Abstract
Purpose of Review
Diabetes mellitus (DM) is a major comorbidity of heart failure (HF). Comparing the similarities and differences in disease characteristics and treatment between the HF patients with and without DM, this review was to investigate whether and how the novel class of sodium-glucose transport protein 2 inhibitors (SGLT2i) would benefit both populations.
Recent Findings
Despite the obviously different clinical profiles, patients of HF with reduced ejection fraction (HFrEF) should be treated the same with guideline directed medical therapy, irrespective of DM status. Upon the mounting evidence that supported its use in diabetic patients at high risk of HF, recent large clinical trials demonstrated that SGLT2i could further reduce HF hospitalization or cardiovascular mortality and improve quality of life in diabetic and non-diabetic HFrEF patients who were optimally managed.
Summary
SGLT2i expands the foundation of HFrEF therapy. Whether it is equally effective in HF with preserved ejection fraction awaits more evidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetes mellitus (DM) is a common comorbidity in heart failure (HF) patients, occurring in 20–40% of patients with HF with reduced ejection fraction (HFrEF) and more frequently in HF with preserved ejection fraction (HFpEF) [1,2,3]. Besides diabetic cardiomyopathy which displays two distinct phenotypes as metabolism-mediated restrictive HFpEF phenotype and autoimmune-mediated dilated HFrEF phenotype [4], DM drives a fourfold higher prevalence of HF via its combined atherogenic effect with hypertension and dyslipidemia [5]. Conversely, HF patients are predisposed to DM through dysregulated neurohormonal system [6], HF medication, and reduced physical activity [7]. This review will focus on the special patient population of HF with DM and compare to the HF population without DM for similarities and differences in terms of disease profile, clinical impact, as well as the implication of medical therapy by the novel class of anti-diabetic drugs, the sodium-glucose transport protein 2 inhibitors (SGLT2i).
HF Patients With or Without DM: Are They Different?
Clinical Profile
HF patients with DM are younger, have higher body mass index (BMI), experience worse symptoms, and have a prevalent background of ischemic heart disease both in HFrEF and HFpEF [2, 8,9,10]. In addition to a greater burden of hypertension, chronic kidney disease, hyperlipidemia, anemia, and chronic obstructive pulmonary disease [2, 8, 11], DM was associated with a 34% higher risk of atrial fibrillation (AF) [12]. Diabetic patients with AF were more symptomatic who had markedly increased adverse cardiovascular (CV) outcomes [13], including a 70% increased relative risk of thromboembolic stroke events [14].
Biomarkers in Subtypes of HF
The Prospective Comparison of ARNI With ACEI to Determine Impact on Global Mortality and Morbidity in Heart Failure (PARADIGM-HF) trial found a significantly higher N-terminal pro-brain natriuretic peptide (NT-proBNP) level in HFrEF patients with undiagnosed DM at baseline, compared to the prediabetic and normoglycemic group, but not in those with diagnosed DM [15]. However, the link between NT-proBNP and DM in patients with HFpEF was less consistent across studies which may partially explained by different inclusion criteria: Irbesartan in Heart Failure with Preserved Ejection Fraction (I-PRESERVE) trial showed higher NT-proBNP in patients with DM [9]; Phosphodiesterase-5 Inhibition to Improve Clinical Status and Exercise Capacity in Heart Failure With Preserved Ejection Fraction (RELAX) trial found similar NT-proBNP between DM and non-DM cohorts [16]; the Get With The Guidelines (GWTG)-HF registry, however, showed lower NT-proBNP in patients with DM [11]. Furthermore, Fousteris et al. demonstrated an increased soluble ST2 (sST2) in patients with DM, which was more pronounced in the presence of left ventricular diastolic dysfunction [17]. A similar trend was observed in both HFrEF [18] and HFpEF cohorts [19]. In the RELAX trial, diabetic patients with HFpEF had higher levels of galectin-3 (Gal-3) [16]. Alanso et al. showed an elevated Gal-3 level, rather than sST2, in ambulatory HF patients with DM; after adjusting for age, sex, BMI, and estimated glomerular filtration rate (eGFR), the correlation attenuated [20]. Note that the relationship between Gal-3 and DM might be complicated by renal dysfunction [21].
Myocardial Imaging
Either eccentric (dilated/HFrEF) or concentric (restrictive/HFpEF) remodeling is typical structural and functional alterations [22]. Decreased myocardial compliance extensively presents in both phenotypes, as evidenced by higher early mitral inflow velocity and mitral annular early diastolic velocity (E/e’) ratio [2, 9, 16, 23]. DM is associated with smaller left ventricles, greater LV mass, and thicker ventricular wall in HFpEF [16, 23], whereas it only leads to mildly enlarged left ventricular end-diastolic volume index in HFrEF [2, 16, 24, 25]. Despite similar left ventricular ejection fraction (LVEF) between DM and non-DM cohorts, Tanaka et al. demonstrated that global longitudinal strain (GLS) was significantly lower in patients with dilated cardiomyopathy with DM than those without [26]. Cardiac magnetic resonance (CMR) adds more information on DM-related changes of the heart, though they have not been investigated in HF patients. Wong et al. found that DM raised extracellular volume fraction (ECV) in patients with underlying CV diseases and comorbid hypertension referred for clinical CMR [27]. In a Western cohort, patients with prediabetes and DM had lower ECV, higher cell volume, and greater burden of late gadolinium enhancement (LGE) [28]. Paiman et al. found that ECV increased in South Asian but not European patients with DM [29]. Levelt et al. detected increased myocardial triglyceride content and phosphocreatine-to-ATP ratio using 1H and 31P magnetic resonance spectroscopy in patients with DM [30], indicating a potential role of cardiac steatosis in LV concentric remodeling [30, 31]. DM also impaired myocardial perfusion reserve but had an inconsistent correlation with cardiac dysfunction [32, 33].
Mortality and HF Hospitalization
Undoubtedly, HF patients with DM are at greater risk of death and HF hospitalization, which exaggerates in younger women [2, 8, 9, 34,35,36]. However, limited data have suggested the differential impact of DM on patients with HFpEF and HFrEF. Candesartan in Heart failure-Assessment of Reduction in Mortality and Morbidity (CHARM) study showed that DM conferred more adverse effects on patients with HFpEF by increasing the risk of the combined outcome of CV death and HF hospitalization [8]. In contrast, an analysis from Asian Sudden Cardiac Death in Heart Failure (ASIAN-HF) found no interaction between DM and subtype of HF in HF hospitalization [2]. Ather et al. also demonstrated that DM was associated with a similarly increased risk of all-cause mortality in HFrEF and HFpEF patients [3].
HF Patients With or Without DM: Shall Treatment Be Different?
Effects of Anti-HF Therapy on DM Subgroup
HF medications had comparable survival benefits between patients with and without DM, which was delicately concluded in a recent American Heart Association (AHA)/Heart Failure Society of American (HFSA) statement [37]. Briefly, angiotensin converting enzymeinhibitor (ACEI) (captopril [38] and trandolapril [39]), angiotensin receptor blocker (ARB) (valsartan [40, 41], losartan [42], and candesartan [8]), sacubitril-valsartan [15], mineralocorticoid receptor antagonist (MRA) (eplerenone [43]), and ivabradine [44] were equally effective according to the secondary analyses of the pivotal trials, respectively. Treatment effect was concluded to be the same for beta-blocker (carvedilol, metoprolol succinate, and bisoprolol) and enalapril in a meta-analysis [45]. Combined with renin-angiotensin system blockades, carvedilol has more favorable metabolic effects when compared to metoprolol [46]. Notably, sacubitril-valsartan exhibited an extra glucose-lowering effect when compared to enalapril, favoring its use in patients with HF and DM [47]. Device therapy with implantable cardioverter defibrillator (ICD) and cardiac resynchronisation therapy (CRT) also showed consistent benefit in both DM and non-DM patients [48,49,50,51].
Goal of Glucose-lowering Treatment
The optimal range for blood glucose control in patients with HF is not well defined. In Diabetes Mellitus and Diastolic Dysfunction (DADD) study, Jarnert et al. observed no improvement in myocardial diastolic dysfunction and perfusion reserve by implementing strict glycemic control in DM [52]. Multiple studies illustrated a “U” shape relationship between the mortality risk and hemoglobin A1C (HbA1c) in patients with HF, where the lowest point occurred with HbA1c levels of 7.0–7.9% [46, 53, 54]. Despite the lack of consensus, a general target of HbA1c lower than 7.0% is well-accepted. For patients with advanced HF and more serious comorbidities, a lenient glycemic control with a HbA1c level of < 8.5% should be considered [37, 55].
Recent studies have demonstrated that glycemic variability was a more potent prognostic factor [56]. In a secondary analysis from the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial, a relative 10% increase or decrease in HbA1c was associated with 32% and 55% higher risks of HF in patients with DM [57]. Echouffo-Tcheugui et al. found that a greater visit-to-visit variability of fasting blood glucose increased the mortality risk in patients free of CV diseases at baseline [58].
Choice of Metformin or SGLT2i as the First-line Glucose-lowering Agent
Metformin has been the most widely used oral anti-diabetic drug for decades [59]. Since 2006, it was recommended as the first-line glucose-lowering agent for its CV protective effects [60]. There were initial concerns for lactic acidosis when treated patients with HF. Two large observational studies, however, demonstrated that metformin significantly reduced the risk of death and hospitalization compared to sulfonylurea monotherapy in patients with HF, without causing additional metabolic acidosis. In response to these results, FDA removed the warning for HF patients in 2006 [61,62,63]. A systematic review involving 9 observational studies and 34,000 patients with HF and DM further confirmed its efficacy and safety, showing decreased risks of mortality and all-cause hospitalization and a similar risk of lactic acidosis when compared with the control group (mostly treated with sulfonylurea) [64]. Thus, metformin became the first-line drug for glycemic control in patients with HF according to the 2016 European Society of Cardiology (ESC) guidelines on HF management (class IIa, level of evidence C), but is contraindicated in patients with severe renal or hepatic impairment [65]. However, all the data were generated from observational studies. The ongoing Metformin in Patients with Chronic Heart Failure and Diabetes or Insulin Resistance Trial (Met-HeFT) will be the largest randomized study to date powered to address the effects of metformin on clinical outcomes in chronic HFrEF patients [66].
Recently, SGLT2i, a novel class of anti-diabetic agents, exhibited unexpected CV benefits in the CV outcome trials (CVOTs) mandated by FDA since 2008. SGLT2i blocks the reabsorption of glucose by inhibiting SGLT2 in the proximal tubule. The Empagliflozin Cardiovascular Outcome Event Trial in Type 2 Diabetes Mellitus Patients–Removing Excess Glucose (EMPA-REG Outcome) (2015) [67] and the Canagliflozin Cardiovascular Assessment Study (CANVAS) (2017) [68] showed a decreased risk of hospitalization for HF in SGLT2i versus placebo in diabetic patients with CVD [empagliflozin, hazard ratio (HR) 0.65, 95% confidence interval (CI) 0.50–0.85; canagliflozin, HR 0.67, 95% CI 0.52–0.87]. Similar effects were observed with dapagliflozin [Dapagliflozin Effect on Cardiovascular Events (DECLEAR-TIMI 58), 2019] [69] and ertugliflozin [Cardiovascular Outcomes Following Ertugliflozin Treatment in Type 2 Diabetes Mellitus Participants With Vascular Disease (VERTIS CV), 2020] [70, 71]. Accordingly, the American Diabetes Association (ADA)/European Association for the Study of Diabetes (EASD) [72], AHA [37], and Canadian Cardiovascular Society (CCS) [73] recommended SGLT2i for those at high risk or with index HF. But the debate about SGLT2-i or metformin as the first-line choice persists. A recent retrospective multi-institution cohort study enrolled 41,020 DM patients with either SGLT2i or metformin as the first-line therapy. During the 1-year follow-up, patients on SGLT2i had lower risks of HF hospitalization (HR 0.47; 95% CI 0.41–0.54), and all-cause mortality (HR 0.49, 95% CI 0.44–0.55), but a higher risk for ischemic stroke (HR 1.21, 95% CI 1.10–1.32) [74].
Despite the mounting evidence that supported the use of SGLT2i in diabetic patients with HF, higher cost, limited experience, a lack of head-to-head study with metformin, and inconsistent recommendations from different communities hinder its application. In 2019, ESC presented a “major paradigm shift,” which proposes prescribing SGLT2i to diabetic patients at high risks of CV diseases and HF or with index CV diseases, before the initiation of metformin [55]. However, ADA/EASD still advocates metformin for its established pharmacological effects and safety profile, whereas SGLT2i (empagliflozin, canagliflozin, and dapagliflozin) is included in the add-on regimen for diabetic patients with HF or chronic kidney disease irrespective of HbA1c [72, 75, 76].
HF Patients With or Without DM: Not Different in the Era of SGLT2i?
SGLT2i Reduces Mortality and Hospitalization in Chronic HFrEF
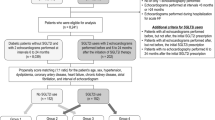
Although the CVOTs of SGLT2i revealed a robust reduction in HF hospitalization and mortality in patients with DM, no more than 20% patients enrolled had established HF, and the characteristics of HF were not well established. It was not confirmed whether the benefit of SGLT2i could extrapolate to HF patients without DM, until recent announcement of two late-breaking randomised control trials (RCTs) known as the Dapagliflozin and Prevention of Adverse-Outcomes in Heart Failure (DAPA-HF) [77••] and the Empagliflozin Outcome Trial in Patients With Chronic Heart Failure With Reduced Ejection Fraction (EMPEROR-Reduced) [78••] which enrolled both diabetic and non-diabetic HF patients (with LVEF ≤ 40%). The trials examined the add-on efficacy of dapagliflozin or empagliflozin versus placebo in patients with HFrEF who had already received guideline-directed medical therapy, respectively. Regardless of mild differences in baseline characteristics, i.e. patients in EMPEROR-Reduced had lower LVEF (27.2% vs. 30.9%) and eGFR (62.2 vs. 65.5 mL·min−1·1.73 m−2) and had more patients with DM (49.8% vs. 41.8%), HF hospitalization (HHF) in previous 12 month (30.7% vs. 27.4%), angiotensin receptor-neprilysin inhibitor (ARNI) (20.7% vs. 10.9%) and CRT (11.9% vs. 6.9%) treatment, but few ischemic cardiomyopathy (50.7% vs. 57.3%), the two trials showed a similar risk reduction in primary outcome of CV death or hospitalization for worsening HF (DAPA-HF: HR 0.74, 95% CI: 0.65–0.85; EMPEROR-Reduced: HR 0.75, 95% CI: 0.65–0.86) [79,80,81]. In the pooled patient-level data analysis of these two trials including 8,474 patients, it reconfirmed that the reduction in relative risk of combined CV death or first hospitalization for HF by using SGLT2i was 26% and 25% in patients with and without DM, respectively (p < 0.0001). The pooled treatment effects showed consistent benefits for predefined subgroups of age, gender, background ARNI therapy, and baseline eGFR [82].
SGLT2i Improves Quality of Life in Chronic HFrEF
The DAPA-HF trial also revealed that patients treated with dapagliflozin had greater improvement in Kansas City Cardiomyopathy Questionnaire (KCCQ)-total symptom score, clinical summary score, and overall summary score at 8 months (2.8, 2.5, and 2.3 points higher versus placebo; p < 0.0001 for all) [83]. Dapagliflozin Effect on Symptoms and Biomarkers in Patients With Heart Failure (DEFINE-HF) was an investigator-initiated, multicenter RCT that investigated the effect of dapagliflozin on biomarkers, symptoms, and functional status in patients with HFrEF. A total of 263 HFrEF patients (63% DM) were randomized to dapagliflozin or placebo treatment for 12 weeks. Dapagliflozin was attributable to both higher proportions of patients with ≥ 5-point improvement in KCCQ overall summary score (42.9 vs. 32.5%, adjusted OR 1.73, 95% CI 0.98–3.05) and ≥ 20% reduction in NT-proBNP (44.0 vs. 29.4%, adjusted OR 1.9, 95% CI 1.1–3.3), which were consistent among patients with or without DM [84]. A substudy of the DEFINE-HF measured lung fluid volumes by remote dielectric sensing and found more patients in the dapagliflozin group who experienced improvement in lung fluid volumes (52.6% vs. 36.8%, p = 0.04) [85].
SGLT2i Benefits in Acute HF or HFpEF Awaits for More Evidence
Ibrahim et al. conducted a RCT to assess the addition of dapagliflozin to furosemide in managing patients with admitted decompensated HFrEF and DM. One hundred patients were randomized into study arm (dapagliflozin plus furosemide) and control arm (furosemide alone). At discharge, the study arm displayed a lower mean total dose of furosemide (597 mg vs. 855 mg), a higher percent in weight loss (5% vs. 3.4%), more patients without dyspnea (34% vs. 16%), and a tendency of fewer patients with worsening renal function (16% vs. 28%, p = 0.148) [86]. Another exploratory RCT also observed in a small group with DM and acute decompensated HF (n = 59) that empagliflozin as an add-on therapy was associated with reduced levels of NT-proBNP and hematocrit but without an increased risk of worsening renal function [87].
Effect of Sotagliflozin on Cardiovascular Events in Patients With Type 2 Diabetes Post Worsening Heart Failure (SOLOIST-WHF) is a trial designed to examine the safety and efficacy of sotagliflozin (an SGLT2i that also provides some gastrointestinal SGLT1 inhibition) in DM patients who were recently hospitalized for worsening HF with a full spectrum of LVEF. The study was ended early due to loss of funding in the COVID-19 crisis. Clinically stabilized patients were randomly assigned to receive sotagliflozin or placebo either before or within 3 days after discharge, who were followed up for a median of 9 months. The sotagliflozin was associated with 33% reduction in primary end-point of CV death, HF hospitalization and urgent visits for HF (first and subsequent events), including 16% reduction in death from CV causes, and 18% in death from any cause. More impressively, the effects on primary outcomes were similar between subgroups of age, gender, and HF phenotypes (HFrEF and HFpEF). However, sotagliflozin also led to increased risks of diarrhea (6.1% vs. 3.4%) and severe hypoglycemia (1.5% vs. 0.3%) [88].
Effects of Empagliflozin on Clinical Outcomes in Patients With Acute Decompensated Heart Failure (EMPA-RESPONSE-AHF) was the first randomized, double-blind, placebo-controlled, multicenter pilot study on the effects of empagliflozin in acute HF (AHF) patients irrespective of LVEF classification and comorbid DM (n = 80) [89]. No difference was observed in VAS dyspnea score, diuretic response, length of stay, or change in NT‐proBNP between empagliflozin and placebo. However, empagliflozin induced more urinary output during the first 4 days [difference 3,449 (95% CI 578–6,321) mL; p < 0.01] with no recorded adverse effects on blood pressure or renal function. More importantly, empagliflozin reduced a combined endpoint of in‐hospital worsening HF, rehospitalization for HF, or death at 60 days compared with placebo (10% vs. 33%, p = 0.014). Currently, other SGLT2i trials in AHF are underway, which include Efficacy and Safety of Dapagliflozin in Acute Heart Failure (DICTATE-AHF), Ertugliflozin in Acute Heart Failure, A Study to Test the Effect of Empagliflozin in Patients Who Are in Hospital for Acute Heart Failure (EMPULSE), Effects of Empagliflozin on Diuresis and Renal Function in Patients With Acute Decompensated Heart Failure (EMPAG-HF), and Effect of Empagliflozin on Cardiac Output in Patients With Acute Heart Failure (EMPA Acute Heart Failure).
In vitro studies demonstrated that SGLT2i could improve left ventricular diastolic function, relieve wall stress, reduce preload, and diminish tissue fibrosis [90]. A number of clinical trials are ongoing to testify mortality or exercise capacity benefits of SGLT2i in patients with HFpEF, such as Dapagliflozin in Preserved Ejection Fraction Heart Failure (PRESERVED-HF), Dapagliflozin Evaluation to Improve the Lives of Patients With Preserved Ejection Fraction Heart Failure (DELIVER), Dapagliflozin Effect on Exercise Capacity Using a 6-min Walk Test in Patients With Heart Failure With Preserved Ejection Fraction (DETERMINE-preserved), and Empagliflozin outcome trial in Patients With chronic heart Failure With Preserved Ejection Fraction (EMPEROR-Preserved).
SGLT2i Emerges as an Anti-HF Drug in the “Fantastic Four” [91]: Call for Action
Real-world studies are useful to examine the degree to which extent the results from RCTs could apply to patients outside the trials and also to assess long-term response and safety. The Comparative Effectiveness of Cardiovascular Outcomes in New Users of SGLT-2 Inhibitors (CVD-REAL) study enrolled more than 300,000 patients with DM and newly initiated on any SGLT2i or other glucose-lowering drugs from six countries in the USA or Europe. Patients treated with SGLT2i in CVD-REAL were younger (56.9 vs. 63.1 vs. 63.3 years), had more females (43.3 vs. 28.8 vs. 35.8%), and fewer established CVD (13.1 vs. 99 vs. 65.6%) than patients in EMPA-REG Outcome and CANVAS. However, the CVD-REAL revealed similar results that SGLT2i was associated with a 39% relative risk reduction in HF hospitalization, 51% in all-cause mortality when compared to other glucose-lowering drugs after propensity score matching to account for potential confounding factors [92]. The results were consistent across countries, regardless of the use of specific SGLT2i (predominantly canagliflozin in the USA; dapagliflozin in Europe), suggesting a class effect rather. Subsequently, the CVD-REAL2 study conducted in over 400,000 patients from Asia Pacific (South Korea, Japan, Singapore, and Australia), Middle East (Israel), and North America (Canada) demonstrated the benefits of SGLT2i over other oral glucose-lowering drugs, with a 49% relative risk reduction in death, 36% in HHF, 19% in myocardial infarction and 32% in stroke. The results were consistent across countries and patient subgroups, including those with and without CV diseases [93]. Unfortunately, the real-world data are not available yet to examine whether the findings of the DAPA-HF and EMPEROR-Reduced trials could be extrapolated to routine HFrEF patient care.
Despite solid evidence and strong recommendation by guidelines, the use of SGLT2i in DM patients with indications is much fewer than expected. In a Denmark cohort study of 41,733 patients with a new diagnosis of DM and CVD, the 1-year cumulative user proportions of SGLT2i increased from 0.2% in 2012 to only 8.7% in 2018 [94]. Another real-world use of new agents with CV benefits was examined in a cohort of 21,173 patients with DM and CVD [95], which revealed a slow increase in SGLT2i initiation (5 new prescriptions in the first half of 2014 to 83 new prescriptions in the first half of 2019) and a very low prescription rate of SGLT2i (in 1.4% patients only). Primary care physicians accounted for 53.4% of SGLT2i prescriptions, endocrinologists for 30.3%, and cardiologists for 6.0% [95]. Although no data is available for the use of SGLT2 in real-world HF population, a cohort of 154,714 hospitalized patients with HFrEF (LVEF ≤ 40%) in the GWTG-HF registry identified that four in five patients (irrespective of DM status) would be candidates for dapagliflozin based on the 2020 FDA approval of dapagliflozin for patients with HFrEF to reduce risk of CV death and HHF [96].
Although the mechanisms underlying cardioprotection of SGLT2i has not completely clarified (the proposed hypotheses cover decrease in arterial stiffness and cardiac remodeling, reduction in blood pressure [97], inhibition of cardiac Na + /H + exchanger [98], suppression of cardiac fibrosis [99], natriuresis, and osmotic diuresis [100]), this will not stop SGLT2i from becoming the fourth drug class (following ARNI/ACEI/ARB, beta-blocker, and MRA) that fulfills the goals of HFrEF management independent of glycemic effect. In recently released 2021 update to the 2017 ACC expert consensus decision pathway for optimization of HF treatment, dapagliflozin or empagliflozin representative of SGLT2i is now a followed add-on therapy for HFrEF patients with or without diabetes after ARNI/ACEI/ARB and beta-blocker treatment have started [101].
Conclusion
HF and DM are the two apparently separate disease entities from pathophysiology, diagnosis, and treatment. With the increase in incidence and prevalence of the two conditions, cardiologists and endocrinologists now encounter a crossing path of patient management. The cumulating evidence supports the reduction of HHF for DM patients treated with SGLT2i and recently extended late-breaking evidence of reducing HHF and improving quality of life by SGLT2i in HFrEF patients with and without DM. Such findings not only shifted the paradigm for the foundation of HFrEF therapy, but also pushing into revision of the HF treatment guidelines. Whether SGLT2i is equally effective in HFpEF awaits further multicenter clinical trials.
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
Echouffo-Tcheugui JB, Xu H, DeVore AD, et al. Temporal trends and factors associated with diabetes mellitus among patients hospitalized with heart failure: findings from Get With The Guidelines-Heart Failure registry. Am Heart J. 2016;182:9–20.
Yap J, Tay WT, Teng TK, et al. Association of diabetes mellitus on cardiac remodeling, quality of life, and clinical outcomes in heart failure with reduced and preserved ejection fraction. J Am Heart Assoc. 2019;8(17):e013114.
Ather S, Chan W, Bozkurt B, et al. Impact of noncardiac comorbidities on morbidity and mortality in a predominantly male population with heart failure and preserved versus reduced ejection fraction. J Am Coll Cardiol. 2012;59(11):998–1005.
Seferovic PM, Paulus WJ. Clinical diabetic cardiomyopathy: a two-faced disease with restrictive and dilated phenotypes. Eur Heart J. 2015;36(27):1718–27, 1727a-1727c.
Dei Cas A, Khan SS, Butler J, et al. Impact of diabetes on epidemiology, treatment, and outcomes of patients with heart failure. JACC Heart Fail. 2015;3(2):136–45.
Paolillo S, Rengo G, Pellegrino T, et al. Insulin resistance is associated with impaired cardiac sympathetic innervation in patients with heart failure. Eur Heart J Cardiovasc Imaging. 2015;16(10):1148–53.
Preiss D, van Veldhuisen DJ, Sattar N, et al. Eplerenone and new-onset diabetes in patients with mild heart failure: results from the Eplerenone in Mild Patients Hospitalization and Survival Study in Heart Failure (EMPHASIS-HF). Eur J Heart Fail. 2012;14(8):909–15.
MacDonald MR, Petrie MC, Varyani F, et al. Impact of diabetes on outcomes in patients with low and preserved ejection fraction heart failure: an analysis of the Candesartan in Heart failure: Assessment of Reduction in Mortality and morbidity (CHARM) programme. Eur Heart J. 2008;29(11):1377–85.
Kristensen SL, Mogensen UM, Jhund PS, et al. Clinical and echocardiographic characteristics and cardiovascular outcomes according to diabetes status in patients with heart failure and preserved ejection fraction: a report from the I-Preserve Trial (Irbesartan in Heart Failure With Preserved Ejection Fraction). Circulation. 2017;135(8):724–35.
Aguilar D, Deswal A, Ramasubbu K, Mann DL, Bozkurt B. Comparison of patients with heart failure and preserved left ventricular ejection fraction among those with versus without diabetes mellitus. Am J Cardiol. 2010;105(3):373–7.
McHugh K, DeVore AD, Wu J, et al. Heart failure with preserved ejection fraction and diabetes: JACC state-of-the-art review. J Am Coll Cardiol. 2019;73(5):602–11.
Huxley RR, Filion KB, Konety S, Alonso A. Meta-analysis of cohort and case-control studies of type 2 diabetes mellitus and risk of atrial fibrillation. Am J Cardiol. 2011;108(1):56–62.
Du X, Ninomiya T, de Galan B, et al. Risks of cardiovascular events and effects of routine blood pressure lowering among patients with type 2 diabetes and atrial fibrillation: results of the ADVANCE study. Eur Heart J. 2009;30(9):1128–35.
Patti G, Cavallari I, Andreotti F, et al. Prevention of atherothrombotic events in patients with diabetes mellitus: from antithrombotic therapies to new-generation glucose-lowering drugs. Nat Rev Cardiol. 2019;16(2):113–30.
Kristensen SL, Preiss D, Jhund PS, et al. Risk related to pre-diabetes mellitus and diabetes mellitus in heart failure with reduced ejection fraction: insights from prospective comparison of ARNI with ACEI to determine impact on global mortality and morbidity in heart failure trial. Circ Heart Fail. 2016;9(1):e002560.
Lindman BR, Davila-Roman VG, Mann DL, et al. Cardiovascular phenotype in HFpEF patients with or without diabetes: a RELAX trial ancillary study. J Am Coll Cardiol. 2014;64(6):541–9.
Fousteris E, Melidonis A, Panoutsopoulos G, et al. Toll/interleukin-1 receptor member ST2 exhibits higher soluble levels in type 2 diabetes, especially when accompanied with left ventricular diastolic dysfunction. Cardiovasc Diabetol. 2011;10:101.
Ky B, French B, McCloskey K, et al. High-sensitivity ST2 for prediction of adverse outcomes in chronic heart failure. Circ Heart Fail. 2011;4(2):180–87.
AbouEzzeddine OF, McKie PM, Dunlay SM, et al. Suppression of tumorigenicity 2 in heart failure with preserved ejection fraction. J Am Heart Assoc. 2017;6(2):e004382.
Alonso N, Lupon J, Barallat J, et al. Impact of diabetes on the predictive value of heart failure biomarkers. Cardiovasc Diabetol. 2016;15(1):151.
de Boer RA, Edelmann F, Cohen-Solal A, Mamas MA, Maisel A, Pieske B. Galectin-3 in heart failure with preserved ejection fraction. Eur J Heart Fail. 2013;15(10):1095–101.
Paulus WJ, Dal Canto E. Distinct myocardial targets for diabetes therapy in heart failure with preserved or reduced ejection fraction. JACC Heart Fail. 2018;6(1):1–7.
Mohammed SF, Borlaug BA, Roger VL, et al. Comorbidity and ventricular and vascular structure and function in heart failure with preserved ejection fraction: a community-based study. Circ Heart Fail. 2012;5(6):710–9.
Shah AM, Shin SH, Takeuchi M, et al. Left ventricular systolic and diastolic function, remodelling, and clinical outcomes among patients with diabetes following myocardial infarction and the influence of direct renin inhibition with aliskiren. Eur J Heart Fail. 2012;14(2):185–92.
MacDonald MR, She L, Doenst T, et al. Clinical characteristics and outcomes of patients with and without diabetes in the Surgical Treatment for Ischemic Heart Failure (STICH) trial. Eur J Heart Fail. 2015;17(7):725–34.
Tanaka H, Tatsumi K, Matsuzoe H, Matsumoto K, Hirata KI. Impact of diabetes mellitus on left ventricular longitudinal function of patients with non-ischemic dilated cardiomyopathy. Cardiovasc Diabetol. 2020;19(1):84.
Wong TC, Piehler KM, Kang IA, et al. Myocardial extracellular volume fraction quantified by cardiovascular magnetic resonance is increased in diabetes and associated with mortality and incident heart failure admission. Eur Heart J. 2014;35(10):657–64.
Storz C, Hetterich H, Lorbeer R, et al. Myocardial tissue characterization by contrast-enhanced cardiac magnetic resonance imaging in subjects with prediabetes, diabetes, and normal controls with preserved ejection fraction from the general population. Eur Heart J Cardiovasc Imaging. 2018;19(6):701–8.
Paiman EHM, van Eyk HJ, Bizino MB, et al. Phenotyping diabetic cardiomyopathy in Europeans and South Asians. Cardiovasc Diabetol. 2019;18(1):133.
Levelt E, Mahmod M, Piechnik SK, et al. Relationship between left ventricular structural and metabolic remodeling in type 2 diabetes. Diabetes. 2016;65(1):44–52.
Rijzewijk LJ, van der Meer RW, Smit JW, et al. Myocardial steatosis is an independent predictor of diastolic dysfunction in type 2 diabetes mellitus. J Am Coll Cardiol. 2008;52(22):1793–9.
Larghat AM, Swoboda PP, Biglands JD, Kearney MT, Greenwood JP, Plein S. The microvascular effects of insulin resistance and diabetes on cardiac structure, function, and perfusion: a cardiovascular magnetic resonance study. Eur Heart J Cardiovasc Imaging. 2014;15(12):1368–76.
Korosoglou G, Humpert PM, Ahrens J, et al. Left ventricular diastolic function in type 2 diabetes mellitus is associated with myocardial triglyceride content but not with impaired myocardial perfusion reserve. J Magn Reson Imaging. 2012;35(4):804–11.
Dauriz M, Targher G, Temporelli PL, et al. Prognostic impact of diabetes and prediabetes on survival outcomes in patients with chronic heart failure: a post-hoc analysis of the GISSI-HF (Gruppo Italiano per lo Studio della Sopravvivenza nella Insufficienza Cardiaca-Heart Failure) Trial. J Am Heart Assoc. 2017;6(7):e005156.
MacDonald MR, Jhund PS, Petrie MC, et al. Discordant short- and long-term outcomes associated with diabetes in patients with heart failure: importance of age and sex. Circ Heart Fail. 2008;1(4):234–41.
Chandramouli C, Teng TK, Tay WT, et al. Impact of diabetes and sex in heart failure with reduced ejection fraction patients from the ASIAN-HF registry. Eur J Heart Fail. 2019;21(3):297–307.
Dunlay SM, Givertz MM, Aguilar D, et al. Type 2 diabetes mellitus and heart failure: a scientific statement from the American Heart Association and the Heart Failure Society of America: This statement does not represent an update of the 2017 ACC/AHA/HFSA heart failure guideline update. Circulation. 2019;140(7):e294–324.
Murcia AM, Hennekens CH, Lamas GA, et al. Impact of diabetes on mortality in patients with myocardial infarction and left ventricular dysfunction. Arch Intern Med. 2004;164(20):2273–9.
Gustafsson I, Torp-Pedersen C, Køber L, Gustafsson F, Hildebrandt P. Effect of the angiotensin-converting enzyme inhibitor trandolapril on mortality and morbidity in diabetic patients with left ventricular dysfunction after acute myocardial infarction. Trace Study Group. J Am Coll Cardiol. 1999;34(1):83–9.
Cohn JN, Tognoni G. A randomized trial of the angiotensin-receptor blocker valsartan in chronic heart failure. N Engl J Med. 2001;345(23):1667–75.
Pfeffer MA, McMurray JJ, Velazquez EJ, et al. Valsartan, captopril, or both in myocardial infarction complicated by heart failure, left ventricular dysfunction, or both. N Engl J Med. 2003;349(20):1893–906.
Brenner BM, Cooper ME, de Zeeuw D, et al. Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. N Engl J Med. 2001;345(12):861–9.
Eschalier R, McMurray JJ, Swedberg K, et al. Safety and efficacy of eplerenone in patients at high risk for hyperkalemia and/or worsening renal function: analyses of the EMPHASIS-HF study subgroups (Eplerenone in Mild Patients Hospitalization And SurvIval Study in Heart Failure). J Am Coll Cardiol. 2013;62(17):1585–93.
Komajda M, Tavazzi L, Francq BG, et al. Efficacy and safety of ivabradine in patients with chronic systolic heart failure and diabetes: an analysis from the SHIFT trial. Eur J Heart Fail. 2015;17(12):1294–301.
Shekelle PG, Rich MW, Morton SC, et al. Efficacy of angiotensin-converting enzyme inhibitors and beta-blockers in the management of left ventricular systolic dysfunction according to race, gender, and diabetic status. J Am Coll Cardiol. 2003;41(9):1529–38.
Bakris GL, Fonseca V, Katholi RE, et al. Metabolic effects of carvedilol vs metoprolol in patients with type 2 diabetes mellitus and hypertension: a randomized controlled trial. JAMA. 2004;292(18):2227–36.
Seferovic JP, Claggett B, Seidelmann SB, et al. Effect of sacubitril/valsartan versus enalapril on glycaemic control in patients with heart failure and diabetes: a post-hoc analysis from the PARADIGM-HF trial. Lancet Diabetes Endocrinol. 2017;5(5):333–40.
Wittenberg SM, Cook JR, Hall WJ, McNitt S, Zareba W, Moss AJ. Comparison of efficacy of implanted cardioverter-defibrillator in patients with versus without diabetes mellitus. Am J Cardiol. 2005;96(3):417–9.
Hoppe UC, Freemantle N, Cleland JG, Marijianowski M, Erdmann E. Effect of cardiac resynchronization on morbidity and mortality of diabetic patients with severe heart failure. Diabetes Care. 2007;30(3):722–4.
Ghali JK, Boehmer J, Feldman AM, et al. Influence of diabetes on cardiac resynchronization therapy with or without defibrillator in patients with advanced heart failure. J Cardiac Fail. 2007;13(9):769–73.
Martin DT, McNitt S, Nesto RW, Rutter MK, Moss AJ. Cardiac resynchronization therapy reduces the risk of cardiac events in patients with diabetes enrolled in the multicenter automatic defibrillator implantation trial with cardiac resynchronization therapy (MADIT-CRT). Circ Heart Fail. 2011;4(3):332–8.
Jarnert C, Landstedt-Hallin L, Malmberg K, et al. A randomized trial of the impact of strict glycaemic control on myocardial diastolic function and perfusion reserve: a report from the DADD (Diabetes mellitus And Diastolic Dysfunction) study. Eur J Heart Fail. 2009;11(1):39–47.
Lawson CA, Jones PW, Teece L, et al. Association between type 2 diabetes and all-cause hospitalization and mortality in the UK general heart failure population: stratification by diabetic glycemic control and medication intensification. JACC Heart Fail. 2018;6(1):18–26.
Eshaghian S, Horwich TB, Fonarow GC. An unexpected inverse relationship between HbA1c levels and mortality in patients with diabetes and advanced systolic heart failure. Am Heart J. 2006;151(1):91.
Cosentino F, Grant PJ, Aboyans V, et al. 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J. 2020;41(2):255–323.
Ceriello A, Monnier L, Owens D. Glycaemic variability in diabetes: clinical and therapeutic implications. Lancet Diabetes Endocrinol. 2019;7(3):221–30.
Segar MW, Patel KV, Vaduganathan M, et al. Association of long-term change and variability in glycemia with risk of incident heart failure among patients with type 2 diabetes: a secondary analysis of the ACCORD trial. Diabetes Care. 2020;43(8):1920–8.
Echouffo-Tcheugui JB, Zhao S, Brock G, Matsouaka RA, Kline D, Joseph JJ. Visit-to-visit glycemic variability and risks of cardiovascular events and all-cause mortality: the ALLHAT study. Diabetes Care. 2019;42(3):486–93.
Nicolucci A, Charbonnel B, Gomes MB, et al. Treatment patterns and associated factors in 14 668 people with type 2 diabetes initiating a second-line therapy: Results from the global DISCOVER study programme. Diabetes Obes Metab. 2019;21(11):2474–85.
Nathan DM, Buse JB, Davidson MB, et al. Management of hyperglycaemia in type 2 diabetes: a consensus algorithm for the initiation and adjustment of therapy. A consensus statement from the American Diabetes Association and the European Association for the Study of Diabetes. Diabetologia. 2006;49(8):1711–21.
Inzucchi SE, Masoudi FA, McGuire DK. Metformin in heart failure. Diabetes Care. 2007;30(12):e129.
Masoudi FA, Inzucchi SE, Wang Y, Havranek EP, Foody JM, Krumholz HM. Thiazolidinediones, metformin, and outcomes in older patients with diabetes and heart failure: an observational study. Circulation. 2005;111(5):583–90.
Eurich DT, Majumdar SR, McAlister FA, Tsuyuki RT, Johnson JA. Improved clinical outcomes associated with metformin in patients with diabetes and heart failure. Diabetes Care. 2005;28(10):2345–51.
Eurich DT, Weir DL, Majumdar SR, et al. Comparative safety and effectiveness of metformin in patients with diabetes mellitus and heart failure: systematic review of observational studies involving 34,000 patients. Circ Heart Fail. 2013;6(3):395–402.
Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37(27):2129–200.
Wiggers H, Køber L, Gislason G, et al. The DANish randomized, double-blind, placebo controlled trial in patients with chronic HEART failure (DANHEART): A 2 × 2 factorial trial of hydralazine-isosorbide dinitrate in patients with chronic heart failure (H-HeFT) and metformin in patients with chronic heart failure and diabetes or prediabetes (Met-HeFT). Am Heart J. 2021;231:137–46.
Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373(22):2117–28.
Neal B, Perkovic V, Mahaffey KW, et al. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med. 2017;377(7):644–57.
Wiviott SD, Raz I, Bonaca MP, et al. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2019;380(4):347–57.
Marx N, Davies MJ, Grant PJ, et al. Guideline recommendations and the positioning of newer drugs in type 2 diabetes care. Lancet Diabetes Endocrinol. 2021;9(1):46–52.
Cannon CP, Pratley R, Dagogo-Jack S, et al. Cardiovascular outcomes with Ertugliflozin in type 2 diabetes. N Engl J Med. 2020;383(15):1425–35.
Davies MJ, D'Alessio DA, Fradkin J, et al. Management of hyperglycemia in type 2 diabetes, 2018. A Consensus Report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2018;41(12):2669–701.
Ezekowitz JA, O’Meara E, McDonald MA, et al. 2017 Comprehensive Update of the Canadian Cardiovascular Society Guidelines for the Management of Heart Failure. Can J Cardiol. 2017;33(11):1342–433.
Chen TH, Li YR, Chen SW, et al. Sodium-glucose cotransporter 2 inhibitor versus metformin as first-line therapy in patients with type 2 diabetes mellitus: a multi-institution database study. Cardiovasc Diabetol. 2020;19(1):189.
Buse JB, Wexler DJ, Tsapas A, et al. 2019 Update to: management of hyperglycemia in type 2 diabetes, 2018. A Consensus Report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2020;43(2):487–93.
Pharmacologic approaches to glycemic treatment. standards of medical care in diabetes-2021. Diabetes Care. 2021;44(Suppl 1):S111-s124.
•• McMurray JJV, Solomon SD, Inzucchi SE, et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med. 2019;381(21):1995–2008. This study demonstrated that dapagliflozin reduced the risk of admitted HF or death from cardiovascular causes in patients with HFrEF despite optimal therapy, irrespective of DM.
•• Packer M, Anker SD, Butler J, et al. Empagliflozin in patients with heart failure, reduced ejection fraction, and volume overload: EMPEROR-reduced trial. J Am Coll Cardiol. 2021;77(11):1381–92. This study demonstrated that empagliflozin reduced the risk of cardiovascular death or HF hospitalization in patients with chronic HFrEF, regardless of DM.
Butt JH, Nicolau JC, Verma S, et al. Efficacy and safety of dapagliflozin according to aetiology in heart failure with reduced ejection fraction: insights from the DAPA-HF trial. Eur J Heart Fail. 2021;23(4):601–13.
Packer M, Anker SD, Butler J, et al. Influence of neprilysin inhibition on the efficacy and safety of empagliflozin in patients with chronic heart failure and a reduced ejection fraction: the EMPEROR-Reduced trial. Eur Heart J. 2021;42(6):671–80.
Verma S, McGuire DK, Kosiborod MN. Two tales: one story: EMPEROR-reduced and DAPA-HF. Circulation. 2020;142(23):2201–4.
Zannad F, Ferreira JP, Pocock SJ, et al. SGLT2 inhibitors in patients with heart failure with reduced ejection fraction: a meta-analysis of the EMPEROR-Reduced and DAPA-HF trials. The Lancet. 2020;396(10254):819–29.
Kosiborod MN, Jhund PS, Docherty KF, et al. Effects of dapagliflozin on symptoms, function, and quality of life in patients with heart failure and reduced ejection fraction: results from the DAPA-HF trial. Circulation. 2020;141(2):90–9.
Nassif ME, Windsor SL, Tang F, et al. Dapagliflozin effects on biomarkers, symptoms, and functional status in patients with heart failure with reduced ejection fraction: The DEFINE-HF Trial. Circulation. 2019;140(18):1463–76.
Nassif ME, Windsor SL, Tang F, et al. Dapagliflozin effects on lung fluid volumes in patients with heart failure and reduced ejection fraction: Results from the DEFINE-HF trial. Diabetes Obes Metab. 2021;23(6):1426–30.
Ibrahim A, Ghaleb R, Mansour H, et al. Safety and efficacy of adding dapagliflozin to furosemide in type 2 diabetic patients with decompensated heart failure and reduced ejection fraction. Front Cardiovasc Med. 2020;7:602251.
Tamaki S, Yamada T, Watanabe T, et al. Effect of empagliflozin as an add-on therapy on decongestion and renal function in patients with diabetes hospitalized for acute decompensated heart failure: a prospective randomized controlled study. Circ Heart Fail. 2021;14(3):e007048.
Bhatt DL, Szarek M, Steg PG, et al. Sotagliflozin in patients with diabetes and recent worsening heart failure. N Engl J Med. 2021;384(2):117–28.
Damman K, Beusekamp JC, Boorsma EM, et al. Randomized, double-blind, placebo-controlled, multicentre pilot study on the effects of empagliflozin on clinical outcomes in patients with acute decompensated heart failure (EMPA-RESPONSE-AHF). Eur J Heart Fail. 2020;22(4):713–22.
Zeng Q, Zhou Q, Liu W, Wang Y, Xu X, Xu D. Mechanisms and perspectives of sodium-glucose co-transporter 2 inhibitors in heart failure. Front Cardiovasc Med. 2021;8:636152.
Bauersachs J. Heart failure drug treatment: the fantastic four. Eur Heart J. 2021;42(6):681–3.
Kosiborod M, Cavender MA, Fu AZ, et al. Lower risk of heart failure and death in patients initiated on sodium-glucose cotransporter-2 inhibitors versus other glucose-lowering drugs: the CVD-REAL study (comparative effectiveness of cardiovascular outcomes in new users of sodium-glucose cotransporter-2 inhibitors). Circulation. 2017;136(3):249–59.
Kosiborod M, Lam CSP, Kohsaka S, et al. Cardiovascular events associated with SGLT-2 inhibitors versus other glucose-lowering drugs: the CVD-REAL 2 study. J Am Coll Cardiol. 2018;71(23):2628–39.
Funck KL, Knudsen JS, Hansen TK, Thomsen RW, Grove EL. Real-world use of cardioprotective glucose-lowering drugs in patients with type 2 diabetes and cardiovascular disease: a Danish nationwide cohort study, 2012 to 2019. Diabetes Obes Metab. 2021;23(2):520–9.
Hamid A, Vaduganathan M, Oshunbade AA, et al. Antihyperglycemic therapies with expansions of US Food and Drug Administration indications to reduce cardiovascular events: prescribing patterns within an academic medical center. J Cardiovasc Pharmacol. 2020;76(3):313–20.
Vaduganathan M, Greene SJ, Zhang S, et al. Applicability of US Food and Drug Administration labeling for dapagliflozin to patients with heart failure with reduced ejection fraction in US clinical practice: the get with the guidelines-heart failure (GWTG-HF) registry. JAMA Cardiol. 2020;6(3):1–10.
Loutradis C, Papadopoulou E, Theodorakopoulou M, Karagiannis A, Sarafidis P. The effect of SGLT-2 inhibitors on blood pressure: a pleiotropic action favoring cardio- and nephroprotection. Future Med Chem. 2019;11(11):1285–303.
Uthman L, Baartscheer A, Bleijlevens B, et al. Class effects of SGLT2 inhibitors in mouse cardiomyocytes and hearts: inhibition of Na(+)/H(+) exchanger, lowering of cytosolic Na(+) and vasodilation. Diabetologia. 2018;61(3):722–6.
Lin YW, Chen CY, Shih JY, et al. Dapagliflozin improves cardiac hemodynamics and mitigates arrhythmogenesis in mitral regurgitation-induced myocardial dysfunction. J Am Heart Assoc. 2021;10(7):e019274.
Galli M, D’Amario D, Sofia C, Vaccarella M, Crea F, Aspromonte N. Clinical potential relevance of metabolic properties of SGLT2 inhibitors in patients with heart failure. Expert Opin Drug Metab Toxicol. 2018;14(12):1273–85.
Writing C, Maddox TM, Januzzi JL, Jr., et al. 2021 Update to the 2017 ACC expert consensus decision pathway for optimization of heart failure treatment: answers to 10 pivotal issues about heart failure with reduced ejection fraction: a report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2021;77(6):772–810.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Global Cardiovascular Health
Rights and permissions
About this article
Cite this article
Zhang, Q., Kang, Y., Tang, S. et al. Intersection Between Diabetes and Heart Failure: Is SGLT2i the “One Stone for Two Birds” Approach?. Curr Cardiol Rep 23, 171 (2021). https://doi.org/10.1007/s11886-021-01591-3
Accepted:
Published:
DOI: https://doi.org/10.1007/s11886-021-01591-3