Abstract
Purpose of this Review
We discuss the role of observational studies and cardiac registries during the COVID-19 pandemic. We focus on published cardiac registries and highlight contributions to the field that have had clinical implications.
Recent Findings
We included observational studies of COVID-19 patients published in peer-reviewed medical journals with defined inclusion and exclusion criteria, defined study design, and primary outcomes. A PubMed and MEDLINE literature review results in 437 articles, of which 52 include patients with COVID-19 with cardiac endpoints. From July 2020 to December 2021, the average time from last data collected to publication was 8.9 ± 4.1 months, with an increasing trend over time (R = 0.9444, p < 0.0001). Of the 52 articles that met our inclusion criteria, we summarize main findings of 4 manuscripts on stroke, 14 on acute coronary syndrome, 4 on cardiac arrest, 7 on heart failure, 7 on venous thromboembolism, 5 on dysrhythmia, and 11 on different populations at risk for cardiovascular.
Summary
Registries are cost effective, not disruptive to essential health services, and can be rapidly disseminated with short intervals between last data point collected and publication. In less than 2 years, cardiac registries have filled important gaps in knowledge and informed the care of COVID-19 patients with cardiovascular conditions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) causes the coronavirus disease 2019 (COVID-19) which has rapidly resulted in a global pandemic. Cardiovascular complications of COVID-19 cause significant morbidity and mortality. Given the infectious nature of this disease, rapid responses from health care workers are required, and as such, there is a need to develop methods which can help analyze a high volume of reliable, accurate, patient-level data with avenues for rapid dissemination of information [1••]. We discuss characteristics of this pandemic that illustrate the advantages of conducting research using observational studies rather than interventional trials. Secondly, we will focus on the impact of cardiac registries during the pandemic and highlight lessons learnt that have helped us navigate cardiac care during this challenging period.
Registries as the Ideal Vehicle of Research During COVID-19 Pandemic
The National Committee on Vital and Health Statistics defines registries as systems for “the collection, storage, retrieval, analysis, and dissemination of information on individuals who have either a particular disease or a risk factor(s) known or suspected to cause adverse health effects, to be useful for specific public health purposes” [2•, 3•]. Table 1 summarizes characteristics of the COVID-19 pandemic that made registries valuable for the rapid collection and dissemination of knowledge ideal for conducting research.
Given that multiple mutations have created an evolving myriad of complications and patterns of transmission, data obtained from registries can provide health care workers with rapid real-time information to inform clinical decision making. Much like the disease itself, registries have a capacity to change over time to enhance efficiency. Indeed, vital information can be added to registries in a dynamic manner, thereby providing registries with the flexibility to adjust according to changes during the pandemic. Observational data can be valuable in helping to accelerate the dissemination of information and provide real-world evidence in a time and cost-effective manner to manage this challenging disease.
The initial COVID-19 research came from single center or regional collaborators with small sample sizes, and this evolved over time [4•] to multinational collaborators that resulted in an increase in global article production from 3.6 to 4.9% [4•]. With an emphasis on collaboration, there have been dynamic changes in the structure of scientific activity [4•], which includes the flexibility to provide funding to address urgent needs, overcoming the potentially elevated costs associated with extensive international collaboration. Registries are more cost effective than RCTs, and depending on study characteristics, can result in savings of up to USD 600,000 on data-associated costs alone [5].
The COVID-19 pandemic has caused significant strain on research infrastructure [6]. Specifically, the dynamic nature of the pandemic requires the availability of appropriate resources for allocation to the most severe patients. Indeed, hospitals were stressed financially, and in combination with an elevated fear of infection, this resulted in national and international lockdowns. A large number of investigators and sponsors stopped clinical trial enrollment, a practice which has been commonplace during the pandemic. Registries allowed real-time, observational research with limited burden on the health care system by allowing waiver of consents, minimizing patient contact, and flexible abstraction of information during the pandemic [7•].
Methods
For this review, cardiac registries were defined as outlined by the National Committee on Vital and Health Statistics and recent research by Dawson et al. [8•], and were only included if they had the following characteristics:
-
1.
Well-defined inclusion and exclusion criteria
-
2.
Defined study design
-
3.
Primary outcome measures
-
4.
Results published in a peer-reviewed medical journal
-
5.
Defined patient population with confirmed COVID-19 infection
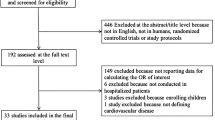
We searched PubMed (including MEDLINE) from May 2020 to December 31, 2021, using the search terms “COVID” AND “Cardiac” AND “Registry” for peer-reviewed studies published in English. This search yielded 437 studies. After removal of retractions, RCTs, non-English articles, reviews, protocols, and brief reports, 320 articles remained. From these 320, 99 were removed as they did not focus on patients with COVID-19, and from the remaining 221 articles, 52 manuscripts met our inclusion guidelines (Fig. 1). The 52 manuscripts included 14 related to myocardial injury/acute coronary syndrome (ACS), 11 to at-risk populations, 7 to venous thromboembolism (VTE), 7 to heart failure (HF), 5 to dysrhythmia, 4 to stroke, and 4 to cardiac arrest (CA). Supplementary Table 1 summarizes populations studied and results from the above studies.
Rapid Dissemination of Information
From July 2020 to December 2021, the average time from last data point included to publication was 8.9 ± 4.1 months, with an increase in publication time towards December 2021 (R = 0.9444, p < 0.0001) (Fig. 2). The average number of months between the last data point collected and publication in the months of July to September 2020 was 2.8 ± 1.6 months, compared to 13.6 ± 4.2 months in October to December of 2021. These intervals are significantly shorter than typical intervals in standard registry publications in pre-pandemic times with examples from STEMI registries ranging from 54 to 186 months [9, 10].
ACS/Myocardial Injury
Based on 14 registries with 18–1310 patients with COVID-19 and ACS or myocardial injury, the North American COVID-19 Myocardial Infarction registry found that patients with COVID-19 and STEMI are more likely to be non-white and diabetic [11••]. Furthermore, patients with COVID-19 and STEMI have higher in-hospital mortality, have higher rates of cardiogenic shock, and are more likely to have no culprit lesions identified on invasive angiography as compared to STEMI patients without COVID-19 [11••, 12,13,14,15]. Patients with NSTEMI and COVID-19 are less likely to undergo invasive coronary angiography and PCI than patients with NSTEMI but without COVID-19, and they tend to have higher hospital admission and mortality rates than patients with COVID-19 and STEMI [14]. Finally, in contrast to increased prevalence of cardiogenic shock in patients with COVID-19 and STEMI, cardiogenic shock prevalence is not increased in patients with COVID-19 and NSTEMI [13].
Patients with severe COVID-19 admitted to the hospital have elevated C-reactive protein, D-Dimer, and troponins, which can increase risk of death or ICU admission [16]. Furthermore, elevated troponin levels appear to be associated with mortality in older and in intubated or severe patients with COVID-19 [17,18,19]. In hospitalized patients with COVID-19 and elevated troponin levels, 65.7% show left and/or right ventricular dysfunction by conventional and speckle tracking echocardiography [20]. Imaging studies suggest multiple mechanisms of injury to help describe the COVID-19 microthrombi pathway, including fibrosis, edema, myocarditis, elevated troponin, and elevated native T1 and T2 cardiovascular magnetic resonance imaging values [21,22,23,24].
Stroke
Four registries with 38–5761 patients with COVID-19 and stroke were included, with results showing that COVID-19-associated ischemic strokes are more severe with worse functional outcome and higher mortality than non-COVID-19 ischemic strokes [25••]. Furthermore, COVID-19 is a risk factor for ischemic stroke [26]. Those who suffer from ischemic stroke tend to be older with the median time between the onset of COVID-19 symptoms and diagnosis of stroke at 2 weeks [26, 27]. In one registry of patients with COVID-19 and stroke, intracerebral hemorrhage was common occurring in 15.2% [28].
VTE/Thrombosis
Seven registries with 49–2601 patients suggest that although asymptomatic patients with COVID-19 have elevated markers of thrombo-inflammatory activation (such as ferritin and D-Dimers) [29], this did not translate into higher rates of VTE in patients with COVID-19 compared to those without COVID-19 [30]. However, those with COVID-19 and prior oral anticoagulants had higher mortality than those not taking oral anticoagulants [31], with a potential benefit associated with antiplatelet use [32]. Critically ill patients with COVID-19 infection have a much more aggressive thrombotic profile. Close to 1 in 4 ICU patients with COVID-19 suffer from venous thrombotic events with up to 52% of these complications representing pulmonary embolism [30, 33,34,35].
Arrhythmias
Arrhythmias are more frequent in hospitalized patients who are older, male, and critically ill with COVID-19, with an incidence of 11.7 to 21.8% [36, 37]. These include sinus bradycardia, paroxysmal supraventricular tachycardia, and tachyarrhythmias—all of which have been associated with increased mortality in patients hospitalized with COVID-19 [36,37,38,39,40]. Repolarization abnormalities are also predictive of clinical outcomes [40]. Atrial fibrillation appears to be the most common arrhythmia, accounting for 62.5% of all reported arrhythmias [37], and is associated with an elevated in-hospital mortality as compared to patients with COVID-19 and no atrial fibrillation [36,37,38,39,40].
Cardiac Arrest
In-hospital CA occurs in approximately 5.9% of hospitalized COVID-19 patients. Up to 74% of these in-hospital cardiac arrests occur in ICU patients [41•]. Prior history of coronary artery disease, atrial fibrillation/flutter, cerebrovascular disease, hypertension, HF, chronic kidney disease [41•, 42, 43], and diabetes mellitus [43, 44] are major risk factors for patients with in-hospital CA. The 30-day mortality rate was lower among in-hospital CA patients than out of hospital CA patients with COVID-19 [44].
At-Risk Populations
While nearly 1 in 3 hospitalized patients with COVID-19 have a history of heart disease [45], there is heterogeneity in the strength of association between heart disease and in-hospital mortality [45,46,47,48]. Risk of mortality appears to range between 29.7 and 35.7% in hospitalized patients with COVID-19 and a history of CVD [45,46,47]. History of HF is independently associated with in-hospital mortality [45, 49, 50]. Patients with COVID-19 who were already on ACEIs/ARBs, β-blockers, glucocorticoids, and statins have a better survival rate compared to those not on these medications [49,50,51,52,53,54]. COVID-19 mortality in adults with congenital heart disease was not greater than the general population and was increased in those with worsening physiologic stage as opposed to anatomic complexity alone [55•].
Heart Failure
Based on 7 registries with 40–12,226 patients hospitalized with COVID-19 and pre-existing CVD, 20% had HF [56•]. Patients with HF and COVID-19 were generally older [56•, 57,58,59,60,61] and had associated cardiovascular comorbidities [56•, 58,59,60] compared to those without COVID-19. Patients with COVID-19 and HF are more likely to require ICU admission [56•, 58, 59], more likely to require mechanical ventilation support or intubation [56•, 58,59,60], and have a higher in-hospital mortality than patients with COVID-19 and no heart failure [56•, 57,58,59,60,61,62].
Limitations
The majority of registry data come from hospitalized patients, with a paucity of data for outpatients with COVID-19. Observational patient data are mostly derived from the early phases of the pandemic, which can lead to selection bias as it fails to capture areas affected in subsequent waves. Some of the sample sizes in the abovementioned studies are small, with data gathered retrospectively potentially leading to bias.
Conclusion
To adequately understand and respond to this evolving COVID-19 pandemic, there is a need for a research platform that is flexible and modifiable, accommodates international collaboration, is cost effective, is not disruptive to essential health services, and has avenues for rapid dissemination. Registries can best serve this purpose. In less than 2 years, cardiac registries have taught us that patients with COVID-19 have a high chance of having underlying cardiovascular disease when hospitalized, have distinct clinical characteristics, and have worse hospital outcomes when presenting with ACS. Furthermore, these patients with COVID-19 have a high incidence of fatal stroke complications and pulmonary embolism when critically ill. Arrhythmias are not uncommon in this patient population, and along with heart failure, signalize worse outcomes compared to those without these features. We await with enthusiasm further publications from these registries as investigators seek to shed light into mechanisms and pathophysiology of disease to help us refine management.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
•• Albhaisi, S, Wenzel R. P. The value of medical registries and observational studies early in pandemics: the COVID-19 experience. Clin Infect Dis. 2021. This review includes a through analyses of the definition, utility and limitations of registries, with a very broad focus.
• Brindis RG, Bates ER, Henry TD. Value of registries in st-segment-elevation myocardial infarction care in both the pre-coronavirus disease 2019 and the coronavirus disease 2019 Eras. J Am Heart Assoc. 2021;10(1):e019958. This commentary includes a brief update on the current state of cardiac registries through the COVID-19 era and highlights the changes in treatment efficiency.
• Gliklich R, Dreyer NLM. Registries for evaluating patient outcomes: a user’s guide. 3rd ed. 2014. Available from: https://www.ncbi.nlm.nih.gov/books/NBK208643/. Accessed 30 Nov 30, 2021. This guide discusses the many types of registries and highlights the importance of the different types. This guides also helps to define what a registry is.
• Fry CV, et al. Consolidation in a crisis: patterns of international collaboration in early COVID-19 research. PLoS One. 2020;15(7):e0236307. This study shows how collaboration and the scientific team structure has changed internationally during the COVID-19 era.
Anderson BR, et al. Registry-based trials: a potential model for cost savings? Cardiol Young. 2020;30(6):807–17.
Leclerc T, et al. Prioritisation of ICU treatments for critically ill patients in a COVID-19 pandemic with scarce resources. Anaesth Crit Care Pain Med. 2020;39(3):333–9.
• Dehghani P, et al. North American COVID-19 ST-Segment-Elevation Myocardial Infarction (NACMI) registry: rationale, design, and implications. Am Heart J. 2020;227:11–8. This study protocol highlights the potential that registries can have during the COVID-19 era, including the waived consent option to help facilitate research.
• Dawson LP, et al. Characteristics and quality of national cardiac registries: a systematic review. Circ Cardiovasc Qual Outcomes. 2021;14(9):e007963. This review helped to develop the registry guidelines included in this manuscript and helped with understanding the quality of the registries.
Russo JJ, et al. Safety and efficacy of staged percutaneous coronary intervention during index admission for st-elevation myocardial infarction with multivessel coronary disease (Insights from the University of Ottawa Heart Institute STEMI Registry). Am J Cardiol. 2015;116(8):1157–62.
Zeymer U, et al. The ESC ACCA EAPCI EORP acute coronary syndrome ST-elevation myocardial infarction registry. Eur Heart J Qual Care Clin Outcomes. 2020;6(2):100–4.
•• Garcia S, et al. Initial findings from the North American COVID-19 myocardial infarction registry. J Am Coll Cardiol. 2021;77(16):1994–2003. This study demonstrates efficiency that a registry can have during a pandemic: 64 sites collected data on 1,185 patients in 13 months and published practice-changing findings in a high-impact journal on patients with STEMI and COVID-19.
De Luca G, et al. Impact of SARS-CoV-2 positivity on clinical outcome among STEMI patients undergoing mechanical reperfusion: Insights from the ISACS STEMI COVID 19 registry. Atherosclerosis. 2021;332:48–54.
Kite TA, et al. International Prospective Registry of Acute Coronary Syndromes in Patients with COVID-19. J Am Coll Cardiol. 2021;77(20):2466–76.
Rashid M, et al. Outcomes of COVID-19-positive acute coronary syndrome patients: a multisource electronic healthcare records study from England. J Intern Med. 2021;290(1):88–100.
Rodriguez-Leor O, et al. In-hospital outcomes of COVID-19 ST-elevation myocardial infarction patients. EuroIntervention. 2021;16(17):1426–33.
Hodges G, et al. Association between biomarkers and COVID-19 severity and mortality: a nationwide Danish cohort study. BMJ Open. 2020;10(12):e041295.
De Marzo V, et al. Prevalence and prognostic value of cardiac troponin in elderly patients hospitalized for COVID-19. J Geriatr Cardiol. 2021;18(5):338–45.
Metkus TS, et al. Myocardial Injury in Severe COVID-19 Compared with Non-COVID-19 acute respiratory distress syndrome. Circulation. 2021;143(6):553–65.
Si D, et al. Death, discharge and arrhythmias among patients with COVID-19 and cardiac injury. CMAJ. 2020;192(28):E791–8.
Bieber S, et al. Left and right ventricular dysfunction in patients with COVID-19-associated myocardial injury. Infection. 2021;49(3):491–500.
Daniels CJ, et al. Prevalence of clinical and subclinical myocarditis in competitive athletes with recent SARS-CoV-2 infection: results from the big ten COVID-19 cardiac registry. JAMA Cardiol. 2021;6(9):1078–87.
Maurus S, et al. Differences in cardiac magnetic resonance imaging markers between patients with COVID-19 associated Myocardial Injury and Patients With Clinically Suspected Myocarditis. J Thorac Imaging. 2021;36(5):279–85.
Puntmann VO, et al. Outcomes of Cardiovascular Magnetic Resonance Imaging in Patients Recently Recovered From Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020;5(11):1265–73.
Weckbach LT, et al. Myocardial Inflammation and Dysfunction in COVID-19-Associated Myocardial Injury. Circ Cardiovasc Imaging 2021;14(1):e012220.
•• Ntaios G, et al. characteristics and outcomes in patients with COVID-19 and acute ischemic stroke: the global COVID-19 stroke registry. Stroke 2020;51(9):e254 e258. This registry-based study showed that COVID-19 associated ischemic strokes result in worse functional outcome and higher mortality than non-COVID-19 ischemic strokes.
Katsoularis I, et al. Risk of acute myocardial infarction and ischaemic stroke following COVID-19 in Sweden: a self-controlled case series and matched cohort study. Lancet. 2021;398(10300):599–607.
Sluis WM, et al. Risk, Clinical Course, and Outcome of Ischemic Stroke in Patients Hospitalized With COVID-19: A Multicenter Cohort Study. Stroke. 2021;52(12):3978–86.
Shakil SS, et al. Stroke among patients hospitalized with COVID-19: results from the american heart association COVID-19 cardiovascular disease registry. Stroke. 2021:Strokeaha121035270.
Cremer S, et al. Elevated markers of thrombo-inflammatory activation predict outcome in patients with cardiovascular comorbidities and COVID-19 disease: insights from the LEOSS registry. Clin Res Cardiol. 2021;110(7):1029–40.
Rieder M, et al. Rate of venous thromboembolism in a prospective all-comers cohort with COVID-19. J Thromb Thrombolysis. 2020;50(3):558–66.
Rivera-Caravaca JM, et al. Clinical profile and prognosis in patients on oral anticoagulation before admission for COVID-19. Eur J Clin Invest. 2021;51(1):e13436.
Santoro F, et al. Antiplatelet therapy and outcome in COVID-19: the Health Outcome Predictive Evaluation Registry. Heart. 2021.
Bemtgen X, et al. Thrombotic circuit complications during venovenous extracorporeal membrane oxygenation in COVID-19. J Thromb Thrombolysis. 2021;51(2):301–7.
Santoro F, et al. Anticoagulation Therapy in Patients With Coronavirus Disease 2019: Results From a Multicenter International Prospective Registry (Health Outcome Predictive Evaluation for Corona Virus Disease 2019 [HOPE-COVID19]). Crit Care Med. 2021;49(6):e624–33.
Tacquard C, et al. Impact of High-Dose Prophylactic Anticoagulation in Critically Ill Patients With COVID-19 Pneumonia. Chest. 2021;159(6):2417–27.
Fumagalli S, et al. Atrial fibrillation and COVID-19 in older patients: how disability contributes to shape the risk profile. An analysis of the GeroCovid registry. Aging Clin Exp Res. 2021:1–8.
Mesquita D, et al. Cardiac arrhythmias in patients presenting with COVID-19 treated in Portuguese hospitals: A national registry from the Portuguese Association of Arrhythmology. Pacing and Electrophysiology Rev Port Cardiol (Engl Ed). 2021;40(8):573–80.
Turagam MK, et al. Malignant Arrhythmias in Patients With COVID-19: Incidence, Mechanisms, and Outcomes. Circ Arrhythm Electrophysiol. 2020;13(11):e008920.
Uribarri A, et al. Atrial fibrillation in patients with COVID-19. Usefulness of the CHA2DS2-VASc score: an analysis of the international HOPE COVID-19 registry. Rev Esp Cardiol. 2021;74(7):608–615.
Vandenberk B, et al. Repolarization abnormalities on admission predict 1-year outcome in COVID-19 patients. Int J Cardiol Heart Vasc. 2021;37:100912.
• Acharya P, et al. Incidence, Predictors, and Outcomes of In-Hospital Cardiac Arrest in COVID-19 Patients Admitted to Intensive and Non-Intensive Care Units: Insights From the AHA COVID-19 CVD Registry. J Am Heart Assoc. 2021;10(16):e021204. This registry-based study helped to characterize the outcomes of patients with COVID-19 and cardiac arrest, including stratified analyses based on ICU admission.
Chelly J, et al. Incidence, clinical characteristics, and outcome after unexpected cardiac arrest among critically ill adults with COVID-19: insight from the multicenter prospective ACICOVID-19 registry. Ann Intensive Care. 2021;11(1):155.
Nene RV, et al. Outcomes for in-hospital cardiac arrest for COVID-19 patients at a rural hospital in Southern California. Am J Emerg Med. 2021;47:244–7.
Sultanian P, et al. Cardiac arrest in COVID-19: characteristics and outcomes of in- and out-of-hospital cardiac arrest. A report from the Swedish Registry for Cardiopulmonary Resuscitation. Eur Heart J. 2021;42(11):1094–1106.
CAPACITY-COVID Collaborative Consortium and LEOSS Study Group. Clinical presentation, disease course, and outcome of COVID-19 in hospitalized patients with and without pre-existing cardiac disease: a cohort study across 18 countries. Eur Heart J. 2022;43(11):1104–1120.
Linschoten M, et al. Cardiac complications in patients hospitalised with COVID-19. Eur Heart J Acute Cardiovasc Care. 2020;9(8):817–23.
Tehrani DM, et al. Impact of cancer and cardiovascular disease on in-hospital outcomes of COVID-19 patients: results from the american heart association COVID-19 cardiovascular disease registry. Cardiooncology. 2021;7(1):28.
Phelps M, et al. Cardiovascular comorbidities as predictors for severe COVID-19 infection or death. Eur Heart J Qual Care Clin Outcomes. 2021;7(2):172–80.
Cabezon Villalba G, et al. Impact of the presence of heart disease, cardiovascular medications and cardiac events on outcome in COVID-19. Cardiol J. 2021;28(3):360–8.
Terlecki M, et al. Association between cardiovascular disease, cardiovascular drug therapy, and in-hospital outcomes in patients with COVID-19: data from a large single-center registry in Poland. Kardiol Pol. 2021;79(7–8):773–80.
Daniels LB, et al. Relation of prior statin and anti-hypertensive use to severity of disease among patients hospitalized with COVID-19: Findings from the American Heart Association's COVID-19 Cardiovascular Disease Registry. PLoS One. 2021;16(7):e0254635.
Nunez-Gil IJ, et al. Underlying heart diseases and acute COVID-19 outcomes. Cardiol J. 2021;28(2):202–14.
Pagnesi M, et al. Determinants of the protective effect of glucocorticoids on mortality in hospitalized patients with COVID-19: Insights from the Cardio-COVID-Italy multicenter study. Int J Infect Dis. 2021;108:270–3.
Pareek M, et al. Relation of Cardiovascular Risk Factors to Mortality and Cardiovascular Events in Hospitalized Patients With Coronavirus Disease 2019 (from the Yale COVID-19 Cardiovascular Registry). Am J Cardiol. 2021;146:99–106.
• Broberg CS, et al. COVID-19 in Adults With Congenital Heart Disease. J Am Coll Cardiol. 2021;77(13):1644–55. This registry-based study helped to characterize the impact of COVID-19 on patients with congenital heart disease, including the association of mortality with physiological state.
• Sokolski M, et al. Heart failure in COVID-19: the multicentre, multinational PCHF-COVICAV registry. ESC Heart Fail. 2021. This registry-based study helped to characterize the impact of COVID-19 on patients with heart failure. Their analyses included comparisons of patients with HF to those with other cardiovascular disease and risk factors.
Birati EY, et al. Characteristics and Outcomes of COVID-19 in Patients on Left Ventricular Assist Device Support. Circ Heart Fail. 2021;14(4):e007957.
Caraballo C, et al. COVID-19 infections and outcomes in a live registry of heart failure patients across an integrated health care system. PLoS One. 2020;15(9):e0238829.
Goyal P, et al. Clinical characteristics and outcomes of adults with a history of heart failure hospitalized for COVID-19. Circ Heart Fail. 2021;14(9):e008354.
Panagides V, et al. History of heart failure in patients with coronavirus disease 2019: Insights from a French registry. Arch Cardiovasc Dis. 2021;114(5):415–25.
Salinas-Botrán A, et al. Clinical characteristics and risk factors for mortality upon admission in patients with heart failure hospitalized due to COVID-19 in Spain. Rev Clin Esp. 2021.
Rodilla E, et al. Impact of Arterial Stiffness on All-Cause Mortality in Patients Hospitalized With COVID-19 in Spain. Hypertension. 2021;77(3):856–67.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Garcia reports grants and personal fees from Edwards Lifesciences and Medtronic, personal fees from BSCI, and grants from Abbott Vascular, outside the submitted work. The other authors do not have anything to disclosure, including no relationship to industry pertaining to this manuscript.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Interventional Cardiology
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Singh, J., Durr, MR.R., Deptuch, E. et al. Cardiac Registries During the COVID-19 Pandemic: Lessons Learned. Curr Cardiol Rep 24, 659–665 (2022). https://doi.org/10.1007/s11886-022-01686-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11886-022-01686-5