Abstract
Purpose of Review
Cardiovascular disease (CVD) and breast cancer (BC) are significant causes of mortality globally, imposing a substantial health burden. This review article aims to examine the shared risk factors and social determinants that contribute to the high prevalence of both diseases, with a focus on social risk factors.
Recent Findings
The common risk factors for CVD and BC, such as hypertension, diabetes, obesity, aging, and physical inactivity, are discussed, emphasizing their modifiability. Adhering to ideal cardiovascular health behaviors has shown a trend toward lower BC incidence. Increased risk of CVD-related mortality is significantly impacted by age and race in BC patients, especially those over 45 years old. Additionally, racial disparities in both diseases highlight the need for targeted interventions. Social determinants of health, including socioeconomic status, education, employment, and neighborhood context, significantly impact outcomes for both CVD and BC.
Summary
Addressing social factors is vital in reducing the burden of both CVD and BC and improving overall health equity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiovascular disease (CVD) and cancer are two of the leading causes of mortality worldwide, accounting for over one million deaths in the USA alone in 2020 [1, 2]. Breast cancer (BC) continues to be the most common cancer in women, while CVD is the leading cause of death in women, accounting for about one in every five deaths [2]. The risk factors for CVD, including hypertension, diabetes, aging, metabolic syndrome, smoking, and physical inactivity, also contribute to the development of BC [3, 4]. Moreover, BC and its treatments are independent risk factors for CVD, contributing to CVD-related mortality in nearly 16% of women diagnosed with BC [3]. Additionally, CVD may be linked to cancer development [4,5,6,7]. This review article highlights the key social factors that play a role in the high prevalence of both CVD and BC. Specifically, we will discuss the impact of socioeconomic status, education, employment, environmental factors, diet, social isolation, physical inactivity, and smoking/alcohol use. It will also explore preventive strategies and future directions to improve both diseases, aiming to reduce the burden and improve health outcomes for at-risk individuals.
The Burden of CVD and BC
The burden of CVD and BC is a substantial health concern in the USA. In 2020, the prevalence of BC among women in the USA was 3,886,830 cases, with an increasing incidence by 0.5% per year, but declining mortality of 43% through 2020 [8, 9]. In 2021, more than 60 million women have been diagnosed with some form of CVD, and CVD claimed more lives than cancer and chronic lower respiratory disease combined [10]. The number of patients living with BC and CVD has substantially increased as mortality is declining in both diseases over the past 20 years. Survival for BC has increased dramatically, with almost 90% of patients surviving at least 5 years after initial diagnosis [8]. The annual economic burden of CVD and BC in the USA is estimated to be approximately $272.5 billion and $16.5 billion, respectively, and is expected to continue to rise [11,12,13].
BC survivors face an increased risk of CVD-related mortality compared to women without a history of BC, particularly around 7 years after diagnosis [12]. Therefore, early detection and management of CVD risk factors are essential in mitigating the burden of CVD during this timeframe.
Common Risk Factors
Growing epidemiological evidence supports the shared risk factors and mechanisms between BC and CVD, aligning with the common soil hypothesis (Fig. 1) [14]. Researchers have emphasized the identification of cardiac risk factors to mitigate the impact of CVD for over six decades. Likewise, BC shares numerous CVD risk factors, including hypertension, obesity, diabetes, and aging, most of which are modifiable [15]. Studies demonstrate that up to 80% of CVD morbidity can be prevented by modifying risk factors through better control of diabetes, dyslipidemia and hypertension, increasing physical activity, consuming a healthy balanced diet, and smoking cessation [16,17,18]. These risk factors exhibit comparable associations with BC risk, while others demonstrate intricate interactions [15].
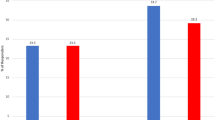
Adhering to ideal cardiovascular health behaviors from the American Heart Association’s Life’s Simple 7 has been linked to a trend towards a lower incidence of BC [16]. In a meta-analysis of 18 cohort studies, it was found that women with lower risk profiles have substantially reduced CVD events. Patients with 0, 1, or ≥2 risk factors have an incidence of CVD events of 4.1%, 20.2%, and 30.7%, respectively [15]. Studies have demonstrated that controlling these risk factors is associated with a reduction in lifetime cancer risk [17].
Raising awareness about controlling risk factors has led to increased attention towards preventing BC. Recent discussions have highlighted the importance of identifying and addressing these shared risk factors. Thus, developing effective prevention strategies that can address both BC and CVD requires a better understanding of the common soil hypothesis and the interconnected mechanisms linking both diseases.
Effect of Age and Race
Age
The risk of developing BC and CVD increases with age [18, 19]. The lifetime risk of developing BC for women is estimated to be one in eight. Additionally, more than 40% of BC patients are older than 65, and they account for nearly 60% of BC deaths [20]. A study observed that BC patients who did not receive chemotherapy or radiation therapy had a significantly higher standardized mortality ratio (SMR = 2.196, 95% CI: 2.148–2.245, P < 0.001) related to CVD compared to the general population [21]. Another study reported SMR for death from heart disease at 10+ years for patients who received radiotherapy and chemotherapy were 2.92 (95% CI 2.81–3.04, p < 0.001) and 5.05 (95% CI 4.57–5.55, p < 0.001), respectively [22].
Race
The incidence and mortality rates of CVD and BC are influenced by race and geographic location [23, 24]. Racial disparities exist in the risk of developing BC, with non-Hispanic white women having a higher incidence than other racial groups [23]. Conversely, mortality rates for BC are higher among black females [23]. Black women also have higher incidence and mortality rates for CVD, suggesting a complex relationship between race and disease manifestation [24, 25]. One study reported that the incidence of premenopausal triple negative breast cancer is higher among black females [26]. The etiology of these racial disparities is complex, with multiple social factors contributing to disease susceptibility, including socioeconomic status, lifestyle factors, and barriers to healthcare accessibility [20,21,22,23,24,25,26]. A comprehensive understanding of these factors can formulate tailored approaches to reduce the burden of both CVD and BC by race.
Social Risk Factors
Social Determinant of Health
Social determinants of health (SDOH), as defined by both the Center for Disease Control (CDC) and the World Health Organization (WHO), encompass a broad range of environmental conditions that impact an individual’s health, well-being, and overall quality of life. These determinants are influenced by various factors, including the places where people live, work, learn, play, worship, and age [27••, 28]. It is widely acknowledged that SDOH has a significant impact on disease outcomes, particularly with respect to CVD and BC [29•, 30].
Socioeconomic Status
Socioeconomic status (SES) encompasses factors including income, wealth, and education. Racial and ethnic health disparities in the USA are largely driven by financial hardship, housing insecurity, racism, and residential segregation [30]. Higher SES has been linked to a higher incidence of BC compared to women with low SES [31]. This higher incidence is related to differences in risk profiles in women with different SES. Women with high SES have fewer children, have their first child at an older age, and are less likely to breastfeed [31, 32]. Conversely, lower SES is associated with a higher CVD risk [33] and has been linked to worse outcomes in both diseases [33]. Studies reported that BC survival and mortality are associated with the level of education, district of residence, and social class in childhood [34]. BC mortality is significantly higher in blacks compared to non-Hispanic white [35]. Furthermore, a study reported that among adults aged 30 to 59, low SES is associated with a greater than two-fold increase in mortality from ischemic heart disease [36]. Additionally, literature reported that lower income among women was associated with a 10.1-year shorter life span between the poorest and richest individuals [37]. Studies also demonstrated that low SES conditions lead to poor health more frequently than poor health leads to low SES [38]. The difference can be attributed to multiple factors including access to care and higher risk profile [32, 39]. In high-income countries, higher CVD risk factors tend to cluster in low SES populations [40]. The combined effect of individual risk factors is multiplicative rather than additive; therefore, there is a markedly increased risk of CVD and premature disease among individuals of low SES [41]. Furthermore, people with low SES are less likely to receive guideline-recommended medical therapy and cardiac catheterization within 24 hour of acute coronary syndromes [39].
Education and Employment
Education is needed for health literacy and effective communication with healthcare providers and provides access to higher-paying jobs and stable employment. Literature has demonstrated that a lower educational level is associated with a higher risk of acute MI, CAD, stroke, and heart failure (HF) [42]. It is also associated with a lower incidence of BC [43], however a higher BC mortality rate [44]. Income provides for basic needs such as food, housing, and healthcare services. There is a correlation between income level and the ability to afford a healthier lifestyle and a better-resourced neighborhood, lowering risk of health complications [27••, 29•].
Unemployment is associated with a higher risk of CVD and BC. A French study reported a 20% increase in CAD events among unemployed people without pre-existing heart disease, after adjustment for age, sex, diet, and lifestyle, and nearly 46% of the CAD is explained by dietary and lifestyle factors [45]. A US study reported a 35% increase in acute MI among unemployed people [46]. Even those who are unemployed with high SES have a high risk of CAD events, despite adjustment for covariates such as age, sex, biological characteristics, behavioral variables, and socioeconomic factors. Moreover, the unemployed have worse outcomes in comparison to the retired population [47]. The detrimental effect of unemployment may be driven by the job loss itself or by poor health associated with being unemployed. Employment has a vital impact on health access as health insurance is obtained through employers, and flexibility in the work schedule and paid time off allows individuals to adhere to medical treatment plans [29•, 48]. Black women are more likely to develop BC at a younger age than non-Hispanic white women, increasing the reliance on employer-provided health insurance. However, insufficient sick leave often prevents them from receiving adequate treatment [29•, 49].
Recent research has highlighted the importance of health insurance in promoting health equity, particularly in the context of BC and CVD. Those who are uninsured/underinsured are less likely to have access to preventive medical care and screenings. This can lead to delays in diagnosis and treatment, lower rates of medication adherence and management of chronic illnesses [50]. In BC, advanced stages of the disease have been linked to uninsured black, Indigenous, and Latinx women compared to non-Hispanic whites [51]. Medicaid expansion has been associated with higher mammography screening rates and reduced incidence of advanced BC, with black women and those under 50 years of age achieving the greatest benefit. From 2012 to 2016, there was a significant decrease in the incidence rates of advanced BC in black women in expansion states compared to non-expansion states. In the expansion states, the rates decreased from 24.6 to 21.6%, while in the non-expansion states, the rates remained unchanged at 27.4% [52, 53••].
Neighborhood Context and Environmental Factors
Neighborhood context plays an important role in health inequities, including disparities in BC and CVD outcomes. Access to resources such as grocery stores, gyms, sports centers, safe places to recreate, and preventive healthcare are essential factors in promoting healthy behaviors [49, 54,55,56]. In the USA, the impact of the neighborhood is well documented in the literature; zip code can predict life expectancy, health status, and clinical outcomes [57]. Low-income neighborhoods face challenges in healthcare access due to inadequate resources and poor infrastructure. While physical barriers such as housing insecurity, transportation limitations, and travel costs have not been extensively studied [58], high poverty rates and inner-city disadvantages have been associated with worse BC outcomes [59]. Women with non-metastatic BC living in low SES neighborhoods are more likely to present with more aggressive advanced disease and subtypes and have higher disease-specific mortality compared to women in high SES areas [60]. High neighborhood income has been associated with a lower CVD risk. The literature has reported a 10% reduction in acute MI mortality for every $10,000 increase in neighborhood median income [61]. Additionally, neighborhood deprivation, including low income, education, occupation, and housing quality, has been linked to an increased risk of HF and poorer HF outcomes regardless of the SES [62].
Several studies have shown that more individuals in low SES neighborhoods exhibit unhealthy lifestyle behaviors. Specifically, residing in a low SES neighborhood is linked to increased accessibility to fast food establishments [63], reduced engagement in physical exercise, increased sedentary behavior [64], higher likelihood of obesity [65], and tobacco use [66]. These factors, in turn, contribute to various health problems, particularly CVD. Housing instability, including homelessness and difficulty paying rent, is a growing issue that contributes to CVD risk factors and higher CVD mortality rates [67].
In addition to these socioeconomic factors, policy and practice barriers further contribute to health inequities. These policies have led to ongoing racial segregation in the USA, which has significant impacts on health outcomes [49, 54]. Many black patients reside in neighborhoods that limit their ability to achieve optimal health. This can include barriers to obtaining BC and CVD screening and treatment, leading to poorer outcomes for these populations [49, 54]. A study revealed that black women born in Jim Crow states had poorer BC outcomes, including more aggressive forms of cancer, than non-Hispanic white women, regardless of their state of birth [56]. Similarly, the ongoing impact of slavery on heart disease mortality rates has been demonstrated, with black living in regions of the USA with a historical legacy of slavery having worse survival rates from CVD and fewer improvements in disease survival compared to regions that did not practice slavery [55].
Chronic exposure to social and environmental stressors is a major contributor to racial and ethnic inequities in both BC and CVD. Studies have reported that chronic stressors can have a negative impact on health through complex cascades that include the release of epinephrine and norepinephrine. These hormones can result in high blood pressure and poor immune system function, increasing the risk and poor outcomes in both diseases [68]. Epigenetics is a burgeoning field in medicine that focuses on how gene expression is affected by environmental and social factors [69]. Linnenbringer et al. linked this to BC mortality disparities by suggesting that “weathering” of the body’s stress response system may contribute to the expression of BC subtypes with less favorable outcomes [70].
Diet and Food Insecurity
Diet has been shown to impact the risk of chronic diseases such as CVD and BC. Healthy diets rich in whole grains, fruits, vegetables, and lean proteins have been associated with a lower risk of CVD [71], while unhealthy diets high in saturated fats, added sugars, and sodium have been linked to higher cardiovascular mortality [72]. The effect of diet on BC risk is still controversial, with some studies suggesting a protective effect of a healthy diet, particularly high in fruits and vegetables [73], while others show no significant association [74]. Ultra-processed foods, including sugar-sweetened beverages, have been linked to increased risks of both CVD and BC [75].
There is ongoing research evaluating the influence of dietary factors on BC risk, including the consumption of processed and unprocessed meats. Increased intake of meat has been associated with a higher risk of premenopausal BC, while processed meat intake has shown an association with postmenopausal BC [76]. However, the relationship between diet and BC risk is complex and influenced by various factors such as alcohol consumption and gut microbiota composition. Further investigation is necessary to better understand the impact of diet on BC risk, considering gene-environment interactions and long-term epigenetic mechanisms.
Studies have shown disparities in diet quality based on race, ethnicity, SES, education level, income, and use of food assistance programs in the USA [77,78,79]. Literature reported that from 1988 to 2010, the percentage of blacks with poor diet was higher than that of non-Hispanic whites by 6.8 to 11.7%, but no difference was observed in 2011 to 2014 due to declining diet quality among non-Hispanic whites [80,81,82,83]. Over time, there have been improvements in diet quality among higher-income individuals, while no significant changes were observed for blacks and Mexican Americans [78, 79]. Individuals participating in food assistance programs, such as Supplemental Nutrition Assistance Program (SNAP), generally exhibit suboptimal dietary patterns [81].
Food insecurity (FI) and food deserts are major health problems that contribute to poor dietary patterns and increased risk of CVD. FI refers to limited or uncertain access to adequate food, while food deserts are areas in low-income neighborhoods with limited access to grocery stores providing fresh fruits and vegetables [80]. These challenges make it difficult for individuals to adhere to recommended healthy diets for CVD prevention and management. People experiencing FI and living in food deserts are at greater risk of diet-related CVD, and it is important to recognize and address these issues in clinical settings, particularly among those with existing CVD conditions [81, 82].
Social Isolation and Loneliness
Social isolation and loneliness are chronic stressors that can have a negative impact on physical and mental health [84]. Changes in society’s structure and demographics have increased the risk of loneliness among individuals [85]. Factors such as increased life expectancy and a growing population of older adults have contributed to reduced social interactions, longer periods of living alone, and a higher prevalence of loneliness among older adults [86]. However, it is important to note that loneliness is not limited to older age but can be encountered at various stages of life [87].
Literature has shown that social networks and connections are important for people with BC and CVD [88]. Adequate social support can have a protective effect on physical and mental health and overall quality of life. Studies have shown that people who lack strong social support have a higher mortality rate, both all-cause mortality and BC mortality. These studies assess social support based on the number of individuals within the social network and the frequency of contact with friends and family following cancer diagnosis [89]. A study that included 2835 participants from the Nurses’ Health Study found that socially isolated participants were twice as likely to die compared to socially connected individuals [89]. Additionally, individuals with robust social support were more likely to adhere to treatment regimens, access healthcare, and effectively utilize treatment options [90].
In a study conducted in 1992, patients with CAD who were unmarried and lacked a confidant experienced a significantly higher 5-year mortality incidence rate compared to those who had a spouse/partner [91]. A recent systematic review and meta-analysis of 16 prospective longitudinal studies revealed a correlation between loneliness and social isolation with an increased risk of CAD (29%) and stroke (32%) [92]. Another cohort study involving 57,825 older women in the USA found that social isolation and loneliness were associated with an 8.0% and 5.0% higher risk of incident CVD, respectively, even after adjusting for health behaviors and outcomes. Women experiencing greater social isolation and loneliness faced a 13 to 27% higher risk of developing CVD compared to those with lower levels of social isolation and loneliness [93].
Tobacco Use
Tobacco use is a well-established risk factor for CVD [94]. However, its association with BC remains controversial, with conflicting findings reported in the literature. A recent meta-analysis analyzing over 400,000 BC cases found evidence to support a positive dose-response relationship between smoking intensity and BC risk. This may suggest a causal relationship between smoking and BC development [95]. However, other studies have only found weak associations [96]. Additionally, several studies have suggested that the age of smoking initiation is a significant factor in BC risk, with earlier onset associated with a higher risk of developing BC [97]. Furthermore, a meta-analysis of nearly 2.4 million smokers and non-smokers reported that female smokers had a 25% higher risk of developing coronary heart disease than male smokers, with a 95% confidence interval of 1.12 to 1.39 [98].
The effect of passive smoking on BC risk is controversial, with some studies suggesting an increased risk [99] and others finding no significant association [100]. Additionally, some literature suggests that the effect of tobacco use on BC risk is modified by genetic variants in enzymes involved in carcinogen metabolism, particularly NAT2. Patients with slow acetylator variant NAT2 genotypes have a higher risk of developing BC, especially in women with a higher pack year [101].
Alcohol Use
Alcohol consumption is another well-established risk factor for the development of BC in the scientific literature [102]. Meta-analyses and systematic reviews of epidemiological studies have consistently reported a dose-response relationship between alcohol intake and BC risk. This relationship is most pronounced in patients with estrogen receptor-positive (ER+) BC [3]. In a recent meta-analysis of 22 cohort studies and 45,350 BC cases, the risk of BC increased by 10.5% for every additional 10 g of alcohol consumed per day. This risk was even higher among postmenopausal women, with an increased risk of 11.1% [103]. A review article estimated that in 2012, globally, 144,000 (95% confidence interval [CI]: 88,000 to 200,000) BC cases and 38,000 (95% CI: 2,400 to 53,000) BC deaths were attributable to alcohol consumption, with 18.8% of these cases and 17.5% of these deaths affecting women who were light alcohol consumers [104].
The effect of alcohol consumption on cardiovascular risk is controversial. Observational studies and meta-analyses of observational studies have suggested that light to moderate alcohol intake has a cardioprotective effect on ischemic heart disease [105]. However, heavy alcohol consumption has a deleterious effect on the heart and increased mortality from CVD [105]. Nevertheless, the effect of alcohol consumption on other types of CVD and all-cause mortality remains ambiguous. Recently, Mendelian randomization studies using genetic polymorphisms in enzymes have questioned the beneficial association of low-moderate drinking with the cardiovascular system [106]. As there are considerable variations in the literature, it is difficult to determine a protective effect of moderate alcohol consumption by itself.
Sedentary Lifestyle and Physical Activity
Sedentary Lifestyle
Sedentary behavior has been associated with increased risk of CVD and BC [107]. A large observational study involving 71,018 women reported that prolonged sitting more than 10 hours per day was associated with increased CVD risk, even after adjusting for physical activity [108]. Sedentary behavior has also been linked to high breast density, a strong independent risk factor for BC [109]. One case-control study found that sedentary behavior was associated with BC risk, independent of moderate to vigorous activity. Racial differences were observed in the association between sedentary behavior and BC risk, with white women at higher risk than black women [110]. Therefore, reducing sedentary behavior and increasing physical activity are potential targets for CVD and BC prevention intervention.
Physical Activity
Physical activity has been shown to have benefits for cardiovascular health, including a reduction in the risk of all-cause and cardiovascular mortality, as well as a lower risk of total CVD, coronary heart disease, hypertension, and type 2 diabetes [111]. Only 17.6% of American women meet the recommended guidelines of 150 minutes of moderate-intensity physical activity per week [112]. A growing body of evidence also supports the protective effect of physical activity against BC development among both premenopausal and postmenopausal women, with a linear dose-response relationship observed [113]. A meta-analysis of 29 observational studies found a significant reduction in BC risk among the most physically active women compared to the least active [114]. Furthermore, a more recent meta-analysis of 22 studies involving 123,574 participants found an inverse relationship between physical activity and BC events and deaths. Women who engage in high levels of lifetime recreational physical activity have a significantly lower risk of BC-related death compared to those who report low or no recreational physical activity, and physical activity during adolescence may also lower the risk of premenopausal BC [115]. Epidemiological studies have primarily focused on the benefits of aerobic activities, and more research is needed to explore the role of muscle-strengthening activities in cancer prevention [116]. The underlying biological mechanisms that explain the protective effect of physical activity against BC remain unclear, although studies suggest potential hormonal and non-hormonal pathways. Hormonal pathways may involve reduced levels of estrogen in postmenopausal women, while non-hormonal pathways may involve immune function, inflammation, oxidative stress, myokines, insulin, insulin-like growth factors, and adipokines [117].
Future Directions
There is an increasing recognition of social risk factors’ significance in CVD and BC outcomes, leading to the development of targeted interventions to address health disparities. However, more work remains to be done. Improving access to healthcare and addressing social determinants of health are key areas that require attention. This involves enhancing affordable and comprehensive healthcare access, promoting healthy behaviors through environmental improvements, and addressing social and economic inequalities contributing to health disparities. Interventions such as the SNAP can mitigate food insecurity, while collaboration among healthcare providers, policymakers, community partners, and patients is crucial for developing comprehensive intervention strategies. By improving education and healthcare access as well as addressing housing, food, and transportation issues, policy makers can help reduce inequality. Addressing other issues including racial segregation, institutional racism, and social isolation are all important components of this comprehensive approach (Table 1).
Furthermore, increasing awareness and education on social risk factors for CVD and BC among healthcare providers and patients is crucial, along with the development of culturally sensitive interventions. Public awareness and education efforts can help reduce stigma and improve health behaviors. Additionally, further research is needed to understand the mechanisms through which social risk factors influence disease. This entails identifying biomarkers and molecular pathways affected by social factors and creating targeted interventions. Identifying vulnerable subgroups, such as those with specific genetic and physiological profiles, is also essential in advancing understanding and intervention strategies related to social risk factors. By implementing these mitigation strategies, it is possible to improve health outcomes and reduce disparities associated with CVD and BC.
Conclusion
CVD and BC are multifaceted conditions influenced by various clinical, social, and environmental factors. Despite the significance of genetic and physiological components in the development and progression of these diseases, social determinants of health such as socioeconomic status, education level, race/ethnicity, environmental exposures, and psychosocial factors also have a substantial impact on disease risk and outcomes. To mitigate health disparities and devise effective interventions, it is crucial to comprehend the social risk factors involved in the etiology of CVD and BC and their underlying mechanisms. Addressing social risk factors can lead to a future where all individuals receive equitable prevention and treatment for these diseases, irrespective of their social or economic status.
Abbreviations
- CVD:
-
Cardiovascular disease
- BC:
-
Breast cancer
- SMR:
-
Standardized mortality ratio
- SES:
-
Socioeconomic status
- MI:
-
Myocardial infarction
- CAD:
-
Coronary artery disease
- HF:
-
Heart failure
- SNAP:
-
Supplemental Nutrition Assistance Program
- AA:
-
African American
- WHO:
-
World Health Organization
- CDC:
-
Centers for Disease Control and Prevention
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Heron M. Deaths: leading causes for 2017. Natl Vital Stat Rep. 2019;68(6):1–77.
Giaquinto AN, Sung H, Miller KD, Kramer JL, Newman LA, Minihan A, et al. Breast cancer statistics, 2022. CA Cancer J Clin. 2022;72(6):524–41.
Patnaik JL, Byers T, DiGuiseppi C, Dabelea D, Denberg TD. Cardiovascular disease competes with breast cancer as the leading cause of death for older females diagnosed with breast cancer: a retrospective cohort study. Breast Cancer Res. 2011;13(3):R64.
Guha A, Fradley MG, Dent SF, Weintraub NL, Lustberg MB, Alonso A, et al. Incidence, risk factors, and mortality of atrial fibrillation in breast cancer: a SEER-Medicare analysis. Eur Heart J. 2022;43(4):300–12.
Koelwyn GJ, Newman AAC, Afonso MS, van Solingen C, Corr EM, Brown EJ, et al. Myocardial infarction accelerates breast cancer via innate immune reprogramming. Nat Med. 2020;26(9):1452–8.
Meijers WC, Maglione M, Bakker SJL, Oberhuber R, Kieneker LM, de Jong S, et al. Heart failure stimulates tumor growth by circulating factors. Circulation. 2018;138(7):678–91.
Koene RJ, Prizment AE, Blaes A, Konety SH. Shared risk factors in cardiovascular disease and canceR. Circulation. 2016;133(11):1104–14.
SEER*Explorer: An interactive website for SEER cancer statistics [Internet]. Surveillance Research Program, National Cancer Institute. 2023. [Updated: 2023 Jun 8; cited 2023 Jul 24]. Available from: https://seer.cancer.gov/statistics-network/explorer/. Data source(s): U.S. Mortality Data (1969–2020), National Center for Health Statistics, CDC.
Giaquinto AN, et al. Breast cancer statistics, 2022. CA Cancer J Clin. 2022;72(6):524–41. https://doi.org/10.3322/caac.21754.
Keteepe-Arachi T, Sharma S. cardiovascular disease in women: understanding symptoms and risk factors. European Cardiology Review. 2017;12(1):10.
Tsao CW, et al. Heart disease and stroke statistics-2023 update: a report from the American Heart Association. Circulation. 2023;147(8):e93–621. https://doi.org/10.1161/CIR.0000000000001123.
Heidenreich PA, Trogdon JG, Khavjou OA, Butler J, Dracup K, Ezekowitz MD, et al. Forecasting the future of cardiovascular Disease in the United States. Circulation. 2011;123(8):933–44.
Ramin C, Schaeffer ML, Zheng Z, Connor AE, Hoffman-Bolton J, Lau B, et al. All-cause and cardiovascular disease mortality among breast cancer survivors in CLUE II, a long-standing community-based cohort. J Natl Cancer Inst. 2021;113(2):137–45.
Iacoviello L, Bonaccio M, de Gaetano G, Donati MB. Epidemiology of breast cancer, a paradigm of the “common soil” hypothesis. Semin Cancer Biol. 2021;72:4–10.
Berry JD, Dyer A, Cai X, Garside DB, Ning H, Thomas A, et al. Lifetime risks of cardiovascular disease. N Engl J Med. 2012;366(4):321–9.
Rasmussen-Torvik LJ, Shay CM, Abramson JG, Friedrich CA, Nettleton JA, Prizment AE, et al. Ideal cardiovascular health is inversely associated with incident cancer. Circulation. 2013;127(12):1270–5.
Kushi LH, Doyle C, McCullough M, Rock CL, Demark-Wahnefried W, Bandera EV, et al. American Cancer Society guidelines on nutrition and physical activity for cancer prevention. CA Cancer J Clin. 2012;62(1):30–67.
Garcia M, Mulvagh SL, Bairey Merz CN, Buring JE, Manson JE. Cardiovascular disease in women. Circ Res. 2016;118(8):1273–93.
McGuire A, Brown J, Malone C, McLaughlin R, Kerin M. Effects of age on the detection and management of breast cancer. Cancers (Basel). 2015;7(2):908–29.
United Kingdom Office for National Statistics. Cancer survival in England: patients diagnosed 2007–2011 and followed up to 2012. United Kingdom Office for National Statistics; Newport, UK: 2013.
Guan T, Zhang H, Yang J, Lin W, Wang K, Su M, et al. Increased risk of cardiovascular death in breast cancer patients without chemotherapy or (and) radiotherapy: a large population-based study. Front Oncol. 2021;10.
Agha A, Wang X, Wang M, et al. Long-term risk of death from heart disease among breast cancer patients. Front Cardiovasc Med. 2022;9:784409. Published 2022 Apr 13. https://doi.org/10.3389/fcvm.2022.784409.
Hirko KA, Rocque G, Reasor E, Taye A, Daly A, Cutress RI, et al. The impact of race and ethnicity in breast cancer—disparities and implications for precision oncology. BMC Med. 2022;20(1):72.
Graham G. Disparities in cardiovascular disease risk in the United States. Curr Cardiol Rev. 2015;11(3):238–45.
Andrews JO, Graham-Garcia J, Raines TL. Heart disease mortality in women: racial, ethnic, and geographic disparities. J Cardiovasc Nurs. 2001;15(3):83–7.
Carey LA, Perou CM, Livasy CA, Dressler LG, Cowan D, Conway K, et al. Race, breast cancer subtypes, and survival in the Carolina Breast Cancer Study. JAMA. 2006;295(21):2492.
•• Powell-Wiley TM, Baumer Y, Baah FO, Baez AS, Farmer N, Mahlobo CT, et al. Social determinants of cardiovascular disease. Circ Res. 2022;130(5):782–99. The article underscores the significance of social determinants of health (SDoH) in relation to cardiovascular disease (CVD) by identifying key factors spanning structural, socioeconomic, environmental, and psychosocial aspects. It delves into the biological mechanisms connecting SDoH with CVD, including stress hormones, inflammation, immune cell function, and cellular aging, while referencing pivotal and recent studies. The article also outlines a roadmap for forthcoming research on SDoH, emphasizing individual, clinical, and policy strategies to advance community-engaged interventions for enhancing cardiovascular health.
Hahn RA. What is a social determinant of health? Back to basics. J Public Health Res. 2021;10(4):jphr.2021.2324.
• Gehlert S, Hudson D, Sacks T. A critical theoretical approach to cancer disparities: breast cancer and the social determinants of health. Front Public Health. 2021;9. This article shifts the discussion of breast cancer disparities from individual-level factors to a Critical Race Theory perspective, highlighting historical and systemic influences on unequal outcomes for Black women. By examining social determinants and discriminatory policies, the study aims to address breast cancer disparities through inclusive healthcare training and equitable public policies to counteract the disproportionate mortality experienced by Black and lower socioeconomic status women.
Braveman P, Egerter S, Williams DR. The social determinants of health: coming of age. Annu Rev Public Health. 2011;32(1):381–98.
Palmer JR, Boggs DA, Wise LA, Adams-Campbell LL, Rosenberg L. Individual and neighborhood socioeconomic status in relation to breast cancer incidence in African-American women. Am J Epidemiol. 2012;176(12):1141–6.
Katuwal S, Tapanainen J, Pukkala E. Multivariate analysis of independent roles of socioeconomic status, occupational physical activity, reproductive factors, and postmenopausal hormonal therapy in risk of breast cancer. Breast Cancer Res Treat. 2022;193(2):495–505.
Clark AM, DesMeules M, Luo W, Duncan AS, Wielgosz A. Socioeconomic status and cardiovascular disease: risks and implications for care. Nat Rev Cardiol. 2009;6(11):712–22.
Davoudi Monfared E, Mohseny M, Amanpour F, Mosavi Jarrahi A, Moradi Joo M, Heidarnia MA. Relationship of social determinants of health with the three-year survival rate of breast cancer. Asian Pac J Cancer Prev. 2017;18(4):1121–6.
Yedjou CG, Sims JN, Miele L, Noubissi F, Lowe L, Fonseca DD, et al. Health and racial disparity in breast cancer. 2019. p. 31–49.
Avendano M. Socioeconomic status and ischaemic heart disease mortality in 10 western European populations during the 1990s. Heart. 2005;92(4):461–7.
Chetty R, Stepner M, Abraham S, Lin S, Scuderi B, Turner N, et al. The Association between income and life expectancy in the United States, 2001–2014. JAMA. 2016;315(16):1750.
Shishehbor MH. Association of socioeconomic status with functional capacity, heart rate recovery, and all-cause mortality. JAMA. 2006;295(7):784.
Yong CM, Abnousi F, Asch SM, Heidenreich PA. Socioeconomic inequalities in quality of care and outcomes among patients with acute coronary syndrome in the modern era of drug eluting stents. J Am Heart Assoc. 2014;3(6).
Warburton DER. Health benefits of physical activity: the evidence. Can Med Assoc J. 2006;174(6):801–9.
Castelli WP. Epidemiology of coronary heart disease: the Framingham study. Am J Med. 1984;76(2):4–12.
Liu K, Cedres LB, Stamler J, Dyer A, Stamler R, Nanas S, et al. Relationship of education to major risk factors and death from coronary heart disease, cardiovascular diseases and all causes, Findings of three Chicago epidemiologic studies. Circulation. 1982;66(6):1308–14.
Dong JY, Qin LQ. Education level and breast cancer incidence: a meta-analysis of cohort studies. Menopause. 2020;27(1):113–8.
Bahk J, Jang SM, Jung-Choi K. Increased breast cancer mortality only in the lower education group: age-period-cohort effect in breast cancer mortality by educational level in South Korea, 1983–2012. Int J Equity Health. 2017;16(1):56.
Méjean C, Droomers M, van der Schouw YT, Sluijs I, Czernichow S, Grobbee DE, et al. The contribution of diet and lifestyle to socioeconomic inequalities in cardiovascular morbidity and mortality. Int J Cardiol. 2013;168(6):5190–5.
Dupre ME, George LK, Liu G, Peterson ED. The cumulative effect of unemployment on risks for acute myocardial infarction. Arch Intern Med. 2012;172(22):1731.
Meneton P, Kesse-Guyot E, Méjean C, Fezeu L, Galan P, Hercberg S, et al. Unemployment is associated with high cardiovascular event rate and increased all-cause mortality in middle-aged socially privileged individuals. Int Arch Occup Environ Health. 2015;88(6):707–16.
Keisler-Starkey K, Bunch LN. Health insurance coverage in the United States: 2019. (2020). Available online at: https://www.census.gov/library/publications/2020/demo/p60-271.html. Accessed Apr 2023.
Brawley OW, Goldberg P. How we do harm: a doctor breaks ranks about being sick in America. New York, NY: St. Martin’s Press; 2012.
Farrell CM, Gottlieb A. The effect of health insurance on health care utilization in the justice-involved population: United States, 2014–2016. Am J Public Health. 2020;110(S1):S78-84.
Ko NY, Hong S, Winn RA, Calip GS. Association of insurance status and racial disparities with the detection of early-stage breast cancer. JAMA Oncol. 2020;6(3):385.
Toyoda Y, Jeong OHE, Premaratne ID, Chiuzan C, Rohde CH. Affordable Care Act state-specific medicaid expansion: impact on health insurance coverage and breast cancer screening rate. J Am Coll Surg. 2020;230(5):775–83.
•• Le Blanc JM, Heller DR, Friedrich A, Lannin DR, Park TS. Association of Medicaid expansion under the affordable care act with breast cancer stage at diagnosis. JAMA Surg. 2020;155(8):752. This cohort study examines the impact of Medicaid expansion on breast cancer stage at diagnosis and associated disparities in insurance status, age, and race/ethnicity. The study shows that Medicaid expansion was linked to decreased numbers of uninsured patients and reduced incidence of advanced-stage breast cancer. Particularly, African American patients and those under 50 years of age experienced significant benefits, suggesting that expanding access to healthcare resources could lead to changes in the distribution of breast cancer stage at diagnosis.
Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep. 2001;116(5):404–16.
Sistrunk C, Tolbert N, Sanchez-Pino MD, Erhunmwunsee L, Wright N, Jones V, et al. Impact of federal, state, and local housing policies on disparities in cardiovascular disease in Black/African American men and women: from policy to pathways to biology. Front Cardiovasc Med. 2022;9.
Ford CL. Public health critical race praxis: an introduction, an intervention, and three points for consideration. Wisconsin Law Rev. 2016;3:477–91.
Arcaya MC, Tucker-Seeley RD, Kim R, Schnake-Mahl A, So M, Subramanian SV. Research on neighborhood effects on health in the United States: a systematic review of study characteristics. Soc Sci Med. 2016;168:16–29.
Henry KA, Boscoe FP, Johnson CJ, Goldberg DW, Sherman R, Cockburn M. Breast cancer stage at diagnosis: is travel time important? J Community Health. 2011;36(6):933–42.
DeGuzman PB, Cohn WF, Camacho F, Edwards BL, Sturz VN, Schroen AT. Impact of urban neighborhood disadvantage on late stage breast cancer diagnosis in Virginia. J Urban Health. 2017;94(2):199–210.
Abdel-Rahman O. Impact of NCI socioeconomic index on the outcomes of nonmetastatic breast cancer patients: analysis of SEER census tract–level socioeconomic database. Clin Breast Cancer. 2019;19(6):e717–22.
Gerber Y, Weston SA, Killian JM, Therneau TM, Jacobsen SJ, Roger VL. Neighborhood income and individual education: effect on survival after myocardial infarction. Mayo Clin Proc. 2008;83(6):663–9.
Akwo EA, Kabagambe EK, Harrell FE, Blot WJ, Bachmann JM, Wang TJ, et al. Neighborhood deprivation predicts heart failure risk in a low-income population of blacks and whites in the southeastern United States. Circ Cardiovasc Qual Outcomes. 2018;11(1).
Hilmers A, Hilmers DC, Dave J. Neighborhood disparities in access to healthy foods and their effects on environmental justice. Am J Public Health. 2012;102(9):1644–54.
Xiao Q, Keadle SK, Berrigan D, Matthews CE. A prospective investigation of neighborhood socioeconomic deprivation and physical activity and sedentary behavior in older adults. Prev Med (Baltim). 2018;111:14–20.
Mohammed SH, Habtewold TD, Birhanu MM, Sissay TA, Tegegne BS, Abuzerr S, et al. Neighbourhood socioeconomic status and overweight/obesity: a systematic review and meta-analysis of epidemiological studies. BMJ Open. 2019;9(11): e028238.
Hitchman SC, Fong GT, Zanna MP, Thrasher JF, Chung-Hall J, Siahpush M. Socioeconomic status and smokers’ number of smoking friends: findings from the International Tobacco Control (ITC) Four Country Survey. Drug Alcohol Depend. 2014;143:158–66.
Charkhchi P, Fazeli Dehkordy S, Carlos RC. Housing and food insecurity, care access, and health status among the chronically ill: an analysis of the behavioral risk factor surveillance system. J Gen Intern Med. 2018;33(5):644–50.
Akinyemiju TF, Demb J, Izano MA, Rehkopf DH, Fang ML, Hiatt RA, et al. The association of early life socioeconomic position on breast cancer incidence and mortality: a systematic review. Int J Public Health. 2018;63(7):787–97.
Al Aboud NM, Tupper C, Jialal I. Genetics, Epigenetic Mechanism. 2023.
Linnenbringer E, Gehlert S, Geronimus AT. Black-white disparities in breast cancer subtype: the intersection of socially patterned stress and genetic expression. AIMS Public Health. 2017;4(5):526–56.
Heidemann C, Schulze MB, Franco OH, van Dam RM, Mantzoros CS, Hu FB. Dietary patterns and risk of mortality from cardiovascular disease, cancer, and all causes in a prospective cohort of women. Circulation. 2008;118(3):230–7.
Satija A, Bhupathiraju SN, Spiegelman D, Chiuve SE, Manson JE, Willett W, et al. Healthful and unhealthful plant-based diets and the risk of coronary heart disease in U.S. adults. J Am Coll Cardiol. 2017;70(4):411–22.
Velie EM, Schairer C, Flood A, He JP, Khattree R, Schatzkin A. Empirically derived dietary patterns and risk of postmenopausal breast cancer in a large prospective cohort study. Am J Clin Nutr. 2005;82(6):1308–19.
Adebamowo CA, Hu FB, Cho E, Spiegelman D, Holmes MD, Willett WC. Dietary patterns and the risk of breast cancer. Ann Epidemiol. 2005;15(10):789–95.
Srour B, Fezeu LK, Kesse-Guyot E, Allès B, Méjean C, Andrianasolo RM, et al. Ultra-processed food intake and risk of cardiovascular disease: prospective cohort study (NutriNet-Santé). BMJ. 2019;l1451.
Castelló A, Pollán M, Buijsse B, Ruiz A, Casas AM, Baena-Cañada JM, et al. Spanish Mediterranean diet and other dietary patterns and breast cancer risk: case–control EpiGEICAM study. Br J Cancer. 2014;111(7):1454–62.
Taylor EF, Burley VJ, Greenwood DC, Cade JE. Meat consumption and risk of breast cancer in the UK Women’s Cohort Study. Br J Cancer. 2007;96(7):1139–46.
Wang DD, Leung CW, Li Y, Ding EL, Chiuve SE, Hu FB, et al. Trends in dietary quality among adults in the United States, 1999 through 2010. JAMA Intern Med. 2014;174(10):1587.
Rehm CD, Peñalvo JL, Afshin A, Mozaffarian D. Dietary intake among US adults, 1999–2012. JAMA. 2016;315(23):2542.
Brown AF, Liang LJ, Vassar SD, Escarce JJ, Merkin SS, Cheng E, et al. Trends in racial/ethnic and nativity disparities in cardiovascular health among adults without prevalent cardiovascular disease in the United States, 1988 to 2014. Ann Intern Med. 2018;168(8):541.
Nguyen BT, Shuval K, Njike VY, Katz DL. The Supplemental Nutrition Assistance Program and Dietary Quality among US adults: findings from a nationally representative survey. Mayo Clin Proc. 2014;89(9):1211–9.
Kolak M, Bradley M, Block DR, Pool L, Garg G, Toman CK, et al. Urban foodscape trends: disparities in healthy food access in Chicago, 2007–2014. Health Place. 2018;52:231–9.
Mokdad AH, Ballestros K, Echko M, Glenn S, Olsen HE, Mullany E, et al. The state of US health, 1990–2016. JAMA. 2018;319(14):1444.
McPherson M, Smith-Lovin L, Brashears ME. Social isolation in America: changes in core discussion networks over two decades. Am Sociol Rev. 2006;71(3):353–75.
Masi CM, Chen HY, Hawkley LC, Cacioppo JT. A meta-analysis of interventions to reduce loneliness. Pers Soc Psychol Rev. 2011;15(3):219–66.
Hansen T, Slagsvold B. Late-Life Loneliness in 11 European Countries: Results from the Generations and Gender Survey. Soc Indic Res. 2016;129(1):445–64.
Beutel ME, Klein EM, Brähler E, Reiner I, Jünger C, Michal M, et al. Loneliness in the general population: prevalence, determinants and relations to mental health. BMC Psychiatry. 2017;17(1):97.
Coughlin SS. Social determinants of breast cancer risk, stage, and survival. Breast Cancer Res Treat. 2019;177(3):537–48.
Kroenke CH, Kubzansky LD, Schernhammer ES, Holmes MD, Kawachi I. Social networks, social support, and survival after breast cancer diagnosis. J Clin Oncol. 2006;24(7):1105–11.
Gage-Bouchard EA. Social support, flexible resources, and health care navigation. Soc Sci Med. 2017;190:111–8.
Williams RB, Barefoot JC, Califf RM, Haney TL, Saunders WB, Pryor DB, et al. Prognostic importance of social and economic resources among medically treated patients with angiographically documented coronary artery disease. JAMA. 267(4):520–4.
Valtorta NK, Kanaan M, Gilbody S, Ronzi S, Hanratty B. Loneliness and social isolation as risk factors for coronary heart disease and stroke: systematic review and meta-analysis of longitudinal observational studies. Heart. 2016;102(13):1009–16.
Golaszewski NM, LaCroix AZ, Godino JG, Allison MA, Manson JE, King JJ, et al. Evaluation of social isolation, loneliness, and cardiovascular disease among older women in the US. JAMA Netw Open. 2022;5(2): e2146461.
Lakier JB. Smoking and cardiovascular disease. Am J Med. 1992;93(1):S8-12.
Scala M, Bosetti C, Bagnardi V, Possenti I, Specchia C, Gallus S, et al. Dose-response relationships between cigarette smoking and breast cancer risk: a systematic review and meta-analysis. J Epidemiol. 2023;JE20220206.
US Department of Health and Human Services. The health consequences of smoking: 50 years of progress: a report of the Surgeon General. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014.
Xue F, Willett WC, Rosner BA, Hankinson SE, Michels KB. Cigarette smoking and the incidence of breast cancer. Arch Intern Med. 2011;171(2).
Johnson KC, Miller AB, Collishaw NE, Palmer JR, Hammond SK, Salmon AG, et al. Active smoking and secondhand smoke increase breast cancer risk: the report of the Canadian Expert Panel on Tobacco Smoke and Breast Cancer Risk (2009). Tob Control. 2011;20(1):e2–e2.
Huxley RR, Woodward M. Cigarette smoking as a risk factor for coronary heart disease in women compared with men: a systematic review and meta-analysis of prospective cohort studies. Lancet. 2011;378(9799):1297–305.
Johnson KC. Accumulating evidence on passive and active smoking and breast cancer risk. Int J Cancer. 2005;117(4):619–28.
Yang Y, Zhang F, Skrip L, Wang Y, Liu S. Lack of an association between passive smoking and incidence of female breast cancer in non-smokers: evidence from 10 prospective cohort studies. PLoS ONE. 2013;8(10): e77029.
Liu Y, Nguyen N, Colditz GA. Links between alcohol consumption and breast cancer: a look at the evidence. Women’s Health. 2015;11(1):65–77.
Sun Q, Xie W, Wang Y, Chong F, Song M, Li T, et al. Alcohol consumption by beverage type and risk of breast cancer: a dose-response meta-analysis of prospective cohort studies. Alcohol Alcohol. 2020;55(3):246–53.
Shield KD, Soerjomataram I, Rehm J. Alcohol use and breast cancer: a critical review. Alcohol Clin Exp Res. 2016;40(6):1166–81.
Goel S, Sharma A, Garg A. Effect of alcohol consumption on cardiovascular health. Curr Cardiol Rep. 2018;20(4):19.
Tolstrup JS, Gronbaek M, Nordestgaard BG. Alcohol intake, myocardial infarction, biochemical risk factors, and alcohol dehydrogenase genotypes. Circ Cardiovasc Genet. 2009;2(5):507–14.
Katzmarzyk PT, Church TS, Craig CL, Bouchard C. Sitting time and mortality from all causes, cardiovascular disease, and cancer. Med Sci Sports Exerc. 2009;41(5):998–1005.
Chomistek AK, Manson JE, Stefanick ML, Lu B, Sands-Lincoln M, Going SB, et al. Relationship of sedentary behavior and physical activity to incident cardiovascular disease. J Am Coll Cardiol. 2013;61(23):2346–54.
Tamimi RM, Byrne C, Colditz GA, Hankinson SE. Endogenous hormone levels, mammographic density, and subsequent risk of breast cancer in postmenopausal women. J Natl Cancer Inst. 2007;99(15):1178–87.
Dallal CM, Brinton LA, Matthews CE, Lissowska J, Peplonska B, Hartman TJ, et al. Accelerometer-based measures of active and sedentary behavior in relation to breast cancer risk. Breast Cancer Res Treat. 2012;134(3):1279–90.
Bull FC, Al-Ansari SS, Biddle S, Borodulin K, Buman MP, Cardon G, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54(24):1451–62.
Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics—2016 update. Circulation. 2016;133(4).
Moore SC, Lee IM, Weiderpass E, Campbell PT, Sampson JN, Kitahara CM, et al. Association of leisure-time physical activity with risk of 26 types of cancer in 1.44 million adults. JAMA Intern Med. 2016;176(6):816.
Lynch BM, Neilson HK, Friedenreich CM. Physical activity and breast cancer prevention. 2010. p. 13–42.
Lahart IM, Metsios GS, Nevill AM, Carmichael AR. Physical activity, risk of death and recurrence in breast cancer survivors: a systematic review and meta-analysis of epidemiological studies. Acta Oncol (Madr). 2015;54(5):635–54.
Clinton SK, Giovannucci EL, Hursting SD. The world cancer research fund/American institute for cancer research third expert report on diet, nutrition, physical activity, and cancer: impact and future directions. J Nutr. 2020;150(4):663–71.
Rock CL, Thomson C, Gansler T, Gapstur SM, McCullough ML, Patel AV, et al. American Cancer Society guideline for diet and physical activity for cancer prevention. CA Cancer J Clin. 2020;70(4):245–71.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Disclaimer
This research was supported (in whole or in part) by HCA Healthcare and/or an HCA Healthcare affiliated entity. The views expressed in this publication represent those of the author(s) and do not necessarily represent the official views of HCA Healthcare or any of its affiliated entities.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Obeidat, O., Charles, K.R., Akhter, N. et al. Social Risk Factors That Increase Cardiovascular and Breast Cancer Risk. Curr Cardiol Rep 25, 1269–1280 (2023). https://doi.org/10.1007/s11886-023-01957-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11886-023-01957-9