Abstract
Purpose of Review
Heart failure is a serious global health problem, and coronary artery disease is one of the main causes. At present, the treatment options for ischemic heart failure (IHF) are limited. This article mainly aims to explore the evidence of enhanced external counterpulsation (EECP) as a non-invasive cardiac rehabilitation method in patients with IHF and to make a preliminary exploration of its mechanisms.
Recent Findings
According to the existing evidence, the standard course of EECP is safe in patients with IHF and can significantly improve the quality of life of these patients. The effect of EECP on systolic function is still unclear, while EECP has a significant improvement effect on cardiac diastolic function. At the same time, this treatment can reduce the re-hospitalization rate and emergency visit rate of patients within 6 months. In terms of mechanisms, in addition to the immediate hemodynamic effect, existing evidence mostly suggests that its improvement of cardiac function may come from its upregulation of shear stress to improve myocardial perfusion.
Summary
EECP is safe to use in patients with stable ischemic heart failure, and it can improve the performance status of patients and may be beneficial to cardiac function and reduce the short-term re-hospitalization rate.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
With the progress of population aging, heart failure has gradually become an important health problem in today’s world, causing huge social and economic burden. In recent years, although the incidence of heart failure has decreased compared with before under active prevention and control, the mortality rate is still on the rise [1]. The 2020 China Heart Failure Medical Quality Control Report pointed out that coronary heart disease (CHD) is one of the main causes of heart failure in China, accounting for 48.3% [2]. Therefore, the diagnosis and treatment of ischemic heart failure (IHF) is urgent. The enhanced external counterpulsation (EECP) is a safe and effective cardiac rehabilitation treatment. Its unique dual-pulsed blood flow effect can increase immediate coronary perfusion, reduce cardiac afterload, and relieve myocardial ischemia [3]. It has now been recommended for use in patients with refractory angina [4, 5]. Regarding the role of EECP in patients with IHF, previous researchers have focused more on the improvement of ischemic symptoms in such patients. It was found that EECP can also significantly improve ischemic symptoms in IHF patients [6,7,8]. Therefore, in 2002, the US FDA approved the application of EECP to patients with angina pectoris combined with heart failure. This article intends to summarize and analyze the literature on the impact of EECP on the cardiac function of patients with IHF and its related mechanisms.
Efficacy
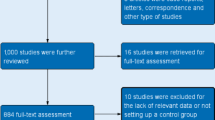
There are only a few randomized controlled studies on the clinical efficacy of EECP in patients with IHF, most of which are cohort studies, and the sample sizes included are relatively small (see Table 1 for details).
EECP Effects on the Performance Status of IHF Patients
In 2006, Arthur et al. published the results of the PEECH study, which included 130 IHF patients with NYHA class II–III, who were randomly assigned to the EECP group or the control group. It was found that the NYHA classification and quality of life of the EECP group were significantly improved after treatment. In terms of exercise tolerance, the total exercise time of the EECP group was significantly higher than that of the control, and this effect lasted for 6 months after treatment. Improvement in peak oxygen uptake (VO2peak) was also observed in the EECP group 1 week after treatment, but this effect disappeared during follow-up [9]. Subsequent researchers conducted subgroup analysis based on age and defined an increase in exercise time by 60 s and an increase in VO2peak by 1.25 ml/kg/min as exercise response. It was found that in subjects over 65 years old, both exercise response rates were significantly higher in the EECP group. The above differences may be due to weaker baseline exercise capacity in elderly patients, which may make it easier to demonstrate the benefits of intervention [10]. Since then, some small sample cohort studies have been conducted one after another, and the results are consistent with the PEECH study. In a word, after the standard course of EECP treatment, total exercise time, 6-min walk test, and NYHA classification were significantly improved in patients with IHF, and these effects did not vary with the difference in baseline ejection fraction levels [8, 11,12,13,14].
EECP Effects on Systolic Function of IHF Patients
Regarding changes in objective indicators of systolic function, left ventricular ejection fraction (LVEF) is the most common evaluation index. However, there is no unified conclusion on the effect of EECP on LVEF. Amr et al. included 42 patients with IHF after coronary artery bypass surgery, and no improvement in LVEF was found after 3 months of follow-up after the treatment [13]. Yavari et al. also did not find a significant improvement in LVEF after EECP treatment in 67 patients with IHF (46.48 ± 13.49% vs. 48.14 ± 16.03, NS) [15]. However, a small sample cohort study conducted by Maryam et al. (N = 20) showed that LVEF improved significantly after standard EECP treatment (40.25 ± 12.72% vs. 46.25 ± 12.97%, P < 0.01) [16]. Fariba followed up 50 patients with IHF who underwent EECP treatment for 1 year and found a significant improvement in LVEF, but in subgroup analysis the efficacy was only observed in patients with baseline LVEF < 40% [17]. While in Ramasamy’s study, the above conclusions did not appear; they included 72 CHD patients with left ventricular dysfunction and found that regardless of the baseline LVEF; this parameter was all improved after EECP treatment [18].
The reasons for the different results above might be affected by the heterogeneity of the included patients, including the differences in the degree of coronary artery lesion, revascularization strategy, and baseline LVEF, which may affect the efficacy of EECP. In addition, for patients with preserved or mildly decreased ejection fraction, whether LVEF is an appropriate evaluation index is also worth exploring. In recent years, the development of cardiac speckle-tracking technology has been rapid. Its myocardial strain parameters can more sensitively and comprehensively evaluate myocardial systolic function than LVEF. A small amount of research has applied speckle-tracking technology to evaluate the clinical efficacy of EECP in CHD patients without heart failure and found significant improvement in global longitude strain (GLS) during EECP treatment [16, 19]. Therefore, it may be necessary to comprehensively evaluate the effect of EECP on cardiac systolic function in patients with IHF by more sensitive indicators on the basis of standardizing the subjects.
EECP Effects on Diastolic Function of IHF Patients
As for the impact of EECP on cardiac diastolic function, there are fewer relevant studies, but the conclusions are relatively consistent [14, 16, 20]. Maryam et al. included 20 angina patients in NYHA functional class III–IV and evaluated diastolic function by E/A (0.92 ± 0.41 vs. 1.08 ± 0.46, P < 0.05) and E/Ea (12.61 ± 4.22 vs. 15.44 ± 6.96, P < 0.05); the above indicators improved significantly after EECP treatment. Other researchers evaluated patients with CHD without heart failure using E/A, left ventricular end-diastolic pressure, peak filling rate (PFR), and the time to PFR, and found that EECP has a potential positive effect on cardiac diastolic function.
EECP Effects on Prognosis of IHF Patients
In the PEECH study, the effect of EECP on short-term prognosis was evaluated; 9% of patients underwent EECP and 13.6% of controls were readmitted within 180 days [9]. Kristen M. et al. enrolled 99 IHF patients who were readmitted for heart failure and gave them EECP treatment after discharge to evaluate the readmission rate within 90 days; only 6 patients (6.1%) had unplanned readmissions compared to the predicted 34%. The above results suggested that EECP might reduce the short-term all-cause readmission rate of IHF patients [11]. In a study of 450 patients with refractory angina and left ventricular dysfunction (LVEF < 30 ± 8%), EECP significantly reduced 6-month emergency room visits by 78% and hospitalizations by 73% [7]. Although the above studies seem to suggest that EECP has some improvement effect on the prognosis of IHF, the heterogeneity of the existing studies is obvious, the observation indicators are relatively single, and they all limit the credibility of the results. In the future, it is necessary to further expand the sample size and extend the follow-up time.
Safety
Given the hemodynamic changes during EECP treatment, an increase in the amount of blood returning to the heart might worsen congestive heart failure. Hence, the evaluation of the safety of EECP in IHF patients is extremely important. However, in clinical practice, no increase in heart failure exacerbation or thrombotic events was observed during or after EECP treatment. The safety of elderly subjects was consistent with that of the entire study population. However, discomfort such as skin and bone occurred significantly more frequently than in the control group [9, 10].
The Potential Mechanisms by Which EECP Improves IHF
At this stage, the mechanisms of EECP are mainly divided into immediate hemodynamic effects and long-term anti-ischemic mechanisms mediated by shear stress, and there are still other potential mechanisms that need to be explored (see Fig. 1 for details).
Reducing Cardiac Load
EECP has significant hemodynamic effects. The synchronous release of all cuffs during systole can reduce systolic blood pressure by 9–16 mmHg, thereby reducing cardiac afterload [6]. In addition, lots of research has shown that EECP can improve shear stress, which can act on endothelial cells, increasing the expression of vasodilators such as NO and decreasing vasoconstrictors such as ET-1 [21, 22, 23•], so the endothelial cell-dependent vasodilation effect increases, further reducing peripheral blood pressure. Darren and other researchers used pulse wave analysis technology and found that the left ventricular energy consumption index and myocardial oxygen demand decreased after EECP treatment [24]. Other researchers observed a significant decrease in resting heart rate after EECP treatment [7, 14]. The above results further indicate a reduction in cardiac load after EECP treatment.
Reducing the Loss of Myocardium
For IHF, the loss of myocardium is mainly due to ischemia. Combined with the existing literature, EECP improves ischemia mainly through the following two mechanisms. One is through direct hemodynamic effects; sequential inflation of EECP cuffs during diastole increases the blood flow at the root of the aorta, raising diastolic blood pressure levels by 26—157% and improving coronary perfusion [6]. And the other mechanism is through improving shear stress to exert subsequent effects. The damage of endothelial cells is the initiation of atherosclerotic lesions, and endothelial cells are also the main responsive cells to shear stress. They can sense and transduct the mechanical signals, initiating mechanical biological signal conversion and feedback mechanisms, ultimately changing endothelial cell morphology and function [25]. Firstly, shear stress can promote the growth of new endothelial cells by directly acting or promoting directional differentiation of endothelial progenitor cells and inhibiting their excessive proliferation and apoptosis [26,27,28]. Secondly, as mentioned above, shear stress can affect the secretion of vasoactive substances by endothelial cells, thereby promoting coronary artery dilation [25, 29, 30]. Thirdly, shear stress can regulate inflammatory factors and oxidative stress and slow down the progression of atherosclerosis and stabilize plaques, reducing the occurrence of acute coronary events. Finally, vascular endothelial growth factor and angiopoietin which involved in regulating vascular generation can respond to changes in shear stress [31,32,33,34,35]. The proliferation, differentiation, and tube formation of endothelial progenitor cells are also regulated by shear stress [36,37,38]. Therefore, shear stress can relieve the ischemia by promoting angiogenesis. Buschmann et al. selected 23 patients with stable angina pectoris and divided them into EECP group and control group; coronary angiography was performed before and after treatment. It was found that the collateral flow index (CFI) and fractional flow reserve (FFR) in the EECP group were significantly improved. The above studies indicate that EECP treatment can clearly improve myocardial perfusion, and its mechanism may be related to increasing collateral circulation [39].
Enhancing the Contractility
As mentioned earlier, EECP can enhance cardiac contractility by improving myocardial ischemia. However, there is no study to evaluate whether EECP can directly affect the myocardial tissue. Mitochondria are important places for cells to perform respiration and oxidative phosphorylation, and finally produce ATP. Cardiac mitochondria provide continuous energy for the beating heart, and its functional state directly affects cardiac contractility. Recent works of authors’ research group suggested that standard course of EECP treatment may increase plasma adrenomedullin (ADM) level. ADM is a vasodilator peptide which secreted by endothelium. Previous animal studies have found that the absence of ADM action could induce myocardial fibrosis and decrease LVEF, accompanied by a decrease in mitochondrial number, membrane potential, and respiratory function [40•]. At the same time, previous studies have suggested that ADM can affect the L-type calcium current in guinea-pig ventricular myocytes, and calcium ion level is an important factor affecting myocardial contractility, which is the basis for myocardial electromechanical coupling [41]. Therefore, we are curious whether EECP can directly increase cardiac contractility by improving mitochondrial function or affecting electromechanical coupling through upregulating ADM or other substances, and whether this process is mediated by shear stress. However, the existing evidence is not enough to support the above hypothesis. Further studies are needed to clarify in the future.
Summary
Given the mechanisms of EECP, the primary concern for its application in patients with heart failure is safety assessment. Based on existing research results, the use of EECP in the stable stage of ischemic heart failure does not increase the risk of serious adverse events (including worsening heart failure and thrombotic events), but the discomforts of skin and bone may increase. In terms of effectiveness, EECP treatment can significantly improve NYHA classification and increase exercise time regardless of the cause of heart failure or baseline LVEF. At the same time, there is a clear improvement in diastolic function of the heart, while the effect on systolic function is not clear. There is an improvement in short-term prognosis indicators such as heart failure readmission after EECP treatment. In terms of exploring the mechanisms by which EECP improves heart failure, in addition to its immediate hemodynamic effects to reduce cardiac afterload and increase coronary perfusion, existing evidence mainly suggests that EECP can improve endothelial cell function to increase vasodilator release and promote neovascularization by upregulating shear stress and thus increasing myocardial contractility.
Combining the above conclusions, it can be found that there are still many limitations in the exploration of EECP application in IHF: ① lack of large-scale RCT studies, existing research designs have shortcomings such as small sample size, non-blinding, high heterogeneity, which affect the reliability of results; ② lack of long-term follow-up observation limits the long-term evaluation of safety and efficacy of EECP in patients with IHF; ③ the evaluation indicators are relatively single, the comprehensive application of echocardiography, speckle-tracking imaging, cardiac magnetic resonance, and other methods can more comprehensively and sensitively evaluate changes in cardiac function; ④ in terms of exploring the mechanisms, it is currently mainly limited to its improvement in myocardial perfusion. Future research would explore whether EECP can directly enhance myocardial cell contractility to improve cardiac function.
Data Availability
Data availability is not applicable to this article as no new data were created or analyzed in this study.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Chinese College of Cardiovascular Physicians, Chinese Heart Failure Center Alliance. Expert Consensus on Decision-making Pathway for Quadruple Pharmacotherapy Management of Chronic Heart Failure. Chin Circ J. 2022;37:769–81.
Liyuan M, ZengW W, Jing F, Shengshou H. Summary of the China cardiovascular health and disease report 2021. Chin J Intervent Cardiol. 2022;30(7):481–95.
Guifu W, Zhimin D, Chengheng H, et al. Enhanced External Counterpulsation-Theory and Practice, 1st edit. People’s Medical Publishing House; 2012.
Gibbons RJ, Abrams J, Chatterjee K, et al. ACC/AHA 2002 guideline update for the management of patients with chronic stable angina-summary article: a report of the American College of Cardiology /American Heart Association Task Force on Practice Guidelines (Committee on the Management of Patients With Chronic Stable Angina). Circulation. 2003;107(1):149–58.
Task Force M, Montalescot G, Sechtem U, et al. 2013 ESC guidelines on the management of stable coronary artery disease: the task force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J. 2013;34(38):2949–3003.
Cardiovascular Group, Geriatrics Branch, Chinese Medical Association. Expert consensus on the clinical application of external counterpulsation in elderly people. Chin J Geriatr. 2019;38(9):953–61.
Sharma U, Ramsey HK, Tak T. The role of enhanced external counter pulsation therapy in clinical practice. Clin Med Res. 2013;1(4):226–32.
William E, Lawsom, Marc AS, et al. Angina patients with diastolic versus systolic heart failure demonstrate comparable immediate and one-year benefit from enhanced external counterpulsation. Journal of Cardiac Failure. 2005;11(1):61–6.
Soran O, Kennard ED, Kfoury AG, et al. Two-year clinical outcomes after enhanced external counterpulsation (EECP) therapy in patients with refractory angina pectoris and left ventricular dysfunction (Report from the International EECP Patient Registry). Am J Cardiol. 2006;97:17–20.
Abbottsmith CW, Chung ES, Varricchione T, et al. Enhanced external counterpulsation improves exercise duration and peak oxygen consumption in older patients with heart failure: a subgroup analysis of the PEECH trial. Congest Heart Fail. 2006;12(6):307–11.
Tecson KM, Silver MA, Brune SD, et al. Impact of enhanced external counterpulsation on heart failure rehospitalization in patients with ischemic cardiomyopathy. Am J Cardiol. 2016;117:901–5.
Manchanda A, Soran O. Enhanced external counterpulsation and future directions step beyond medical management for patients with angina and heart failure. J Am Coll Cardiol. 2007;50:1523–31.
Abdelwahab AA, Elsaied AM. Can enhanced external counter pulsation as a non-invasive modality be useful in patients with ischemic cardiomyopathy after coronary artery bypass grafting? The Egyptian Heart Journal. 2018;70:119–23.
Bonetti PO, Holmes DR, Lerman A, et al. Enhanced external counterpulsation for ischemic heart disease what’s behind the curtain? J Am Coll Cardiol. 2003;41:1918–25.
Yavari M, Montazeri HR. Effects of enhanced external counterpulsation on anginal symptoms and improvements in objective measures of myocardial ischaemia. Cardiovasc J South Afr. 2007;18:154–6.
Esmaeilzadeh M, Khaledifar A, Maleki M, et al. Evaluation of left ventricular systolic and diastolic regional function after enhanced external counterpulsation therapy using strain rate imaging. Eur J Echocardiogr. 2009;10(1):120–6.
Fariba E, Naser A, Babak M, et al. Therapeutic effects of enhanced external counterpulsation (EECP) on clinical symptoms, echocardiographic measurements, perfusion scan parameters and exercise tolerance test in coronary artery disease patients with refractory angina. Int J Med Sci Public Health. 2013;2(2):187–95.
Ramasamy S, Sushma N, Chokkalingam M, et al. Effect of enhanced external counterpulsation treatment on aortic blood pressure, arterial stiffness and ejection fraction in patients with coronary artery disease. JCDR. 2016;10(10):30–4.
Eftekhari A, May O. The immediate hemodynamic effects of enhanced external counterpulsation on the left ventricular function. Scandinavian Cardiovascular Journal. 2012;46(2):81–6.
Urano H, Ikeda H, Ueno T, et al. Enhanced external counterpulsation improves exercise tolerance, reduces exercise-induced myocardial ischemia and improves left ventricular diastolic filling in patients with coronary artery disease. J Am Coll Cardiol. 2001;37:93–9.
Zhang Y, He XH, Liu DH, et al. Enhanced external counterpulsation attenuates atherosclerosis progression through modulation of proinflammatory signal pathway. Arterioscler Thromb Vasc Biol.2010;30(4):773–80.
Alvaro NG, Randy WB. Enhanced external counterpulsation creates acute blood flow patterns responsible for improved flow-mediated dilation in humans. Hypertens Res. 2013;36(4):297–305.
• Xu L, Chen X, Cui M, et al. The improvement of the shear stress and oscillatory shear index of coronary arteries during enhanced external counterpulsation in patients with coronary heart disease. PLoS ONE. 2020;15(3):e0230144. This study used computational fluid dynamics to simulate the hemodynamic changes of the coronary tree before and during EECP treatment and found that EECP can significantly increase the shear stress and improve the local blood flow state, laying the foundation for the exploration of the mechanism of EECP.
Beck DT, Casey DP, Jeffrey S, et al. Enhanced external counterpulsation reduces indices of central blood pressure and myocardial oxygen demand in patients with left ventricular dysfunction. Clin Exp Pharmacol Physiol. 2015;42(4):315–20.
Jing Z, Yi SL, Shu C. Shear stress-initiated signaling and its regulation of endothelial function. Arterioscler Thromb Vasc Biol. 2014;34(10):2191–8.
Frank G, Yuki K, Peter B, et al. Expert recommendations on the assessment of wall shear stress in human coronary arteries: existing methodologies, technical considerations, and clinical applications. Eur Heart J. 2019;40(41):1–17.
Kimiko Y, Tomono T, Takayuki A, et al. Proliferation, differentiation, and tube formation by endothelial progenitor cells in response to shear stress. J Appl Physiol. 2003;95(5):2081–8.
Zeng LF, Xiao QZ, Andriana M, et al. Shear stress-induced stem cell differentiation toward endothelial cells is regulated by HDAC-P53-P21 pathways. 14th IVBM Abstracts. 2012;E52.
Chiu JJ, Lee PL, Chen CN, et al. Shear stress increases ICAM-1 and decreases VCAM-1 and E-selectin expressions induced by tumor necrosis factor-α in endothelial cells. Arterioscler Thromb Vasc Biol. 2004; 24(1):73–9.
Lee DY, Chiu JJ. Atherosclerosis and flow: roles of epigenetic modulation in vascular endothelium. J Biomed Sci; 2019;26(1):56–73.
Brian SC, Zhong DS, Zhao WD, et al. Shear stress regulates occludin and VEGF expression in porcine arterial endothelial cells. J Surg Res. 2002;102(1):13–21.
Joseph WW, Sarah D, Helen MM, et al. Shear stress regulated gene expression and angiogenesis in vascular endothelium. Microcirculation. 2014;21(4):290–300.
Sven C, Nigussie MD, Margret H, et al. Regulation of Foxo-1 and the angiopoietin-2/Tie2 system by shear stress. FEBS Lett. 2007;581(4):673–80.
Madhulika D, Elke B, Beate F, et al. Shear stress-induced activation of the AMP-activated protein kinase regulates FoxO1a and angiopoietin-2 in endothelial cells. Cardiovasc Res. 2008;77(1):160–8.
Sarah LT, Huang RP, Tomsen Nicholas T, et al. Laminar shear inhibits tubule formation and migration of endothelial cells by an angiopoietin-2–dependent mechanism. Arterioscler Thromb Vasc Biol. 2007;27(10):2150–6.
Syotaro O, Haruchika M, Tomoko S, et al. Fluid shear stress induces differentiation of circulating phenotype endothelial progenitor cells. Am J Physiol Cell Physiol. 2012;303(6):595–606.
Zhen Y, Xia WH, Zhang YY, et al.Shear stress-induced activation of Tie2-dependent signaling pathway enhances reendothelialization capacity of early endothelial progenitor cells. J Mol Cell Cardiol. 2012;52(5):1155–63.
Sarah LT. Role of shear stress in angiopoietin-2 dependent neovascularization: implications in occlusive vascular disease and atherosclerosis (Dissertation). Georgia Institute of Technology: Emory University; 2008.
Buschmann EE, Utz W, Pagonas N, et al. Improvement of fractional flow reserve and collateral flow by treatment with external counterpulsation (Art.Net.-2 Trial). Eur J Clin Invest. 2009; 39 (10):866–75.
• Cui NQ, Sakurai T, Kamiyoshi A, et al. Adrenomedullin-RAMP2 and -RAMP3 systems regulate cardiac homeostasis during cardiovascular stress. Endocrinology. 2021;162(3):1–20. This study proves that ADM plays an important role in maintaining the aerobic oxidation capacity of mitochondria, thereby further ensuring the cardiac systolic function. Combined with the previous research results of our research group, it provides clues for other potential mechanisms of EECP.
Du YM, Tang M, Liu CJ, et al. Inhibitory effect of adrenomedullin on L-type calcium currents in guinea-pig ventricular myocytes. Sheng Li Xue Bao; 2002;54(6):479–84.
Funding
This work was supported by the “Clinical key project of the Peking University Third Hospital of Peking University (BYSYZD2021008),” “Youth incubation fund of the Peking University Third Hospital of Peking University (BYSYFY2021013),” and “Beijing Haidian District Health Development Scientific Research Cultivation Program (HP2023-03–501001).”
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Literature retrieval and analysis were performed by LingXu. The first draft of the manuscript was written by LingXu, the revise of the manuscript was performed by MingCui and WeiZhao, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical Approval
Not applicable.
Competing Interests
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Xu, L., Cui, M. & Zhao, W. The Effect of EECP on Ischemic Heart Failure: a Systematic Review. Curr Cardiol Rep 25, 1291–1298 (2023). https://doi.org/10.1007/s11886-023-01943-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11886-023-01943-1