Abstract
Purpose of Review
The objective of this review is to shed light on the transformative potential of machine learning (ML) in coronary angiography. We aim to understand existing developments in using ML for coronary angiography and discuss broader implications for the future of coronary angiography and cardiovascular medicine.
Recent Findings
The developments in invasive and noninvasive imaging have revolutionized diagnosis and treatment of coronary artery disease (CAD). However, CAD remains underdiagnosed and undertreated. ML has emerged as a powerful tool to further improve image analysis, hemodynamic assessment, lesion detection, and predictive modeling. These advancements have enabled more accurate identification of CAD, streamlined workflows, reduced the need for invasive diagnostic procedures, and improved the diagnostic value of invasive procedures when they are needed. Further integration of ML with coronary angiography will advance the prevention, diagnosis, and treatment of CAD.
Summary
The integration of ML with coronary angiography is ushering in a new era in cardiovascular medicine. We highlight five use cases to leverage ML in coronary angiography: (1) improvement of quality and efficacy, (2) characterization of plaque, (3) hemodynamic assessment, (4) prediction of future outcomes, and (5) diagnosis of non-atherosclerotic coronary disease.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: Update From the GBD 2019 Study. J Am Coll Cardiol. 2020;76(25):2982–3021. https://doi.org/10.1016/j.jacc.2020.11.010.
Stone GW, Maehara A, Lansky AJ, de Bruyne B, Cristea E, Mintz GS, et al. A prospective natural-history study of coronary atherosclerosis. N Engl J Med. 2011;364(3):226–35. https://doi.org/10.1056/NEJMoa1002358.
Davies JE, Sen S, Dehbi HM, Al-Lamee R, Petraco R, Nijjer SS, et al. Use of the instantaneous wave-free ratio or fractional flow reserve in PCI. N Engl J Med. 2017;376(19):1824–34. https://doi.org/10.1056/NEJMoa1700445.
Nørgaard BL, Leipsic J, Gaur S, Seneviratne S, Ko BS, Ito H, et al. Diagnostic performance of noninvasive fractional flow reserve derived from coronary computed tomography angiography in suspected coronary artery disease: the NXT trial (Analysis of Coronary Blood Flow Using CT Angiography: Next Steps). J Am Coll Cardiol. 2014;63(12):1145–55. https://doi.org/10.1016/j.jacc.2013.11.043.
Taylor CA, Fonte TA, Min JK. Computational fluid dynamics applied to cardiac computed tomography for noninvasive quantification of fractional flow reserve: scientific basis. J Am Coll Cardiol. 2013;61(22):2233–41. https://doi.org/10.1016/j.jacc.2012.11.083.
Miller JM, Rochitte CE, Dewey M, Arbab-Zadeh A, Niinuma H, Gottlieb I, et al. Diagnostic performance of coronary angiography by 64-row CT. N Engl J Med. 2008;359(22):2324–36. https://doi.org/10.1056/NEJMoa0806576.
Williams MC, Moss AJ, Dweck M, Adamson PD, Alam S, Hunter A, et al. Coronary artery plaque characteristics associated with adverse outcomes in the SCOT-HEART study. J Am Coll Cardiol. 2019;73(3):291–301. https://doi.org/10.1016/j.jacc.2018.10.066.
Johnson KW, Torres Soto J, Glicksberg BS, Shameer K, Miotto R, Ali M, et al. Artificial intelligence in cardiology. J Am Coll Cardiol. 2018;71(23):2668–79. https://doi.org/10.1016/j.jacc.2018.03.521.
Budoff MJ, Dowe D, Jollis JG, Gitter M, Sutherland J, Halamert E, et al. Diagnostic performance of 64-multidetector row coronary computed tomographic angiography for evaluation of coronary artery stenosis in individuals without known coronary artery disease: results from the prospective multicenter ACCURACY (Assessment by Coronary Computed Tomographic Angiography of Individuals Undergoing Invasive Coronary Angiography) trial. J Am Coll Cardiol. 2008;52(21):1724–32. https://doi.org/10.1016/j.jacc.2008.07.031.
Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, et al. Heart disease and stroke statistics-2019 update: a report from the American Heart Association. Circulation. 2019;139(10):e56–528. https://doi.org/10.1161/cir.0000000000000659.
Jonas RA, Weerakoon S, Fisher R, Griffin WF, Kumar V, Rahban H, et al. Interobserver variability among expert readers quantifying plaque volume and plaque characteristics on coronary CT angiography: a CLARIFY trial sub-study. Clin Imaging. 2022;91:19–25. https://doi.org/10.1016/j.clinimag.2022.08.005. Findings from this study highlights the subjectivity and inherent variability of coronary computer tomography angiography evaluations.
Zhang H, Mu L, Hu S, Nallamothu BK, Lansky AJ, Xu B, et al. Comparison of physician visual assessment with quantitative coronary angiography in assessment of stenosis severity in China. JAMA Intern Med. 2018;178(2):239–47. https://doi.org/10.1001/jamainternmed.2017.7821.
Priest VL, Scuffham PA, Hachamovitch R, Marwick TH. Cost-effectiveness of coronary computed tomography and cardiac stress imaging in the emergency department: a decision analytic model comparing diagnostic strategies for chest pain in patients at low risk of acute coronary syndromes. JACC Cardiovasc Imaging. 2011;4(5):549–56. https://doi.org/10.1016/j.jcmg.2011.03.008.
Litjens G, Sánchez CI, Timofeeva N, Hermsen M, Nagtegaal I, Kovacs I, et al. Deep learning as a tool for increased accuracy and efficiency of histopathological diagnosis. Sci Rep. 2016;6:26286. https://doi.org/10.1038/srep26286.
Chilamkurthy S, Ghosh R, Tanamala S, Biviji M, Campeau NG, Venugopal VK, et al. Deep learning algorithms for detection of critical findings in head CT scans: a retrospective study. Lancet. 2018;392(10162):2388–96. https://doi.org/10.1016/s0140-6736(18)31645-3.
Lansberg MG, Christensen S, Kemp S, Mlynash M, Mishra N, Federau C, et al. Computed tomographic perfusion to predict response to recanalization in ischemic stroke. Ann Neurol. 2017;81(6):849–56. https://doi.org/10.1002/ana.24953.
Esteva A, Kuprel B, Novoa RA, Ko J, Swetter SM, Blau HM, et al. Dermatologist-level classification of skin cancer with deep neural networks. Nature. 2017;542(7639):115–8. https://doi.org/10.1038/nature21056.
Gulshan V, Peng L, Coram M, Stumpe MC, Wu D, Narayanaswamy A, et al. Development and validation of a deep learning algorithm for detection of diabetic retinopathy in retinal fundus photographs. JAMA. 2016;316(22):2402–10. https://doi.org/10.1001/jama.2016.17216.
Al’Aref SJ, Anchouche K, Singh G, Slomka PJ, Kolli KK, Kumar A, et al. Clinical applications of machine learning in cardiovascular disease and its relevance to cardiac imaging. Eur Heart J. 2019;40(24):1975–86. https://doi.org/10.1093/eurheartj/ehy404.
Kang D, Dey D, Slomka PJ, Arsanjani R, Nakazato R, Ko H, et al. Structured learning algorithm for detection of nonobstructive and obstructive coronary plaque lesions from computed tomography angiography. J Med Imaging (Bellingham). 2015;2(1):014003. https://doi.org/10.1117/1.Jmi.2.1.014003.
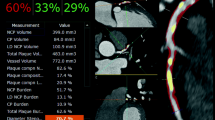
Lin A, Manral N, McElhinney P, Killekar A, Matsumoto H, Kwiecinski J, et al. Deep learning-enabled coronary CT angiography for plaque and stenosis quantification and cardiac risk prediction: an international multicentre study. Lancet Digit Health. 2022;4(4):e256–65. https://doi.org/10.1016/s2589-7500(22)00022-x. In this international, multicenter study, a comprehensive and externally validated machine learning model was developed for rapid measurements of plaque volume and stenosis. It demonstrated that the model agreed closely with the expert readers but was more consistent and significantly faster.
Madani A, Arnaout R, Mofrad M, Arnaout R. Fast and accurate view classification of echocardiograms using deep learning. NPJ Digit Med. 2018;1. https://doi.org/10.1038/s41746-017-0013-1
van Rosendael AR, Maliakal G, Kolli KK, Beecy A, Al’Aref SJ, Dwivedi A, et al. Maximization of the usage of coronary CTA derived plaque information using a machine learning based algorithm to improve risk stratification; insights from the CONFIRM registry. J Cardiovasc Comput Tomogr. 2018;12(3):204–9. https://doi.org/10.1016/j.jcct.2018.04.011.
Shen D, Wu G, Suk HI. Deep learning in medical image analysis. Annu Rev Biomed Eng. 2017;19:221–48. https://doi.org/10.1146/annurev-bioeng-071516-044442.
Liu F, Jang H, Kijowski R, Bradshaw T, McMillan AB. Deep learning MR imaging-based attenuation correction for PET/MR imaging. Radiology. 2018;286(2):676–84. https://doi.org/10.1148/radiol.2017170700.
Wang G, Li W, Ourselin S, Vercauteren T. Automatic brain tumor segmentation based on cascaded convolutional neural networks with uncertainty estimation. Front Comput Neurosci. 2019;13:56. https://doi.org/10.3389/fncom.2019.00056.
Douglas PS, Hoffmann U, Patel MR, Mark DB, Al-Khalidi HR, Cavanaugh B, et al. Outcomes of anatomical versus functional testing for coronary artery disease. N Engl J Med. 2015;372(14):1291–300. https://doi.org/10.1056/NEJMoa1415516.
De la Garza-Salazar F, Lankenau-Vela DL, Cadena-Nuñez B, González-Cantú A, Romero-Ibarguengoitia ME. The effect of functional and intra-coronary imaging techniques on fluoroscopy time, radiation dose and contrast volume during coronary angiography. Sci Rep. 2020;10(1):6950. https://doi.org/10.1038/s41598-020-63791-1.
Koskinas KC, Nakamura M, Räber L, Colleran R, Kadota K, Capodanno D, et al. Current use of intracoronary imaging in interventional practice - results of a European Association of Percutaneous Cardiovascular Interventions (EAPCI) and Japanese Association of Cardiovascular Interventions and Therapeutics (CVIT) Clinical Practice Survey. EuroIntervention. 2018;14(4):e475–84. https://doi.org/10.4244/eijy18m03_01.
Dey D, Gaur S, Ovrehus KA, Slomka PJ, Betancur J, Goeller M, et al. Integrated prediction of lesion-specific ischaemia from quantitative coronary CT angiography using machine learning: a multicentre study. Eur Radiol. 2018;28(6):2655–64. https://doi.org/10.1007/s00330-017-5223-z.
Jia H, Dai J, Hou J, Xing L, Ma L, Liu H, et al. Effective anti-thrombotic therapy without stenting: intravascular optical coherence tomography-based management in plaque erosion (the EROSION study). Eur Heart J. 2017;38(11):792–800. https://doi.org/10.1093/eurheartj/ehw381.
Krittanawong C, Zhang H, Wang Z, Aydar M, Kitai T. Artificial intelligence in precision cardiovascular medicine. J Am Coll Cardiol. 2017;69(21):2657–64. https://doi.org/10.1016/j.jacc.2017.03.571.
Fahed AC, Jang IK. Plaque erosion and acute coronary syndromes: phenotype, molecular characteristics and future directions. Nat Rev Cardiol. 2021;18(10):724–34. https://doi.org/10.1038/s41569-021-00542-3.
Motwani M, Dey D, Berman DS, Germano G, Achenbach S, Al-Mallah MH, et al. Machine learning for prediction of all-cause mortality in patients with suspected coronary artery disease: a 5-year multicentre prospective registry analysis. Eur Heart J. 2017;38(7):500–7. https://doi.org/10.1093/eurheartj/ehw188.
Tonino PA, De Bruyne B, Pijls NH, Siebert U, Ikeno F, van’t Veer M, et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med. 2009;360(3):213–24. https://doi.org/10.1056/NEJMoa0807611.
Douglas PS, De Bruyne B, Pontone G, Patel MR, Norgaard BL, Byrne RA, et al. 1-year outcomes of FFRCT-guided care in patients with suspected coronary disease: the PLATFORM study. J Am Coll Cardiol. 2016;68(5):435–45. https://doi.org/10.1016/j.jacc.2016.05.057.
Cho H, Lee JG, Kang SJ, Kim WJ, Choi SY, Ko J, et al. Angiography-based machine learning for predicting fractional flow reserve in intermediate coronary artery lesions. J Am Heart Assoc. 2019;8(4):e011685. https://doi.org/10.1161/jaha.118.011685.
Kogame N, Ono M, Kawashima H, Tomaniak M, Hara H, Leipsic J, et al. The impact of coronary physiology on contemporary clinical decision making. JACC Cardiovasc Interv. 2020;13(14):1617–38. https://doi.org/10.1016/j.jcin.2020.04.040.
Detrano R, Guerci AD, Carr JJ, Bild DE, Burke G, Folsom AR, et al. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med. 2008;358(13):1336–45. https://doi.org/10.1056/NEJMoa072100.
Kral BG, Becker LC, Vaidya D, Yanek LR, Qayyum R, Zimmerman SL, et al. Noncalcified coronary plaque volumes in healthy people with a family history of early onset coronary artery disease. Circ Cardiovasc Imaging. 2014;7(3):446–53. https://doi.org/10.1161/circimaging.113.000980.
Nakanishi R, Slomka PJ, Rios R, Betancur J, Blaha MJ, Nasir K, et al. Machine learning adds to clinical and CAC assessments in predicting 10-year CHD and CVD deaths. JACC Cardiovasc Imaging. 2021;14(3):615–25. https://doi.org/10.1016/j.jcmg.2020.08.024. This study demonstrated that a machine learning model was superior in predicting cardiovascular disease and coronary heart disease related mortality compared to existing prediction tools including atherosclerotic cardiovascular disease risk calculators and coronary artery calcium score.
Hayes SN, Kim ESH, Saw J, Adlam D, Arslanian-Engoren C, Economy KE, et al. Spontaneous coronary artery dissection: current state of the science: a scientific statement from the American Heart Association. Circulation. 2018;137(19):e523–57. https://doi.org/10.1161/cir.0000000000000564.
Tweet MS, Hayes SN, Pitta SR, Simari RD, Lerman A, Lennon RJ, et al. Clinical features, management, and prognosis of spontaneous coronary artery dissection. Circulation. 2012;126(5):579–88. https://doi.org/10.1161/circulationaha.112.105718.
Alfonso F, Paulo M, Lennie V, Dutary J, Bernardo E, Jiménez-Quevedo P, et al. Spontaneous coronary artery dissection: long-term follow-up of a large series of patients prospectively managed with a “conservative” therapeutic strategy. JACC Cardiovasc Interv. 2012;5(10):1062–70. https://doi.org/10.1016/j.jcin.2012.06.014.
Costanzo MR, Dipchand A, Starling R, Anderson A, Chan M, Desai S, et al. The International Society of Heart and Lung Transplantation Guidelines for the care of heart transplant recipients. J Heart Lung Transplant. 2010;29(8):914–56. https://doi.org/10.1016/j.healun.2010.05.034.
Mehra MR, Crespo-Leiro MG, Dipchand A, Ensminger SM, Hiemann NE, Kobashigawa JA, et al. International Society for Heart and Lung Transplantation working formulation of a standardized nomenclature for cardiac allograft vasculopathy-2010. J Heart Lung Transplant. 2010;29(7):717–27. https://doi.org/10.1016/j.healun.2010.05.017.
Del Buono MG, Montone RA, Camilli M, Carbone S, Narula J, Lavie CJ, et al. Coronary microvascular dysfunction across the spectrum of cardiovascular diseases: JACC state-of-the-art review. J Am Coll Cardiol. 2021;78(13):1352–71. https://doi.org/10.1016/j.jacc.2021.07.042.
Marinescu MA, Löffler AI, Ouellette M, Smith L, Kramer CM, Bourque JM. Coronary microvascular dysfunction, microvascular angina, and treatment strategies. JACC Cardiovasc Imaging. 2015;8(2):210–20. https://doi.org/10.1016/j.jcmg.2014.12.008.
Mathew RC, Bourque JM, Salerno M, Kramer CM. Cardiovascular imaging techniques to assess microvascular dysfunction. JACC Cardiovasc Imaging. 2020;13(7):1577–90. https://doi.org/10.1016/j.jcmg.2019.09.006.
Ford TJ, Stanley B, Sidik N, Good R, Rocchiccioli P, McEntegart M, et al. 1-year outcomes of angina management guided by invasive coronary function testing (CorMicA). JACC Cardiovasc Interv. 2020;13(1):33–45. https://doi.org/10.1016/j.jcin.2019.11.001.
Topol EJ. High-performance medicine: the convergence of human and artificial intelligence. Nat Med. 2019;25(1):44–56. https://doi.org/10.1038/s41591-018-0300-7.
Obermeyer Z, Emanuel EJ. Predicting the future - big data, machine learning, and clinical medicine. N Engl J Med. 2016;375(13):1216–9. https://doi.org/10.1056/NEJMp1606181.
Brisimi TS, Chen R, Mela T, Olshevsky A, Paschalidis IC, Shi W. Federated learning of predictive models from federated electronic health records. Int J Med Inform. 2018;112:59–67. https://doi.org/10.1016/j.ijmedinf.2018.01.007.
Castelvecchi D. Can we open the black box of AI? Nature. 2016;538(7623):20–3. https://doi.org/10.1038/538020a.
Simonyan K, Vedaldi A, Zisserman A. Deep inside convolutional networks: visualising image classification models and saliency maps. 2013. https://doi.org/10.48550/arXiv.1312.6034
Zhou B, Khosla A, Lapedriza A, Oliva A, Torralba A. Learning deep features for discriminative localization. 2016 IEEE Conference on Computer Vision and Pattern Recognition (CVPR)2016. p. 2921–9.
Olah C, Mordvintsev A, Schubert L. Feature Visualization. Distill. https://doi.org/10.23915/distill.00007
McGovern A, Lagerquist R, John Gagne D, Jergensen GE, Elmore KL, Homeyer CR, et al. Making the black box more transparent: understanding the physical implications of machine learning. Bull Am Meteor Soc. 2019;100(11):2175–99. https://doi.org/10.1175/BAMS-D-18-0195.1.
Wagstaff KL, Lee J. Interpretable discovery in large image data sets. 2018. https://doi.org/10.48550/arXiv.1806.08340
Funding
Dr. Unlu receives funding from the National Heart Lung and Blood Institute under award number T32HL007604. Dr. Fahed receives funding from the National Heart Lung and Blood Institute under award numbers K08 HL161448 and R01 HL164629.
Author information
Authors and Affiliations
Contributions
O.U. and A.C.F conceptualized and wrote the main manuscript text and prepared tables and figures.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of Interest
Dr. Fahed reports being co-founder of Goodpath and received a research grant from Abbott Vascular, unrelated to the subject of this manuscript. Dr. Unlu has nothing to disclose.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Unlu, O., Fahed, A.C. Machine Learning in Invasive and Noninvasive Coronary Angiography. Curr Atheroscler Rep 25, 1025–1033 (2023). https://doi.org/10.1007/s11883-023-01178-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11883-023-01178-z