Abstract
Purpose of Review
Diabetes affects about a third of all hospitalized patients and up to 50% of inpatients go on to experience hyperglycemia. Despite strong evidence supporting the importance of adequate glycemic control, as well detailed guidelines from major national organizations, many patients continue to have hypo- and hyperglycemia during their hospital stay. While this may be partially related to provider and patient-specific factors, system-based barriers continue to pose a major obstacle. Therefore, there is a need to go beyond merely discussing specific insulin protocols and provide guidance for effective models of care in the acute glycemic management of hospitalized patients.
Recent Findings
To date, there is limited data evaluating the various models of care for inpatient diabetes management in terms of efficacy or cost, and there is no summary on this topic guiding physicians and hospital administrators.
Summary
In this paper, four common models of inpatient diabetes care will be presented including those models led by the following: an endocrinologist(s), mid-level provider(s), pharmacist(s), and a virtual glucose management team. The authors will outline the intrinsic benefits as well as limitations of each model of care as well as cite supporting evidence, when available. Discussion pertaining to how a given model of care shapes and formulates a particular organization’s structured glucose management program (GMP) will be examined. Furthermore, the authors describe how the model of care chosen by an institution serves as the foundation for the creation of a GMP. Finally, the authors examine the critical factors needed for GMP success within an institution and outline the nature of hospital administrative support and accompanying reporting structure, the function of a multidisciplinary diabetes steering committee, and the role of the medical director.
Similar content being viewed by others
Introduction
Diabetes has been declared a pandemic by the Centers for Disease Control (CDC) [1]. In the U.S., it affects about 10% of the total population [2] and is prevalent within a third of all hospitalized patients [3, 4]. Inpatients with diabetes or hyperglycemia have increased length of stay (LOS), higher readmission rates, and higher rate of morbidity and mortality compared to those not afflicted with the aforementioned conditions [4, 5]. Given adverse outcomes associated with poor glycemic control, arguments can be made for the necessity of appropriate glucose control as reflected in recommendations by major international organizations [5, 6]. Many barriers often exist within healthcare systems serving as a hindrance to attainment of optimal glycemic outcomes [7]. Some of these barriers are inherent to the given disease process, while others are connected to the sheer volume and diversity of patients with hyperglycemia. Oftentimes, the underlying metabolic dysfunction is overshadowed or superimposed by the non-diabetes ailment(s) invoking the patient’s hospitalization. Consequently, the management of the patient’s blood glucose is frequently low on a given provider’s priority list. Furthermore, increasingly complex pharmacotherapeutic outpatient regimens usually require transition to insulin-based formulary alternative, a skill that is limited for many providers. Complex hospital system design, where patient care is often fragmented, creates additional challenges within organizations.
Hence, major national and international organizations (including American Diabetes Association (ADA), Endocrine Society, and many others)) have placed a significant amount of effort providing protocols and crafting guidelines aimed at helping healthcare providers (HCP) achieve optimal inpatient glucose control [5, 6]. However, little is known about the way these guidelines should be adopted and implemented within healthcare organizations, creating effective models of care. There is a need for high quality research to identify the most effective glycemic management program characteristics, model components, and the information system required to maintain them [7]. The goal of this manuscript is to describe common models used for inpatient diabetes management, provide evidence (when available) for their use, and offer recommendations for an array of choices that hospitals can consider when structuring their inpatient glucose management program.
In order to develop an appropriate model of care, we need to understand the three major factors that affect the creation of such models:
-
I.
Healthcare Providers
We will address the roles of physicians, trainees (residents and fellows), mid-level providers (physician assistants (PA) and nurse practitioners (APRN)), pharmacists, and address the specific roles and responsibilities of the medical director.
-
II.
Technology
We will address the role of technology and discuss how electronic glycemic management software (eGMS) systems may promote glucose management within a given organization.
-
III.
Healthcare Infrastructure
We will discuss how regulatory agencies and local hospital administrative factors impact and shape the development of models of care.
Finally, the author’s will provide recommendations for models of care that could be utilized or implemented across institutions differing in size and scope, provided available resources (e.g., from the more basic to the more comprehensive), as outlined in Table 1.
Healthcare Providers
Physicians
Endocrinologist
Many, but not all models of inpatient diabetes care rely heavily on services provided by an endocrinologist. Endocrinologist participation in the diabetes care model may be direct (individual consultants or as a part of multidisciplinary team) or indirect (leading system-wide model or through remote monitoring). We will discuss how the nature of the Endocrinologist’s involvement may be extrapolated to four unique models of care:
Endocrinologist as a Consultant
This is the most intuitive model of care when considering the traditional consult service. Upon receiving a consult, an endocrinologist provides assessment, writes orders, follows patients daily, and communicates with the primary medical service. Despite the widespread use of the traditional model, there are very few studies evaluating the glycemic outcomes of this model. Levetan et al. showed that consultation by an individual endocrinologist decreased the average LOS of hospitalized patients with a primary diagnosis of diabetes; the earlier the consultation, the shorter the LOS, in a direct linear relationship [8]. The obvious advantage of this specific model is that the most expert physician is in charge of direct patient care, which then generates billable services. The inherent disadvantage of this model is related to limited number of board certified endocrinologists in the USA, even more prominently illustrated in rural areas where typically endocrinology services are limited.
Endocrinologist as Part of a Diabetes Team
In this model, the endocrinologist leads a multidisciplinary team, typically consisting of mid-level providers such as NP or APRN. The mid-level providers are responsible for daily notes and orders, and interaction with attending physicians and nurses, while the endocrinologist oversees patient care and typically acts as a medical director for the institution. Mid-level providers also screen patients for hyperglycemia and work with medical teams to improve glucose control [9].
A randomized controlled prospective feasibility study of 179 hospitalized patients illustrated that a diabetes team intervention (endocrinologist, diabetes nurse educator, and registered dietician) significantly decreased the LOS for both patients with a primary as well as secondary diagnosis of diabetes. One month after the team intervention was initiated, 75% of patients in the intervention group were in good glycemic control, compared with 46% in the control group. Readmissions rates at 3 months were also significantly lower in the intervention group (15 vs. 32%, P = 0.01) [10].
Levetan et al. evaluated the effect of an endocrine (individual endocrinologist) and multidisciplinary diabetes team (endocrinologist, diabetes nurse educator, and registered dietician) consultation model had on hospital stay for patients with the primary diagnosis of diabetes. The average LOS for diabetes team patients was 56% shorter than that of a non-consultation group (P < 0.0001), and 35% shorter in patients who received a traditional individual endocrine consultation (P < 0.05). Endocrinologist-led inpatient diabetes teams have been shown to be effective in decreasing the LOS and also improving glycemic outcomes in various other studies [9,10,11].
As illustrated from the previous study, timely involvement of a consultant model directly correlates to and improves upon the outcome of care. However, endocrinologists are too often consulted after days of hyperglycemia and frequently, not at all. Currently, there are no set guidelines to identify which patients might benefit from diabetes team consultation and it is within the discretion of the primary team to make this decision. Rajendran et al. developed a scoring system to facilitate timely consultation. The diabetes patient at risk (DPAR) score incorporates a number of factors including the following: admissions for DKA/HHS, new onset diabetes, insulin naïve patients, insulin pump users, severe hypoglycemia, recurrent hypoglycemia, patients on steroids, specialized nutrition, and foot ulcer. Higher DPAR score was found to be valuable in successfully identifying appropriate patients and facilitated referrals in a timely manner to the diabetes team [12•].
The endocrinology team model described above strengthens multidisciplinary approach to patient care allowing each professional within the team to share different areas of expertise which also helps in improving the education of team as a whole.
Endocrinologists Leading a System-Wide Model
In this model, an endocrinologist oversees hospital-wide program which includes devising and implementing protocols to identify patients with hyper/hypoglycemia, developing web-based protocols/algorithms for management of these patients, education and training of the staff involved in care of these patients. Work by McDonnell et al. and Korytkowski et al., in particular, illustrates the powerful effect of endocrinologist leading the development of an inpatient glucose management program (GMP), fostering quality improvement of hospital inpatient care, as well as standardization of inpatient glycemic management [13,14,15,16]. The primary role of the endocrinologist is to serve as a leader of quality improvement initiatives, while also serving as a resource for complex cases. The success of this model depends upon the support that the hospital organization provides.
Virtual Glucose Monitoring
This is a novel approach in inpatient glucose management that does not involve an official consultation of the endocrine services; however, the physician is not directly involved in patient care. Rather, the electronic health record is used to generate a daily report of out-of-range glucose values to be reviewed by a number of diabetes specialists, who then remotely chart review and make pharmacotherapeutic recommendations via an electronic note.
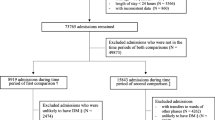
Rushakoff et al. evaluated the association between a virtual glucose management service (vGMS) and glycemic control in hospitalized adult patients. Based on daily glycemic reports, patients with two or more glucoses over 225 mg/dl and/or a glucose < 70 mg/dl in the past 24 h were identified by diabetes specialists (an endocrinologist or pharmacist-diabetes educator or nurse-CDE). A vGMS note with management recommendations was placed in electronic medical chart. Following the introduction of the vGMS, the proportion of hyperglycemic patients decreased 39% from a baseline of 6.5 per 100 patient-days to 4.0 per 100 patient-days. The hypoglycemia proportion decreased by 36% [17•].
Similar virtual monitoring named daily inpatient glycemic survey (DINGS) was undertaken by Mendez et al. [18]. In this study, using an electronic query hospitalized patients with glucose values < 70 or > 350 mg/dl were identified, their charts were reviewed by the team of multidisciplinary diabetes specialist providers. When opportunities for improvement were identified an electronic medical note was entered with recommendations to the primary team. After implementing the DINGS model, there was a significant decrease in patient-day mean glucose, percentage of patient-days with any value > 350 mg/dl, glycemic variability, and rates of hypoglycemia.
It is important to note that the “virtual” glucose management services do not replace, but rather usually compliment other models of care, via either the traditional consultant or the team model.
The above presented data illustrate the benefit of a dedicated inpatient diabetes consult service and virtual glucose monitoring. However, in the inpatient setting where specialists are not always present, one alternative model is the implementation of tele-health services. Telemedicine has been shown to be effective in inpatient management of other disease conditions like stroke [19] and has been utilized extensively for the outpatient management of diabetes as well [20]; however, there is currently no data on inpatient teleconsulting service for diabetes.
Hospitalists
Hospitalists have been a significant part of healthcare system and are now a mainstay of inpatient care. They are not only involved in direct care of patients with diabetes admitted under them but also frequently co-manage surgical patients with diabetes. Hospitalists with special interests in diabetes form a vital part of diabetes model of care through their involvement in hospital quality assurance and protocol development. They can work independently or in collaboration with an endocrinologist [21].
Residents and Trainees
Resident physicians form an integral part of the medical care team and are often the first contact with patients at academic institutions. The existence of knowledge gaps pertaining to insulin regimens, lack of awareness of existing hospital glycemic protocols and policies, and fear of hypoglycemia among resident physicians have been identified as most common barriers to glycemic care in various studies [22, 23]. It is important to address these deficits by proper education, as we know that education and experience during training years will influence future practice patterns. Education in the form of case-based study [24], computer training programs [25], dissemination of hospital guidelines, and protocols for inpatient diabetes management using mobile-based tools [26] have all been shown to be effective at improving healthcare professionals’ knowledge with inpatient diabetes management.
Endocrinology Fellows
Endocrinology fellows are a valuable part of the inpatient diabetes care model. The intense training and experience they receive in direct diabetes care fosters their ability to design patient-tailored insulin regimens as well as manage hyperglycemia in patients with complex conditions (e.g., patients on insulin pump therapy, concurrent steroid use, nutritional support). In turn, fellows can impart the knowledge they received to the residents and medical students, thus forming a model for layered learning [14, 15].
Mid-Level Providers: Nurse Practitioners and Physician Assistants
Mid-level providers, when incorporated within a model of diabetes care, have demonstrated the ability to effectively care for broad population of patients with diabetes. Different models are described in the literature:
Endocrine APRN Team: APRN-Led by a Clinical Endocrinologist
Wallia et al. described inpatient endocrine glucose management service (GMS), comprised of APRN overseen by an attending endocrinologist [27]. This service developed and implemented insulin protocols for management of heart transplant patients and empowered ICU nurses to initiate consultation with the APRN team. The APRNs followed a clearly outlined therapeutic protocol facilitating transition of patients from intravenous insulin drip to subcutaneous insulin. Patients achieved adequate glucose control, while the occurrence of hypoglycemia during the insulin therapy of heart transplant patient was very rare. The key elements assuring the success of this program were the fact that the APRN were given a clear protocol outlining insulin adjustments, deviations were allowed as clinically indicated, daily rounds were performed by GMS, and APRNs were an integral part of the protocol development and adjustment.
APRN’s Cross-Trained in Inpatient Diabetes Management
Mackey et al. described a model of diabetes care assisted by an APRN(s)/PA(s) trained in inpatient diabetes management [28•]. Their involvement resulted in a greater use of recommended basal-bolus insulin therapy which correlated with lower mean glucose levels before discharge in a subset of non-critically ill patients. In a similar model, described by Apsey et al. [29], the APRN was recruited from a surgical department and received further training on inpatient diabetes management from an academic endocrine service. Subsequently, the APRN monitored all glucose levels for patients on a surgery service and contacted the surgery service with specific advice about starting and adjusting insulin therapy. Compared to historical control, this model led to greater utilization of a basal-bolus protocol and improved glucose control without increasing hypoglycemia.
Given limited endocrinology resources that most hospitals face, these models of care offer a potential to meet the needs of the larger patient population. Adapting a APRN/PA model of care for use outside an endocrinology consult service can be further explored as a way to bring expertise to a broader inpatient population with diabetes.
Remote Monitoring Led by APRNs
In a pilot study by Donihi et al., the authors developed a Targeted Glycemic Management (TGM) service composed of a diabetes nurse-educator, two nurse-practitioners, a pharmacist, and a dietician [30]. Patients with a BG level ≥ 300 mg/dL were identified using daily glycemic reports, and their charts were then reviewed by the TGM service. If no appropriate action was taken by the primary team to correct the hyperglycemia, a templated note was placed in the patient’s chart reinforcing the availability of existing protocols and order-sets for inpatient glycemic management. No specific insulin dosing change was recommended, rather, diabetes team consultation was advised for challenging patients and those on insulin pumps. The TGM pilot intervention lasted for 12 weeks. Comparison was then made in glycemic outcomes and provider’s response to hyperglycemia between pre-, during, and post-TGM implementation. There was significant improvement noted in the percentage of patients with hyperglycemia during TGM period compared to pre- and post-TGM periods. There was also a significant improvement in provider response to severe hyperglycemia during the TGM period (49 vs. 73 vs. 50%, before, during, and after TGM, respectively; P = 0.044).
Pharmacists
Pharmacists have the potential to bridge the gap and enhance models of inpatient diabetes care, as non-physician healthcare providers, regardless of a given institution’s size or scope of the patient population that is served. When provided with organizational leadership and provider support, pharmacists have demonstrated the propensity to not only improve specific institutional glycemic outcome measures but also lower healthcare costs associated with delivering enhanced patient care. The aforementioned improvements have been captured through the direct result of organizations implementing collaborative practice agreements, enhancing the scope of practice for their given pharmacists [31,32,33]. Expanded authorization given to these pharmacists would include the ability to make changes to the type, dosing, and frequency of insulin utilized as well as to any accompanying laboratory monitoring associated with the insulin regimen implemented.
Warrington et al. demonstrated that when a multidisciplinary glucose management team (GMT) (comprised of hospitalists, internists, nurses, and dieticians) led by a pharmacist (Pharm.D.), were given the organizational authority to direct inpatient glycemic management through a collaborative practice agreement, an improvement in both glycemic and clinical outcomes were noted in cardiac surgery patients [31]. The pharmacist-led GMT was able to demonstrate a statistically significant improvement in post-op day 1 and day 2 blood glucose levels exceeding 200 mg/dL following cardiac surgery versus a historical model of care. Improvement in the occurrence of hypoglycemic events was noted, as well is improved incidence of sternal wound infections (pharmacist-led GMT 3.18% (2010) vs. historical model 6.57% (2008)).
Similarly, Mularski et al. analyzed the impact of collaborative practice protocol, empowering a group of pharmacists termed the glycemic control team (GCT), on post-operative glycemic outcomes in surgical and medical patients [32•]. The GCT pharmacists had the ability to initiate, modify, change insulin orders, as well as all associative laboratory orders (e.g., A1c, serum creatinine). The pharmacist managed GCT was able to demonstrate a statistically significant improvement in post-op blood glucose readings, within the defined target range of 70–180 mg/dL, on day 1 (odds ratio [OR] 3.10, 95% CI, 2.62–3.67, p < 0.0001) and day 2 ([OR] 1.65, 95% CI, 1.34–2.04, p < 0.0001) versus a historical model of care not managed by pharmacists. Moreover, the pharmacist managed GCT had a statistically significant improvement in the occurrence of hypoglycemia (defined as a blood glucose < 70 mg/dL) on post-operative days 1 through 3 versus that seen with the existing model of care during a similar time period (OR 0.34, 95% CI, 0.28–0.40, p < 0.0001).
Last, Hodges et al. demonstrated that when pharmacists were utilized via a consultation model, they could improve institutional hyperglycemia outcomes (measured by mean blood glucose) within a community hospital [33]. Utilizing a multimodal weight-based insulin dosing protocol, over a 3-month duration, patients that had their blood glucose treated via a pharmacist-directed model were shown to attain mean blood glucose values ≤ 80 mg/dL on day 3 of hospitalization versus patients that were receiving physician-managed glycemic care.
In summary, pharmacists have demonstrated the ability to safely and effectively positively impact clinical outcomes pertaining to models of care related to glycemic management, when empowered by institutional leadership.
Pharmacy Stewardship
Stewardship is a commonly referred term utilized within healthcare today, usually in the context of antimicrobial stewardship programs (ASP) for hospitals where pharmacists serve as indispensable members of the antimicrobial team, working within a multidisciplinary group of healthcare providers [34,35,36,37,38]. Paterson et al. described the term stewardship in 2006 when describing ASP as “healthcare programs focusing on ensuring the proper use of medications to provide the best patient outcomes, lessen the risk of adverse effects, promote cost-effectiveness, while reducing the levels of sentinel events.” [39] Building upon the aforementioned description, in the presence of an increasingly large proportion of inpatients with a known comorbidity of diabetes, author’s institution initiated a unique model of care with the creation of the diabetes stewardship pharmacist. The purpose of the Diabetes Stewardship position was to facilitate further expansion, collaboration, as well as serve in a complimentary role within the existing GMP to improve upon organizational glycemic outcomes (Fig. 1). Collaborating with existing professional lines within the organization (CDEs; inpatient pharmacy service lines; nursing and medical staff; system analysts for the electronic record system) as well as serving as an extension to the diabetes, endocrine, and metabolism (DEM) specialty service line; the diabetes stewardship pharmacist constructed an institutional glycemic quality improvement model of care based upon a “vertical” and “horizontal” approach [40].
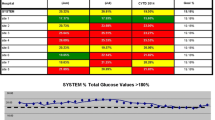
In the author’s organization, a “vertical approach” was implemented via an organizational virtual surveillance tool constructed within the electronic medical record (EMR) system, termed “diabetes stewardship dashboard” (Fig. 2). The diabetes stewardship pharmacist utilizes the EMR dashboard on a daily basis to efficiently and effectively identify, triage, and make therapeutic recommendations. Integration of the diabetes dashboard within the existing framework of our organization’s EMR, staffing model (i.e., team-based pharmacist incorporated within multidisciplinary rounds), electronic communications systems (i.e., electronic messaging applications), as well as documentation within the EMR has allowed the diabetes stewardship pharmacist the capability to communicate evidence-based glycemic recommendations throughout the organization while being centrally stationed.
It should be noted that the diabetes stewardship pharmacist does not write direct orders within the EMR. Rather the pharmacist provides electronic recommendations and works directly with the primary medical team’s pharmacist to convey appropriate recommendations (Fig. 3) who in turn ensures those are appropriately considered and tailored by the medical team given the patient’s current clinical status. This approach has many similarities to the physician-led initiative described by Rushakoff et al. [41].
In addition, enhancements to institutional glycemic management systems, based on a “horizontal approach,” which is comprised of multiple layers that include institutional glycemic education (references, pocket cards, discipline-specific education); policy, procedure and protocol development as well as amendment; formulary management; construction of therapeutic interchanges; EMR system level enhancements to improve all discipline prescribing and management of diabetic patients; as well as others.
Our diabetes stewardship pharmacist serves as an extension to the endocrine team, and offers a novel consideration to the models of care outlined within this manuscript. Organizations without an endocrinologist could adopt a similar model in partnership with other disciplines including hospitalist(s) or APRN/PA run inpatient diabetes program.
Technology
At the core of any given model of care is the safe and effective delivery of care. Glycemic management of inpatients with diabetes is inherently difficult in nature due to multiple variables related to physician, patient, and organizational factors, complicating the medical decision-making process even for the most experienced endocrinologist. Therefore, there is a significant need to create tools which support and foster improved selection of appropriate treatment strategies while serving the model of care.
Computerized Protocols and Computerized Physician Order Entry
The development of order sets by itself does not necessarily ensure best care practices due to lack of complete standardization and a variable rate of adoption. Thus, the efficacy of order set is difficult to evaluate in isolation of other quality initiatives. A Schnipper et al. effectively evaluated this issue and found that the addition of an order set built into a hospital’s computerized physician order entry (CPOE) system was associated with improved glucose control in comparison with physician and nurse education and a glycemic management protocol alone [42]. From that perspective appropriate integration of CPOE into physician work flow as well as patient care work flow is an important element assuring successes of any particular model of care.
Electronic Glycemic Management Software System (eGMS): EndoTool © and Glucommander ©
Currently, there are several commercially available, FDA approved, eGMS systems on the market. These computerized software systems utilize evidence-based algorithms to provide real-time insulin dosing recommendations (intravenous and subcutaneous) to healthcare providers serving acutely ill patients. Utilizing patient-specific characteristics imputed from healthcare staff or data that is directly pulled from an organization’s EMR (age, weight, height, renal function, home insulin regimen), the eGMS system provides specific insulin dosing guidance and recommendations (intravenous, subcutaneous, transition of care from IV to SubQ) to frontline staff in real-time. The patient specific dosing recommendations continuously adapt to a given resultant blood glucose value, hemoglobin A1c results, rate of blood glucose change over time, as well as individualized insulin sensitivity factors computed by the software. These eGMS systems have demonstrated the ability to positively affect multiple glycemic outcomes (hyperglycemia and hypoglycemia occurrence, time within and time to achieve glycemic target range), decrease institutional cost expenditure for select patient populations, as well as increase provider and nursing staff satisfaction scores relating to the ease of use and perceived effectiveness of the software system [43].
The advantages of incorporating an eGMS system within an institution’s model of care include: standardizing insulin prescribing, diminish clinical inertia, decrease human calculation errors, and improve glucometrics. The eGMS systems offer a potential to address an endocrinologist or provider gap present within their organization. Limitations to the use of an eGMS system include the cost to acquire and maintain the software solution, ability to integrate the given software within an existing EMR, IT support to address the initial build, software updates, and down-time support, institutional education and training that would need to be constructed, disseminated, and implemented across an entire organization, as well as adaptations to discipline specific work-flows that would need to follow to effectively implement and sustain the utility of the eGMS system.
In summary, when utilized in the aforementioned manner, technology serves as an active member of the models of care for organizations large and small, influencing the approach, cost, resource support, as well as the very infrastructure of an organization.
Healthcare Infrastructure
Hospital infrastructure may very well be the most important component facilitating effective models of care. An organization’s infrastructure provides the framework for model integration of providers, processes, and technology, and allows a creation of inpatient diabetes program (IDP) also frequently called glucose management program (GMP). Over a decade ago, the American College of Endocrinology and American Diabetes Association endorsed the need for formation of Inpatient Diabetes Programs and published a consensus statement recommending the resources warranted of the following: (a) administrative support; (b) multidisciplinary steering committee; (c) regular assessment of processes, quality of care, and barriers; (d) development of interventions such as protocols, policies, and algorithms; and (e) metrics for programmatic evaluation [44]. While the clinical practice guidelines recommend that hospital provide administrative support for GMPs, there are no standards for the specific infrastructure requirement that takes into the account the hospital size or patient case mix or the minimum financial support for the execution of the program. The literature has accumulated some data on the minimum startup cost for the program [14] as well as the support for the salary of the medical director, at minimum annual 15% director full time equivalent [14]. The aforementioned ambiguities surrounding hospital support for GMP may be related to the fact that there is currently a lack of mandate by government bodies including CMS and Joint Commission that have traditionally standardized the management of other disease processes including infections disease and heart failure. The Joint Commission offers hospitals Advanced Certification in Inpatient Diabetes, but participation is voluntary, and not tied to direct financial reward for the institution. Furthermore, standardization of glucometrics and benchmarking among institutions is still in development [7] with the most robust program developed and described by Maynard et al. [21] enrolling around 161 hospitals to date. Furthermore, it is not clear where the best “home” for GMPs should reside, as some of them function within the domain of Patient Safety while others serve as a disease-specific sector encapsulated within Risk Management. Thus, incentives for hospitals to put effort and resources into organizing highly effective GMPs are somewhat limited.
The formal GMP is considered to be the “best practice standard” for delivering inpatient glycemic care and forms the backbone for any model of care. GMPs have been shown to reduce: LOS [8, 9], wound infection rates, and hospital readmission rates [16]. Defining and optimizing GMP’s operational structure for a particular institution is crucial to the success of any model of care. Figure 1 illustrates the possible approaches to the structure of GMP. The key stakeholders of GMP are the following: diabetes nurse case managers, diabetes resource nurses, pharmacists, program director or a program lead, and a medical director.
Diabetes nurse case managers are certified diabetes educators involved in day-to-day management of high-risk hospitalized patients. In addition to providing care by consultation, they screen all hospitalized patients for hypo- and hyperglycemia, and in this manner, uncover hospital-wide opportunities for improvement in glucose control. It is estimated that one case manager for ~ 150 hospitalized patients is needed for a typical organization [9]. Diabetes case managers also support diabetes resource nurses—unit nurses designated as local “Diabetes Champions” who receive an extra training in diabetes management and become a resource to other floor nurses to assist with diabetes related questions [9, 45]. We are also proposing a crucial role for the pharmacist (Figs. 1 and 3) either as medication safety pharmacist for the organization or designated diabetes stewardship pharmacist as discussed above. The program typically has a program director or a program lead, depending on institution size and reporting structure. This operational role is usually given to a nurse (RN, CDE) that works closely with the medical director in order to implement system wide initiatives recommended by Diabetes Steering Committee. The Lead is responsible for implementation of educational initiatives, reporting of glucometrics, Joint Commission accreditation (if applicable), as well as provides education to Case Managers. Medical director is a physician champion, responsible for implementation of policies decided on by the Diabetes Steering Committee who provides direct oversight of glucose quality initiatives and reports to executive-level leadership. In terms of educational/training background, this role is typically given to an endocrinologist (where one is present) or a hospitalist. Perhaps more impactful than formal qualifications, it is important to note that this physician should have a skill set beyond the expertise in day to day glucose management. This physician needs to understand glucometrics, be able to perform data analysis in order to assess the impact of quality initiative, have leadership skills needed to lead the program and communicate effectively with the C-suite. Essentially, the medical director needs to have basic skill set of a clinical researcher and an epidemiologist, a role that has been dubbed the “Diabetes Healthcare Epidemiologist” by Mathiouddakis et al. [46].
There are three critical factors contributing to the success of a GMP:
-
1.
Presence of hospital administrative support
-
2.
Creation of multidisciplinary diabetes steering committee (DSC)
-
3.
Identification of healthcare provider champion, who typically serves as a medical director for GMP.
Institutional administrative support is necessary to assure adequate support for the medical director, to empower DSC’s executive function, as well as to ensure support for glucometrics evaluation and to assure the effective reporting system.
Diabetes steering committee is an overseeing committee that facilitates the work of GMP. The structure is outlined in Fig. 4. This centralized multidisciplinary group is charged with making decisions and implementing the necessary changes related to system-wide glycemic control. The role of the DSC is to work on quality initiatives for an institution, including creating and editing of order sets, review incident report errors, and use them to target ongoing education of institutional healthcare providers, provide safety recommendations, and define quality outcomes for the organizations such as glucometrics. The chair of Diabetes Steering Committee is usually the medical director of the glucose management program or it can be co-chaired by the inpatient program lead/director (RN) and the medical director (MD) as is the case in the author’s institution. It is important to get broad membership reflecting all stakeholders which include but are not limited to endocrinologist/diabetologist, mid-level providers, endocrine pharmacist, Hospitalist, Nurse Educators, Dietician, Floor nurses, Laboratory, and IT personnel.
In order to be effective, the DSC must have an authoritative rather than consultative nature and a clearly outlined reporting structure. Ideally, the DSC serves an avenue of communication to other leadership groups including Pharmacy and Therapeutics, Medication safety committees, and Quality Improvement committee.
The optimal reporting structure is organization dependent, and suggested approach is outlined in Fig. 4.
Models Summary
All the models of care presented so far confer the fundamental quality of multidisciplinary approach as the integral part of the diabetes care and include participation of physicians, mid-level providers, and pharmacists as active members of the team. There is no such thing as a “best model” or “one size fits all” as all of them need to be adapted to fit a particular institution’s need. As suggested by Pietras et al. [14], the optimal program structure should be tailored to reflect three major characteristics of the hospital environment: institutional infrastructure, patient acuity and complexity, and available provider expertise.
Table 1 summarizes multiple model examples that can be considered for a broad spectrum of institutions, ranging from community to academic, rural to urban. Irrespective of the program structure, the multidisciplinary nature of the model is essential to its success. Interaction between providers fosters the mutual education and management support that are fundamental to diabetes care. In teaching institutions, additional value of the service is to provide training not only to fellows, residents, and medical students but also pharmacy residents, APRN/PA students whenever possible, as future champions for diabetes care.
Conclusions
Several successful models of inpatient diabetes care have been published and have been illustrated within this manuscript. Each given model of care described, confer the fundamental quality of utilizing a multidisciplinary approach to serve as an integral foundation for the successful model of diabetes care, evidenced through incorporation of physicians, mid-level providers, and pharmacists. It should be noted that there is no such thing as a “best model of care.” Each model needs to be adapted to fit a particular institutional infrastructure, while addressing patient complexity as well as draw upon the provider expertise readily available within a given institution. Once a model has been chosen, it forms the backbone of hospital’s GMP. The fundamental factors contributing to the success of GMP are the choice of model of care, hospital administrative support, and effective oversight provided by multidisciplinary DSC.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Herman WH, Zimmet P. Type 2 diabetes: an epidemic requiring global attention and urgent action. Diabetes Care. 2012;35(5):943–4.
Centers for Disease Control and Prevention. National Diabetes Statistics Report, 2017. Atlanta, GA: Centers for Disease Control and Prevention, U.S. Dept of Health and Human Services; 2017.
Donnan PT, Leese GP, Morris AD, Diabetes A, Research in Tayside SMMUC. Hospitalizations for people with type 1 and type 2 diabetes compared with the nondiabetic population of Tayside, Scotland: a retrospective cohort study of resource use. Diabetes Care. 2000;23(12):1774–9. https://doi.org/10.2337/diacare.23.12.1774.
Umpierrez GE, Isaacs SD, Bazargan N, You X, Thaler LM, Kitabchi AE. Hyperglycemia: an independent marker of in-hospital mortality in patients with undiagnosed diabetes. J Clin Endocrinol Metab. 2002;87(3):978–82. https://doi.org/10.1210/jcem.87.3.8341.
Umpierrez GE, Hellman R, Korytkowski MT, Kosiborod M, Maynard GA, Montori VM, et al. Management of hyperglycemia in hospitalized patients in non-critical care setting: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2012;97(1):16–38. https://doi.org/10.1210/jc.2011-2098.
ADA standards of care 2017. Diabetes Care 2017 Jan ; 40 (Supplement 1).
Draznin B, Gilden J, Golden SH, Inzucchi SE, investigators P, Baldwin D, et al. Pathways to quality inpatient management of hyperglycemia and diabetes: a call to action. Diabetes Care. 2013;36(7):1807–14. https://doi.org/10.2337/dc12-2508.
Levetan CS, Salas JR, Wilets IF, Zumoff B. Impact of endocrine and diabetes team consultation on hospital length of stay for patients with diabetes. Am J Med. 1995;99(1):22–8. https://doi.org/10.1016/S0002-9343(99)80100-4.
Newton CA, Young S. Financial implications of glycemic control: results of an inpatient diabetes management program. Endocr Pract. 2006;12(Suppl 3):43–8. https://doi.org/10.4158/EP.12.S3.43.
Koproski J, Pretto Z, Poretsky L. Effects of an intervention by a diabetes team in hospitalized patients with diabetes. Diabetes Care. 1997;20(10):1553–5. https://doi.org/10.2337/diacare.20.10.1553.
Puig J, Supervia A, Marquez MA, Flores J, Cano JF, Gutierrez J. Diabetes team consultation: impact on length of stay of diabetic patients admitted to a short-stay unit. Diabetes Res Clin Pract. 2007;78(2):211–6. https://doi.org/10.1016/j.diabres.2007.03.010.
• Rajendran R, Round RM, Kerry C, Barker S, Rayman G. Diabetes patient at risk score—a novel system for triaging appropriate referrals of inpatients with diabetes to the diabetes team. Clin Med (Lond). 2015;15(3):229–33. This study provides a scoring system to identify patients who would beneft from diabetes team consultation. https://doi.org/10.7861/clinmedicine.15-3-229.
Korytkowski M, Dinardo M, Donihi AC, Bigi L, Devita M. Evolution of a diabetes inpatient safety committee. Endocr Pract. 2006;12(Suppl 3):91–9. https://doi.org/10.4158/EP.12.S3.91.
Pietras SM, Hanrahan P, Arnold LM, Sternthal E, McDonnell ME. State-of-the-art inpatient diabetes care: the evolution of an academic hospital. Endocr Pract. 2010;16(3):512–21. https://doi.org/10.4158/EP09319.CO.
Munoz M, Pronovost P, Dintzis J, Kemmerer T, Wang NY, Chang YT, et al. Implementing and evaluating a multicomponent inpatient diabetes management program: putting research into practice. Jt Comm J Qual Patient Saf. 2012;38(5):195–206. https://doi.org/10.1016/S1553-7250(12)38025-2.
Olson L, Muchmore J, Lawrence CB. The benefits of inpatient diabetes care: improving quality of care and the bottom line. Endocr Pract. 2006;12(Suppl 3):35–42. https://doi.org/10.4158/EP.12.S3.35.
• Rushakoff RJ, Sullivan MM, MacMaster HW, Shah AD, Rajkomar A, Glidden DV, et al. Association between a virtual glucose management service and glycemic control in hospitalized adult patients: an observational study. Ann Intern Med. 2017;166(9):621–7. Recent study evaluating the effect of remote monitoring on glycemic control. https://doi.org/10.7326/M16-1413.
Mendez CE, Ata A, Rourke JM, Stain SC, Umpierrez G. Daily inpatient glycemic survey (Dings): a process to remotely identify and assist in the management of hospitalized patients with diabetes and hyperglycemia. Endocr Pract. 2015;21(8):927–35. https://doi.org/10.4158/EP14577.OR.
Johansson T, Wild C. Telemedicine in acute stroke management: systematic review. Int J Technol Assess Health Care. 2010;26(2):149–55. https://doi.org/10.1017/S0266462310000139.
Shea S, Weinstock RS, Teresi JA, Palmas W, Starren J, Cimino JJ, et al. A randomized trial comparing telemedicine case management with usual care in older, ethnically diverse, medically underserved patients with diabetes mellitus: 5 year results of the IDEATel study. J Am Med Inform Assoc. 2009;16(4):446–56. https://doi.org/10.1197/jamia.M3157.
Maynard G, Kulasa K, Ramos P, Childers D, Clay B, Sebasky M, et al. Impact of a hypoglycemia reduction bundle and a systems approach to inpatient glycemic management. Endocr Pract. 2015;21(4):355–67. https://doi.org/10.4158/EP14367.OR.
Cheekati V, Osburne RC, Jameson KA, Cook CB. Perceptions of resident physicians about management of inpatient hyperglycemia in an urban hospital. J Hosp Med. 2009;4(1):E1–8. https://doi.org/10.1002/jhm.383.
Cook CB, McNaughton DA, Braddy CM, Jameson KA, Roust LR, Smith SA, et al. Management of inpatient hyperglycemia: assessing perceptions and barriers to care among resident physicians. Endocr Pract. 2007;13(2):117–24. https://doi.org/10.4158/EP.13.2.117.
Tamler R, Green DE, Skamagas M, Breen TL, Looker HC, Babyatsky M, et al. Effect of case-based training for medical residents on inpatient glycemia. Diabetes Care. 2011;34(8):1738–40. https://doi.org/10.2337/dc11-0517.
Vaidya A, Hurwitz S, Yialamas M, Min L, Garg R. Improving the management of diabetes in hospitalized patients: the results of a computer-based house staff training program. Diabetes Technol Ther. 2012;14(7):610–8. https://doi.org/10.1089/dia.2011.0258.
Desimone ME, Blank GE, Virji M, Donihi A, DiNardo M, Simak DM, et al. Effect of an educational Inpatient Diabetes Management Program on medical resident knowledge and measures of glycemic control: a randomized controlled trial. Endocr Pract. 2012;18(2):238–49. https://doi.org/10.4158/EP11277.OR.
Wallia A, Gupta S, Garcia C, Schmidt K, Oakes DJ, Aleppo G, et al. Examination of implementation of intravenous and subcutaneous insulin protocols and glycemic control in heart transplant patients. Endocr Pract. 2014;20(6):527–35. https://doi.org/10.4158/EP13354.OR.
• Mackey PA, Boyle ME, Walo PM, Castro JC, Cheng MR, Cook CB. Care directed by a specialty-trained nurse practioner or physician assistant can overcome clinical inertia in management of inpatient diabetes. Endocr Pract. 2014;20(2):112–9. This study evaluated a model led by cross trained mid level providers in inpatient diabetes management. https://doi.org/10.4158/EP13201.OR.
Apsey HA, Coan KE, Castro JC, Jameson KA, Schlinkert RT, Cook CB. Overcoming clinical inertia in the management of postoperative patients with diabetes. Endocr Pract. 2014;20(4):320–8. https://doi.org/10.4158/EP13366.OR.
Donihi AC, Gibson JM, Noschese ML, DiNardo MM, Koerbel GL, Curll M, et al. Effect of a targeted glycemic management program on provider response to inpatient hyperglycemia. Endocr Pract. 2011;17(4):552–7. https://doi.org/10.4158/EP10330.OR.
Warrington L, Ayers P, Baldwin AM, Wallace V, Riche KD, Saulters R, et al. Implementation of a pharmacist-led, multidisciplinary diabetes management team. Am J Health Syst Pharm. 2012;69(14):1240–5. https://doi.org/10.2146/ajhp110297.
• Mularski KS, Yeh CP, Bains JK, Mosen DM, Hill AK, Mularski RA. Pharmacist glycemic control team improves quality of glycemic control in surgical patients with perioperative dysglycemia. Perm J. 2012;16(1):28–33. This study evaluated how a pharmacist-led model of care impacted postoperative glycemic outcomes in surgical patients.
Hodges A, Hall J, Castellanos E, Laue E, Ellis T, Oelschlaeger L. Implementing a pharmacist consultation model for multimodal insulin therapy. Am J Health Syst Pharm. 2017;74(9):e224–9. https://doi.org/10.2146/ajhp150941.
Joint Commission Perspectives®, July 2016. 36(7):1–8.
Heyerly A, Jones R, Bokhart G, Shoaff M, Fisher D. Implementation of a pharmacist-direct antimicrobial stewardship protocol utilizing rapid diagnostic testing. Hosp Pharm. 2016;51(10):815–22. https://doi.org/10.1310/hpj5110-815.
Wenzler E, Wang F, Goff DA, Prier B, Mellett J, Mangino JE, et al. An automated, pharmacist-driven initiative improves quality of care for Staphylococcus aureus bacteremia. Clin Infect Dis. 2017;65(2):194–200. https://doi.org/10.1093/cid/cix315.
Zhang X, Rowan N, Pflugeisen BM, Alajbegovic S. Urine culture guided antibiotic interventions: a pharmacist driven antimircrobial stewardship effort in the ED. Am J Emerg Med. 2017;35(4):594–8. https://doi.org/10.1016/j.ajem.2016.12.036.
Heil EL, Kuti JL, Bearden DT, Gallagher JC. The essential role of pharmacists in antimicrobial stewardship. Infect Control Hosp Epidemiol. 2016;37(7):753–4. https://doi.org/10.1017/ice.2016.82.
Paterson DL. The role of antimicrobial management programs in optimizing antibiotic prescribing within hospitals. Clin Infect Dis. 2006;42(2):S90–5. https://doi.org/10.1086/499407.
Golmann A, Yokoe S. Approaches for preventing healthcare-associated infections: go long or go wide? Infect Control Hosp Epidemiol. 2014;35(7):797–801.
Rushakoff RJ, Rushakoff JA, Kornberg Z, MacMaster HW, Shah AD. Remote monitoring and consultation of inpatient populations with diabetes. Curr Diab Rep. 2017;17(9):70. https://doi.org/10.1007/s11892-017-0896-x.
Schnipper JL, Liang CL, Ndumele CD, Pendergrass ML. Effects of a computerized order set on the inpatient management of hyperglycemia: a cluster-randomized controlled trial. Endocr Pract. 2010;16(2):209–18. https://doi.org/10.4158/EP09262.OR.
Espina C, Jenkins I, Taylor L, Farah R, Cho E, Epworth J, et al. Blood glucose control using a computer-guided glucose management system in allogeneic hematopoietic cell transplant recipients. Bone Marrow Transplant. 2016;51(7):973–9. https://doi.org/10.1038/bmt.2016.78.
American College of Endocrinology and American Diabetes Association Consensus statement on inpatient diabetes and glycemic control. Diabetes Care. 2006;29(8):1955–62.
Drincic A, Pfeffer E, Luo J, Goldner WS. The effect of diabetes case management and diabetes resource nurse program on readmissions of patients with diabetes mellitus. J Clin Transl Endocrinol. 2017;8:29–34. https://doi.org/10.1016/j.jcte.2017.03.003.
Mathioudakis N, Pronovost PJ, Cosgrove SE, Hager D, Golden SH. Modeling inpatient glucose management programs on hospital infection control programs: an infrastructural model of excellence. Jt Comm J Qual Patient Saf. 2015;41(7):325–36. https://doi.org/10.1016/S1553-7250(15)41043-8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Andjela Drincic, Padmaja Akkireddy, and Jon Knezevich declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Health Care Delivery Systems and Implementation in Diabetes
Rights and permissions
About this article
Cite this article
Drincic, A.T., Akkireddy, P. & Knezevich, J.T. Common Models Used for Inpatient Diabetes Management. Curr Diab Rep 18, 10 (2018). https://doi.org/10.1007/s11892-018-0972-x
Published:
DOI: https://doi.org/10.1007/s11892-018-0972-x