported and measured sleep times: the sleep heart health study (SHHS). J Clin Sleep Med : JCSM : Off Publ Am Acad Sleep Med. 2007;3(6):622–30.
Krueger PM, Friedman EM. Sleep duration in the United States: a cross-sectional population-based study. Am J Epidemiol. 2009;169(9):1052–63. https://doi.org/10.1093/aje/kwp023.
Lauderdale DS, Knutson KL, Yan LL, Rathouz PJ, Hulley SB, Sidney S, et al. Objectively measured sleep characteristics among early-middle-aged adults: the CARDIA study. Am J Epidemiol. 2006;164(1):5–16. https://doi.org/10.1093/aje/kwj199.
Chen X, Wang R, Zee P, Lutsey PL, Javaheri S, Alcantara C, et al. Racial/ethnic differences in sleep disturbances: the multi-ethnic study of atherosclerosis (MESA). Sleep. 2015;38(6):877–88. https://doi.org/10.5665/sleep.4732.
Hale L, Do DP. Racial differences in self-reports of sleep duration in a population-based study. Sleep. 2007;30(9):1096–103.
Ertel KA, Berkman LF, Buxton OM. Socioeconomic status, occupational characteristics, and sleep duration in African/Caribbean immigrants and US White health care workers. Sleep. 2011;34(4):509–18.
Stamatakis KA, Kaplan GA, Roberts RE. Short sleep duration across income, education, and race/ethnic groups: population prevalence and growing disparities during 34 years of follow-up. Ann Epidemiol. 2007;17(12):948–55. https://doi.org/10.1016/j.annepidem.2007.07.096.
Ryu SY, Kim KS, Han MA. Factors associated with sleep duration in Korean adults: results of a 2008 community health survey in Gwangju metropolitan city. Korea J Korean Med Sci. 2011;26(9):1124–31. https://doi.org/10.3346/jkms.2011.26.9.1124.
Patel SR, Sotres-Alvarez D, Castaneda SF, Dudley KA, Gallo LC, Hernandez R, et al. Social and health correlates of sleep duration in a US Hispanic population: results from the Hispanic community health study/study of Latinos. Sleep. 2015;38(10):1515–22. https://doi.org/10.5665/sleep.5036.
Basner M, Fomberstein KM, Razavi FM, Banks S, William JH, Rosa RR, et al. American time use survey: sleep time and its relationship to waking activities. Sleep. 2007;30(9):1085–95.
Ogilvie RP, Patel SR. The epidemiology of sleep and obesity. Sleep Health. 2017;3(5):383–8. https://doi.org/10.1016/j.sleh.2017.07.013.
Capers PL, Fobian AD, Kaiser KA, Borah R, Allison DB. A systemic review and meta-analysis of randomized controlled trials of the impact of sleep duration on adiposity and components of energy balance. Obes Rev : Off J Int Assoc Stud Obes. 2015;16(9):771–82. https://doi.org/10.1111/obr.12296.
Patel SR, Hu FB. Short sleep duration and weight gain: a systematic review. Obesity. 2008;16(3):643–53. https://doi.org/10.1038/oby.2007.118.
Patel SR, Malhotra A, White DP, Gottlieb DJ, Hu FB. Association between reduced sleep and weight gain in women. Am J Epidemiol. 2006;164(10):947–54. https://doi.org/10.1093/aje/kwj280.
Spaeth AM, Dinges DF, Goel N. Effects of experimental sleep restriction on weight gain, caloric intake, and meal timing in healthy adults. Sleep. 2013;36(7):981–90. https://doi.org/10.5665/sleep.2792.
Bromley LE, Booth JN 3rd, Kilkus JM, Imperial JG, Penev PD. Sleep restriction decreases the physical activity of adults at risk for type 2 diabetes. Sleep. 2012;35(7):977–84. https://doi.org/10.5665/sleep.1964.
Cizza G, Piaggi P, Rother KI, Csako G. Sleep Extension Study G. Hawthorne effect with transient behavioral and biochemical changes in a randomized controlled sleep extension trial of chronically short-sleeping obese adults: implications for the design and interpretation of clinical studies. PloS one. 2014;9(8):e104176. https://doi.org/10.1371/journal.pone.0104176.
Cespedes EM, Hu FB, Redline S, Rosner B, Alcantara C, Cai J, et al. Comparison of self-reported sleep duration with actigraphy: results from the Hispanic community health study/study of Latinos Sueno ancillary study. Am J Epidemiol. 2016;183(6):561–73. https://doi.org/10.1093/aje/kwv251.
Jackson CL, Patel SR, Jackson WB, 2nd, Lutsey PL, Redline S. Agreement between self-reported and objectively measured sleep duration among white, black, Hispanic, and Chinese adults in the United States: multi-ethnic study of atherosclerosis. Sleep 2018. https://doi.org/10.1093/sleep/zsy057.
Lauderdale DS, Knutson KL, Yan LL, Liu K, Rathouz PJ. Self-reported and measured sleep duration: how similar are they? Epidemiology. 2008;19(6):838–45. https://doi.org/10.1097/EDE.0b013e318187a7b0.
Matthews KA, Patel SR, Pantesco EJ, Buysse DJ, Kamarck TW, Lee L, et al. Similarities and differences in estimates of sleep duration by polysomnography, actigraphy, diary, and self-reported habitual sleep in a community sample. Sleep Health. 2018;4(1):96–103. https://doi.org/10.1016/j.sleh.2017.10.011.
Bakker JP, Weng J, Wang R, Redline S, Punjabi NM, Patel SR. Associations between obstructive sleep apnea, sleep duration, and abnormal fasting glucose. The multi-ethnic study of atherosclerosis. Am J Respir Crit Care Med. 2015;192(6):745–53. https://doi.org/10.1164/rccm.201502-0366OC.
Shan Z, Ma H, Xie M, Yan P, Guo Y, Bao W, et al. Sleep duration and risk of type 2 diabetes: a meta-analysis of prospective studies. Diabetes Care. 2015;38(3):529–37. https://doi.org/10.2337/dc14-2073.
Knutson KL. Does inadequate sleep play a role in vulnerability to obesity? Am J Hum Biol. 2012;24(3):361–71. https://doi.org/10.1002/ajhb.22219.
Patel SR, Blackwell T, Ancoli-Israel S, Stone KL. Osteoporotic fractures in men-Mr OSRG. Sleep characteristics of self-reported long sleepers. Sleep. 2012;35(5):641–8. https://doi.org/10.5665/sleep.1822.
Patel SR, Malhotra A, Gottlieb DJ, White DP, Hu FB. Correlates of long sleep duration. Sleep. 2006;29(7):881–9.
Liu R, Zee PC, Chervin RD, Arguelles LM, Birne J, Zhang S, et al. Short sleep duration is associated with insulin resistance independent of adiposity in Chinese adult twins. Sleep Med. 2011;12(9):914–9. https://doi.org/10.1016/j.sleep.2011.04.006.
Pyykkonen AJ, Isomaa B, Pesonen AK, Eriksson JG, Groop L, Tuomi T, et al. Sleep duration and insulin resistance in individuals without type 2 diabetes: the PPP-Botnia study. Ann Med. 2014;46(5):324–9. https://doi.org/10.3109/07853890.2014.902226.
Chaput JP, Despres JP, Bouchard C, Astrup A, Tremblay A. Sleep duration as a risk factor for the development of type 2 diabetes or impaired glucose tolerance: analyses of the Quebec Family Study. Sleep Med. 2009;10(8):919–24. https://doi.org/10.1016/j.sleep.2008.09.016.
Gottlieb DJ, Punjabi NM, Newman AB, Resnick HE, Redline S, Baldwin CM, et al. Association of sleep time with diabetes mellitus and impaired glucose tolerance. Arch Intern Med. 2005;165(8):863–7. https://doi.org/10.1001/archinte.165.8.863.
Knutson KL, Van Cauter E, Zee P, Liu K, Lauderdale DS. Cross-sectional associations between measures of sleep and markers of glucose metabolism among subjects with and without diabetes: the Coronary Artery Risk Development in Young Adults (CARDIA) sleep study. Diabetes Care. 2011;34(5):1171–6. https://doi.org/10.2337/dc10-1962.
Cappuccio FP, D'Elia L, Strazzullo P, Miller MA. Quantity and quality of sleep and incidence of type 2 diabetes: a systematic review and meta-analysis. Diabetes Care. 2010;33(2):414–20. https://doi.org/10.2337/dc09-1124.
• Ferrie JE, Kivimaki M, Akbaraly TN, Tabak A, Abell J, Davey Smith G, et al. Change in sleep duration and type 2 diabetes: the Whitehall II study. Diabetes Care. 2015;38(8):1467–72. https://doi.org/10.2337/dc15-0186. This study showed that both persistent short sleepers and those who increased their sleep over five years had a higher risk of incident type 2 diabetes compared to those consistently sleeping 7 h a night.
Al Khatib HK, Hall WL, Creedon A, Ooi E, Masri T, McGowan L, et al. Sleep extension is a feasible lifestyle intervention in free-living adults who are habitually short sleepers: a potential strategy for decreasing intake of free sugars? A randomized controlled pilot study. Am J Clin Nutr. 2018;107(1):43–53. https://doi.org/10.1093/ajcn/nqx030.
Dong JY, Zhang YH, Qin LQ. Obstructive sleep apnea and cardiovascular risk: meta-analysis of prospective cohort studies. Atherosclerosis. 2013;229(2):489–95. https://doi.org/10.1016/j.atherosclerosis.2013.04.026.
Punjabi NM. The epidemiology of adult obstructive sleep apnea. Proc Am Thorac Soc. 2008;5(2):136–43. https://doi.org/10.1513/pats.200709-155MG.
Kushida CA, Littner MR, Morgenthaler T, Alessi CA, Bailey D, Coleman J Jr, et al. Practice parameters for the indications for polysomnography and related procedures: an update for 2005. Sleep. 2005;28(4):499–521.
Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013;177(9):1006–14. https://doi.org/10.1093/aje/kws342.
Resnick HE, Redline S, Shahar E, Gilpin A, Newman A, Walter R, et al. Diabetes and sleep disturbances: findings from the sleep heart health study. Diabetes Care. 2003;26(3):702–9.
Foster GD, Sanders MH, Millman R, Zammit G, Borradaile KE, Newman AB, et al. Obstructive sleep apnea among obese patients with type 2 diabetes. Diabetes Care. 2009;32(6):1017–9. https://doi.org/10.2337/dc08-1776.
Einhorn D, Stewart DA, Erman MK, Gordon N, Philis-Tsimikas A, Casal E. Prevalence of sleep apnea in a population of adults with type 2 diabetes mellitus. Endocr Pract. 2007;13(4):355–62. https://doi.org/10.4158/EP.13.4.355.
Bixler EO, Vgontzas AN, Lin HM, Ten Have T, Rein J, Vela-Bueno A, et al. Prevalence of sleep-disordered breathing in women: effects of gender. Am J Respir Crit Care Med. 2001;163(3 Pt 1):608–13. https://doi.org/10.1164/ajrccm.163.3.9911064.
Bixler EO, Vgontzas AN, Ten Have T, Tyson K, Kales A. Effects of age on sleep apnea in men: I. Prevalence and severity. Am J Respir Crit Care Med. 1998;157(1):144–8. https://doi.org/10.1164/ajrccm.157.1.9706079.
Young T, Shahar E, Nieto FJ, Redline S, Newman AB, Gottlieb DJ, et al. Predictors of sleep-disordered breathing in community-dwelling adults: the sleep heart health study. Arch Intern Med. 2002;162(8):893–900.
Ancoli-Israel S, Kripke DF, Klauber MR, Mason WJ, Fell R, Kaplan O. Sleep-disordered breathing in community-dwelling elderly. Sleep. 1991;14(6):486–95.
Duran J, Esnaola S, Rubio R, Iztueta A. Obstructive sleep apnea-hypopnea and related clinical features in a population-based sample of subjects aged 30 to 70 yr. Am J Respir Crit Care Med. 2001;163(3 Pt 1):685–9. https://doi.org/10.1164/ajrccm.163.3.2005065.
Tishler PV, Larkin EK, Schluchter MD, Redline S. Incidence of sleep-disordered breathing in an urban adult population: the relative importance of risk factors in the development of sleep-disordered breathing. JAMA. 2003;289(17):2230–7. https://doi.org/10.1001/jama.289.17.2230.
Heinzer R, Vat S, Marques-Vidal P, Marti-Soler H, Andries D, Tobback N, et al. Prevalence of sleep-disordered breathing in the general population: the HypnoLaus study. Lancet Respir Med. 2015;3(4):310–8. https://doi.org/10.1016/S2213-2600(15)00043-0.
Mirer AG, Young T, Palta M, Benca RM, Rasmuson A, Peppard PE. Sleep-disordered breathing and the menopausal transition among participants in the sleep in midlife women study. Menopause. 2017;24(2):157–62. https://doi.org/10.1097/GME.0000000000000744.
Peppard PE, Young T, Palta M, Dempsey J, Skatrud J. Longitudinal study of moderate weight change and sleep-disordered breathing. JAMA. 2000;284(23):3015–21.
Grunstein R, Wilcox I, Yang TS, Gould Y, Hedner J. Snoring and sleep apnoea in men: association with central obesity and hypertension. Int J Obes Relat Metab Disord. 1993;17(9):533–40.
Newman AB, Foster G, Givelber R, Nieto FJ, Redline S, Young T. Progression and regression of sleep-disordered breathing with changes in weight: the sleep heart health study. Arch Intern Med. 2005;165(20):2408–13. https://doi.org/10.1001/archinte.165.20.2408.
Araghi MH, Chen YF, Jagielski A, Choudhury S, Banerjee D, Hussain S, et al. Effectiveness of lifestyle interventions on obstructive sleep apnea (OSA): systematic review and meta-analysis. Sleep. 2013;36(10):1553–62, 62A-62E. https://doi.org/10.5665/sleep.3056.
Greenburg DL, Lettieri CJ, Eliasson AH. Effects of surgical weight loss on measures of obstructive sleep apnea: a meta-analysis. Am J Med. 2009;122(6):535–42. https://doi.org/10.1016/j.amjmed.2008.10.037.
Young T, Peppard PE, Taheri S. Excess weight and sleep-disordered breathing. J Appl Physiol (1985). 2005;99(4):1592–9. https://doi.org/10.1152/japplphysiol.00587.2005.
Mehra R, Stone KL, Blackwell T, Ancoli Israel S, Dam TT, Stefanick ML, et al. Prevalence and correlates of sleep-disordered breathing in older men: osteoporotic fractures in men sleep study. J Am Geriatr Soc. 2007;55(9):1356–64. https://doi.org/10.1111/j.1532-5415.2007.01290.x.
Lee RW, Vasudavan S, Hui DS, Prvan T, Petocz P, Darendeliler MA, et al. Differences in craniofacial structures and obesity in Caucasian and Chinese patients with obstructive sleep apnea. Sleep. 2010;33(8):1075–80.
Aronsohn RS, Whitmore H, Van Cauter E, Tasali E. Impact of untreated obstructive sleep apnea on glucose control in type 2 diabetes. Am J Respir Crit Care Med. 2010;181(5):507–13. https://doi.org/10.1164/rccm.200909-1423OC.
Kent BD, Grote L, Ryan S, Pepin JL, Bonsignore MR, Tkacova R, et al. Diabetes mellitus prevalence and control in sleep-disordered breathing: the European Sleep Apnea Cohort (ESADA) study. Chest. 2014;146(4):982–90. https://doi.org/10.1378/chest.13-2403.
Muraki I, Tanigawa T, Yamagishi K, Sakurai S, Ohira T, Imano H, et al. Nocturnal intermittent hypoxia and the development of type 2 diabetes: the Circulatory Risk in Communities Study (CIRCS). Diabetologia. 2010;53(3):481–8. https://doi.org/10.1007/s00125-009-1616-0.
Nagayoshi M, Punjabi NM, Selvin E, Pankow JS, Shahar E, Iso H, et al. Obstructive sleep apnea and incident type 2 diabetes. Sleep Med. 2016;25:156–61. https://doi.org/10.1016/j.sleep.2016.05.009.
Botros N, Concato J, Mohsenin V, Selim B, Doctor K, Yaggi HK. Obstructive sleep apnea as a risk factor for type 2 diabetes. Am J Med. 2009;122(12):1122–7. https://doi.org/10.1016/j.amjmed.2009.04.026.
Kendzerska T, Gershon AS, Hawker G, Tomlinson G, Leung RS. Obstructive sleep apnea and incident diabetes. A historical cohort study. Am J Respir Crit Care Med. 2014;190(2):218–25. https://doi.org/10.1164/rccm.201312-2209OC.
Sullivan CE, Issa FG, Berthon-Jones M, Eves L. Reversal of obstructive sleep apnoea by continuous positive airway pressure applied through the nares. Lancet. 1981;1(8225):862–5.
Iftikhar IH, Hoyos CM, Phillips CL, Magalang UJ. Meta-analyses of the association of sleep apnea with insulin resistance, and the effects of CPAP on HOMA-IR, adiponectin, and visceral adipose fat. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine. 2015;11(4):475–85. https://doi.org/10.5664/jcsm.4610.
Weinstock TG, Wang X, Rueschman M, Ismail-Beigi F, Aylor J, Babineau DC, et al. A controlled trial of CPAP therapy on metabolic control in individuals with impaired glucose tolerance and sleep apnea. Sleep. 2012;35(5):617–25B. https://doi.org/10.5665/sleep.1816.
Salord N, Fortuna AM, Monasterio C, Gasa M, Perez A, Bonsignore MR, et al. A randomized controlled trial of continuous positive airway pressure on glucose tolerance in obese patients with obstructive sleep apnea. Sleep. 2016;39(1):35–41. https://doi.org/10.5665/sleep.5312.
Pamidi S, Wroblewski K, Stepien M, Sharif-Sidi K, Kilkus J, Whitmore H, et al. Eight hours of nightly continuous positive airway pressure treatment of obstructive sleep apnea improves glucose metabolism in patients with prediabetes. A randomized controlled trial. Am J Respir Crit Care Med. 2015;192(1):96–105. https://doi.org/10.1164/rccm.201408-1564OC.
Ioachimescu OC, Anthony J Jr, Constantin T, Ciavatta MM, McCarver K, Sweeney ME. VAMONOS (veterans affairs’ metabolism, obstructed and non-obstructed sleep) study: effects of CPAP therapy on glucose metabolism in patients with obstructive sleep apnea. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine. 2017;13(3):455–66. https://doi.org/10.5664/jcsm.6502.
McEvoy RD, Antic NA, Heeley E, Luo Y, Ou Q, Zhang X, et al. CPAP for prevention of cardiovascular events in obstructive sleep apnea. N Engl J Med. 2016;375(10):919–31. https://doi.org/10.1056/NEJMoa1606599.
Babu AR, Herdegen J, Fogelfeld L, Shott S, Mazzone T. Type 2 diabetes, glycemic control, and continuous positive airway pressure in obstructive sleep apnea. Arch Intern Med. 2005;165(4):447–52. https://doi.org/10.1001/archinte.165.4.447.
Myhill PC, Davis WA, Peters KE, Chubb SA, Hillman D, Davis TM. Effect of continuous positive airway pressure therapy on cardiovascular risk factors in patients with type 2 diabetes and obstructive sleep apnea. J Clin Endocrinol Metab. 2012;97(11):4212–8. https://doi.org/10.1210/jc.2012-2107.
Donovan LM, Rueschman M, Weng J, Basu N, Dudley KA, Bakker JP, et al. The effectiveness of an obstructive sleep apnea screening and treatment program in patients with type 2 diabetes. Diabetes Res Clin Pract. 2017;134:145–52. https://doi.org/10.1016/j.diabres.2017.10.013.
Dawson A, Abel SL, Loving RT, Dailey G, Shadan FF, Cronin JW, et al. CPAP therapy of obstructive sleep apnea in type 2 diabetics improves glycemic control during sleep. J Clin Sleep Med : JCSM : Off Publ Am Acad Sleep Med. 2008;4(6):538–42.
West SD, Nicoll DJ, Wallace TM, Matthews DR, Stradling JR. Effect of CPAP on insulin resistance and HbA1c in men with obstructive sleep apnoea and type 2 diabetes. Thorax. 2007;62(11):969–74. https://doi.org/10.1136/thx.2006.074351.
Martinez-Ceron E, Barquiel B, Bezos AM, Casitas R, Galera R, Garcia-Benito C, et al. Effect of continuous positive airway pressure on glycemic control in patients with obstructive sleep apnea and type 2 diabetes A randomized clinical trial. Am J Respir Crit Care Med. 2016;194(4):476–85. https://doi.org/10.1164/rccm.201510-1942OC.
•• Shaw JE, Punjabi NM, Naughton MT, Willes L, Bergenstal RM, Cistulli PA, et al. The effect of treatment of obstructive sleep apnea on glycemic control in type 2 diabetes. Am J Respir Crit Care Med. 2016;194(4):486–92. https://doi.org/10.1164/rccm.201511-2260OC. This multicenter randomized trial showed that among patients with relatively well-controlled type 2 diabetes and obstructive sleep apnea, there was no effect of treating obstructive sleep apnea with CPAP on glycemic control.
Mokhlesi B, Grimaldi D, Beccuti G, Van Cauter E. Effect of one week of CPAP treatment of obstructive sleep apnoea on 24-hour profiles of glucose, insulin and counter-regulatory hormones in type 2 diabetes. Diabetes Obes Metab. 2017;19(3):452–6. https://doi.org/10.1111/dom.12823.
Leong WB, Jadhakhan F, Taheri S, Chen YF, Adab P, Thomas GN. Effect of obstructive sleep apnoea on diabetic retinopathy and maculopathy: a systematic review and meta-analysis. Diabet Med. 2016;33(2):158–68. https://doi.org/10.1111/dme.12817.
• Altaf QA, Dodson P, Ali A, Raymond NT, Wharton H, Fellows H, et al. Obstructive sleep apnea and retinopathy in patients with type 2 diabetes. A longitudinal study. Am J Respir Crit Care Med. 2017;196(7):892–900. https://doi.org/10.1164/rccm.201701-0175OC. In a clinic-based study, OSA was associated with sight threatening diabetic retinopathy cross-sectionally and progression to preproliferative/proliferative diabetic retinopathy longitudinally.
Mason RH, Kiire CA, Groves DC, Lipinski HJ, Jaycock A, Winter BC, et al. Visual improvement following continuous positive airway pressure therapy in diabetic subjects with clinically significant macular oedema and obstructive sleep apnoea: proof of principle study. Respiration. 2012;84(4):275–82. https://doi.org/10.1159/000334090.
Furukawa S, Saito I, Yamamoto S, Miyake T, Ueda T, Niiya T, et al. Nocturnal intermittent hypoxia as an associated risk factor for microalbuminuria in Japanese patients with type 2 diabetes mellitus. Eur J Endocrinol. 2013;169(2):239–46. https://doi.org/10.1530/EJE-13-0086.
Stadler S, Zimmermann T, Franke F, Rheinberger M, Heid IM, Boger CA, et al. Association of sleep-disordered breathing with diabetes-associated kidney disease. Ann Med. 2017;49(6):487–95. https://doi.org/10.1080/07853890.2017.1306100.
Tahrani AA, Ali A, Raymond NT, Begum S, Dubb K, Altaf QA, et al. Obstructive sleep apnea and diabetic nephropathy: a cohort study. Diabetes Care. 2013;36(11):3718–25. https://doi.org/10.2337/dc13-0450.
Gu X, Luo X, Wang X, Tang J, Yang W, Cai Z. The correlation between obstructive sleep apnea and diabetic neuropathy: a meta-analysis. Prim Care Diabetes 2018. https://doi.org/10.1016/j.pcd.2018.03.005.
Altaf QA, Ali A, Piya MK, Raymond NT, Tahrani AA. The relationship between obstructive sleep apnea and intra-epidermal nerve fiber density, PARP activation and foot ulceration in patients with type 2 diabetes. J Diabetes Complicat. 2016;30(7):1315–20. https://doi.org/10.1016/j.jdiacomp.2016.05.025.
Bureau of Labor Statistics U.S. Department of Labor. Workers on flexible and shift schedules in May 2004. 2005. https://www.bls.gov/news.release/pdf/flex.pdf.
McHill AW, Melanson EL, Higgins J, Connick E, Moehlman TM, Stothard ER, et al. Impact of circadian misalignment on energy metabolism during simulated nightshift work. Proc Natl Acad Sci U S A. 2014;111(48):17302–7. https://doi.org/10.1073/pnas.1412021111.
Buxton OM, Cain SW, O'Connor SP, Porter JH, Duffy JF, Wang W, et al. Adverse metabolic consequences in humans of prolonged sleep restriction combined with circadian disruption. Sci Transl Med. 2012;4(129):129ra43. https://doi.org/10.1126/scitranslmed.3003200.
Bescos R, Boden MJ, Jackson ML, Trewin AJ, Marin EC, Levinger I, et al. Four days of simulated shift work reduces insulin sensitivity in humans. Acta Physiol (Oxf). 2018;223(2):e13039. https://doi.org/10.1111/apha.13039.
Wang F, Zhang L, Zhang Y, Zhang B, He Y, Xie S, et al. Meta-analysis on night shift work and risk of metabolic syndrome. Obesity reviews : an official journal of the International Association for the Study of Obesity. 2014;15(9):709–20. https://doi.org/10.1111/obr.12194.
Liu Q, Shi J, Duan P, Liu B, Li T, Wang C et al. Is shift work associated with a higher risk of overweight or obesity? A systematic review of observational studies with meta-analysis. Int J Epidemiol 2018. https://doi.org/10.1093/ije/dyy079.
Gan Y, Yang C, Tong X, Sun H, Cong Y, Yin X, et al. Shift work and diabetes mellitus: a meta-analysis of observational studies. Occup Environ Med. 2015;72(1):72–8. https://doi.org/10.1136/oemed-2014-102150.
Knutsson A, Kempe A. Shift work and diabetes--a systematic review. Chronobiol Int. 2014;31(10):1146–51. https://doi.org/10.3109/07420528.2014.957308.
Pan A, Schernhammer ES, Sun Q, Hu FB. Rotating night shift work and risk of type 2 diabetes: two prospective cohort studies in women. PLoS Med. 2011;8(12):e1001141. https://doi.org/10.1371/journal.pmed.1001141.
American Academy of Sleep Medicine. International classification of sleep disorders. 3rd ed. Darien, IL: American Academy of Sleep Medicine; 2014.
Roth T, Coulouvrat C, Hajak G, Lakoma MD, Sampson NA, Shahly V, et al. Prevalence and perceived health associated with insomnia based on DSM-IV-TR; international statistical classification of diseases and related health problems, tenth revision; and research diagnostic criteria/international classification of sleep disorders, second edition criteria: results from the America insomnia survey. Biol Psychiatry. 2011;69(6):592–600. https://doi.org/10.1016/j.biopsych.2010.10.023.
Ford ES, Cunningham TJ, Giles WH, Croft JB. Trends in insomnia and excessive daytime sleepiness among U.S. adults from 2002 to 2012. Sleep Med. 2015;16(3):372–8. https://doi.org/10.1016/j.sleep.2014.12.008.
Ford DE, Kamerow DB. Epidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention? JAMA. 1989;262(11):1479–84.
Buysse DJ, Angst J, Gamma A, Ajdacic V, Eich D, Rossler W. Prevalence, course, and comorbidity of insomnia and depression in young adults. Sleep. 2008;31(4):473–80.
Morphy H, Dunn KM, Lewis M, Boardman HF, Croft PR. Epidemiology of insomnia: a longitudinal study in a UK population. Sleep. 2007;30(3):274–80.
Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev. 2002;6(2):97–111.
Lin CL, Chien WC, Chung CH, Wu FL. Risk of type 2 diabetes in patients with insomnia: a population-based historical cohort study. Diabetes Metab Res Rev. 2018;34(1). https://doi.org/10.1002/dmrr.2930.
Vgontzas AN, Liao D, Pejovic S, Calhoun S, Karataraki M, Bixler EO. Insomnia with objective short sleep duration is associated with type 2 diabetes: a population-based study. Diabetes Care. 2009;32(11):1980–5. https://doi.org/10.2337/dc09-0284.
Cespedes EM, Dudley KA, Sotres-Alvarez D, Zee PC, Daviglus ML, Shah NA, et al. Joint associations of insomnia and sleep duration with prevalent diabetes: the Hispanic Community Health Study/Study of Latinos (HCHS/SOL). J Diabetes. 2016;8(3):387–97. https://doi.org/10.1111/1753-0407.12308.
Gore M, Brandenburg NA, Dukes E, Hoffman DL, Tai KS, Stacey B. Pain severity in diabetic peripheral neuropathy is associated with patient functioning, symptom levels of anxiety and depression, and sleep. J Pain Symptom Manag. 2005;30(4):374–85. https://doi.org/10.1016/j.jpainsymman.2005.04.009.
Galer BS, Gianas A, Jensen MP. Painful diabetic polyneuropathy: epidemiology, pain description, and quality of life. Diabetes Res Clin Pract. 2000;47(2):123–8.
Chiu AF, Huang MH, Wang CC, Kuo HC. Higher glycosylated hemoglobin levels increase the risk of overactive bladder syndrome in patients with type 2 diabetes mellitus. Int J Urol. 2012;19(11):995–1001. https://doi.org/10.1111/j.1442-2042.2012.03095.x.
Skomro RP, Ludwig S, Salamon E, Kryger MH. Sleep complaints and restless legs syndrome in adult type 2 diabetics. Sleep Med. 2001;2(5):417–22.
Lopes LA, Lins Cde M, Adeodato VG, Quental DP, de Bruin PF, Montenegro RM Jr, et al. Restless legs syndrome and quality of sleep in type 2 diabetes. Diabetes Care. 2005;28(11):2633–6.
Merlino G, Fratticci L, Valente M, Del Giudice A, Noacco C, Dolso P, et al. Association of restless legs syndrome in type 2 diabetes: a case-control study. Sleep. 2007;30(7):866–71.
Plantinga L, Rao MN, Schillinger D. Prevalence of self-reported sleep problems among people with diabetes in the United States, 2005-2008. Prev Chronic Dis. 2012;9:E76.
Funding
This work was supported by NIH grant numbers HL082610 and HL127307.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Rachel P. Ogilvie declares that she has no conflict of interest. Sanjay R. Patel reports grants from the American Sleep Medicine Foundation, the ResMed Foundation, Bayer Pharmaceuticals, and Philips Respironics.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Diabetes Epidemiology
Rights and permissions
About this article
Cite this article
Ogilvie, R.P., Patel, S.R. The Epidemiology of Sleep and Diabetes. Curr Diab Rep 18, 82 (2018). https://doi.org/10.1007/s11892-018-1055-8
Published:
DOI: https://doi.org/10.1007/s11892-018-1055-8