Abstract
The nature and airborne dispersion of the underestimated biological agents, monitoring, analysis and transmission among the human occupants into building environment is a major challenge of today. Those agents play a crucial role in ensuring comfortable, healthy and risk-free conditions into indoor working and leaving spaces. It is known that ventilation systems influence strongly the transmission of indoor air pollutants, with scarce information although to have been reported for biological agents until 2019. The biological agents’ source release and the trajectory of airborne transmission are both important in terms of optimising the design of the heating, ventilation and air conditioning systems of the future. In addition, modelling via computational fluid dynamics (CFD) will become a more valuable tool in foreseeing risks and tackle hazards when pollutants and biological agents released into closed spaces. Promising results on the prediction of their dispersion routes and concentration levels, as well as the selection of the appropriate ventilation strategy, provide crucial information on risk minimisation of the airborne transmission among humans. Under this context, the present multidisciplinary review considers four interrelated aspects of the dispersion of biological agents in closed spaces, (a) the nature and airborne transmission route of the examined agents, (b) the biological origin and health effects of the major microbial pathogens on the human respiratory system, (c) the role of heating, ventilation and air-conditioning systems in the airborne transmission and (d) the associated computer modelling approaches. This adopted methodology allows the discussion of the existing findings, on-going research, identification of the main research gaps and future directions from a multidisciplinary point of view which will be helpful for substantial innovations in the field.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Release, circulation and dispersion of chemical (harmful pollutants) and biological agents within confined indoor spaces can be easily inhaled. For that reason, it is considered a serious threat for public health and therefore there is a continuous effort for preventing or controlling their release (Jones 1999). Such agents may include from toxic chemicals, pathogenic microorganisms (e.g. fungal and bacterial spores) and microbe-bearing air particles, such as droplets to various types of solids such as dust (Ghosh et al. 2015). Those are responsible for chemical poisoning or serious respiratory infections via the spread of infectious biological agents at hospitals, long-term care facilities (Vogazianos et al. 2021), schools and office areas (Taylor et al. 2012). The main route of human infection by biological agents is usually via the human respiratory system. This takes place by inhalation of tiny particles or droplets, commonly referred as particulates, however, in the case of pathogens those can be also contracted from touching infected surfaces, such as door handles, taps and furniture (Madigan 2009; Prat and Lacoma 2016).
The shape, size and formation–dispersion mechanisms of these particulates when especially are in a liquid place (droplets) as well as their physicochemical properties affect significantly their potential to cause respiratory diseases. Those characteristics determine biological agents transmission patterns and how easy it is to be inserted into the human body via inhalation and further penetrating into the tissues of the lower respiratory system. Usually, only the micron-sized particulates can reach our lungs and the alveoli, leading to serious respiratory diseases (Bansal et al. 2018; Jones 1999). More information on which particle/droplet sizes are deposited in which part of the human respiratory tract, depending on the nature of the particulates, can be found in the following sections.
New respiratory pathogens have emerged during the last couple of years, with the most notorious being SARS-CoV-2, a novel coronavirus which is responsible for the infectious disease COVID-19 that has caused more than a million of deaths worldwide in 2019–2020 according to Rothan and Byrareddy (2020). Another coronavirus, MERS (Middle East respiratory syndrome), also caused many deaths in the Middle East in 2017 (Hageman 2020).
In addition, traditional pulmonary infectious agents, such as influenza virus (causing common flu), Streptococcus pneumoniae (causing pneumonia), Mycobacterium tuberculosis (causing tuberculosis) and Aspergillus fumigatus (causing lung aspergillosis) are still considered major health hazards (Hunter 2016; Latgé and Chamilos 2019; Murray et al., 2013; Pleschka 2013).
In order to rapidly detect and identify these infectious biological agents in the air or on surfaces, an arsenal of sophisticated new technologies is necessary to be developed. Those technologies will provide real-time accurate information about the presence of particulates in an indoor environment. Several such approaches have been developed (Huffman et al. 2020; Nasir et al. 2019; Usachev et al. 2013); however, most of them are still at low technology readiness level, an experimental level, and they are not routinely applied.
In addition, Heating, Ventilation and Air-Conditioning (HVAC) systems can be employed to control the transmission of harmful particles (solids or droplets). Different types of HVAC methods can reduce the spread of such agents in buildings or even eliminate the threat posed by pathogenic infectious microorganisms (Li et al. 2007); Shajahan et al. 2019).
Also, factors like the ventilation rate and heating/cooling settings of such systems can significantly influence the indoor transmission of hazardous agents (Li et al. 2007; Zhang et al. 2020a, b, c, d).
Moreover, computer modelling approaches have been used for predicting transmission patterns of chemical and biological agents in confined indoor areas. The most predominant methods are multi-zone and CFD modelling that are often used in combination for obtaining more robust results (Wang and Chen 2008a). Numerous such studies have been carried out in key close space areas such as hospitals and offices and have helped in designing new effective sanitation approaches (Chen et al. 2011; Emmerich et al. 2013; Karakitsios et al. 2020; Lim et al. 2011).
The aim of this multidisciplinary review is to examine the critical issue of harmful particles control, with the emphasis drawn on biological agents, within indoor environments from four different angles (physical, biological, HVAC and computer modelling), highlighting key research gaps in each area and suggest solutions that could lead to substantially improved indoor health strategies in the near future.
This manuscript is organised in seven sections. The ‘Introduction’ section presents a short introduction to the reviewed topic. The ‘Methods–literature review approach’ section includes the classification of the present review and methodology of the collection and analysis of the relevant research works in the field. In the ‘Droplet formation mechanisms’ section, the effect of the physicochemical nature (chemical characteristics, size and shape) of particulates such as dust and droplets of water, the most characteristic formation mechanisms of droplets and aerosols and their dispersion into indoor space environment are discussed. The ‘Aerosols and bioaerosols’ section includes the most characteristic microbiological agents that are carried within aerosols with an account on the methods that are currently used for their detection and identification. In the ‘The role of heating, ventilation and air-conditioning systems’ section, the role of heating, ventilation and air-conditioning (HVAC) systems in association with the alternative ventilation patterns regarding the dispersion of pollutants and biological agents into indoor spaces is presented. The ‘Computer modelling of particles and biological agents’ airborne transmission into indoor built environment’ section exhibits the available computational modelling techniques for the prediction of biological agents’ airborne transmission routes. Finally, in the ‘Conclusions—future directions’ section, the major findings, remarks and recommendations for future research are presented.
Methods—literature review approach
The present review is classified as a semi-systematic review, designed for the topic of dispersion of biological agents and pollutants in indoor air environments. This type of literature review studies is suitable for works of multidisciplinary group of researchers within diverse disciplines of engineering and other sciences as described in (Snyder 2019). The adopted literature review strategy focused on how the research in the field of the indoor air pollutants of biological origin, the latest often underestimated, has progressed and developed over time. The authors attempt to identify the potentially relevant research aspects which are important for the corresponding topic and synthesise these instead of measuring effect size, by using meta-narratives.
The importance of contribution of the present work is (a) mapping the recent trends of biological agents and pollutant dispersion in the indoor air research, (b) synthesize the current status of knowledge from different perspectives of a variety of disciplines and (c) create an updated agenda for further multidisciplinary research on the topic of indoor air pollution from biological agents, the main focus of this study, in which the current literature is scarce.
The research methodology used in the present semi-systematic review is composed of three primary and independent steps:
-
Step 1: Database selection. Scopus, Google Scholar, PubMed, Web of Science and database platforms were used to retrieve the relevant literature related to the scope of the study.
-
Step 2: Searching Keywords. Due to the multidisciplinary context of this work, four different keyword families were used to identify the relevant articles per section. In the ‘Droplet formation mechanisms’ section, the words “particles”, “particulates”, “size”, “shape”, “indoor air pollution”, transmission”, “dispersion droplets”, “formation”, “technology”, “mechanism”, “suspension”, “re-suspension”, “particle size distribution”, “atomisation” and “coalescence”, as well as any combination among them, was used. The research works found were further narrowed down to the engineering aspects of the particles and droplets formation and airborne dispersion in the field of indoor air quality. In the ‘Aerosols and bioaerosols’ section, the names of the microbial agents and the relevant methods were used as keywords, in addition to biomedical terms such as “bio-aerosols”, “dust”, “pollen”, “transmission”, “air microbiology”, “microbial identification”, “airborne disease”, “respiratory disease”, “lung infection”, “infectious dose” and “immunity”, used to identify the relevant articles. The terms “ventilation”, “natural ventilation”, “personal ventilation”, “mixed ventilation”, “underfloor ventilation”, “mechanical ventilation”, “air distribution” and combined with the Boolean operators “OR” and “AND” with the associated terms “airborne transmission”, “thermal plume”, “droplet”, “contaminant removal efficiency” “heating”, “cooling” and “bioaerosol” were adopted in the ‘The role of heating, ventilation and air-conditioning systems’ section. In the ‘Computer modelling of particles and biological agents’ airborne transmission into indoor built environment’ section, regarding turbulence, modelling techniques terms such as “Reynolds-Averaged Navier–Stokes (RANS)”, “Unsteady Reynolds-Averaged Navier–Stokes (URANS)”, “Detached Eddy Simulation (DES)”, “Reynolds stress models (RSM)” and “Large Eddy Simulation (LES)” were used, in addition, to terms such as “indoor dispersion”, “dilution” “multiphase flows”, “Eulerian–Lagrangian techniques”, “Eulerian-Eulerian techniques”, multizone models”, “CFD—Physiologically Based Pharmacokinetic (PBPK)” or “CFD—Physiologically Based Toxicokinetic (PBTK)”. Furthermore, the combination of the aforementioned terms/ keywords from the ‘Droplet formation mechanisms’ and ‘‘Aerosols and bioaerosols’ sections along with “CFD” was also used to identify relevant papers.
-
Step 3: Article screening and reviewing. Articles were preliminary analysed through title, keywords, abstract and conclusions. This analysis was later on followed by an extensive reviewing of the articles selected from the screening process. The available material is certainly too much to be reviewed in a single paper. For this reason, regarding the modelling papers, the authors give special attention to what they consider the better established or more promising modelling approaches, such as single- and multi-zone models, CFD, coupling of CFD and multi-zone models, CFD-PKTE or CFD-PTBK models. No disrespect is therefore implied for studies with other models. It should be noted that extensive use has been made of the published literature on the field and of previous reviews.
Droplet formation mechanisms
The challenging nature of biological agents’ transmission in indoor environment
The importance of indoor air quality (IAQ) and spreading of pollutants and biological agents into indoor air, ranges from new types of chemicals and particulates released to infectious droplets spreading several kinds of diseases, and those are well known threats for the societies (Brundage et al. 1988; Cooke 1991; Jones 1999; Mutuku et al. 2020a). At the opening of the twentieth century (1918–2019), the outbreak of Spanish flu (H1N1) caused more than 1 billion infections and was then considered as the most lethal flu pandemic. Recently, Ni et al. (2020) reported that people spend approximately 90% of their time indoors with minimum time for outdoor activities. It is then obvious that staying long periods of time in a contaminated indoor environment increases the risk of respiratory diseases triggered due to the poor IAQ.
The nature, characteristics, behaviour and release mode of different pollutants and more importantly biological agents in indoor environment are still some of the areas which cause confusion among the researchers. This might be happening for reasons expanding from, for instance, the volatilisation or release of new types of chemicals emerging from new types of processes such as construction materials (Salthammer 2020) to recently developed unknown types of respiratory diseases. From all respiratory diseases, the severe acute respiratory ones are deemed to be the most important due to the nature of the disease spreading and infection via the ‘invisible’ airborne routes.
Nowadays, there is a good understanding of pollutants’ nature and their impact on human health. The way also the modern types of indoor air purification systems and processes are operating to more efficiently trap and separate indoor air pollutants, as well as their spreading mode (Luengas et al. 2015) is better understood. For the most common, old-generation indoor polluting agents such as chemicals ranging from asbestos, tar droplets of tobacco products, carbon monoxide (CO), volatile organic compounds (VOCs) to dust, coal and pollen particulates, there is a much thorough and better understanding of their transmission to humans when these released into indoor air. The same good level of understanding exists of their associated health problems, causes and effects for those well-known pollutants which are studied for more than two decades (Domingo et al. 2020; Jones 1999; Monn 2001).
How the recently appeared droplets of infectious diseases occur, it is still though unclear to the global scientific community, as well as how they spread into indoor air and infect human occupants. Two very characteristic examples are the infectious severe acute respiratory syndrome (SARS) or SARS-CoV-2 variant or subvariant respiratory system diseases. Such types of biological agents are dispersed and, most importantly, among infected to non-infected individuals, resulting in alarming public health problems.
Lately, there is also an increasing concern of companion animal-to-human transmission risk (Yin et al. 2020) and other animals infected by coronaviruses (Carducci et al., 2020). There is also a lively discussion around transmission of such diseases by contaminated droplets of human saliva, along with a discussion on the origin and nature of the new infectious diseases which proved to lead to epidemic crisis, such the one caused by SARS-CoV-2.
Today, the general understanding is that the infectious saliva droplets are transmitted in indoor spaces via two prevailing modes: (1) the direct and (2) indirect mode of transmission between the occupants of a confined indoor space environment (Dhand and Li 2020; Galvin et al. 2020). The alarming and yet urgent need for better understanding of the above-mentioned transmission routes have led the scientific community to classify and further investigate such biological agents transmitting modes, focusing especially on the most risky ones to be released in indoor environments.
The importance of not only better understanding, but also hindering the transmission of such airborne, either biological agents or hazardous chemicals inhaled, and targeting the human respiratory system, can be showcased by the SARS outbreak which first appeared in 2002–2003, (Morawska 2006) causing 774 deaths worldwide [www.nhs.uk/conditions/sars/, last accessed on 14.10.2022] (Lauxmann et al. 2020; Razzini et al. 2020). SARS-CoV-2 has recently been declared a pandemic by the World Health Association (WHO) and during the 21 months of 2020–2021 (January 2019–November 2021) killed more than 6,586,200 patients around the globe [https://www.worldometers.info/coronavirus/, last accessed on 26.10.2022].
According to Zhang et al. (2020a, b, c, d), the lower respiratory infections remain the primary cause of patients mortality worldwide, accounting for 650,000 deaths each year. This fact makes the issue of shading light and better understanding the pollutants and biological agents’ transmission through the droplet formation during inhalation and retention in the human tracheobronchial system, an area of research which necessitates further investigation as a matter of urgency. On the other hand, the chemical pollutants’ transport and deposition in the respiratory system have been studied excessively (Lauxmann et al. 2020; Mittal et al. 2020; Rothan and Byrareddy 2020) and as a result the main focus of this study will mainly be on the biological agents nature, spreading and transmission.
The human respiratory system
The anatomy and physiology of the human respiratory system both play an important role in either short (~ 2 m) or long distance transmission (> 2 m) of the airborne infectious diseases. During the accidental release of pollutants and/or biological agents in a sick building environment (Jones 1999) or unintentional release by a patient of a contaminant and inhalation of droplets from other healthy adults, there is a direct relevance of the human respiratory system’s role and especially the lungs’ operation (Bansal et al. 2018).
The human respiratory system is very complex and is constituted from many compartments of different shapes and sizes. It has the ability to absorb the indoor air’s droplets or solid particulates by inhalation (Steiner et al. 2020). When a person talks, coughs and sneezes spreads a cloud of tiny saliva droplets (aerosol) in a very short period, of a couple of hundreds of milliseconds (200 ms) (Bourouiba et al. 2014; Scharfman et al. 2016). Sneezes especially, which in fact are described as violent exhalation incidents, have received much less attention in the scientific literature and it is a field which needs further investigation. A sneeze leads to an extremely short (in the order of 150 ms) incident of aerosols formation and spreads at extremely high speed in the order of 35 m/s (Scharfman et al. 2016). The occurrence of such events is very similar to that of the well know liquid atomisation process of the liquid fuels (Vadivukkarasan et al. 2020). It is also important to note that aerosols of infectious respiratory diseases like SARS-CoV-2 survives for at least 3 h (Netz 2020), while similar viruses might survive for days. When those droplets land on open surfaces substantially increasing the risk of indirect transmission to humans via touches. As aerosol is defined the suspension of fine solid particles or liquid droplets in a gaseous medium. Both droplets and particulates, commonly known in engineering science as particles can be potentially carried away by indoor air flows, in either short or long distances. How far those aerosol droplets or any other infected solid nanoparticles can be transported depends mainly on their size, which only in the case of solids is a stable characteristic. This is much more complicated for the case of different transport mechanisms of droplets of infectious diseases and particulates taking place simultaneously. For example, in an air-conditioned environment convective mass transfer (enhanced by the air currents) is taking place when a patient sneezes or coughs then an aerosol formed which can be dispersed in the indoor space. At the same time the infected saliva droplets might be unstable in size as a result of the effect of room temperature, humidity or their droplet breaking up tendency due to hydrodynamics (behaviour of droplets in air). It has been found that a sneeze releases approximately 40,000 droplets, while a cough produces a considerably lower number of droplets at around 3,000 (Dhand and Li 2020). Similarly, when a person walking or touching areas full of dust infected solid particles can spread in air. However, the size of the solid particles is not changing as a result of the indoor environment conditions and thus understanding of this mode of transmission is less complicated compared to the airborne droplets transmission mechanism. Regardless their behaviour though, both saliva droplets and/or any infected solid particulates are inevitably and unconsciously inhaled by the occupants of confined indoor spaces. Both those agents, infectious or not, and depending on their size, they are diffused at different concentrations in the many different compartments of the human respiratory system. Additionally, it is widely known from engineering studies that the airflow inside a specific geometry is strongly influenced by the geometric shape of the air flow pathways. Similar rules are applied in the human respiratory system and its compartments. Therefore, understanding the human’s inhalation/exhalation geometry route is a useful step towards simulation studies of the inhaled/and exhaled pollutants and biological agents (Mutuku et al. 2020a; Mutuku et al. 2020b).
On the other hand, and for the purpose of computational modelling studies, it is useful to know that the lung of an adult man offers the incredible air exchange surface area of approximately 100 m2. The mean lug capacity of an adult man is of 1.5 L (Scharfman et al. 2016) and he is able to inhale and exhale over 10,000 L of air per day while resting (Ni et al. 2020). This huge permeable membrane surface, the lungs, is the means by which the indoor air pollutants are absorbed and diffused by mainly the air mass transfer mechanism into the human body. Specifically, air mass transfer by diffusion via membranes is the key engineering mechanism for not only transmitting viruses trapped in saliva droplets, but also, a variety of other aerosol particles and droplets into the human body (Jayaweera et al. 2020). It is also known that the air mass transfer is enhanced by the increased surface areas available to diffusion and the physiology of a human respiratory system is not only quite complicated in anatomical characteristics, but also offers an excessive total surface to enhance any such transmission of biological agents hosted in indoor air. This creates more serious respiratory problems as penetration of pollutants and biological agents can affect every other organ of the human body via their diffusion in veins and the human blood circular system.
The human respiratory system consists of and connects also the mouth, throat and pharynx with the trachea, all of them often known as Generation 0, according to the human tracheobronchial tree. After inhalation, the larger pollutants or biological agents are filtered by the nose or deposit in the oropharynx, whereas smaller particles, droplets and nuclei are possible to penetrate the deeper than Generation 0 parts of the human respiratory system. The Generation 0 system is further leading to two bronchi, commonly known as Generation 2, with then the different branches of the lungs’ system to be continued down to smaller and smaller compartments of, in total, 23 different generations. The lowest and deeper of them, Generation 23, counting at some millions of the smallest lung compartments, being the alveolar sacks and alveoli (Mutuku et al. 2020a). For example, an adult man’s lung is made from approximately 300,000,000 alveoli (~ 200 μm in diameter) where the supply of oxygen takes place through a rich network of blood vessels (Rhodes 2008). Concerning their characteristic lengths, each of the respiratory system compartments, starting from the nose and mouth and ending in the tiniest lung compartments the alveoli, has substantial different sizes. Those sizes range from 30 to 150 μm, with total lengths between 120 mm and 150 μm. Typical air velocities in the respiratory system are ranging from 9 to 4 × 10−5 m/s, with corresponding residence times of contaminated air being between 0.021 s in mouth and the incredible high residence time of 4 s in alveoli (Mutuku et al. 2020a; Rhodes 2008).
The face anatomy though of each individual person varies and at the same time plays a major role to the biological agents’ transmission. For example, the nasal airways of an adults’ narrowest section is ranging from 5 to 9 mm with a resulting cross-sectional area ranging between 20 and 60 mm2, without taking into account the unique face anatomy of each individual. The nose anatomy, for instance, accounts for the 50% of the indoor airflow resistance and creates a natural resistance to biological agents’ and other pollutants inhalation (Rhodes 2008). The typical airflow through the nasal canals ranges from 0.18 to 1 l/s, from normal breathing to strongly sniffing, respectively (Rhodes 2008). The typical airflow from mouth during normal breathing is 3 m/s and depends, as previously stated, on the physiology of the face and lungs of a person (Rhodes 2008).
Table 1 depicts the main characteristics of the human respiratory tract (size (mm), velocity of air (m/s) and residence time (s)). The specific information might be proven useful for studies on lung damage during inhalation of pollutants and biological agents. In Table 1, it can be seen that by decreasing the characteristic length size of the geometry (higher Generation) of the respiratory system part, there is an incredible increase of the residence time of the biological agents which remain in the different generation parts of the human respiratory system.
It is also generally accepted that the respiratory droplets are formed from the fluid lining of the human respiratory track (Mittal et al. 2020), while the biological agents which are dispersed into indoor environments pose a new challenge. This challenge is mainly focused on the understanding of deposition/ diffusion patterns and efficiencies of the infectious aerosols generated from symptomatic and especially asymptomatic patients of infectious diseases (Mutuku et al. 2020a). Shao et al. (2021) stressed out the importance of indoor ventilation system design. More specifically, a properly designed and selected ventilation system is critical for decreasing the transmission risk of infectious diseases, while an inappropriate design can significantly limit the efficiency of droplets removal from indoor air. The local hot spots of biological agents with several orders of magnitude posing higher risks, and at the same time enhancing the droplets deposition causing surface contamination.
The site of droplet nuclei deposition in the lower Generation parts of lungs depends strongly on the droplet shape, size and mass. This transmission route is also dependent on the droplets which are carried in stable and small enough size via indoor air as respiratory droplets of some considerable size or as fine droplet nuclei (Dhand and Li 2020). The very fine droplets and particulates, entering and remaining in the lungs are often an approximate size of up to 7 μm (Jones 1999). In addition, Cheng et al. (2016) found that there was a probability of 50% for the influenza infected nuclei of sizes from 0.3 to 0.4 μm to promote influenza reproduction number (R-0) at values higher than 1, known to increase the risk of transmission of the disease. This only indicates the importance of indoor air biological agents’ size, and how influences their ability to be highly infectious. On the other side, Han et al. (2020) reported that the total dust and the respirable dust should be below 4.0 mg/m3 and 2.5 mg/m3, respectively, to ensure the health and safety of people staying in indoor environments within their usual working timeframe of 8 h. Bourouiba et al. (2014) also reported that tiny droplets and particulates can easily penetrate the respiratory tract, reaching the deeper targeted tissues of the lungs during inhalation of hazardous agents, as shown in Fig. 1.
According to Scheuch (2020), the very fine particles are extremely difficult to separate from the indoor air environment. Those cannot even be effectively deposited in the human respiratory tract compartments, reporting that only 30% of the inhaled particles (0.1–0.5 μm) are deposited in lungs. This means that the rest 70% of the inhaled droplets/particles are exhaled back to the indoor air again. He also claims that while the deposition occurs to a small extent throughout the entire respiratory tract, ranging from nose, mouth to throat, bronchi, bronchiole and alveoli, the preferred site of biological particles deposition is the peripheral area of the lungs.
Aliabadi et al. (2011) indicated that the humidity and temperature of the human respiratory tract varies with the anatomical location of the targeted compartment of the human respiratory system. A temperature, for example, of 37 °C and a relative humidity of 99.5% may be assumed for nasal respiration. For oral respiration the same temperature of 37 °C but lower relative humidity (90%) can be assumed, as well as an increase of the relative humidity by 1% per each Generation of the human airway (branching) until a maximum of 99.5% can be assumed for modelling studies. Varying temperature and relative humidity which prevail in the human respiratory tract are both very important factors due to the impacts on the characteristics of the hygroscopic aerosols, carrying biological or any other chemical agents. As those aerosols inhaled and move along the respiratory tract, their diameter and density might be changing. This is affecting their fate: either those aerosols will be exhaled or end up in deeper Generation part of the human’s respiratory system.
To better understand the importance of the temperature and humidity especially in the survival of biological agents, Zhang et al. (2020a, b, c, d) reported that MERS-CoV exhibited a very strong ability of surviving in air. They indicated that those agents surviving even 1 h after of their atomisation, via a violent for example sneezing, at relative humidity of 79% and ambient temperature of 25 °C. However, when the temperature increased by roughly 10 °C at 38 °C, only 5% survival rate occurred in 1 h when the relative humidity was 27%.
Chemical composition of particles and biological agents
It is widely known that different contaminants and mixtures of droplets present varying physicochemical properties, and those properties affect both the droplets’ and solid particles’ behaviour. The physicochemical characteristics of droplets such as viscosity (μ), density (ρ) and/ or surface tension (σ) affect their shape and characteristic size, among others parameters of the aerosol system (Mandato et al. 2012). Aerosols of human saliva which are infected with viruses, for instance, are primarily composed by water (more than 99% wt), and secondary by traces of enzymes, mucus, white blood cells, enzymes amylase, lipase and antimicrobial agents lysozymes (Al Assaad et al. 2020; Sarkar et al. 2019). Gralton et al. (2011) reported that an increase in the droplets’ size made from saliva and release in indoor air environment is directly related to an increased mucus viscosity.
In the literature as already mentioned it is common to simulate the aerosol droplets of saliva including water (Bourouiba et al. 2014; Liu et al. 2019a, b, c, d, e). However, water has a density of 1,000 kg/m3, viscosity of 10−3 Pa·s and an interfacial surface tension of 0.0728 N/m (Viswanathan 2019) at ambient indoor air conditions, while the saliva has a viscosity 86 to 150 × 10−3 Pa·s and interfacial surface tension of 0.05898 N/m (Sarkar et al. 2019). In the case of droplets’ formation during a coughing incident, the quality of saliva, which is different between a healthy person and a patient, will impact the droplets behaviour. This is done by strengthening the elasticity of the droplets and their resistance into their breaking up to smaller nuclei droplets and residuals, while releasing in the indoor air. As a result the saliva droplets will be more resistant to break, forming a lowest number of fine droplets and fewer droplets of a large size (Zayas et al. 2012). The droplets formed by a respiratory event of a patient can unfortunately be at the same time carriers of a biological agent due to their illness. In addition, contaminated droplets travelling in air might attract other (i.e. chemical contaminants being present in the confined indoor environment). As a result, another healthy person (recipient) can be infected via the unconscious inhalation process (Fig. 1) (Vadivukkarasan et al. 2020).
Similarly, for other types of indoor air contaminants, chemical analyses and characterisation play an important role on understanding their physicochemical characteristics. For example, droplets of tobacco smoke are made only from 20% wt water among the rest several thousands of different traces of their tar constituents (Ni et al. 2020). It is obvious that such properties will be different in nature biological agents and those should be taken into account when modelling the routes of transmission for indoor air agents. Balachandar et al. (2020) claim that although the surface tension of saliva droplets measured similar to that of water, their viscosity can be 1 to 2 orders of magnitude larger than that of water, resulting in making those droplets less coalescence prone.
Shape of particles and biological agents
Another important characteristic of pollutants and biological agents is their shape which has a strong influence on droplets’ and particles’ size (Rhodes 2008). The shape of a particle affects its properties such as the surface area per unit volume (m2/m3) and/or the rate at which particles in general settle in indoor air environments (Rhodes 2008). Defining the droplet, and especially the solid particles’ shape, is dependent on their real shape, the availability and suitability of the analytical methods for their shape determination. More specifically, in the case of droplets their chemical composition has a great impact on their characteristics such as density, viscosity and the forces imparted on particles, while they are expelled and move in the indoor air.
Particles in general, and for the sake of modelling and simulation studies, are usually assumed to be represented by spheres in a 3-D system or circles in a 2-D system, respectively. However, very rarely particles maintain a spherical shape and a uniform size. In practice particles’ shape, either those being plain chemical pollutants such as ash or biological agents, their shape is usually far away from that of a perfect sphere. Simulating solid particles as spheres might not be realistic and thus the dimensionless number of sphericity (φ) is used to determine how far away the shape of a real particle is from the perfect spherical one. Sphericity is defined as the ratio of the surface area of an equal in volume sphere with the real particle to the surface area of the real particle. Sphericity values of particles are always ranging between 0 and 1, with the value of 1 to represent the sphericity of the perfect shape that of the sphere (Rhodes 2008).
When also a droplet or a particle falls freely in air, under the action of gravity, and an indoor air stream blows at an angle, several forces acting on the droplet/particle. Those are the gravitational force due to the mass of the particle, the buoyancy force due to the movement of the particle in a fluid, as well as the inertia and drag forces which oppose the travel direction of the particle. The balance of all these forces imparted on a particle will dictate the terminal velocity by which the particle or droplet of a final stable size, for the latter, will settle in indoor air (Soni et al. 2020).
In fluid dynamics studies, the dimensionless numbers are very useful in analysing the fluid flows, especially the multi-phased ones, where there is an interface between different fluids (gas–gas, gas-liquids). A widely used dimensionless number for this type of flows is the Weber number (We). We number indicates how the shape of a droplet will be in a certain fluid system or when deposited on a surface. Thus, it measures the relative importance of the inertia over the surface tension force and is mainly used to demonstrate the different break-up modes of the droplets and, as the result, the shape of the droplets. We number can also be used in describing the influence on the surface wettability under the effect of droplets. According to Liu et al. (2019e), when the value of We number is less than 0.5, droplets impact differently processes on hydrophobic, hydrophilic and super-hydrophilic surfaces which are dominated by the spreading stage and retraction is not evident.
At low We number, a droplet undergoes shape oscillations at a certain frequency (Fig. 2). As the We number increases slowly, by increasing the aerodynamic force applied on a droplet and keeping the surface tension force constant, the droplet exhibits a transition from the vibrational mode to the ‘bag’ break-up mode of droplets. When the We number is low the droplet tends to maintain its shape. On the other hand, high values of We number along with increasing the aerodynamic forces imparted on the droplet lead to the loss of the almost spherical shape of the droplet and create a ‘bag’ deformation and breakage, which also forms several smaller satellite droplets of smaller dimensions (Soni et al. 2020).
Schematic representation of the vibrational, transitional and bag deformation shape changes of water droplets travelling in air adapted from (Soni et al. 2020)
During the release and travelling of the formed droplets in the air, they interact with their host medium and alter their shape as move along with air, especially at high speed airflows. It is also known that high speeds prevailing when a person coughs or sneezes. Hence, the droplet shape changes depend on different mechanisms such as the vibrational changes of droplets (We = 5.13), transitional towards a bag shape, bag-stamen, dual-bag, multi-mode, shear and catastrophic break-up (We = 6.35) modes, according to the work of Soni et al. (2020). Those transitional areas of the droplet shape-change depend on the conditions under which the experiment is taking place. This spherical shape is changing rapidly in a ‘bag’ shape and breaking via ligaments with the production of finer satellite droplets based on the surface tension and the aerodynamic forces applied on droplets. Relatively little attention has been given though to the instabilities associated with the dynamics of respiratory droplets creation and expelling during especially the coughing or sneezing incidents (Vadivukkarasan et al. 2020).
Size of particles and biological agents
The size of particles, either being solid particulates or liquid droplets, is determined by their characteristic length (size). The size of solid particles very rarely depends on the ambient indoor conditions (temperature, humidity). It also depends on their natural shape and morphology, and their chemical composition (Rhodes 2008). In addition, the particulates found in nature or produced buy processes very rarely possessing the perfect shape of a sphere. Real particles quite often have irregular shapes such as acicular, flaky, spongy or any other shape.
As a result, the size characterisation of solid particles is easier compared to droplets even though their shape is not spherical. The most appropriate characteristic length then for solid particles, instead of the diameter of a perfect sphere, it might be a different size such as the equivalent circle diameter or the surface to volume diameter and Sauter mean diameter and others (Rhodes 2008). All these characteristic lengths are used to describe the real size of a particle in conjunction with their non-spherical shape and real surface area, while they are moving in a fluid under aerodynamic forces. The measurement of the characteristic diameters is achieved by analytical methods such as the scanning electron microscopy (SEM), electro zone sensing, permeatry and other less known analytical and optical methods (Morawska et al. 2009; Rhodes 2008).
On the contrary of the stable size of solid particulates, droplets’ size is not unfortunately remaining stable upon released in indoor air and the droplet size is highly dependent on indoor air conditions. When a liquid is atomised an aerosol of droplets is produced, with those droplets to usually keeping their initial spherical shape for only a short period of time after their formation. Their shape depends on several factors which have to do with the droplet’s physicochemical characteristics and environmental conditions of the indoor space where they are dispersed and move.
The size of droplets highly depends on their formation process with fine ones of less than 1 μm to be produced from engineering manufacturing processes and larger up to 100 μm from mechanical processes (Morawska 2006). It also depends on especially the humidity and temperature (Dhand and Li 2020; Gralton et al. 2011) of the indoor air. The diameter of the droplet is a dynamic property due to the liquid evaporation under certain indoor air conditions. Those conditions are resulting in droplet shrinking by time which finally leads to the formation of the stable droplet nuclei (Ji et al. 2018; Li et al. 2018; Liu et al. 2019a, b, c, d, e; Liu et al. 2017; Morawska et al. 2009; Wang et al. 2019a, b; Wei and Li 2015; Xie et al. 2007; Yang et al. 2018).
In the case of droplets, it should be also considered the effect of droplet’s evaporation (Ji et al. 2018; Li et al. 2018; Liu et al. 2019a, b, c, d, e; Liu et al. 2017; Morawska et al. 2009; Wang et al. 2019a, b; Wei and Li 2015; Xie et al. 2007; Yang et al. 2018). A characteristic example of the effect of the relative humidity (RH) of air in water droplets of 50-μm diameter is that they will evaporate at RH = 50% in less than 3 s (Vuorinen et al. 2020). Droplets also under favourable humidity conditions may even increase in size due to attachment of the surrounding humidity of air on them. As a result, the droplet size varying not only with time, but also depends highly on the environmental conditions of temperature and humidity.
On another aspect the initial formation mechanism of an aerosol of droplets occurs due to mainly water vapour condensing onto the cloud of initial nuclei. This condensation occurs only when air contains slightly more water vapour than it normally holds for a given temperature. Vuorinen et al. (2020) indicated to the importance of understanding what are the humidity supersaturation conditions of atmospheric air and their nuclei, which promote cloud droplet nucleation and growth. Carducci et al. (2020) reported that the different expiratory events such as coughing, sneezing, speaking, singing and simple breathing release droplets of sizes ranging between 1 and 2000 μm noticing, however, that the majority of them has a size between 2 and 100 μm.
Recently, Dhand and Li (2020) indicated that the size of the droplets expelled by a patient mainly depends on their site of origin from their respiratory systems. For example, droplets which are produced by the mouth (oral cavity) have a large size (~ 100 μm), while smaller droplets (~ 1 μm) are formed during talking and coughing. The difference in size of droplets is due to the fact that the smaller droplets originate from the bronchioles, while the larger droplets are generated during normal breathing and from the larynx during talking and coughing. It was also reported that the particle size distribution could be altered by the presence of viruses (Dhand and Li 2020).
The droplet size determination is usually taking place via optical methods and laser analysis (Stadnytskyi et al. 2020; Tang et al. 2009). Ni et al. (2020) reported that recent studies have demonstrated that particulate matter (PM2.5) is closely associated with the chronic lung diseases and special attention should be given to biological pollutants of this specific size range. However, special attention should also be given to the fact that only few studies have conducted with modern techniques, capable of detecting sub-micrometric size particles. Thus, it is necessary to undertake further studies in order to develop a better understanding of the formation mechanisms of fine droplets (Morawska 2006).
Size distribution of a large population of particles and biological agents
The accurate characterisation of a large population of droplets/particulates can be done by investigating their size distribution within the multi-phase cloud of particles. This size distributions changes with time and distance from the source of generation depending on environmental factors, too (Dhand and Li 2020). This can be achieved by three ways and depends on the nature of droplets/ particles. For example, a droplet of an agent, infectious or not, in equilibrium with the environment has a stable size as cannot shrinks or increases in size. The later can be determined as per their particle size distribution based on mass, or surface area or number of particles (Rhodes 2008).
Concerning the aerosols and the size distribution of particles there is a threshold distance of approximately 1.5 m, which distinguishes the two basic droplet and droplet nuclei transmission processes, namely (a) the short-range mode and (b) the long-range airborne route. The short-range mode of transmission includes the conventional, large droplet routes of parabolic travel under the effect of gravity, as well as the newly defined short-range airborne transmission (Liu et al. 2016a, b). However, Pendar and Páscoa (2020) reported lately that the infectious saliva droplets can travel up to 6 m at a wind speed of 15 km h−1and a safe distance of 2 m is not appropriate for outdoor activities.
A large number of studies highlights the importance of the size distribution regarding the particles and biological agents, as well as the occupants in indoor environments (Choi et al. 2015; Cole and Cook 1998; Dhand and Li 2020; Faridi et al. 2020; Faulkner et al. 2015; Feng et al. 2020a, b; Fernstrom and Goldblatt 2013; Ghosh et al. 2015; Gralton et al. 2011; Lv et al. 2018; Milton et al. 2013; Monn 2001; Morawska et al. 2009; Nicas 1996; Nielsen 2015; Phu et al. 2020; Sajjadi et al. 2016); Scheuch 2020; Schroeter et al. 2012; Vianello et al. 2019; Wang and Yoneda 2020; Yang et al. 2016).
Lv et al. (2018) indicated that the supply flowrate of fresh air per unit of closed space volume, defined as air changes per hour (ACH) is also an important factor which influences the indoor particle distribution. They found that the free settling of particles into indoor space for particles ranging from 0.5 μ to 1.0 μm, 1.0 to 3.0 μm and 3.0 to 5.0 μm, presenting a sedimentation rate of 0.086 h−1, 0.122 h−1 and 0.173 h−1, respectively. The same researchers reported that an increase of ACH from 0 to 2.5 yields significantly different values on the sedimentation. Recently though, special attention is given to studies with reference to the size distribution of droplets and the improvement of measurement accuracy for small scales below micrometre range. For instance, a droplet size distribution for coughing indicates a peak drop size of almost 15 μm while the associated settling speed obtained at 6.5 mm/s in an ambient winter indoor air (Bourouiba et al. 2014).
Han et al. (2020) stated that there are several empirical equations to characterise the droplet size distribution such as Nukiyama-Tanasawa, Rosin–Rammler, log-normal, root-normal and log-hyperbolic. Poon et al. (2020) found that the droplets produced by coughing present a wide size distribution of droplets ranging from 0.6 to 16 μm, with a mode of around 6 μm. Lately several studies have been devoted to the size distribution of small droplets expelled during talking, coughing and sneezing; however, uncertainties on the droplet size distribution are still present (Asadi et al. 2019; Scharfman et al. 2016).
The airborne route of transmission of particles and biological agents
The droplet or aerosol airborne transmission route seems to be the most complicated mode of dispersion of particles, droplets and biological agents into indoor environment (Dhand and Li 2020; Ai et al. 2019a, b; Ai and Melikov 2018; Aliabadi et al. 2011; Beggs 2003; Booth et al. 2005; Drossinos and Stilianakis 2020; Monn 2001) and as a result remains one of the most difficult aspects to study. Aerosols of particulates and droplets pose a major challenge: being invisible in human eye, they are transported as a cloud of submicron-sized particles generated especially by coughing and sneezing via a process which is called atomisation in engineering practise, or trapped in liquid micro-sized water droplets (Vuorinen et al. 2020) or even drifted away by being attached on solid particulates (e.g. dust and pollen) (Griffin 2007).
The airborne transmission is further classified as short and long range, with most of the scientific community to be still unclear on the determination of the safety distances need to be kept to avoid infections. This becomes even more unclear considering especially infectious diseases which have the ability to spread in short and long diseases (Bourouiba et al. 2014) and under the two most widely known modes of transmission the short and long one. It seems that the most common indirect transmission route is occurring via spreading of an infected cloud of small saliva droplets (aerosols) during talking, coughing, sneezing or breathing (Gralton et al. 2011; Tang et al. 2009; Zhao et al. 2005). Lately, Godri Pollitt et al. (2020) demonstrated that the short-range airborne route of infection may be the most common transmission way of infectious diseases. Carducci et al. (2020) also refer that droplets up to 5 μm, fall next to the donor source, within a distance of approximately 1–2 m, due to the effect of the gravitational force prevailing on the large droplets. The smaller aerosols though can remain suspended and travel at greater distances in the indoor air environment. More information on the aerosol’s nature, generation and behaviour can be found in next sections.
Aerosols of particles and biological agents
An aerosol is defined as a population of submicron particles or a suspension of droplets and droplet nuclei in the air. An aerosol of droplets is usually created by a violent respiratory event such as a cough or sneeze (Sakharov and Zhukov 2020). Jayaweera et al. (2020) claimed that up to 90% of the aerosol droplets generated by a human expiratory activities. Since aerosols are particles or biological agents of less than 50 μm, they remain suspended into indoor air due to their small size for extended periods of time. The larger airborne particles (> 50 mm) are too heavy to become suspended in the air for longer periods of time (Marui et al. 2019). In addition, the droplet nuclei residuals remain into indoor air at a fine and stable size, in the range of 5–10 μm (Bourouiba et al. 2014). This final stable size of the residual droplets/nuclei is determined by the equilibrium with the moisture of ambient indoor air (Vuorinen et al. 2020). The dynamic reduction in the size of the infectious droplets leads to a change in the pattern of transporting in air, depending also in the indoor air currents, humans moving and talking, coughing or sneezing all known to be able to create a laminar or event transient and turbulent flow of the aerosols in confined spaces.
Many researchers study how the diameter of the liquid droplets changes dynamically and strongly affected by the temperature and relative humidity (RH) of indoor air (Aliabadi et al. 2011; Dedesko and Siegel 2015; Faridi et al. 2020; Shajahan et al. 2019; Verijkazemi et al. 2018; Zhang et al. 2019). Aerosols of less than 1 μm, with the lowest density are generated by nasal breathing, while the highest density by coughing in very short time (up to 500 ms) (Bourouiba et al. 2014). Exhaled breath is also more responsible for transmitting viruses of size of approximately 0.1 μm, compared to the bacteria transmission with particle size over 1 μm (Zhang et al. 2019). From the above-mentioned, it is evident that all the above factors, chemical composition, shape and size of droplets are interconnected.
The main characteristics of an aerosol depend on the characteristics of the single droplet and the forces imparted on them as the move along with the air currents (Rhodes 2008). The shape, and as a result size, of droplets depends on the spray/aerosol angle, covering of surface, droplet velocity distribution, volume distribution and pattern is different for different aerosol systems (Broniarz-Press et al. 2009). Some physicochemical properties of the droplets, such as viscosity, might vary, and depend on the fluid environment where the droplets are hosted (other liquid or air environments). For an aerosol of droplets in air, for instance, the relative viscosity of the liquid compared to the surrounding gas viscosity is high (50%), while in a liquid host is relatively low (Ben-Tzvi and Rone 2010).
In general, the larger the droplets and particles are, the quickest they settle and in a shortest distance they travel, as this will determine how far the particles will be dispersed. This is based on the force by which they are expelled from the source, either the source being a person or a ventilation equipment. It is widely acceptable that the respiratory droplets evaporate to form smaller droplet nuclei, remain then suspended in air due to Brownian motion, and susceptible individuals from the source could inhale them even when stand far away. Scheuch (2020) indicated that for small particles, the main mechanism of their transport in air is the Brownian motion and this mechanism works relatively effectively with droplets size in the range of 5–100 nm. Scheuch (2020) stated that the second important physical mechanism of eliminating particles from the indoor air is sedimentation. This mechanism is effective for aerosol particles above 0.5 μm – 1 μm. Stilianakis and Drossinos (2010) indicated that all droplets generated by an expiratory event, either this being coughing, sneezing, laughing, talking or breathing cover a large size range from approximately 0.6 to more than 1000 µm.
Atomisation of liquids
Atomisation is the process of formation of fine droplets, or an aerosol of droplets or biological agents in the case of indoor environments (Morawska 2006). The atomisation as a process creates small fractions of the liquid droplets affecting considerably other pollutants emission and spreading (Urbán et al. 2017), especially in indoor spaces. Ai and Melikov (2018) reported that the techniques of producing aerosols are increasingly been used to investigate airborne transmission of biological and chemical agents.
For example, a sneezing or violent coughing incident in terms of engineering is a large-scale atomisation process and formation of an aerosol of saliva droplets and nuclei. The atomisation as a mechanical process is affected by the geometry of the source, the aerodynamic forces imparted on particles, the surface tension and viscosity of the droplet. The aerodynamic forces are of considerable effect on the droplet or particle, while travelling in the air with the dominant being the gravitational forces or mass body forces which are imparted on relatively large particles. Thus, larger droplets settle quickly and the smaller airborne droplet nuclei are travelling over longer distances by the indoor air streams (Dhand and Li 2020). The drag force being also opposite to the gravitational force leading to the resistance in motion of droplets/particles in air. The surface tension, too, is the natural tendency of a liquid droplet to stabilise the shape of a droplet of a certain volume, offering the minimum surface area possible. The surface tension has a consolidating influence, which contradicts with the opposite tendency of the surface of the droplet to extent and wet a surface. The viscosity is a property which describes the rheological properties-behaviour of a fluid, and is opposing any change of the shape of the liquid droplets as they flow (Morawska 2006).
Atomisation is further classified as primary, upon injection of droplets and particles i.e. by a person sneezing, and secondary atomisation (Kuznetsov et al. 2019). The secondary atomisation takes place by the droplet size disruption due to interference of a solid surface such as a collision with a wall or a substrate (e.g. hand in front of the mouth while sneezing). This creates a second wave of atomisation due to the fact that the single cloud of droplets colliding with each other, a micro-explosive break-up of droplets is taking place, especially under the effect of the increased temperature and heat, as well as the interference of an existing indoor air stream flow. Han et al. (2020) indicated that increasing the mean air velocity results in larger aerodynamic forces which reduce the droplet sizes, while an increase in air pressure reduces the droplet size. The same researchers (Han et al. 2020) reported that the droplet size distribution is a crucial parameter of the atomisation process besides the mean diameter of droplets.
Suspension and resuspension of particles and biological agents
Suspension time of indoor pollutants is defined as the time that small droplets or particles remain suspended on air, carried away at short or long distances due to airflow motion and without necessary settling on horizontal surfaces such as the floor. Their velocity also plays an important role on the analysis and simulation of the aerosol systems and their suspension time. The effects of gravity or inertia forces on droplets of less than 30 μm are negligible as they are too small in size; their transmission then is mainly influenced by the indoor airflow as those particles remain suspended for long time and as a result the risk to be inhaled is high (Zhu et al. 2006). Results of studying a coughing incident showed that more than 6.7 mg of saliva are expelled as droplets exhibiting a velocity up to 22 m/s, while at the same time a travel distance of more than 2 m has been reported (Zhu et al. 2006). On the other hand, droplets with their size range varying from 50 to 200 μm are of significant size in terms of importance. Those are affected by gravity and fall on the ground as the indoor air flow streams are weakening. Droplets of diameter of 300 μm or larger, which are mostly affected by inertia forces rather than gravitational, rarely fall (Zhu et al. 2006).
In general, the evaporation rate of droplets depends mainly on the ambient temperature and humidity. It was found that droplets of size less than 100 μm will typically become droplet nuclei before settling on the floor. Small droplets of sizes between 5 and 10 μm will rapidly evolve into droplet nuclei with extremely low settling speeds (> 0.003 m/s). As a result those droplet nuclei are able to remain suspended for longer periods of time, however, the fate of droplets are determined by the competing effect of inertia, gravity and evaporation (Mittal et al. 2020). At the same time the nuclei are expected to be crucial in the long-range airborne transmission route. Bourouiba et al. (2014) also highlighted the synergistic effect of Brownian motion in the phenomenon of suspension and resuspension of particles, where air currents are absent. The same mechanism may keep the stable in size droplet nuclei suspended for very long periods of time in such environments.
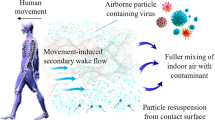
The resuspension of particles into indoor spaces is the phenomenon of the detachment of deposited particles and droplets of other pollutants or biological agents from the surfaces into the bulk air (Al Assaad et al. 2020). The reason of resuspension is usually the human activities such as walking and natural or mechanical ventilation. All these actions cause the aerodynamic and mechanical vibration disturbances of the particles. It seems that particle resuspension takes places within a very narrow time frame of less than 25 s, since the initial disturbance, prior further decreasing to negligible values (Al Assaad et al. 2020).
For different indoor open surfaces, it was found that the resuspension was the lowest for smooth surfaces such as glass, followed by marble and linoleum. When though the aerodynamic disturbances applied on those surfaces were accompanied with vibrations the resuspension of particles increased by more than 45% for all cases (Al Assaad et al. 2020). It also seems that a decrease in the roughness of the indoor space surfaces can increase the particles and droplets adhesive forces reducing considerably the vibration effects which are responsible for enhancing the resuspension in air (Al Assaad et al. 2020). For example, dust is re-suspended when people walking on carpets and has been found that the mass load of dust is generally greater in carpets than the hardwood floors (Haines et al. 2020). They reported other pollutants such as stain-protectors which were found not only in the carpet, attached to dust, but were also detected in the blood serum of the occupants (Haines et al. 2020). The same researchers found that the man-driven resuspension of particles previously settled on carpets and hard flooring is a source of coarse-mode biological agents’ pollution. When an adult, for instance, is walking across the floor, this can create a resuspension of 10 to 100 million particles per minute, many of which are likely to be of biological origin. For particles thought of less than 10 μm mass resuspension rates can exceed 10 mg/min (Haines et al. 2020).
In addition, indoor environmental conditions of temperature, humidity and air streams should not be underestimated, as it was found that 50% of the airborne biological agents could originate from the resuspension of fungi grown at equilibrium relative humidity of more than 85% on dust floor (Dannemiller et al. 2017). You and Wan (2014) based their findings both on experimental and modelling results. They showed that Bacillus anthracis particles’ concentration becomes 1.5 to 3 times and 4 to 8 times higher after the initiation of airflow for particle of sizes between 2 and 4.75 μm. Their study indicated clearly the importance of the airflow to the resuspension of particles.
Evaporation, coalescence and growth of droplets
The evaporation of droplets plays an important role in the later fate of the droplet and competing effects of inertia and gravity. The evaporation rate depends on the difference between the droplet surface saturation vapour pressure and the vapour pressure of the surrounding air, which also depends on the humidity (Mittal et al. 2020). The diffusion mechanism strongly affects the droplets surface-to-temperature difference, and the relative velocity between the droplet and surrounding gas. Thus, dimensionless numbers such as the Sherwood (Sh), Nusselt (Nu) and Reynolds (Rep) for the droplets are important to determine the evaporation phenomenon. It seems that higher temperature and lower relative humidity lead to larger evaporation rates that increase the critical droplet size (Mittal et al. 2020). The temperature effect initiates the evaporation of atomised liquid droplets affecting the overall motion and distribution of droplets. Sakharov and Zhukov (2020) indicated that smaller droplets, 5 μm, would evaporate in less than 3 s, at typical indoor relative humidity of 50%.
Evaporation is a very fast molecular process, for instance, a 20-µm droplet evaporates to 1-µm diameter droplet within only a rate of 0.24 s−1 at 50% ambient relative humidity (Yang et al. 2018; Ai and Melikov 2018). Due to the evaporation phenomenon, the size of the droplets is affected by time, as they are shrinking and this is prominent for droplets with an initial diameter of 100 μm (Yang et al. 2018). Wells (1934) although has already found that by the beginning of the twentieth century, droplets with characteristic diameter larger than 100 μm settle to the ground in less than 1 s, without being significantly affected by evaporation. Similarly Morawska et al. (2009) did not detect droplet evaporation for particle sizes varied between 0.5 and 20 μm, and, if any evaporation occurs, take place at less than 1 s. Studies of water droplets with diameters of 10 to 240 μm indicated that the medium-sized droplets vary from 50 to 170 μm, as the thermal stratification weaken the evaporation of droplets due to less heat and mass transfer between the droplets and air. When the ambient relative humidity increased to 60%, a possible condensation phenomenon occurred on droplets, increasing the suspending time of droplets in the air (Liu et al. 2019a, b, c, d, e). In addition, vapours generated due to evaporation and super-saturated wet air exhaled from the respiratory tracks form a vapour plume in front of the nose and mouth of a person, which, despite the short life time enhances significantly the evaporation of the droplets captured in it (Li et al. 2018). Due to the evaporation and density of airborne droplets and mass concentration of inhalable pathogens, the process can result in a higher risk of infection (Li et al. 2018). The study of Li et al. (2018) demonstrated the importance of considering inhomogeneous humidity field when modelling the evaporation and dispersion of cough droplets.
Droplets might collide with each other and can undergo coalescence. Droplet coalescence is the process of merging of two or more droplets during contact to form a single larger droplet. If droplets are hydroscopic they grow in size or while transported in air might trap particulates such as dust (Han et al. 2020; Morawska 2006). As a result, the coalescence mechanism leads to a change of the particle size distribution with the mode value of droplets to increase as the total number of particles decrease (Morawska 2006). Shao et al. (2021) reported that the viscosity and surface tension of droplets might be of significant importance. They influence the droplet size distribution as both controlling the coalescence and breakage of larger droplets to smaller. However, these mechanisms are important only during the ejection stage of the infected saliva droplets. Once the infected saliva droplets are below 50 μm, the coalescence and break up mechanisms are hindered. Occasionally, the particles may shatter apart into numerous smaller particles; however, this process usually occurs primarily in large particle size droplets, which cannot be considered as aerosols (Shao et al. 2021).
Aerosols and bioaerosols
An overview of airborne particle types that affect respiratory health
As previously discussed, the vast variety of abiotic (chemical agents) and biotic (biological agents) particles being present in air at considerable concentrations can have a negative effect on human respiratory system or human health in general. Such particles are usually present in the form of aerosols which either travelling or being suspended in air. As defined in the ‘Aerosols of particles and biological agents’ section, an aerosol is a suspension of fine solid or liquid particles of varying sizes in air (Fig. 3).
Bioaerosols can be defined as the particulate matter usually associated with compounds of pure biological origin. This definition includes all pathogenic or non-pathogenic media ranging from live or dead fungi and bacteria, viruses, high molecular weight allergens, pollens and many others (Ghosh et al. 2015). The main type of aerosols being of a significant concern for human health is the plume of droplets of micron size that are scattered in the air during breathing, talking, coughing or sneezing (see the ‘The human respiratory system’ section). As these droplets can stay suspended in the air for many minutes and contain pathogenic microorganism that can lead to respiratory diseases (Bourouiba et al. 2014; Cole and Cook 1998) (Fig. 4). Aerosols of biological agents can be also created mechanically by other ways such as emerging from water fountains, shower heads, surgical or dental procedures, as well as faulty air-conditioning or ventilation systems (Tran et al. 2012).
As discussed previously, the size of these droplets is a very important factor affecting the transmission of respiratory diseases. Usually droplets’ size range from 0.01 to 500 μm, although larger droplets have also been reported (Gralton et al. 2011). According to Guzman (2020), only droplets smaller than 5 μm are able to reach the trachea of the recipient, while droplets below 2.5 μm can penetrate to the lower respiratory system and reach the bronchioles and alveoli inside the lungs (see ‘The human respiratory system’ section). Aerosols smaller than 5 μm are considered to be airborne means of disease transmission, since they stay in the air for long periods of time, while larger aerosols are linked with droplet-associated transmission of diseases (Gralton et al. 2011).
The spread of pulmonary aerosols is a major public health concern, especially for indoor environments of hospitals and other healthcare units, where patients often have a weak immune system and at the same time multi-drug microbial pathogens might be present (Stockwell et al. 2019);Tang et al. 2006).
A second type of particles that could be potentially harmful, even though not of biological origin, is related with dust. Dust particles in domestic surfaces, such as floors, furniture or carpets (Haines et al. 2020), may also be contaminated by microbial pathogens (Dannemiller et al. 2017), inducing allergic reactions or worsen the symptoms of an already pre-existing asthma condition. Inhalation of household dust, which contains a variety of aeroallergens, can worsen the symptoms of allergies and asthma. House dust particle sizes range from 2 mm to 63 μm, with approximately 33% of the dust being smaller than 500 μm (Lanzerstorfer 2017). Examples of such allergens include the house dust mite (HDM) protein Der p 1, Can f 1 (associated with dogs) and Fel d 1 (associated with cats). Dust particles < 5 mm tend to remain suspended in the air for a number of days, whereas larger particles (> 5-mm diameter), which remain airborne for a shorter period after disturbance (Hussain et al. 2019). The dust mite itself has a diameter of 200 μm and it is considered too large for penetrating the lungs, however a small proportion of its faeces that are rich in Der p 1 can enter the lungs and cause allergy symptoms (Wilson and Platts-Mills 2018).
House dust particles can also absorb harmful microbial volatile organic compounds (MVOCs). Exposure to low levels of MVOCs in indoor air is related to a range of non-specific symptoms, including redness of the eyes and irritation of the nose and skin, that are known as the sick building syndrome (Wady and Larsson 2005). Other types of dust that could enter inside buildings via open doors or windows include sand particles, farm and coal mine dust and they can all lead to serious lung damage (Khan and Strand 2018; Penconek et al. 2019; Schuijs et al. 2015).
Fungal and bacterial spores can also lead to development of serious lung disease (Cutting and Ricca 2014; Foster et al. 2017; Han and Weiss 2017). Several microorganisms such as fungi (e.g. Aspergillus fumigatus) and bacteria (e.g. Bacillus anthracis) form spores. These are resistant structures with thick cell walls of several layers that provide resistance against extreme environmental conditions, such as adverse temperatures, drought and chemical biocides (Leggett et al. 2012; Madsen et al. 2016). These spores can be easily dispersed in the air, outside aerosols and become inhaled by humans. After inhalation, they end up in the lungs where they germinate and colonise the tissues of the human respiratory system, if they are not controlled by the immune system (Husman 1996). Bacterial spore sizes vary from 0.8 to 1.2 μm (Carrera et al. 2007), while fungal spores range from 2 to 4 μm (Madsen et al. 2016). Fungal spores and vegetative fragments can also be allergenic, bearing a variety of allergens such as Asp f 1, Alt a 1 and Cop c 1 (Crameri et al. 2006; Green et al. 2006). Anthrax spores formed by Bacillus anthracis are considered to be a highly persistent and lethal type of bioterrorism agent, therefore they are a major biosecurity concern, especially for indoor environments, such as offices or schools (Taylor et al. 2012).
Finally, plants produce pollen, which is a powdery substance consisting of pollen grains that contain the male gametes (sperm cells) of the plant. Such particles have a rigid thick exterior layer which protects the genetic material of the gamete. Pollen size ranges generally from 20 to 60 μm (Mander 2016; Rantio-Lehtimäki et al. 1994; Soares et al. 2018). There are, however, exceptions such as Pinaceae pollen which can be of size over 80 μm (Smith et al. 2014). Pollen grains can also travel long distances in air and are known to contain allergenic proteins inducing hay fever and asthma exacerbations. More than 150 different pollen allergens have been identified so far (Mothes and Valenta 2004); Rodríguez et al. 2007); White and Bernstein 2003). The most common ones are the Phl p 1 and Lop p 1. Unfortunately, allergic reactions to pollen represent the most frequent type I allergies affecting up to 30% of the industrialised population (Biedermann et al. 2019; D’Amato et al. 2007; D’Amato et al. 1998). Climatic changes are expected to influence the duration as well as the intensity of pollen seasons which might in hand with air pollution contribute to increased numbers of respiratory allergy and asthma (Pablos et al. 2016).
Major respiratory microbial pathogens and health effects
Numerous infectious agents lead to serious respiratory illness or even death. These belong to three major classes of microorganisms, namely viruses, bacteria and fungi (King and Auger 2002; Prat and Lacoma 2016; Rath et al. 2017) (Fig. 5). Viruses are not considered to be living organisms, as they do not have a metabolism and are unable to replicate outside a host cell. Their viral genetic material is usually protected by a protein capsule. Several viruses are also surrounded by a lipid envelope (Weber and Stilianakis 2008). Bacteria and fungi are living organisms. The morphology of these microbes is extremely diverse in nature, but again the genetic material is enclosed by a lipid membrane and a polysaccharide cell wall. On their surface, these agents have receptors enabling them to attach to human cells and potentially invade into the human cells. In terms of pathogens sizes viruses typically range between 20–300 nm, bacteria 1.0–5.0 μm and fungal cells 2–30 μm (Choudoir et al. 2018; Shi and Tarabara 2018; Weiser 2013) (Table 2). Some bacteria and fungi are able to build long filaments up to several centimetres (cm), while some fungi can form much larger structures in nature (e.g. mushrooms). As discussed in the previous section, the respiratory pathogens usually spread through the air via coughing or sneezing (Barmby and Larguem 2009; Srivastav et al. 2018; Xie et al. 2009), as well as being transmitted by touching contaminated surfaces and then touching the eyes, nose or mouth (Deacon 2006; Madigan 2009).
Viruses
One of the most frequently encountered viral pathogens is the rhinovirus, which is the primary cause of common cold in humans, closely related to respiratory diseases. There are three species of rhinovirus (A, B and C) that include around 160 serotypes (Glanville and Johnston 2015; Pomeranz et al. 2019; Taylor-Robinson and Tyrrell 1962). The symptoms that they cause upon human infection include sore throat, runny nose, nasal congestion, sneezing and cough, muscle aches, fatigue, malaise, headache, muscle weakness and loss of appetite. However, this virus can also cause exacerbation of underlying lung disease, for instance, in critically ill patients with pneumonia, with or without co-pathogens. In terms of particle size, they are among the smallest viruses, with diameters of about 30 nm (Collier et al. 2000; To et al. 2017).
Another very common respiratory viral infectious agent is the influenza virus, which causes the common flu. There are four types of this virus (A, B, C and D) (Iwasaki and Pillai 2014; Kim et al. 2018; Lyons and Lauring 2018). Types A, B and C are known to infect humans (Kumar 2017; Peteranderl et al. 2016; Webster and Govorkova 2014), while D affects cattle. Normally, flu is characterised by systemic symptoms such as fever, myalgia, headaches and severe malaise, and respiratory symptoms such as coughing, sore throat and rhinitis. Those occur after approximately 2 days of an incubation period and can last for up to 7 to 10 days. Coughing and tiredness symptoms though can persist for even up to two weeks. If the virus reaches the alveoli of the lungs, it can result to serious viral pneumonia and interstitial pneumonitis. The influenza virus especially consist a major health risk and hazard for the elderly or immunocompromised individuals (Pleschka 2013).
Coronaviruses is another group of viruses causing diseases in humans, mammals and birds. When humans are infected by coronaviruses, this leads to respiratory infections that can range from mild effect to detrimental for the human health and even lead to death. Mild symptoms are similar to these of common cold, while more lethal strains can result in severe respiratory illnesses such as SARS, MERS and SARS-CoV-2 syndrome (de Wit et al. 2016; Hageman 2020; Yin and Wunderink 2018). The mortality rates range from 5 to 15% (Chan et al. 2003; Singh 2016; Weiss and Murdoch 2020). The SARS-CoV virus pandemic (2002–2004) resulted in 926 deaths worldwide, while the newly identified SARS-CoV-2 virus led to 279,000 deaths worldwide by 21/05/2021, only 6 months after the first outbreak (Lauxmann et al. 2020; Rothan and Byrareddy 2020). As of July 2017, 2040 MERS-CoV laboratory confirmed cases, resulting in 712 deaths, were reported globally, with a majority of these cases from the Arabian Peninsula (Chafekar and Fielding 2018). There are as yet no vaccines or antiviral drugs to prevent or treat human coronavirus infections. Finally, other airborne viral pathogens include respiratory syncytial virus (RSV) and parainfluenza virus (Collier et al. 2000).
Bacteria
Streptococcus pneumoniae is asymptomatically carried in healthy individuals, typically colonising various tissues of the upper respiratory system, as well as the sinuses. However, in susceptible individuals with weaker immune systems, such as the elderly and young children, S. pneumoniae can lead to serious pneumonia. Moreover, several strains of this species have developed resistance to many of the traditional antibiotics, which makes such infections difficult to treat (Feldman and Anderson 2016). This bacterium also causes bronchitis, rhinitis, acute sinusitis, otitis media, conjunctivitis, meningitis, sepsis, osteomyelitis, septic arthritis, endocarditis, peritonitis, pericarditis, cellulitis and brain abscess (Murray et al. 2013).
Haemophilus influenzae is a bacterium that is responsible for a wide range of topical and systemic infections. Most strains of H. influenzae are opportunistic pathogens, as they usually grow on the mucosal layers of the respiratory tract without causing any disease. However, when other factor such as a viral infection, impaired immune function or chronic inflammation create the appropriate conditions, then a disease can occur. In infants and children, H. influenzae type b (Hib) causes bacteraemia, pneumonia and acute meningitis. More rarely, it can also lead to cellulitis, osteomyelitis and infectious arthritis (Butler and Myers 2018).
Legionella pneumophila is a bacterial pathogen which invades and replicates inside macrophages via phagocytosis. Inside the macrophages, the bacteria are enclosed into a membrane-bound vacuole that protects them from degradation by cellular enzymes and allows them to multiply in large numbers. Legionella is most commonly transmitted by inhalation of contaminated aerosols produced by water sprays, jets or mists. This bacterium can cause Legionnaires’ disease and the less severe form, Pontiac fever. The common clinical symptoms of Legionella infection include high fever, cough, chills, difficulty in breathing, neurological problems, muscle weakness, diarrheal, chest pain, headache, nausea and vomiting. Legionnaires’ disease, which is a form of atypical pneumonia, has a mortality rate in the range of ∼10–50% (Murray et al. 2013; Prussin et al. 2017).
Mycobacterium tuberculosis is the causative agent of tuberculosis. Although this type of lung disease was widely controlled after the discovery of antibiotics, new emerging multidrug-resistant (MDR) strains are still a great concern in many areas of the world. Symptoms include chest pain and a prolonged productive cough. Approximately 25% of tuberculosis patients remain asymptomatic, but they can still spread the pathogen (Hunter 2016, 2018; Wang 1999). From time to time, patients may cough up blood in small amounts, while in rare cases, the infection may damage the pulmonary artery, resulting in massive bleeding (Bansal et al. 2018; Beggs et al. 2003). Other bacteria that can lead to serious lung disease are Acinetobacter baumanii, Bordetella pertussis and Klebsiella pneumoniae Pseudomonas aeruginosa, Staphylococcus aureus and Bacillus anthracis (Murray et al. 2013).
Fungi
Aspergillus fumigatus is a fungal pathogen that it is ambiguously found both indoors and outdoors. It forms thousands of tiny spores (2–3 μm) which readily become airborne and after inhalation they can easily penetrate the tissues of the lower respiratory system. The fungus is capable of growth at temperatures up to 50 °C, with spores surviving at 70 °C (Dijksterhuis 2019; Grishkan 2018; Pitt and Christian 1970). Typically, inhaled spores are quickly eliminated by the immune system in healthy individuals. However, in immunocompromised people, such as transplant recipients, AIDS or cancer patients, the fungus is more likely to become pathogenic and lead to more serious lung illnesses such as allergic bronchopulmonary aspergillosis (ABPA), aspergilloma, chronic pulmonary aspergillosis and invasive aspergillosis. Due to the extended use of immune suppressants for treating human diseases, it is estimated that A. fumigatus is the cause of over 600,000 deaths annually, with mortality rates ranging from 25 to 90% (Latgé and Chamilos 2019; Murray et al. 2013). Other important fungi that can cause respiratory disease in immunocompromised patients are Candida albicans, Cryptococcus spp. and Pneumocystis spp. (Murray et al. 2013).
Microbiological and molecular methods for microbial enumeration and identification
Nowadays science innovation arises from the multidisciplinary approach of a variety of scientific fields. Analytical methods often applied in biomedical sciences find applications in engineering. Below, the main microbial and molecular methods for identification or biological agents are reported, and might be proved very useful in engineering applications such as determination of the biological load of indoor air.
Air samplers
The microbiological quality of the air is usually determined by sampling small volumes of air, which contain various bioaerosols. Then the process of enumerating and identifying the microbes within the sample is taking place. Such microbial monitoring is done routinely at healthcare-related areas for assessing environmental quality and deciding if corrective intervention is necessary or not (Napoli et al. 2012; Razzini et al. 2020). Air samplers are the most frequently used devices for such purposes, mainly because of their low costs and easiness of handling. Air samplers draw in air and force the various particles in it to get impacted over collecting surfaces or impinged into a liquid. These samples can also utilise filters for selecting a specific range of particles, while different impaction rates can be used by adjusting the vacuum settings (Ghosh et al. 2015).
Air filtration
Another method for collecting airborne bioaerosols is filtration. During this procedure, air is drawn through a filter with a 0.2-µm pore size, trapping all particles apart from small viruses. This can be facilitated by a vacuum system. The filter can be then used for enumerating the microbes or culturing them before identification with traditional or molecular techniques. One important advantage of filtration is that the captured microorganisms remain viable. Also, the filter can be directly used for nucleic acid extraction (Ferguson et al. 2019). However, such filters are prone to overloading or damage and also desiccation can result in low recovery efficiency of the trapped microbes (Ghosh et al. 2015). Such method of air sampling by filtration was used for sampling of bioaerosols by (Predicala et al. 2002) at a swine farm environment.
Other bio-aerosol precipitation approaches
More laboratory-based approaches are available for precipitating bioaerosols or other particles from the indoor air. Those however are not used as frequently as the ones mentioned above. These include sedimentation and centrifugation, as well as electrostatic or thermal precipitation (Ghosh et al. 2015).
Cotton swabs
Medical-type swabs are often used for taking biological samples from surfaces, for subsequent microbiological or molecular analysis. The procedure is very simple, as the swab is rubbed onto or into the contaminated area and then wiped across a culture medium, such as an agar plate, where the bacteria and fungi from the swab may grow. This has to be done quickly and aseptically, in order to avoid contamination of the sample with other environmental microbes. It has been suggested that if the swab is mildly sonicated after sampling, the microbial recovery rate on the culture media is increased (Ahnrud et al. 2018).
A combination of air sampling and cotton swabs was used this year at a Milanese hospital for detecting SARS-CoV-2 genetic material (RNA) in the air and on key surfaces of the building (Razzini et al. 2020). The most contaminated surfaces were hand sanitizer dispensers (100%), medical equipment (50%), medical equipment touch screens (50%), shelves for medical equipment (40%), bedrails (33.3%) and door handles (25%) (Haun et al. 2016; Kurgat et al. 2019; D. J. Weber et al. 2019). Other recent studies that used cotton swab sampling approaches for microbiological monitoring are these by Lee et al. (2018) and Luksamijarulkul and Pipitsangjan (2015). According to these studies, it was shown that such swabs remain the easiest and most widely used method for surface sampling. A variety of more effective swabbing products, such as nylon, rayon and polyester swabs, has been lately developed (Bruijns et al. 2018).
Microscopy
One of the most traditional methods for microbial identification is observation of the microbe’s physical characteristics, such as shape, size and the types of dyes that absorbs, under a light microscope. For example, the Gram stain can distinguish different bacterial species to Gram-positive or Gram-negative, according to their cell wall structure. Other types of staining can provide information about production of spores (Schaeffer-Fulton staining), capsules (India ink or nigrosine) and mycolic acids (acid-fast staining). Light microscopy can also be used for enumeration of cells, by using of a haemocytometer. For virus identification, the use of electron microscopy is required (Ahmed et al. 2016).
Use of selective and differential culture media for microbial enumeration and identification
The method that is most frequently used for isolating bacteria and fungi involves culturing them on the surface of solid nutrient media (Brugger et al. 2012; Burmølle et al. 2009; Wiegand et al. 2008). Such media contain all the necessary nutrients for the growth of a wide range of microbes, including carbon (C), nitrogen (N) and phosphate (P) sources, amino acids, inorganic salts and trace elements. It also contains 1.5% agar, which is a polysaccharide that gives a gel-like structure to the solid medium. After incubation for 24 h at 37 °C, colonies appear on the surface of the agar, which can be counted and identified based on their morphological characteristics (Collins et al. 1989).
There is a wide range of selective and differential media that are used in clinical microbiology laboratories for microbial enumeration and identification (Bonnet et al. 2020; Reddy et al. 1972; Yoo et al. 2014). Selective media contain compounds that inhibit the growth of some microorganisms, permit however others to grow. Differential media contain ingredients making the colonies of a certain group of microorganisms appear in a different colour than this of other groups. Some differential media are also selective, for instance, MacConkey agar, which is selective for Gram-negative coliforms and can also differentiate between lactose-fermenting and non-lactose-fermenting bacteria (Ahmed et al. 2016; Nigro and Steward 2015). Such traditional microbiological culture-based approaches have been followed recently for indoor bioaerosol characterisation (Yasmeen et al. 2020; and Nasir et al. 2018).
Use of biochemical tests for microbial identification
A plethora of biochemical tests is also available for identifying microbial species. These tests usually determine the ability of a species to grow in media containing certain carbon or nitrogen sources, such as glucose, lactose and urea. As the microbes metabolise these substrates, they produce products leading to a medium colour change, which is regarded as a positive test result. Based on the results from many such tests, a microbiologist can use specific charts for identifying a bacterial pathogen. Automated identifying systems are today available for running these tests in a high-throughput mode, e.g. VITEK2® and FAME, and those have been very useful for bioaerosol profiling (Duquenne 2017). Similar approaches can be used for identifying fungi, but not viruses as they do not have a metabolism activity (Spiegelman et al. 2005).
Polymerase chain reaction
The polymerase chain reaction (PCR) is a widely used method for rapidly amplifying a specific area of the DNA of a sample (Gadsby et al. 2019; Liu et al. 2019a, b, c, d, e; Siqueira and Rôças 2003). The PCR product is then analysed by gel electrophoresis and a final result can be obtained about the identity of microbe, based on whether it contained the targeted area in its DNA or not (Järvinen et al. 2009). Real-time quantitative (qPCR) is a more advanced method and can be used for both identification and quantification of a microbial pathogen in a clinical sample. Real-time qPCR utilises fluorescent chemicals that can be detected by a detection system when amplification of the desired DNA area begins. As a result, there is not a need for gel electrophoresis. This method is more sensitive and precise than the standard PCR method (Kralik and Ricchi 2017). Real-time quantitative and standard PCR methods have been recently applied in several indoor bioaerosol surveillance studies (Coleman and Sigler 2020; Razzini et al. 2020).
Matrix-assisted laser desorption/ionisation
Matrix-assisted laser desorption/ionisation (MALDI) is an ionisation technique for mass spectrometry that uses a laser energy absorbing matrix to create ions from large molecules (Dingle and Butler-Wu 2013; Jang and Kim 2018; Singhal et al. 2015). Biological macromolecules such as DNA, proteins and peptides tend to be fragile and fragment when ionised by more conventional ionisation methods. The advantage of matrix-assisted laser desorption/ionisation (MALDI-TOF) is that it does not lead to such fragmentation, something which makes it suitable for clinical use. Colony material of the microbe in question is placed onto the sample target and overlaid with matrix. The resulting spectra are used for the identification of micro-organisms, after analysis by dedicated software and compared with stored profiles. MALDI-TOF is much faster, more accurate and cheaper than traditional methods (Madsen et al. 2015; Murray 2012; White et al. 2019).
Nucleic acid sequencing
Next-generation sequencing (NGS) is a highly advanced technology that via which millions of DNA fragments can be simultaneously and independently sequenced (Huang et al. 2020; Lin et al. 2019; Sung et al. 2018). In clinical microbiology laboratories, metagenomic NGS (mNGS) is most frequently used for detection of certain pathogens. The cost of such analyses is still very high, and most hospitals cannot afford them even when the results are obtained faster and are much more reliable.
Another advantage of NGS is that analyse DNA or RNA in a clinical sample are surveyed masse, in contrast to PCR that can only analyse few specific targets per run (Gu et al. 2019; Madsen et al. 2015; White et al. 2019). MALDI-TOF and NGS are definitely the most promising advanced technologies for microbial identification at the moment. This year’s “Viruses in the Built Environment (VIBE) meeting in Arlington, Virginia, USA, highlighted the importance of constructing bioinformatic tools and databases that will ensure a quick and accurate microbiological monitoring within buildings (Prussin et al. 2020). Other methods that can also help with microbial identification include DGGE, serological approaches, epifluorescent microscopy and flow cytometry (Ghosh et al. 2015).
New novel approaches for real-time monitoring of bioaerosols
The last few years, several novel approaches have been tested and applied for real-time monitoring and characterisation of bioaerosols. These include fluorescence spectroscopy, elastic scattering, microscopy and holography, Raman spectroscopy, mass spectrometry, breakdown spectroscopy, remote sensing, microfluidic techniques and paired aqueous techniques (Huffman et al. 2020; Nasir et al. 2019). Examples of such modern applications are provided below. In 2013, Usachev et al. (2013) applied a surface plasmon resonance-based immunosensor for real-time bioaerosol detection. The collected viral particles were mixed with a target-specific antibody and the positive aggregates were efficiently detected in less than 2 min.
Choi et al. (2015) developed and tested a micro-optofluidic platform that proved able to accurately detect, quantify and characterise bacterial aerosols, by use of fluorescent dye detection, fluidics and optical microscopy. Furthermore, an adenosine triphosphate (ATP) bioluminescence assay was developed by detecting and measuring the concentration of bacterial aerosols. This assay was coupled with a continuous aerosol sampling device. The collected bacteria were charged, added to a liquid buffer and their numbers were estimated by measurement of the ATP levels generated via microbial metabolism (Park et al. 2016).
Finally, laser-based bio-detectors were applied for characterising a great number of individual particles in seconds, by analysing optical scattering and fluorescence characteristics. Data analysis by use of Artificial Neural Networks led to construction of decision trees for aerosol classification (Leskiewicz et al. 2018). All these approaches seem extremely promising and are expected to be more widely applied for characterisation of medically important aerosols in the near future.
Survival of respiratory microbial pathogens
The duration of survival of different microbial pathogens in the environment is a major public health parameter that has significantly attracted the interest of most epidemiologists worldwide. The main factor that affects this is the structural composition of the pathogen. For instance, fungal and bacterial spores can survive for years due to their thick cell walls and dormant metabolism. Non-enveloped viruses are also very tolerant due to their resistant protein capsule. Enveloped viruses are less resistant, because their lipid bilayer is susceptible to heat, dryness and chemical agents. Finally, fungi are usually better at survival than bacteria due to their stronger cell walls (Table 2). Both bacteria and fungi often require high water activity and nutrient availability in order to survive and grow (Dedesko and Siegel 2015; Mendell et al. 2018). Furthermore, the type of surface is also important for determining the survival of microbial pathogens. For example, moist, porous and soft surfaces such as carpets and curtains are more likely to accommodate microbial growth than dry non-porous hard surfaces such as wood, plastic or metal (Thompson and Bennett 2017).
Some types of surface material such as copper, silver or antibacterial polymers can lead to microbial death and prevention of colonisation (Muller et al. 2016). Finally, environmental factors such as heat, pH, humidity, UV radiation and chemicals can affect microbial viability. Some bacteria are tolerant to adverse environmental condition (Walsh and Camilli 2011), while many bacteria and fungi can form biofilms, slimy layers made of polysaccharides and proteins that protect them from hazardous conditions (Hall-Stoodley et al. 2004). Environmental factors such as humidity and ambient temperature can also affect the survival of microbes in the air, either within or outside bioaerosol droplets, with a subsequent importance for respiratory disease (Prussin et al. 2020; Pyankov et al. 2018; Tang et al. 2006).
Transmission of respiratory microbial pathogens
Microbial pathogens can be transmitted via a variety of routes, including person-to-person (touch, saliva), airborne, foodborne/waterborne, via blood, sex, insects or fomites (non-living objects, such as door handles or towels, etc.). When it comes to airborne transmission, this can be classified as long and short range, depending on the viability of a pathogen in the air or the stability and size of the droplet that might carry it. Large-droplet diameter is considered to be > 50 to 60 μm, small droplet diameter is < 50 to 60 μm and droplet nuclei diameter < 5 to 10 μm (Tang et al. 2006) (see the ‘Size of particles and biological agents’ section). An example of short-range airborne transmission is the inhalation of droplets from a coughing or sneezing infected donor (from a < 1-m distance), while long-range airborne transmission can include inhalation of fungal or bacterial spores that have travelled a long distance in the air via the wind (see ‘The challenging nature of biological agents’ transmission in indoor environment’ section). However, several non-spore bioaerosols can also travel long distances, if certain environmental conditions permit it (e.g. indoor air circulation) or if they are inside small droplets or droplet nuclei.
Many respiratory pathogens can be also transmitted via personal contact, via dust or from fomites, if the recipient touches a contaminated area and then touch facial, oral or nasal areas, allowing the entry of the pathogen into the respiratory tract (Wei and Li 2016a, b). Even if the pathogen enters the upper respiratory system, it might not be able to cause disease unless it penetrates the lower respiratory tract (trachea, bronchi, bronchioles and the alveoli). As it was mentioned in the ‘The human respiratory system’ section, this depends on the size of the infectious agent or the droplet that carries it (< 5 μm are able to penetrate lungs).
Factors that affect the development of respiratory infectious disease
Pathogen-related factors
Several microbe-related factors can affect its ability to cause respiratory disease. Some infectious agents are more pathogenic than others and even within the same species there are often sub-species, serovars or strains that are more virulent than others. This depends on the weaponry of virulent factors that a strain carries, such as toxins, super-antigens and degradative enzymes that destroy the tissues and cause localised damage and inflammation. Moreover, some strains have the ability to form filaments, spores and biofilms that make them more invasive and tolerant to the attacks of the immune system. Finally, the ability of a strain to mutate is an additional factor that affects it virulence (Davidson 2018; Murray et al. 2013).
In addition, the number of the initial infectious agents that enter the site of infection (e.g. lungs) is very important. Usually, low numbers, e.g. 50–150 cells or virus particles, can be easily dealt by the immune system which represses the infection before it leads to disease. Higher infectious doses can be difficult to control. However, this also depends on the type of pathogen that reaches the site of infection. The infectious doses of certain infectious agents that can lead to death have been experimentally measured by use of mice or other laboratory animals (Prussin et al. 2020; Tang et al. 2006) (Table 1).
Host-related factors
There are also many different host-related factors that can determine if a respiratory disease such as pneumonia will develop or not and how severe it will be. Firstly, the age of the patient is important. Young children do not have a fully developed immune system and the elderly have a weakened one that is often unable to eradicate the infectious agent. Vaccination against agents such as the influenza virus, Mycobacterium tuberculosis or Streptococcus pneumoniae can also prevent development of respiratory disease.
Immunocompromised individuals, such as cancer patients, transplant recipients or HIV patients, are also more vulnerable to infectious agents that cannot cause respiratory disease in healthy individuals (e.g. Cryptococcus neofmans, Candida albicans). Moreover, smoking and air pollution destroy the ciliated cells of the respiratory system that are a physical defence mechanism against microbes and push mucous-trapped microorganisms out of the body. This makes smokers more susceptible to lung and airway disease. Finally, underlying disease such as diabetes, obesity or cystic fibrosis can affect the potency of the immune system (Engin et al. 2020; Lacoma et al. 2019; Murray et al. 2013).
The role of heating, ventilation and air-conditioning systems
Heating, ventilation and air-conditioning (HVAC) systems are widely recognised as the most influential engineering approach to control the airborne transmission of the pollutant agents in the internal spaces (Bhagat et al. 2020; Li et al. 2007; Luongo et al. 2016; Qian and Zheng 2018; Shajahan et al. 2019; Wei and Li 2016a, b) as their operation is associated with the movement/ flow of the indoor air due to the introduced buoyancy forces and pressure differences. The operation patterns of these systems have been analysed in several engineering and epidemiological studies in last decades, resulting in the suggestion of three individual characteristics, (a) ventilation rate, (b) airflow direction and (c) thermal plume, to be the main parameters that significantly determine the transportation and the infectious mechanisms.
Adequate ventilation rate is pointed out as an important factor for removing the pollutants in general and especially the less studied biological agents from the indoor spaces. Airflow direction leads the air from the clean zone into the pollutant source area and consequently from the polluted space to outdoors. Thermal plume influences the space stratification conditions and the kinetics of the pollutant agent. The following sections summarise and criticise the results of previous studies related to the aforementioned parameters regarding the control of the airborne transmission of the contaminant agents, and on minimising the risk of cross-infection between the occupants.
The role of ventilation
Ventilation is the supply of the outdoor air into internal building spaces, and can be categorised as natural and mechanical or forced ventilation. Both ventilation options induce different advantages and disadvantages while their combination could provide mixed characteristics (Cao et al. 2014; Gilkeson et al. 2013). Natural ventilation is of low cost and maintenance and allows the ambient air to be entered into the building by various and mixing routes. In contrast, the use of natural ventilation is directly linked with fluctuating ventilation rates that under specific outdoor and indoor conditions the air movement could be inadequate or overabundant. In addition, the intake air is unfiltered and depending on the ambient environmental conditions it may transport a variety of undesirable contaminants (e.g. dust, fumes and microbes, among others).
Mechanical ventilation could supply filtered fresh air and especially in combination with high efficiency minimum efficiency reporting value (MERV) 13–16 filters, the risk of the airborne disease transmission can be significantly reduced (Rui et al. 2008). Although the mechanical ventilation systems offer better control capability of the indoor environment characteristics, however, they introduce significant financial expenditures (Azimi and Stephens 2013; Escombe et al. 2019; Hobday and Dancer 2013). Weather using natural or mechanical ventilation the quantity of pathogens and the quality of the indoor air are not necessarily higher in case of the first or second alternative, e.g. (Qian et al. 2010; Short and Al-Maiyah 2009; Stockwell et al. 2019). This is due to the fact that in both cases the airflow rate and the airflow movement pattern are the most prominent characteristics that determine the efficacy of each option to provide the desirable indoor atmosphere. In general, the use of ventilation in buildings is associated with a dual positive and negative effect against the airborne transmission (Noakes and Andrew Sleigh 2009). The positive role is the dilution of the concentration or the dispersion of the biological agents and particulates leading to minimising the occupants’ risk. In parallel, the transportation of the bio-aerosols and particulates among adjacent spaces is a non-negligible undesirable effect.
Mechanical systems of ventilation
In mechanical ventilation systems, two different airflow patterns are commonly used such as the displacement ventilation (DV) and the entrainment or mixed ventilation (MV) flow (ASHRAE 2017b). There are also advanced mechanical systems such as personalised ventilation (PV) and personalised exhaust which can be installed stand alone or in combination with other ones in spaces with or without specific requirements (Melikov 2004). The application of PV systems in common indoor spaces becomes more attractive, as many recent studies indicate the benefits on the indoor air quality (IAQ) improvement and minimising the airborne transmission risk (Al Assaad et al. 2018; Habchi et al. 2016; Lipczynska et al. 2015; Melikov et al. 2013; Yang et al. 2015).
Except for the fact that any stand-alone or conjugated ventilation system under controlled conditions is able to supply fresh air, however, the differentiation of the airflow direction and pattern-based on the design characteristics of each system in association with ventilation rate- are the most important parameters that influence the (a) contaminant concentration; (b) contaminant removal effectiveness; (c) infection risk; and (d) human’s exposure to pollutants in general and biological agents.
Displacement and entrainment/mixed ventilation systems
Displacement ventilation (DV) system or displacement airflow describes the air movement in one direction by a piston type motion. Ideally, the air is not mixed and the pollutants are totally removed out from the indoor space. The airflow in DV systems could be either downward (ceiling-to-floor) (see Fig. 6) or upward (floor-to-ceiling) (see Fig. 7), based on the design requirements of each space. In both cases, the idea is to supply fresh and clean air with low velocity leading to a laminar airflow which intent to sweep air across the space with the minimum possible mixing (ASHRAE 2017b).
Due to that characteristics, the downward DV system is considering as the ideal system for removing the contaminated indoor air, and is expected to minimise the cross-infection risk (Qian and Zheng 2018; Tang et al. 2006). However, either the design of DV systems with airflow pattern about 4.0 ACH or the synergies with the humans’ thermal plume are impossible to produce laminar flow, thus mixed ventilation airflows occur (Qian et al. 2008).
Entrainment/ mixed ventilation (MV) system or airflow, Fig. 8, refers to a circular pattern of air flow in which the intake fresh air is conventional mixed with the internal air and finally the mixture leaves the space.
In this case, the pollutants are removed by dilution. Entrainment flows, according to mixing conditions are characterised as short-circuit flow or complete/ uniform mixing (well-mixed). In the first case, the supply air leaves the space without mixing with the indoor air as a result of very poor mixing conditions, while in the second one the supply air is instantly and evenly distributed in the space leading to a perfect mixing with the room air (ASHRAE 2017b).
Underfloor air distribution (UFAD or UAD), in Fig. 9, is a hybrid ventilation method that combines the characteristics of both displacement and mixing ventilation schemes. Outdoor air is introduced into a plenum floor and supplied to the indoor space throughout floor-mounted diffusers. The diffusers produce a turbulent flow near to the floor level and the supplied air is mixing with the indoor one. Then the mixed air moves to the ceiling in a laminar flow without mixing phenomena and exhausted from the space through outtake diffusers.
The ventilating performance of the underfloor distribution system is thus between upward DV and MV systems (ASHRAE 2017b). The effectiveness of the DV, MV and UAD systems on minimising the airborne transmission of the infectious agents has been evaluated in several studies using experimental and numerical approaches. A detailed analysis on these studies indicated that the majority of them deal with the assessment of cross-infection risk, while some of them focused on the assessment of the droplet dispersion mechanisms and behaviour.
Qian et al. (2006) performed a series of experiments to understand the interaction of the exhaled bio-aerosols in downward and upward DV and MV airflows in a hospital ward. They reported that downward DV with an airflow rate of 4 ACH has similar behaviour as the MV, due to the turbulent characteristics of the flow. In addition, they do not suggest the installation of upward DV system in hospital wards due to the possibility of increase the exposure level, if an occupant is located in the exhalation jet.
Olmedo et al. (2012) studied the human exposure to the contaminants of the exhaled bio-aerosol among two persons taking into consideration between other parameters the use of upward displacement and mixing ventilation. They found that in the case of upward DV, the exhaled air flows transport for longer distance with higher concentration. Lin et al. (2012) accessed the risk of pathogen inhalation under stratum and upward DV and concluded that the risk was higher when upward DV system was used.
Chen et al. (2014) analysed the person-to-person bio-aerosol transport under upward displacement and mixing ventilation and UAD systems. They indicated that the upward DV and underfloor air distribution have the same performance in reducing the contaminant exposure and were about 20% better than the MV. Although this study presents contradictory behaviour compared to the similar ones, the authors, however, reported that in cases of upward DV and UAD, significant variations in the relative effect on exposure have been noticed. This phenomenon indicates that under certain circumstances, the pointed out relationship among the alternative ventilation systems may be altered (Chen et al. 2014). Similar results and recommendations have also been reported in many studies (Ai et al. 2019a, b; Friberg et al. 1996; Jurelionis et al. 2015; Keshavarz et al. 2017; Li et al. 2012; Lin et al. 2013; Mazumdar et al. 2010; Salmanzadeh et al. 2012; Villafruela et al. 2019; Wu and Lin 2015; Yang 2013; Yin et al. 2009).
Lai and Cheng (2007) studied the droplet’s dispersion in a space under upward displacement and well-mixed ventilation flows. They concluded that for the well-mixed ventilation system, the dispersion pattern is driven by the velocity airflow. High-velocity airflow produces within 1 min a homogeneous bio-aerosol. In contrast, when upward DV with low-velocity airflow is used, the dispersion partner is dominated by the droplets’ size. In this case, 10-μm droplets begin to settle at the lower areas of the located space.
Gao et al. (2008a, b) simulate the dispersion characteristics of an exhaled bio-aerosol consisted with droplets in the range of 1 to 10 μm in an office space using upward DV, MV and UAD systems. The obtained results showed that in MV system the exhaled droplets were uniformly distributed. However, in all ventilation systems, the exhaled flow was trapped in the breathing zone of the occupant.
Mui et al. (2009) stated that the droplet dispersion and mixing in case of DV is poorer, compared to the MV. Sun and Ji (2007) proved again that the efficiency of the upward DV is higher in removing small droplets, while MX has equal efficiency for removing droplets in the range of 80 to 100 μm and higher efficiency in removing large size droplets. They concluded that this behaviour is subjected to the equilibrium between gravitational and buoyancy forces. High gravitational forces occur in the case of large droplets, while the buoyancy forces become significant in the case of small-sized droplets and high-velocity airflow. DV introduce low-velocity airflow, and for the case of upward airflow pattern, the large size particles tend to settle in the lower part of the space. However, for the case study of downward airflow systems, these particles can be efficiently removed by the outlet vents. MV systems are characterised by high airflow patterns leading to a well-mixed bio-aerosol which can be efficiently removed from the space, regardless of the droplet sizes. It is worth noticing that similar results have also been reported in the following studies (Berlanga et al. 2018; Chao and Wan 2006; Gao et al. 2012a, b; Lai and Wong 2011; Seepana and Lai 2012; Li et al. 2011; Yin et al. 2011).
Personalised ventilation systems
Personalised ventilation (PV) system or personalised airflow intents to provide fresh air into breathing zone of an occupant. The system uses air terminal devises that consist of nozzle/s allowing the control of airflow rate by the occupant to the desirable level and direction. The PV system has two main advantages: it improves the quality of the inhaled air and allows the user to control the temperature, velocity and direction of the supplied airflow (Melikov 2004). The contribution of PV systems on the mitigation of the airborne cross-infection risk has been analysed in several studies. Cermak and Melikov (2007) conducted a series of measurements to examine the capability of two PV systems in association with an UAD system to protect occupants from exhaled infectious aerosols and emissions from the floor materials. They found that the conjugated systems protect the occupants from inhaling the aerosols, while the concertation of the pollutants into the indoor air was increased. Pantelic et al. (2009) studied the protective role of a PV system against the infectious cough droplets released near the PV occupant. They addressed that the PV system significantly reduced the bio-aerosol concentration in the breathing area of the occupant. It had also reduced the risk of cross-infection particularly in cases that the source point of the bio-aerosol infection and the occupant were at a distance less than 1.75 m. He et al. (2011) assessed the airborne transmission of an exhaled bio-aerosol between two occupants under three ventilation systems, namely MV, upward DV and UAD working autonomous and in conjugation with PV. They concluded that for PV scenarios the quality of the inhaled air has been improved. A study of Mazej and Butala (2012) proved that by using a PV system, the amount of the re-inhaled bio-aerosol is extremely low; however, the dispersion of bio-aerosol to the indoor air increases the risk of cross-infection onto the occupants who are not using personalised ventilation. Li et al. (2013) analysed the exposure of occupants to the exhaled pollutants under two different conjugated ventilation systems. They concluded that the upward DV combined with PV provides better inhaled air quality compared to the alternative option of MV with personalised one. Pantelic et al. (2015) evaluated the effectiveness of a PV system to reduce the inhalation intake fraction of an infectious bio-aerosol against to MV system. The obtained results indicated that the PV system substantially reduces the intake fraction for the all analysed cases. In addition to the above studies, it is worth mentioning that similar results have also been addressed in many other cases (Bolashikov et al. 2015; Bolashikov and Melikov 2009; Cermak et al. 2006; Nielsen 2009; Nielsen et al. 2007a, b; Nielsen et al. 2007b; Pantelic and Tham 2011; Pantelic and Wai 2009; Tham and Pantelic 2011; Wai and Pantelic 2009; Yang et al. 2015; Zheng et al. 2011). Moreover, detailed reviews on the personalised ventilation systems have been published on (Liu et al. 2019d; Melikov 2004; Zhai and Metzger 2019).
Natural ventilation
Natural ventilation is the physical flow of the external air through the building vents into indoor spaces caused by a thermal and/or wind pressure difference. Under certain circumstances, it can be provided an adequate level of pollutants’ removal, which is not always controlled and acceptable. There are two types of natural ventilation airflow patterns: the cross and the single-sited ventilation. Cross ventilation is achieved using openings in both sides of the space and it is driven by the pressure difference. Single-sited ventilation occurs when one or more openings in the same façade of the building are open. Thus, the airflow could be driven by temperature and/or pressure difference. Although the role of natural ventilation on indoor air quality and comfort levels has been well studied and documented (e.g. (Allocca et al. 2003; Brager and De Dear 1998; De Dear and Brager 2002), however, the effect on the airborne transmission of pollutants and bio-aerosols between the adjusted building units and their dispersion in lower or higher building floors has attracted the research interest mainly after the SARS pandemic in 2003. Li et al. (2005) studied the SARS virus transmission between adjusted flats in a high-rise residential building in Hong Kong. They concluded that in the natural ventilated high-rise apartment buildings it is difficult to control the air leakage between flats as the flow is driven by the air-tightness and the pressure difference. This phenomenon leads to carry bio-aerosols between the apartments of the building. A study by Gao et al. (2008a, b) proved again the airborne transmission across apartments in a high-rise natural ventilated building through open windows between flats caused by buoyancy effect. They reported that the gaseous pollutant’s concentration in the immediate upper flat is 2 orders lower compared to the lower flat in which the gaseous pollutant is generated, while the risk of infection is 1 order lower, respectively. They also noticed the importance of wind speed and concluded that high-speed winds act like air-curtain reducing the pollutants’ spread. However, they clearly reported that in natural ventilated multi-family buildings the inflection control of bio-aerosols should consider the role of this airflow.
In-line with the previous study, the same research team simulated the airborne transmission of particle pollutants (Gao et al. 2009a, b). They found that the concentration of the particle pollutant in the upper floor is between two to three orders lower than in the lower source floor. They also concluded that particles up to 1-μm disperse like gaseous pollutants, while particles larger than 20 μm show a strong deposition on the source space and limit their transport to the up-floor area. Ai and Mak (2014) studied the dispersion characteristics of infectious aerosols exhausted from a building unit in association with the hypothesis that the exhausted aerosol can re-enter into another unit of the building through opened windows. They reported that the re-entry ratios can be reach up to 10% based on the wind direction and façade characteristics, non-flush walls or balconies. The high re-enter ratio is observed in the windward site following by the leeward site both in case of 45° wind direction. In addition, the balconies enhance the re-entering phenomenon of the exhausted bioaerosols, except the case of the normal incident wind direction. Wu et al. (2018) studied the role of infiltration on the airborne transmission route and evaluate the associated infection risk in a high-rise building, under different wind directions and leakage characteristics of doors and windows. They found that infiltration rates below 0.7 ACH increase the cross-infection risk up to 20% compared to the risk of 9% in case of air change rates over 3 ACH. The increase of infiltration rate along the building height leads to the increase of the cross-infection risk in the lower building floors. They also reported that the wind direction is a significant parameter that influence the cross-infection risk. The higher cross-infection risk observed in case of the contaminant source is placed on the windward site and on the adjacent units. Finally, they concluded that improving the air-tightness of the internal openings and increasing the airflow on the external ones is an effective solution for the control of inter-unit airborne transmission. The effect of natural ventilation in the airborne transmission of bio-aerosols in multi-family buildings (in both vertical and horizontal directions) together with the role of wind characteristics has also been investigated by many scientist (Ai and Mak 2016; Ai et al. 2013; Cui et al. 2018; Liu and Niu 2011; Liu et al. 2007; Liu et al. 2008; Liu et al. 2011a, b; Liu et al. 2010, 2011a, b; Mu et al. 2016; Mu et al. 2017; Niu et al. 2005; Niu and Tung 2008; Wang et al. 2010a, b; Wu et al. 2019a, b; Zhou et al. 2014), who finally conclude to similar results and suggestions.
The role of ventilation rate
A minimum level of ventilation rate is recommended by relevant Standards (ASHRAE 2017a, 2019a, b; CEN 2019), in order to maintain the quality of the indoor air to a pre-defined acceptable level and minimise the risk of human exposure to pollutants in general and biological threats. In general, there are three methods for the calculation of the ventilation rate, that based on the: (a) perceived air quality, (b) criteria for individual substances and (c) pre-defined ventilation air flow rates. According to the perceived air quality method, the ventilation rate is found by adding the required air volume for people and emissions. This method is mainly used in residential and non-residential buildings in which critical contaminant sources are not identified. In spaces with essential pollutant sources the ventilation rate is calculated based on the generation rate of the pollutant, the concentration of the pollutant on the supply air, the guideline concertation of the pollutant in the indoor air and on the effectiveness of the ventilation system. The third method introduces pre-defined ventilation air flow rates based on the local climate and building characteristics, and is also used in residential and non-residential buildings. It is worth noticing that the first and third method in case of the non-occupied hours of the building, lower the ventilation rate to a minimum air flow needed to maintain the concentration of the non-human related pollutants to the guided level (CEN 2019). In line with the above strategy, Gao et al. (2012a, b), estimate that increasing the ventilation rate up to 10 ACH in schools led to a reduction of the peak inflection to influenza up to 9% and postponed the peak of outbreak by 3 days. However, they noticed that ventilation rates over 5 ACH may be difficult to reach and suggest to be used in conjunction with alternative prevention policies. A similar study (Gao et al. 2016), regarding the potential outbreak of influenza in Hong Kong, concluded that even in cases that the airborne transmission is 20% of the total inflection the increase of ventilation rate has strong influence on transmission pathways similar to other control measures. Nardell et al. (1991) studied the air borne infection caused by the operation of building’s ventilation and concluded that of increasing the ventilation rate by 67% and 133%, reducing the infection risk by 33% and 52% respectively. The relationship between ventilation rate and infection risk has also been studied in the work of Fennelly and Nardell (1998). They found that the infection risk decreases exponentially with the increase of ventilation rate, for instance, in a moderate-exposure space operated with 6 ACH the probability of infection is 0.42 and decreasing to 0.21 by increasing the ventilation rate to 12 ACH. Similar conclusions regarding the influence of ventilation rate to the inflection risk and on the associated concentration of airborne pathogen bioaerosols into indoor air have also been reported (Beggs et al. 2003; Bergeron et al. 2011; Cao et al. 2015; Chen et al. 2014; Escombe et al. 2007; Escombe et al. 2019; Gao et al. 2009a, b; Knibbs et al. 2014; Knibbs et al. 2011; Lim et al. 2010; Lindsley et al. 2012; Menzies et al. 2000; Milton et al. 2000; Myatt et al. 2004; Nielsen et al. 2010; Qian and Li 2010; Qian et al. 2010; Stockwell et al. 2019; Sun et al. 2011; Tung and Hu 2008).
Although these conclusions led into significant revisions and changes of the recommended ventilation rates on relevant standards and guidelines, over the last years, new findings indicate that the increase of ventilation rate might lead to the increase of the cross-infection risk. This is due to the fact that higher ventilation rates under specific conditions increasing the buoyancy forces of the airborne infectious droplets resulting in the increase of aerosol transmission and associated cross-inflection risk. Bolashikov et al. (2012) examined the exposure of a health professional and a patient to the airborne pathogen caused by an infected patient in a hospital isolation room under different ventilation rates. They performed a series of experiments and concluded that at the distance of 1.1 m for the inflected patient the peak concentration of the pathogen is much higher at the ventilation rate of 12 ACH compared to the ventilation rates of 6 and 3 ACH. Pantelic and Tham (2013) evaluated the capability of the ventilation rate to act as a sole indicator of the effectiveness of an air distribution system on the mitigation of airborne infectious disease transmission. They concluded that the increase of ventilation rate can lead to the increase of exposure risk under certain circumstances (e.g. upward airflow, characteristics of local airflow patterns and airflow quality). This evidence indicates that the use of ventilation rate as a sole indicator for the evaluation of the air distribution system’s effectiveness on the control of the infectious airborne transmission is not possible. Mousavi and Grosskopf (2015) noticed again that increasing the ventilation rate is not proportionately effective for reducing the aerosol concentrations in patient rooms. Ai et al. (2019a, b) studied the airborne transmission between an infected and a healthy person under exposed to a horizontal air flow. They also confirmed that the influence of ventilation rate is not straightforward to the expose index. The obtained experimental results indicated a decrease of the exposure index when the ventilation rate was increased from 2 to 3 ACH and from 6 to 9 ACH, while the increase from 3 to 6 ACH resulted a decrease of exposure index. Similar findings have also been reported (Marshall et al. 1996; Memarzadeh and Xu 2012). It is worth noticing that the above-mentioned studies did not neglect neither the role and the importance of ventilation rate nor the contribution on minimising the airborne transmission. In general, the ventilation rate based on the quantity dilutes the concentration of the infectious airborne bio-aerosols and decreases the risk of transmission. However, based on the velocity and on the air flow pattern, the ventilation rate may lead to the increase of transmission risk. These contradictory effects need to be further studied and evaluated in parallel during the design stage of the ventilation system considering the specific requirements and/or operations of the serviced space.
In addition to the above-mentioned studies, reviews on the role of ventilation rate to the transmission of the airborne infection may be found (Li et al. 2007; Memarzadeh and Xu 2012; Sundell et al. 2011).
The role of space heating and cooling emission system
Space heating and cooling emission units are used to provide energy to end-use space in order to maintain the desirable thermal environment. In general, and considering the main heat transfer mechanism, these units are categorised as free-convention or convector unit, forced-convention or fan-coil unit and radiator or radiant panel unit, or radiant floor/ceiling/wall system. The operation of a convector/ radiator unit or system is associated with thermal plumes that affect the air movement, while a forced-convention unit increases the air velocity in the occupied zone. Both phenomena in conjunction with the ventilation type introduce different temperature and pressure stratification conditions on horizontal and vertical directions; which finally affect the contaminants distribution and the dispersion of the airborne agents into the internal spaces. Several studies analyse the effect of space heating and cooling terminal units in association with different mechanical ventilation systems on the dispersion of pollutants and biological agents. Causone et al. (2010a, b) studied the effect of floor heating system in conjunction with upward displacement ventilation in an experimental chamber. They found that due to the influence of the thermal plume, the actual airflow pattern was between mixing and displacement ventilation, and in case of contaminants production from a heat source, high ventilation rates are required to achieve high ventilation effectiveness. Wu et al. (2014) analysed the ventilation effectiveness of mixing and upward displacement ventilation patterns with floor and ceiling heating systems. They reported that both systems have slightly similar ventilation effectiveness that ranges between 0.97 for the ceiling heating with mixing ventilation system up to 1.14 for the floor heating with displacement ventilation one. Lipczynska et al. (2015) compared the effectiveness of a personalised ventilation with chilled ceiling system against to mixing ventilation, chilled ceiling combined with mixing ventilation and chilled ceiling combined with mixing ventilation and personalised ventilation. They concluded that evaluated personalised ventilation systems was up to 10 time more efficient compared to mixing ventilation ones, and resulted a strongest protection of the occupants from the cross-infection. Jurelionis et al. (2018) accessed the capability of a conjugated floor heating and mixing ventilation system on the dispersion of the air pollutants. They reported that the use of floor heating increased the effectiveness of pollutant dispersion by 5% and reduced the exposure of the occupants by 22% on average. Choi et al. (2019) measured the contaminants concentration profiles in a hospital ward equipped with radiant panel and displacement ventilation. They stated that the heat plume generated by the vertical radiant panel strongly affects the diffusion of the contaminated air. In case of heating operation, the use of radiant panel increases the exposure of a lying patient as the contaminant air is trapped above the lying level. In contrast, during the cooling operation the downward plume drives the exhaled contaminant to the lower high than that of the lying patient, and thus increasing the contaminants concentration in the near to floor levels of the ward. These results proved that the location of the radiant panel and its thermal operation are import parameters which strongly influence the contaminants concentration on the specific levels of the hospital ward. Similar results have also been reported (Causone et al. 2010a, b; Cetin et al. 2020b; Jurelionis et al. 2016; Liu et al. 2019a, b, c, d, e; Olesen et al. 2011; Ouazia et al. 2012; Ouazia et al. 2011; Schiavon et al. 2015; Shi et al. 2019; Wu et al. 2015; Wu et al. 2019a, b; Wu et al. 2020; Zhou et al. 2017). In addition to that, a comprehensive review on the integrated radiant heating and cooling systems in conjunction with the ventilation ones has been reported by Zhang et al. (2020a, b, c, d).
Computer modelling of particles and biological agents’ airborne transmission into indoor built environment
Undoubtedly, mathematical models have proven their value for predicting the high risk and impact of the chemical-biological agents’ exposure on building environment and public health (Argyropoulos et al. 2016, 2018; Bongers et al. 2008). According to Milner et al. (2011) in order to investigate numerically the indoor exposure, a selection of the three following types of IAQ models, namely statistical regression (Valero et al. 2009), micro-environmental (Duan 1982) and CFD models (Béghein et al. 2005; Choi and Edwards 2008, 2012), should be made. The first type involves models employing empirical and semi-empirical approaches to associate indoor environment exposure with significant parameters such as building characteristics, contaminant concentration levels and source strength. The second type of model, adopts the ‘well-mixed’ zone simplification assumption (Axley 2007, 1989; Emmerich 2001) at the building interior for the temperature and contaminant concentration levels and can be further classified into the mass balance (Gerharz et al. 2009; Shrubsole et al. 2012), measurement-based (Kornartit et al. 2010; Ozkaynak et al. 2007), sub-zonal (Megri and Haghighat 2007; Stewart and Ren 2006) and multi-zone models (Argyropoulos et al. 2017a, b; Ashraf et al. 2016; Zhu et al. 2020).
CFD models could be a superior alternative approach to surpass the limitation of the ‘well-mixed’ assumption which does not always hold true especially for non-uniform concentrations in large spaces and transient state (Wang and Chen 2007, 2008a; Wang et al. 2010a, b). CFD models are capable of predicting the airborne transmission of aerosols in indoor spaces, by providing valuable insights into a number of driving factors of the phenomenon such as ventilation system, droplet formation mechanisms, concentrations, turbulence effects, ambient temperature, relative humidity for the survival capability of the agent and on airflow and agent deposition in human airways. However, these models are more computational demanding but more accurate.
A coupling approach of multi-zone and CFD models is preferable for a compromise between computational demands and accuracy (Argyropoulos et al. 2017b; Argyropoulos et al. 2020; Srebric et al. 2008; Wang and Chen 2008a). For detailed evaluation of the all above models, the interested reader is directed to the review papers by Milner et al. (2011) and Wang and Zhai (2016). In the following two subsections, it is presented a review of numerical studies focused mainly on the use of multi-zone and CFD models, as well as its coupling, for investigating the dispersion of airborne pathogens within indoor spaces. Numerical studies related to aircraft and vehicle cabins fall out of the scope of the present study. Finally, few numerical studies based on CFD-PBTΚ (Physiologically-Based ToxicoKinetic) models are also mentioned. This class of models is capable of approximating the kinetic behaviour of contaminants and as a result can assess the internal dose at targeted tissues/organs (Argyropoulos et al. 2018; Feng et al. 2021; Mumtaz et al. 2012).
Single-zone and microenvironment models
This class of models is based on semi-empirical and empirical approaches which include empirical correction factors for a great variety of ingress and egress configurations, as well as different room characteristics. Mass balance models also known as dilution models are deterministic and can be also used for the prediction of indoor contaminant concentrations in different rooms or buildings both spatially and over time.
Chao and Tung (2001), developed an empirical model for the investigation of I/O ratio based on the ventilation influence using a non-steady-state mass balance approach. They found that the air exchange rate has a crucial role to the penetration of outdoor pollutants into residential buildings.
Özkaynak et al. (2008) performed numerical simulations using HAPEM model for estimating the inhalation exposures for over 30 gaseous and particulate pollutants, by examining 37 microenvironments (MEs). The numerical results obtained showed that the predictions are appear to be influenced by the exposure concentration levels due to their dependence on the pollutant type, activity and site. Similarly, Borrego et al. (2006) studied numerically the exposure of concentration levels using an indoor/outdoor function (additional source term) to their model.
A large number of numerical studies has also been devoted to investigate PM (Dimitroulopoulou et al. 2001; Dimitroulopoulou et al. 2006; Nazaroff 2004), element PM (Lunden et al. 2003a, b), airborne bacteria and fungi (Nazaroff 2016), among other contaminants such as CO, Rn, NO2, VOCs and O3 (Briggs et al. 2003; Hicklin et al. 2018; Lee et al. 2004; Li and Niu 2007; Lunden et al. 2003a, b; Mölter et al. 2012).
Multi-zone models
Multi-zone airflow modelling is characterised by great capabilities for simulating the building infiltration, exfiltration and ventilation effects into indoor spaces. Multi-zone models are constituted by a network of elements which represents flow paths (e.g. fans, doorways, opening, cracks and HVAC ducts) among different zones of a building (Fig. 10). Consequently, the air flow rate is calculated from one zone to another as a function of pressure drop along a flow path.
There are many multi-zone simulation programmes such as AIRNET (Walton 1989), CONTAM (Dols and Polidoro 2015; Walton and Dols 2005), COMIS (Feustel 1999; Feustel et al. 1989), BREEZE (Evers and Waterhouse 1978) and CBSAIR (Haghighat and Rao 1991) to name only a few; however, the most popular are CONTAM by the US National Institute of Standards and Technology (NIST) and COMIS by Lawrence Berkeley National Laboratory (LBNL). The first is the most widely used, while a validation study of the last two multi-zone models can be found in the work of Haghighat and Megri (1996). More details for the multi-zone models, the interested reader is directed to the comprehensive reviews by Axley (2007; 1989), Feustel and Dieris (1992) and Emmerich (2001).
According to Dols and Polidoro (2015), the transient partial differential equations for the description of airflow in CONTAM are specified as follows in Eq. (1):
where t is the time, mi the mass of air for zone i, Vi the volume for zone i, ρi the density for zone i, Fij the air flow rate from zone j to i and Fi non-flow processes for zone i (remove or add significant amounts of air from i zone). The above terms Fij and mi can be calculated by using the following formulas (Dols and Polidoro (2015)):
where Pi is the pressure for zone i, Pj the pressure for zone j, f (Pj – Pi) the function of pressure drop n along the flow path, Ti the temperature for zone i and R the ideal gas constant.
Kowalski et al. (2003) performed a multi-zone analysis using CONTAMW (Dols et al. 2000) software for predicting concentration levels and inhaled doses against intentional releases of biological agents into a 40-story commercial office building. They investigated the performance of different cleaning systems such as air-cleaning and air-disinfection systems. They concluded that the combination of ultraviolet germicidal irradiation (UVGI) and filtration as air-cleaning strategy can provide encouraging protection for the occupants and there is no significant improvement beyond the following selected characteristics, i.e. 15% outside air ventilation, filtration of MERV 13–15 and UVGI dose of 1000 μW-s/cm2, for the considered 40-story commercial office building.
An early attempt to conduct multi-zone airflow simulations using CONTAM for studying the severe acute respiratory syndrome (SARS) virus airborne transmission among flats in Block E of the Amoy Gardens was undertaken by Li et al. (2004a, b) and Yu et al. (2004). The numerical results, which describe the evolution of virus spread, presented encouraging agreement with the observed spatial infection data. They concluded that the airborne transmission route was the main reason of SARS spread and building infiltration along with natural ventilation have a positive influence on the infection control. Few years later, Chen et al. (2011) using multi-zone modelling in conjunction with experimental measurements in an environmental chamber found that the air exchange which caused by small temperature differences between cubicles has also significant effect on the transmission of the SARS virus.
Ren and Stewart (2005) modified COMIS with sub-zones (COwZ) for investigating the occupational personal exposure to pollutant sources in a ventilated room. The numerical results were validated by available experimental measurements and CFD data, exhibiting good agreement. They found that the impact of occupant’s location and orientation has significant influence and should be considered for the personal exposure assessment.
Some years later, Lim et al. (2011) performed field measurements of pressure and numerical simulations using CONTAMW to predict both concentration levels and airflow evaluation of virus (H1N1) spread in tall Hospital buildings. Their numerical results showed the possibility of airborne transmission of pathogens through the stack effect within high-rise hospital buildings, presenting encouraging agreement with measurements excluding a few floor cases. Preventive and protection measures were also suggested for minimising the virus spread.
Emmerich et al. (2013) conducted numerical simulations using CONTAM for assessing different control strategies to reduce the dispersion of airborne pathogens (e.g. tuberculosis and squame cells) into a hypothetical hospital. The obtained numerical results indicated that the use of HEPA or MERV-15 filtration have a positive effect on the protection of occupants over pollutant dispersion, as well as UVGI systems. Finally, they also observed that increasing the interior wall leakage by a factor of 5 leads to decrease of pressure difference by a factor of 2.
Recently, numerical simulations were undertaken by Karakitsios et al. (2020) using CONTAM for a hypothetically release of a contaminant within a high-rise building. The simulations examined different scenarios for meteorological conditions, building operational characteristics and source types and location. The obtained results showed that all rooms with ventilation appeared pollutants and there was also transfer of pollutants through leakages towards the stairwell and elevators. Finally, they suggested potential locations for the installation of sensor technologies in order to detect indoor chemical-biological agents.
The same year, Zhu et al. (2020) investigated experimentally and numerically the ventilation effect in two actual building geometries (residence halls) during an entire flu season. By collecting CO2 measurements, they calibrated multi-zone models (CONTAM) in order to simulate airborne transmission of influenza A within adjacent rooms and predict the concentration levels (exposure) for room occupants. The opening doors and windows of dormitory rooms within low ventilated building can improve the ventilation rates, however, this operation sacrifices the thermal comfort (e.g. low outdoor temperatures) of the room occupants. Their numerical results indicated that there is a strong trend between the low outdoor air supply and respiratory infection rates into dormitory rooms; however, more studies are needed to confirm their findings. They also concluded that the cross-infection risk for airborne transmission of influenza A should be considered based on the airflow map rather than the spatial distribution among the occupants’ rooms.
Computational fluid dynamics models
In many cases, computational fluid dynamics (CFD) modelling is the best alternative for investigating the airborne transmission in indoor ventilated spaces, as well as the transmission from human body motion, talking, coughing and breathing.
The mathematical representation of air flow in indoor spaces, based on the set of elliptic, partial differential equations, expressing the mass conservation, momentum, continuity, energy, chemical species concentration and turbulence parameters can be all written in the following general form (Eq. (4)) (Patankar 1980):
where ρ is the air density, t the time, \(\phi\) the dependent variable (u, υ or w for momentum, 1 for continuity, h for enthalpy, c for chemical species concentration, k the kinetic energy of turbulence and ε the eddy dissipation rate), u is the velocity vector of air, \({\Gamma }_{\phi }\) the effective exchange coefficient of variable \(\phi\) (1 for continuity) and \({S}_{\phi }\) the source/sink term of variable \(\phi\). The four terms in Eq. (4) represent the unsteady, convection, diffusion and source terms, respectively.
An important factor of CFD modelling for examining the airborne transmission in indoor built environments is the effect of turbulence motion on the pathogen spread and mean flow field. In the literature, the most of the relevant CFD studies are based on Reynolds-Averaged Navier Stokes (RANS) models (Satheesan et al. 2020; Tao et al. 2020; Wang et al. 2020; Ye et al. 2020; Zhang et al. 2020a) for treating turbulence, and only several Large Eddy Simulation (LES) studies (Berrouk et al. 2010; Liu and You 2011; Tian et al. 2007; Vuorinen et al. 2020; Zhang et al. 2019) have been conducted the previous decades, however, an increasing number of new LES articles due to the SARS-CoV-2 pandemic period is published, as well as an integrated DNS approach for the prediction of cough/sneeze flows by Diwan et al. (2020).
In general, the selection of the appropriate turbulence model for predicting airflow and cross-infection risk in ventilated spaces including the dispersion of airborne pathogens among occupants (e.g. through talking, sneezing, breathing, coughing) is of great challenge due to the complexity of the physical phenomenon (e.g. human body micro-environment, buoyancy, contaminant concentrations, convection, circulation, reattachment and vortices (Zhai et al. 2007). Regarding RANS models for human body micro-environment, the most used are the RNG k-ε and low Reynolds number k-ε (Gao and Niu 2005; Nielsen 2015). An interesting evaluation and comparison of eight different turbulence modelling approaches (i.e. RNG k-ε, SST k-ω, low Reynolds number Launder & Sharma (LRN-LS) k-ε, v2-f), detached Eddy simulation (DES) and LES) and available experimental data from the literature for the prediction of airflow in enclosed environments can be found in the work of Zhang et al. (2007). Subsequently, Phuong and Ito (2015) compared four different turbulence models (LRN-LS k-ε, LRN-ΑΚN (Abe-Kondoh-Nagano) k-ε, RNG k-ε and SST k-ω) against PIV measurements for investigating the flow distribution in upper human airway including oral and nasal inhalation. More details about the equations, advantages, limitations and implementation of different turbulence modelling approaches, the interested reader is directed to the review paper by Argyropoulos and Markatos (2015). Finally, a recent paper by Foster and Kinzel (2021) also presents a useful comparison between CFD models and Wells–Riley mathematical models for SARS-CoV-2 spread into classrooms.
Another important parameter to investigate pathogens transport and trajectory using advanced CFD techniques is the selection of the suitable multiphase model in order to study phenomena such as droplet evaporation, turbulence dispersion forces, droplet breakup and coalescence, among others (Dbouk and Drikakis 2020a; Löhner et al. 2020). It is common practice to choose an Eulerian approach for the gas phase, while the particle (bioaerosol) transport can be simulated using both a Lagrangian or an Eulerian method (Crowe et al. 1996). According to Eulerian–Lagrangian approach, the liquid phase is treated by a Discrete Droplet model; while for the Eulerian-Eulerian method, a Continuum Formulation model is adopted (Novozhilov 2007). Both methods have advantages and drawbacks, while many researchers have investigated extensively their limitations and applications (Zhang and Chen 2007). The mathematical formulation of the aforementioned models along with useful information for their implementation is not repeated herein, due to space limitations, but it may be found in the classical textbooks by Yeoh and Tu (2010), Brennen (2005), and Azzopardi (2006) and review papers by Crowe et al. (1996), Peng et al. (2020). Finally, the equations for the motion of particles/droplets and virus loads may be found (Löhner and Antil 2020; Löhner et al. 2020).
Numerical studies focused on the infection spread into chambers and offices
SHAO et al. (2021) performed CFD simulations using OpenFOAM in conjunction with in-situ measurements to investigate the airborne transmission risk of SARS-CoV-2 by asymptomatic individuals into small classroom, elevator and supermarket. They found that the design of ventilation system in confined spaces plays a major role in the particle removal and deposition. Bad design of ventilation system results in decreasing of particle removal efficiency and increasing of particle deposition in which both increase the risk of contamination. Similarly, Vuorinen et al. (2020) investigated numerically the dispersion and inhalation of droplets in relation to SARS-CoV-2 for open office and supermarket, using an LES approach (Fig. 11). They examined four different open sources CFD codes, namely, PALM, FDS, OpenFOAM and NS3dLab, while a number of Monte Carlo simulations was also conducted to investigate susceptible and infected individuals.

Reproduced from Reference (Vuorinen et al. 2020) with permission from Elsevier
Visualisations demonstrating the effect of particle size (and mass) on the modelled spreading of the cough-released aerosol cloud. For better sense of scale, bystanders are placed 8 m from the coughing person. Instantaneous views on the state of the cloud are shown for realisations where the particles have a no mass, b 1000 kg m−3 density and 10-μm diameter and c 1000 kg m−3 density and 20-μm diameter. Images on the left column are at t = 20 s and on the right column at t = 120 s. Below, d presents the time evolution of the mean elevation of the 99th percentile concentration highlighting the different descent rates. Droplets in these size scales have τevap < 1 s and they would become aerosol-like droplet nuclei very rapidly.
Several relevant LES studies, including ventilation effects, different sub-grid scale models (e.g. WALE, Deardorff model, Smagorinsky) and CFD codes (e.g. ANSY FLUENT and CFX, PHOENICS, OpenFOAM, Star-CCM +), have also published in the literature (Béghein et al. 2005; Berrouk et al. 2010; Choi and Edwards 2008, 2012; Dudalski et al. 2020; Feng et al. 2020a, b; Fontes et al. 2020; Karakitsios et al. 2020; Pendar and Páscoa 2020; Tian et al. 2007; Zhang et al. 2019). It is worth mention that Diwan et al. (2020) also developed a DNS approach for the prediction of cough/sneeze flows. According to their temperature profile results, the dry cough (without liquid droplets) flow was dispersed very fast (cough duration of 0.58 s) at a distance of more than 1 m.
Pendar and Páscoa (2020) proposed a fully coupled Eulerian–Lagrangian method based on the OpenFOAM code for investigating the dispersion of saliva microdroplets generated by sneeze and cough in indoor environment. Their numerical results showed that the use of mask and a full bending of our head during sneeze can reduce significantly the risk of infection. More specifically, the latter action can cause decreasing of the microdroplets travelling distance by > 22%, while the first action can restrict the risk infection in a transmission sphere area of 0.6 m diameter. They also claimed that the social safety distance of 2 m should be increased to 4 m for providing more effective protection.
Feng et al. (2020a, b) conducted LES using ANSYS 17.0 in order to investigate the influence of human microenvironment on the transmission of infection diseases via microbial particles during human respiratory. They showed that an increase of heat flux leads to increase of the air flow flux of the thermal plume, resulting in a further increase of thermal plume ability to transfer particles upward. One year later, Zhang et al. (2019) employed an LES model combined with Lagrangian approach for studying the spread and transmission of bacteria and virus in a ventilated room. The numerical results obtained compared with experimental data from a climate chamber, presenting good agreement. They concluded that the droplet cloud velocity, which is characteristic for respiratory activities such as coughing and breathing, has great influence on the accuracy of the simulation. Choi and Edwards (2012) investigated via LES combined with an Immersed Boundary Method, the contaminant spread in room compartments. The immersed boundary method used for considering heat transfer effects and passive scalar advection. The numerical results obtained were validated by available experimental and CFD data, exhibiting good agreement. Fontes et al. (2020) performed DES for the investigation of human physiology factors (e.g. nasal and buccal passages, with or without teeth) during the human respiratory event of sneezing on the airborne virus transmission. They found that saliva properties have significant effect on the spray formation (i.e. droplet distribution, primary and secondary break-up mechanisms). They also claimed that women seem to be less effective on the transmission of airborne pathogens.
Special attention has also been given to pathogen transmission using Reynolds-averaged Navier Stokes (RANS), unsteady Reynolds-averaged Navier Stokes (URANS) and Reynolds Stress (RS) models associated with ventilation strategies for particle removal and dispersion (Cetin et al. 2020a; He et al. 2011; Katramiz et al. 2020; Murga et al. 2020; Park and Chang 2019; Shao et al. 2020; Wang et al. 2020), human movement (Li et al. 2020; Tao et al. 2020; Tao et al. 2019), comparison of Eulerian-Eulerian and Eulerian–Lagrangian approaches for the pathogens transport and trajectory (Yan et al. 2020) and human expiratory events (e.g. coughing, sneezing, speaking) (Chen and Zhao 2010; de Oliveira et al. 2021; Kang et al. 2015; Li et al. 2018; Licina et al. 2015; Liu et al. 2016a, b; Yan et al. 2019; Zhang et al. 2020a, b, c, d; Zhu et al. 2006), among others.
Ji et al. (2018) investigated numerically the effects of evaporation process of pure water droplet under different RHs (0%, 30%, 90%) and ventilation strategies (displacement and mixing). They concluded that the evaporation process for small droplets occurs rapidly and it is difficult to observe differences between mixing and displacement ventilation. However, RH has small effect on large droplets’ deposition, while displacement ventilation can delay evaporation similar to high RH.
Al Assaad et al. (2018) and Katramiz et al. (2020) performed numerical simulations using the RNG k-ε turbulence model for the investigation of intermittent personalised ventilation with respect to the protection of occupants from indoor contaminants. Their results showed that a selected average flowrate of 7.5 L/s along with an operating frequency of 0.86 Hz are acceptable for providing good ventilation and thermal comfort conditions in order to protect occupants. They also extended their study for the effect of walking occupant on the personalised ventilation in an office (Al Assaad et al. 2019a) and particle resuspension in a prayer room related to human prostration cycle (Al Assaad et al. 2019b). They concluded that the human prostration cycle due to prayers plays an important role in the particle spread from the floor to the upper levels of the confined space, while higher risk of contamination in the breath zone was found in the case of 1 μm particle concentration compared to 10 μm, according to the examined scenarios.
Dbouk and Drikakis (2020a) conducted RANS simulations combined with the k-ω turbulence model, by using the open-source code OpenFOAM. They investigated the spread of saliva droplets generated from a human cough in order to predict the influence of wind on social distancing. Their results showed that in the absence of wind effect the majority of exhaling saliva droplets during a cough can travel up to 1-m distance, while a small number can be travelled further. However, these droplets present low risk due to the low trajectory (< 1 m height). On the other hand, with the presence of wind speed in the range of 4–15 km/h, the travelled distance of the saliva droplets can reach up to 6 m, which is much farther than the recommended social safety distance of 2 m. Dbouk and Drikakis (2020c) presented a continuation of their previous study (Dbouk and Drikakis 2020a) with the aim at extending their work to consider the unsteady evaporation process of the saliva droplets, relative humidity, temperature and wind speed. They concluded that the low relative humidity combined with high temperature foster the droplet evaporation rate, resulting in significant reduction of virus viability. Similarly, Feng et al. (2020a, b) examined the transmission of SARS-CoV-2 droplets between two human bodies by means of RANS approach including evaporation and condensation effects (Fig. 12). They showed that the recommended social distance of 1.83 m (6 ft) is not sufficient to provide protection to people, under different wind conditions and static air environment (exposure at 3.05 m (10 ft)), from SARS-CoV-2 during coughing. Moreover, deposition and transport of droplets are dependent on the wake flow patterns and secondary flow between the two human bodies. Their results also indicated that high RH (99.5%) increases the deposition of droplets in the space, however, without increasing necessarily the risk of exposure. On the other hand, medium RH (40%) fosters the water evaporation phenomenon, resulting in decreasing of droplet diameter and remaining airborne for longer times. Similar studies including evaporation and condensation effects results obtained for coughing from one person have also been reported (Chen and Zhao 2010; Li et al. 2018; Yan et al. 2019).
Numerical studies focused on the infection spread in hospitals and patient wards
A large number of numerical studies have been undertaken by many scientists and engineers for preventing the nosocomial airborne infection in hospitals and patient wards including ventilation and turbulence effects (Qian and Li 2010; Saarinen et al. 2015; Seymour et al. 2000; Shajahan et al. 2019; Wan et al. 2007; Yang 2013), while the current number of relative published papers (Anghel et al. 2020; Borro et al. 2020; Gu et al. 2020; Satheesan et al. 2020; Villafruela et al. 2019; Wang et al. 2021) is continuously increasing due to SARS-CoV-2 pandemic. This is mainly attribute to the strong interest in the SARS-CoV-2 Coronavirus modes transmission among patients, visitors and healthcare personnel in order to protect them.
An early attempt to perform RANS computations using a k-ε turbulence model for the prediction of airborne pathogens transmission in a hospital isolation room, including the effects of ventilation systems, was undertaken by Seymour et al. (2000). Furthermore, Li et al. (2004a, b) conducted CFD simulations to investigate the spread of virus-laden bio-aerosols in a hospital ward during SARS outbreak in Hong Kong, by using the commercial CFD code Fluent 6.1. The numerical results showed that the predicted spread of the viral respiratory disease is in good agreement with the reported SARS cases. Chau et al. (2006) also examined the effects of the local exhaust ventilation system in a hospital patient ward for the protection of healthcare workers from virus diseases such as SARS.
Huang and Tsao (2005) presented numerical and experimental results for the removal of airborne pathogens in negative pressure isolation rooms. Their results showed that the buoyancy effects play an important role to flow and the removal of bacteria, while the redesign of the isolation room can improve the pathogen’s removal. Qian and Li (2010) performed numerical simulations and experiments for studying the ventilation and deposition effects in a six-bed room. They presented CFD simulations using the RNG k-ε turbulence model along with a Lagrangian method for the prediction of particles trajectory. The numerical results, which describe the characteristics of the flow and the distribution of exhaled particles, indicated that the removal of particles is achieved more efficiently by ceiling-level exhausts compared to floor-level exhausts. In a similar way, Yang (2013) investigated the different types of ventilation in a four-bed sickroom using the commercial CFD code Star CD, while Chao et al. (2008) presented numerical and experimental results for the characteristics of the expiratory droplets in a three-bed hospital ward. Recently, Satheesan et al. (2020) presented numerical results for the Middle East respiratory syndrome coronavirus (MERS-CoV) in a six-bed inpatient ward.
King et al. (2015) also exhibited CFD simulations using an RSM closure model in conjunction with particle deposition data for predicting the cross-contamination risk among healthcare workers in single- and four-bed isolation rooms. Their results showed that the cross-infection risk in a single-patient room can be decreased significantly, while the ventilation, infection patients’ location, type of patient’s care and room layout may also affect the infection spread inside four-bed rooms (Sadrizadeh et al. 2014a, b; Sadrizadeh et al. 2018; Sadrizadeh et al. 2014a, b) and Wang et al. (2019a, b) studied numerically the effects of door opening on airborne particle movement, as well as the ventilation and stuff number in operating rooms during simulated surgery. They concluded that the use of a positive-pressure system can be more effective to reduce the airborne particle spread, while the door opening combined with the ventilation system and increased number of staff may expand the contamination risk for the patient into the surgical site.
Borro et al. (2020) performed URANS simulations combined with a Lagrangian approach for the investigation of ventilation system at the Vatican State Children’s hospital (Fig. 13). The numerical results indicated that the proposed methodology is capable of predicting the contamination risk and optimising the ventilation flow in hospitals. They also showed that the installed HVAC system can diffuse the formed droplets from a coughing event, while the turbulence effects of the flow also enhance the pathogens spread and particle suspension for longer time in the room. Finally, they concluded that the use of a LEV unit placed above the face of patients can remove the particles and infected air in just a few seconds after the cough event.
Prospective view of the Scenarios A, B and C at t = 1 s (left) and 5 s (right). The spheres represent the droplets coloured by the diameter size (top right legend). The contaminated air is represented by different iso-surfaces coloured by mass fraction.
Gu et al. (2020) developed and demonstrated a numerical simulation framework based on LES approach and FDS software, for assisting the design of ventilation systems in temporary hospitals, such as the first SARS-CoV-2 Wuhan Huoshenshan hospital in China. The numerical results showed that the proposed methodology is capable of assisting HVAC engineers to select and design the appropriate ventilation system in temporary hospitals. Finally, they claimed that there is no case for contamination risk to the surrounding buildings or the fresh-air intakes due to the release of the infected air from the air outlets of the temporary hospital.
Numerical studies focused on the preventive role of mask against airborne droplet transmission
A significant number of concerns has been raised due to the SARS-CoV-2 pandemic for the efficacy of face masks and coverings in controlling and limiting the transport of infective droplets which are formed during cough and sneeze events. Special attention, therefore, is given to investigate the effectiveness of face masks regarding the transmission of respiratory droplets and the recommended social distancing guidelines, respectively.
An early attempt to investigate the aerodynamics of a gas mask canister numerically and experimentally was undertaken by Li (2009). The numerical and experimental results showed that the proposed methodology can be a useful tool for the design of gas mask canister, even though with a low respiratory drop.
Lei et al. (2012a, b) proposed a CFD approach for the investigation of studying the leakages between a headform and an N95-filtering facepiece respirator (FFR). The numerical results were compared with infrared images of respiratory leakage. Their results also indicated that the use of N95 FFR may cause thermal discomfort due to the temperature increase near the lip. They concluded that the most leak presented at the region of nose (40%), left (26%) and right (26%) cheek. The same group (Lei et al. 2012a, b) also investigated numerically and experimentally the effect of pressure contact on digital headforms.
Dbouk and Drikakis (2020b) performed multiphase CFD simulations for the prediction of the droplet transmission from a headform with and without a surgical mask. Their results showed that during a mild cough event the droplets can reach up to 70-cm distance without the use of surgical mask, and wearing mask the droplets may travel about the half above mentioned distance. They also observed that after 10 cough cycles the efficiency of the surgical mask can be reduced by ~ 8%, while for severe cough events the efficiency drops significantly. Finally, the diameter of the transmitted droplets without the presence of mask on the headform was larger across the cough cycles.
Khosronejad et al. (2020) performed LES using very fine grids for the investigation of saliva droplets transmission during a cough event with and without facial mask (Fig. 14). They also examined the effects of indoor and outdoor conditions during the cough event, namely stagnant background air and unidirectional mild breeze. Their numerical results showed that during a cough event without mask and stagnant background air condition the travelling distance of fine droplets can reach up to 2.62 m, while the larger in diameter droplets fall down in the area between the human and the previous mention distance in less than 2 min.

Reproduced from Reference (Khosronejad et al. 2020) with permission from AIP
Simulated evolution of the 10-µm saliva particulate concentration (volume fraction) after the cough under outdoor conditions (mild breeze) without (top) and with (bottom) the facial mask. [(a) and (f)], [(b) and (g)], [(c) and (h)], [(d) and (i)] and [(e) and (j)] show the simulated saliva particulate concentration fields after 0.24 s, 0.3 s, 0.4 s, 0.5 s and 0.6 s, respectively, on the sagittal plane. The outdoor simulations were stopped after 0.6 s, when the saliva particulates travel ∼2.0 m and 2.2 m without (top) and with (bottom) the facial mask, respectively.
Furthermore, a number of fine droplets can also be remained suspended for several minutes in the air. They also observed that the wearing of a medical and non-medical mask can reduce the travelling distance of saliva droplets at 0.48 m and 0.73 m, respectively. Finally, the droplet evaporation phenomenon can increase the travelling distance to 2.84 m without wearing mask and to 0.91 m for using non-medical mask.
Numerical studies focused on the airflow and aerosols deposition in human airways
CFD modelling can also be helpful to investigate the influence of airflow and aerosols deposition in human airflow. More details regarding the transport of particles and characteristics of the transitional flow mechanisms in the human lungs may be found in the recent review papers by Islam et al. (2020) and Mutuku et al. (2020a).
Ito (2014) proposed an integrated method for investigating the airborne infection transmission of pathogens in a hospital using a combination of CFD and SIR epidemiological models. This approach can allow the consideration of the hospital space in conjunction with the human nasal airway. As a result, the proposed methodology is capable of evaluating the exposure risk of occupants and estimate the contaminant dose. Phuong and Ito (2015) performed RANS simulations using four different turbulence models (i.e. two LRN k-ε, RNG k-ε and SST k-ω) to investigate the airflow in human realistic respiratory tract for three constant breathing conditions (7.5, 1.5 and 30 L/min). The numerical results obtained with LRN-AKN model were compared with PIV measurements, presenting better agreement. Recently, an extension of the previous work was proposed by Phuong et al. (2020).
Haghnegahdar (2019a) et al. developed a Computational Fluid Particle Dynamics (CFPD) model combined with Host Cell Dynamic (HCD) model (Fig. 15) for the prediction of influenza A virus droplets trajectory and deposition in the pulmonary tracts.

Reproduced from Reference (Haghnegahdar et al. 2019a with permission from Elsevier
The framework of the multiscale CFPD-HCD model for the human-to-human IAV infection with a subject-specific airway geometry. The description of the HCD model is given in the ‘The human respiratory system’ section of the original paper (Haghnegahdar et al. 2019a). The detail of the final polyhedral-core mesh is provided at the right nostril and an airway outlet (RUL: right upper lobe, RML: right middle lobe, RLL: right lower lobe, LUL: left upper lobe, LLL: left lower lobe).
Their numerical results showed that the proposed model is capable of predicting the spread of virus and population variations in the upper airways tissues. They also predicted particle deposition fractions values of 26.4%, 23.7% and 24.1% for droplet mass fraction of 0, 0.068 and 0.104, respectively, in the oral cavity, while for the nasal cavity the fraction values are 48.1%, 45.2% and 47.6%, respectively. Finally, the average diameter of deposited droplets on the oral cavity is less than nasal cavity.
Mutuku et al. (2020b) performed CFD simulations for investigating the characteristics of airflow and particle deposition effects of PM2.5 on healthy and Chronic Obstructive Pulmonary Disease (COPD) patients. The numerical results showed that the deposition fractions are between 0.12% and 1.18% for healthy case and between 0.05% and 0.49% for COPD case, while carina 5 was found to be the most important place of particle deposition.
Coupling of multi-zone and CFD models
Multi-zone models suffer from the well-mixing assumption which clearly is not valid in cases for Archimedes number (Ar) smaller than 400 and dimensionless temperature gradient (τ) greater than 0.03 (Wang and Chen, (2008b). To surpass this issue, a combination of a multi-zone model and CFD model can be adopted which is superior for more realistic prediction of pollutant concentration levels and airflow characteristics. The coupling of the models provides a satisfactory compromise between accuracy and computational sources.
Wang and Chen (2008a) presented a coupling approach of CFD and multi-zone model for estimating the concentration levels in case of chemical-biological-radiological agent release within complex three-floor building. They showed that the combination of CFD and multi-zone models is superior and capable of identifying the optimal location of emergency sensors, ventilation strategies for emergency response, as well as to examine proposed routes for evacuation.
Jiang et al. (2009) performed multi-zone simulations for predicting the virus concentration and the required ventilation rate for sufficient air dilution in two Hospitals in Beijing and Guangzhou, respectively. It is worth mentioning that the pressure coefficient was predicted by the commercial CFD software PHOENICS 3.2. (Spalding 1981) and used as input parameter for CONTAM model. Their numerical results were validated against field experiments using tracer gas (SF6), with promising and encouraging results.
Recently, Karakitsios et al. (2020) used COMIS for calculating the inflow and outflow conditions from the openings (windows and doors) and then induced them into ADREA-HF CFD code (Efthimiou et al. 2018; Kovalets et al. 2018) in order to investigate the release of a hazardous agent through the HVAC system in a large office.
CFD-PKTE or CFD-PTBK models
Another interesting combination of models for the investigation of the transport and deposition of particles into human airways is CFD-physiologically based pharmacokinetic (PBPK) or CFD-physiologically based toxicokinetic (PBTK) (Mumtaz et al. 2012), respectively. Recently, Feng et al. (2021) presented a detailed tutorial paper regarding the development, implementation and validation of CFD-PBPK and CFD-PBTK models for investigating the human lung aerosol dynamics numerically.
Yoo and Ito (2018) proposed a computational framework based on CFD, Computer Simulated Person (CSP) and PBPK models for the prediction of inhaled formaldehyde internal dose at human respiratory system. The numerical results indicated that the computational framework is capable of tackling many different types of pollutants and not only the examined formaldehyde. It is also important to mention that the proposed numerical methodology can also provide useful information regarding the exposure to pollutants and health risk assessment into indoor environments. The same group of researchers extended their work (Yoo and Ito (2018) for unsteady breath conditions using the aforementioned computational approach, predicting different concentration levels of formaldehyde inside the room and around the human zone, while for the person breathing zone the concentration values were lower than inside the room.
Murga et al. (2019) conducted health risk assessment in a working environment for the toxic inhalation of breathing air and how affects the human respiratory system, by means of CFD, CSP and PBTK models. The results revealed that the nose area is primarily influenced in all examined cases according to the considered working conditions and there is high risk of acute exposures during the working period.
Haghnegahdar et al. (2019b) also developed a CFD-PTBK model for investigating the transport of xenon gas and how the inhaled dose affects the human body. The numerical results obtained were compared with experimental data, exhibiting good agreement. Finally, the multiscale model is capable of predicting the concentration levels of xenon in the human respiratory system and can also be used for future non-invasive studies regarding patient specific pulmonary diseases.
Conclusions—future directions
The nature and physicochemical characteristics of particles, either those being solids or liquids forming droplets, play an important role in the mode of transmission of a variety of pollutants, contaminants and biological agents in indoor air environments. Understanding the engineering aspects of particle technology plays a major role in designing better depollution or prevention of pollutants and biological agents’ strategies and as a result minimising the risk of transmission in indoor air environments. The current study shade light on the possible gaps and directions for future research in the field of particles transmission in indoor air, focusing especially on biological agents’ transmission:
-
Only a handful of studies conducted with the application of modern techniques capable of detecting sub-micrometer-sized particles, it is important that more work is done in this area to develop a better understanding of the mechanism of droplet generation (Morawska 2006).
-
It is evident that aqueous solution of mucin alone cannot fully represent various physicochemical and biophysical properties of saliva. Systematic studies on designing saliva targeted tribological properties have to be investigated in future (Sarkar et al. 2019).
-
However, studies of how surface contamination is propagated by human touching are scare as there are no experimental data (Xiao et al. 2018).
-
Both studies on the absolute and relative humidity which are known to affect the viral survival need to be further investigated (Poon et al. 2020).
-
The fundamental science underlying the virus –microorganisms transfer mechanisms on soft matter domain (Poon et al. 2020).
-
Studies of how the solid surfaces contamination is propagated by human touching are scarce due to mainly the lack of experimental data (Xiao et al. 2018) due to complexity of such types of experiments and quite intense health and safety protocols, laboratories mainly accessible by medical scientists and difficulties in introducing other disciplines in the field etc.
-
Better understanding the pollutants in general and even more biological agents’ mechanisms in the deeper generation parts of the human tracheobronchial system.
-
The mechanisms of how the droplets are formed near the mouth has not been studied (Vadivukkarasan et al. 2020)
-
Sneezes especially have received much less attention in literature and is a field which needs further investigation (Scharfman et al. 2016).
-
Concentration of biological agents in the droplets (Zhang et al. 2020a, b, c, d).
-
Dependence of evaporation on the temperature and humidity regarding seasonal and geographic variations in transmission rates (Tang et al. 2009).
The installed ventilation system plays significant role on the transmission of the pollutants and biological agents into indoor spaces. The positive and/ or negative influences of either mechanical systems or natural one have been extensive analysed and documented in a series of studies. Hereafter some of the main conclusions regarding HVAC systems are summarised:
-
Mixing ventilation leading to well-mixed homogeneous bio-aerosols and high dispersion rates, regardless of the droplet sizes.
-
Upward displacement ventilation provides high efficiently removing of small size droplets.
-
Downward displacement ventilation is ideally removing the contaminated indoor air, and minimise the cross-infection risk.
-
Human’s thermal plume and walking velocity are significantly influence the dispersion mechanism and kinetics of the bio-aerosols.
-
Relative position and orientation among occupants are critical parameters that influence the cross-infection risk. Face-to-face position and upward exhaled bio-aerosol airflow are of high cross-infection risk.
-
Personalised ventilation decreases the cross-infection risk of the user and increases the risk of cross-infection to the non-personalised occupants of the space.
-
Natural ventilation minimises the cross-infection risk due to high airflow rates and mixed airflow distribution; however, in some cases, the concentration of pollutants in the unfiltered air is significant high.
-
Thermal plumes from radiant heating and convective heating and cooling panels strongly influence the contaminants concentration and the associated cross-infection risk. In general, upward thermal plumes in-line with the airflow pattern have positive effect on the dispersion of airborne agents, while the downward of crossflow ones might need higher airflow rates in order to maintain the ventilation effectiveness.
In addition to the above reporting findings, it is worth noticing that today the main scientific interest on ventilation systems has been turn to the more sophisticated ones, such as personalised systems, which still remaining in a developing stage. The opportunities for future research and the still remaining open research questions in this area have been recently presented by Zhai and Metzger (2019).
Since the 1970’s, the first documented attempts to use CFD in ventilation industry (Chow 1996; Nielsen 2015), the progress of CFD has been tremendous for indoor environments, with promising results for the prediction of pollutant dispersion and concentration levels, as well as for the design of ventilation strategies. Nowadays, the further development of CFD techniques along with the continuing progress of computer-hardware development has established the use of CFD as the main tool for the prediction of air movement and design of HVAC systems for the controlled ventilation of indoor spaces. In the current pandemic of SARS-CoV-2, CFD simulations have played a major role to investigate the airborne saliva droplets transmission among people in enclosed spaces. Below, we present some final comments regarding the aforementioned computational approaches for the pollutants in general and biological agents’ airborne transmission into indoor built environment:
-
Human’s thermal plume and walking velocity are significantly influenced by the dispersion mechanism and kinetics.
-
More research should be devoted to evaluate the probability of droplet vs. viral transmission during airborne droplets transport and coughing (Dbouk and Drikakis 2020a).
-
Regarding face masks and protection from the dispersion of airborne infected saliva droplets further research must be directed to the composition, properties of saliva droplets and mask high-filter efficiency for the prediction of airborne droplet transmission (Dbouk and Drikakis 2020b).
-
LES seems to be the most appropriate method for practical computation for the investigation of droplet transmission, however, it is time consuming and computationally demanding. Furthermore, there are still challenges such as the development of advanced sub-grid scale models, high-order discretisation schemes for the elimination of the numerical errors, implementation on unstructured grids, and interaction with other physical mechanisms (Argyropoulos and Markatos 2015).
-
The combination of CFD and multi-zone models can be very useful for more realistic prediction of pollutant concentration levels and airflow characteristics, and can provide a compromise between accuracy and computational sources.
-
It is important to mention that the CFD-PKTE or CFD-PTBK models for the transport prediction of particles in human respiratory system exhibit many difficulties and should be further improved by developing the next generation of virtual lung computational framework (Feng et al. (2021).
-
There is also a need for further improvement and validation of the current numerical methods in order to be fully capable of predicting accurately complex phenomena of the biopathogens’ transmission mechanisms, such as evaporation, dispersion, droplet distribution, primary and secondary break-up mechanisms, coalescence, turbulence, inhalation and pulmonary transport.
Data availability
Data sharing is not applicable to this manuscript as no datasets were generated or developed during the current study. All the included information has been retrieved from the existing literature.
References
Ahmed N, Glencross H, Wang Q (2016) Biomedical Science practice: experimental & professional skills. Oxford University Press, Oxford
Ahnrud GP, Mendoza AJ, Hurley MJ, Marek PJ (2018) Efficacy of a sonicating swab for removal and capture of microorganisms from experimental and natural contaminated surfaces. Appl Environ Microbiol 84(9):208–218. https://doi.org/10.1128/aem.00208-18
Ai Z, Hashimoto K, Melikov AK (2019a) Airborne transmission between room occupants during short-term events: measurement and evaluation. Indoor Air 29(4):563–576. https://doi.org/10.1111/ina.12557
Ai ZT, Huang T, Melikov AK (2019b) Airborne transmission of exhaled droplet nuclei between occupants in a room with horizontal air distribution. Build Environ 163:106328. https://doi.org/10.1016/j.buildenv.2019.106328
Ai ZT, Mak CM (2014) A study of interunit dispersion around multistory buildings with single-sided ventilation under different wind directions. Atmos Environ 88:1–13. https://doi.org/10.1016/j.atmosenv.2014.01.049
Ai ZT, Mak CM (2016) Large eddy simulation of wind-induced interunit dispersion around multistory buildings. Indoor Air 26(2):259–273. https://doi.org/10.1111/ina.12200
Ai ZT, Mak CM, Niu JL (2013) Numerical investigation of wind-induced airflow and interunit dispersion characteristics in multistory residential buildings. Indoor Air 23(5):417–429. https://doi.org/10.1111/ina.12041
Ai ZT, Melikov AK (2018) Airborne spread of expiratory droplet nuclei between the occupants of indoor environments: a review. Indoor Air 28(4):500–524. https://doi.org/10.1111/ina.12465
Al Assaad D, Ghali K, Ghaddar N (2019a) Effect of flow disturbance induced by walking on the performance of personalized ventilation coupled with mixing ventilation. Build Environ 160:106217. https://doi.org/10.1016/j.buildenv.2019.106217
Al Assaad D, Ghali K, Ghaddar N (2019b) Particles dispersion due to human prostration cycle and ventilation system in a prayer room. Build Environ 150:44–59. https://doi.org/10.1016/j.buildenv.2019.01.005
Al Assaad D, Ghali K, Ghaddar N, Habchi C (2020) Coupled CFD and particle resuspension models under combined effect of mechanical and aerodynamic disturbances. Build Environ 169:106567. https://doi.org/10.1016/j.buildenv.2019.106567
Al Assaad D, Habchi C, Ghali K, Ghaddar N (2018) Effectiveness of intermittent personalized ventilation in protecting occupant from indoor particles. Build Environ 128:22–32. https://doi.org/10.1016/j.buildenv.2017.11.027
Aliabadi AA, Rogak SN, Bartlett KH, Green SI (2011) Preventing Airborne disease transmission: review of methods for ventilation design in health care facilities. Adv Prev Med 2011:124064. https://doi.org/10.4061/2011/124064
Allocca C, Chen Q, Glicksman LR (2003) Design analysis of single-sided natural ventilation. Energy Build 35(8):785–795. https://doi.org/10.1016/S0378-7788(02)00239-6
Anghel L, Popovici C-G, Stătescu C, Sascău R, Verdeș M, Ciocan V, Serban I-L, Mărănducă MA, Hudișteanu S-V, Țurcanu F-E (2020) Impact of HVAC-Systems on the dispersion of infectious aerosols in a cardiac intensive care unit. Int J Environ Res Public Health 17(18):6582 https://doi.org/10.3390/ijerph17186582
Argyropoulos CD, Abraham M, Hassan H, Ashraf AM, Fthenou E, Sadoun E, Kakosimos KE (2016) Modeling of PM10 and PM2.5 building infiltration during a dust event in Doha, Qatar. Paper presented at the 2nd International Conference on Atmospheric Dust, Castellaneta Marina, Italy
Argyropoulos CD, Ashraf AM, Markatos NC, Kakosimos KE (2017a) Mathematical modelling and computer simulation of toxic gas building infiltration. Process Saf Environ Prot 111:687–700. https://doi.org/10.1016/j.psep.2017.08.038
Argyropoulos CD, Ashraf AM, Vechot L, Kakosimos KE (2017b) Coupling multi-zone and CFD models for investigating indoor air quality. Paper presented at the Second International Conference on Energy and Indoor Environment for Hot Climates, Doha, Qatar
Argyropoulos CD, Elkhalifa S, Fthenou E, Efthimiou GC, Andronopoulos S, Venetsanos A, Kovalets IV, Kakosimos KE (2018) Source reconstruction of airborne toxics based on acute health effects information. Sci Rep 8(1):5596. https://doi.org/10.1038/s41598-018-23767-8
Argyropoulos CD, Hassan H, Kumar P, Kakosimos KE (2020) Measurements and modelling of particulate matter building ingress during a severe dust storm event. Build Environ 167:106441. https://doi.org/10.1016/j.buildenv.2019.106441
Argyropoulos CD, Markatos NC (2015) Recent advances on the numerical modelling of turbulent flows. Appl Math Model 39(2):693–732. https://doi.org/10.1016/j.apm.2014.07.001
Asadi S, Wexler AS, Cappa CD, Barreda S, Bouvier NM, Ristenpart WD (2019) Aerosol emission and superemission during human speech increase with voice loudness. Sci Rep 9(1):2348. https://doi.org/10.1038/s41598-019-38808-z
ASHRAE (American Society of Heating Refrigerating and Air-Conditioning Engineers) (2017a) ANSI/ASHRAE/ASHE 170:2017 Ventilation of health care facilities. American Society of Heating Refrigerating and Air-Conditioning Engineers (ASHRAE) Inc., Atlanta
ASHRAE (American Society of Heating Refrigerating and Air-Conditioning Engineers) (2017b) Ventilation and infiltration. In American Society of Heating Refrigerating and Air-Conditioning Engineers (ed) ASHRAE Handbook of Fundamentals 2017. American Society of Heating Refrigerating and Air-Conditioning Engineers, Atlanta, pp 16.11–16.39
ASHRAE (American Society of Heating Refrigerating and Air-Conditioning Engineers) (2019a) ANSI/ASHRAE Standard 62.1:2019 Ventilation for acceptable indoor air quality. American Society of Heating Refrigerating and Air-Conditioning Engineers (ASHRAE) Inc., Atlanta
ASHRAE (American Society of Heating Refrigerating and Air-Conditioning Engineers) (2019b) ANSI/ASHRAE Standard 62.2:2019 Ventilation and acceptable indoor air quality in residential buildings. American Society of Heating Refrigerating and Air-Conditioning Engineers (ASHRAE) Inc., Atlanta
Ashraf AM, Argyropoulos CD, Olewski T, Vechot L, Kakosimos KE (2016) Comparative study on toxic gas infiltration in a nonprocess area using CFD and multi-zone models. Institution of Chemical Engineers. https://www.icheme.org/media/11816/hazards-26-poster-11-comparative-study-on-toxic-gas-infiltration-in-a-non-process-area-using-multizone-and-cfd-models.pdf. Accessed 24 Nov 2022
Axley J (2007) Multizone Airflow modeling in buildings: history and theory. HVAC&R Res 13(6):907–928. https://doi.org/10.1080/10789669.2007.10391462
Axley JW (1989) Multi-zone dispersal analysis by element assembly. Build Environ 24(2):113–130. https://doi.org/10.1016/0360-1323(89)90001-2
Azimi P, Stephens B (2013) HVAC filtration for controlling infectious airborne disease transmission in indoor environments: predicting risk reductions and operational costs. Build Environ 70:150–160. https://doi.org/10.1016/j.buildenv.2013.08.025
Azzopardi BJ (2006) Gas-liquid flows. Begell House, New York
Balachandar S, Zaleski S, Soldati A, Ahmadi G, Bourouiba L (2020) Host-to-host airborne transmission as a multiphase flow problem for science-based social distance guidelines. Int J Multiph Flow 132:103439. https://doi.org/10.1016/j.ijmultiphaseflow.2020.103439
Bansal R, Sharma D, Singh R (2018) Tuberculosis and its treatment: an overview. Mini Rev Med Chem 18(1):58–71. https://doi.org/10.2174/1389557516666160823160010
Barmby T, Larguem M (2009) Coughs and sneezes spread diseases: an empirical study of absenteeism and infectious illness. J Health Econ 28(5):1012–1017. https://doi.org/10.1016/j.jhealeco.2009.06.006
Bean B, Moore BM, Sterner B, Peterson LR, Gerding DN, Balfour HH Jr (1982) Survival of influenza viruses on environmental surfaces. J Infect Dis 146(1):47–51. https://doi.org/10.1093/infdis/146.1.47
Beggs CB (2003) The airborne transmission of infection in hospital buildings: fact or fiction? Indoor and Built Environment 12(1–2):9–18. https://doi.org/10.1177/1420326X03012001002
Beggs CB, Noakes CJ, Sleigh PA, Fletcher LA, Siddiqi K (2003) The transmission of tuberculosis in confined spaces: an analytical review of alternative epidemiological models. Int J Tuberc Lung Dis 7(11):1015–1026
Béghein C, Jiang Y, Chen QY (2005) Using large eddy simulation to study particle motions in a room. Indoor Air 15(4):281–290. https://doi.org/10.1111/j.1600-0668.2005.00373.x
Ben-Tzvi P, Rone W (2010) Microdroplet generation in gaseous and liquid environments. Microsyst Technol 16(3):333–356. https://doi.org/10.1007/s00542-009-0962-7
Bergeron V, Chalfine A, Misset B, Moules V, Laudinet N, Carlet J, Lina B (2011) Supplemental treatment of air in airborne infection isolation rooms using high-throughput in-room air decontamination units. Am J Infect Control 39(4):314–320. https://doi.org/10.1016/j.ajic.2010.06.013
Berlanga FA, de Adana MR, Olmedo I, Villafruela JM, San José JF, Castro F (2018) Experimental evaluation of thermal comfort, ventilation performance indices and exposure to airborne contaminant in an airborne infection isolation room equipped with a displacement air distribution system. Energy Build 158:209–221. https://doi.org/10.1016/j.enbuild.2017.09.100
Berrouk AS, Lai ACK, Cheung ACT, Wong SL (2010) Experimental measurements and large eddy simulation of expiratory droplet dispersion in a mechanically ventilated enclosure with thermal effects. Build Environ 45(2):371–379. https://doi.org/10.1016/j.buildenv.2009.06.016
Bhagat RK, Davies Wykes MS, Dalziel SB, Linden PF (2020) Effects of ventilation on the indoor spread of COVID-19. J Fluid Mech 903:F1–1-F1–18. https://doi.org/10.1017/jfm.2020.720
Biedermann T, Winther L, Till SJ, Panzner P, Knulst A, Valovirta E (2019) Birch pollen allergy in Europe. Allergy 74(7):1237–1248. https://doi.org/10.1111/all.13758
Bolashikov Z, Lu P, Malinowski T, Melikov A (2015) Air quality performance of ductless personalized ventilation in conjunction with displacement ventilation: Impact of walking person. Paper presented at the Healthy Buildings Europe 2015, HB 2015 - Conference Proceedings
Bolashikov ZD, Melikov AK (2009) Methods for air cleaning and protection of building occupants from airborne pathogens. Build Environ 44(7):1378–1385. https://doi.org/10.1016/j.buildenv.2008.09.001
Bolashikov ZD, Melikov AK, Kierat W, Popioek Z, Brand M (2012) Exposure of health care workers and occupants to coughed airborne pathogens in a double-bed hospital patient room with overhead mixing ventilation. HVAC R Res 18(4):602–615. https://doi.org/10.1080/10789669.2012.682692
Bongers S, Janssen NAH, Reiss B, Grievink L, Lebret E, Kromhout H (2008) Challenges of exposure assessment for health studies in the aftermath of chemical incidents and disasters. J Expos Sci Environ Epidemiol 18(4):341–359. Retrieved from https://doi.org/10.1038/jes.2008.23
Bonnet M, Lagier JC, Raoult D, Khelaifia S (2020) Bacterial culture through selective and non-selective conditions: the evolution of culture media in clinical microbiology. New Microbes New Infect 34:100622. https://doi.org/10.1016/j.nmni.2019.100622
Booth TF, Kournikakis B, Bastien N, Ho J, Kobasa D, Stadnyk L, Li Y, Spence M, Paton S, Henry B, Mederski B, White D, Low DE, McGeer A, Simor A, Vearncombe M, Downey J, Jamieson FB, Tang P, Plummer F (2005) Detection of airborne severe acute respiratory syndrome (SARS) Coronavirus and environmental contamination in SARS outbreak units. J Infect Dis 191(9):1472–1477. https://doi.org/10.1086/429634
Borrego C, Tchepel O, Costa AM, Martins H, Ferreira J, Miranda AI (2006) Traffic-related particulate air pollution exposure in urban areas. Atmos Environ 40(37):7205–7214. https://doi.org/10.1016/j.atmosenv.2006.06.020
Borro L, Mazzei L, Raponi M, Piscitelli P, Miani A, Secinaro A (2020) The role of air conditioning in the diffusion of Sars-CoV-2 in indoor environments: a first computational fluid dynamic model, based on investigations performed at the Vatican State Children’s hospital. Environ Res 193:110343. https://doi.org/10.1016/j.envres.2020.110343
Bourouiba L, Dehandschoewercker E, Bush JWM (2014) Violent expiratory events: on coughing and sneezing. J Fluid Mech 745:537–563. https://doi.org/10.1017/jfm.2014.88
Brager GS, De Dear RJ (1998) Thermal adaptation in the built environment: a literature review. Energy Build 27(1):83–96
Brennen EC (2005) Fundamentals of multiphase flows. Cambridge University Press, Cambridge
Breslow JM, Meissler JJ Jr, Hartzell RR, Spence PB, Truant A, Gaughan J, Eisenstein TK (2011) Innate immune responses to systemic Acinetobacter baumannii infection in mice: neutrophils, but not interleukin-17, mediate host resistance. Infect Immun 79(8):3317–3327. https://doi.org/10.1128/iai.00069-11
Briggs DJ, Denman AR, Gulliver J, Marley RF, Kennedy CA, Philips PS, Field K, Crockett RM (2003) Time activity modelling of domestic exposures to radon. J Environ Manag 67(2):107–120. https://doi.org/10.1016/S0301-4797(02)00159-7
Broniarz-Press L, Ochowiak M, Rozanski J, Woziwodzki S (2009) The atomization of water–oil emulsions. Exp Thermal Fluid Sci 33(6):955–962. https://doi.org/10.1016/j.expthermflusci.2009.04.002
Brugger SD, Baumberger C, Jost M, Jenni W, Brugger U, Mühlemann K (2012) Automated counting of bacterial colony forming units on agar plates. PLoS One 7(3):e33695. https://doi.org/10.1371/journal.pone.0033695
Bruijns BB, Tiggelaar RM, Gardeniers H (2018) The extraction and recovery efficiency of pure DNA for different types of swabs. J Forensic Sci 63(5):1492–1499. https://doi.org/10.1111/1556-4029.13837
Brundage JF, Scott RM, Lednar WM, Smith DW, Miller RN (1988) Building-associated risk of febrile acute respiratory diseases in army trainees. JAMA 259(14):2108–2112. https://doi.org/10.1001/jama.1988.03720140028029
Burmølle M, Johnsen K, Abu Al-Soud W, Hansen LH, Sørensen SJ (2009) The presence of embedded bacterial pure cultures in agar plates stimulate the culturability of soil bacteria. J Microbiol Methods 79(2):166–173. https://doi.org/10.1016/j.mimet.2009.08.006
Butler DF, Myers AL (2018) Changing epidemiology of Haemophilus influenzae in children. Infect Dis Clin North Am 32(1):119–128. https://doi.org/10.1016/j.idc.2017.10.005
Cao G, Awbi H, Yao R, Fan Y, Sirén K, Kosonen R, Zhang J (2014) A review of the performance of different ventilation and airflow distribution systems in buildings. Build Environ 73:171–186. https://doi.org/10.1016/j.buildenv.2013.12.009
Cao G, Nielsen PV, Jensen RL, Heiselberg P, Liu L, Heikkinen J (2015) Protected zone ventilation and reduced personal exposure to airborne cross-infection. Indoor Air 25(3):307–319. https://doi.org/10.1111/ina.12142
Carducci A, Federigi I, Verani M (2020) Covid-19 Airborne transmission and its prevention: waiting for evidence or applying the precautionary principle? Atmosphere 11(7):710. https://doi.org/10.3390/atmos11070710
Carrera M, Zandomeni RO, Fitzgibbon J, Sagripanti JL (2007) Difference between the spore sizes of Bacillus anthracis and other Bacillus species. J Appl Microbiol 102(2):303–312. https://doi.org/10.1111/j.1365-2672.2006.03111.x
Causone F, Baldin F, Olesen BW, Corgnati SP (2010a) Floor heating and cooling combined with displacement ventilation: possibilities and limitations. Energy Build 42(12):2338–2352. https://doi.org/10.1016/j.enbuild.2010.08.001
Causone F, Olesen BW, Corgnati SP (2010b) Floor heating with displacement ventilation: an experimental and numerical analysis. HVAC R Res 16(2):139–160. https://doi.org/10.1080/10789669.2010.10390898
CEN (Εuropean Committee for Standardization) (2019) EN 16798–1:2019 Energy performance of buildings. Ventilation for buildings. Indoor environmental input parameters for design and assessment of energy performance of buildings addressing indoor air quality, thermal environment, lighting and acoustics. European Committee for Standardization, Brussels
Cermak R, Melikov AK (2007) Protection of occupants from exhaled infectious agents and floor material emissions in rooms with personalized and underfloor ventilation. HVAC R Res 13(1):23–38. https://doi.org/10.1080/10789669.2007.10390942
Cermak R, Melikov AK, Forejt L, Kovar O (2006) Performance of personalized ventilation in conjunction with mixing and displacement ventilation. HVAC R Res 12(2):295–311. https://doi.org/10.1080/10789669.2006.10391180
Cetin YE, Avci M, Aydin O (2020a) Influence of ventilation strategies on dispersion and removal of fine particles: an experimental and simulation study. Sci Technol Built Environ 26(3):349–365. https://doi.org/10.1080/23744731.2019.1701332
Cetin YE, Avci M, Aydin O (2020b) Particle dispersion and deposition in displacement ventilation systems combined with floor heating. Sci Technol Built Environ. https://doi.org/10.1080/23744731.2020.1760637
Chafekar A, Fielding BC (2018) MERS-CoV: understanding the latest human coronavirus threat. Viruses 10(2):22. https://doi.org/10.3390/v10020093
Chan KS, Zheng JP, Mok YW, Li YM, Liu YN, Chu CM, Ip MS (2003) SARS: prognosis, outcome and sequelae. Respirology 8 Suppl(Suppl 1):S36–40. https://doi.org/10.1046/j.1440-1843.2003.00522.x
Chao CYH, Tung TC (2001) An empirical model for outdoor contaminant transmission into residential buildings and experimental verification. Atmos Environ 35(9):1585–1596. https://doi.org/10.1016/S1352-2310(00)00458-1
Chao CYH, Wan MP (2006) A study of the dispersion of expiratory aerosols in unidirectional downward and ceiling-return type airflows using a multiphase approach. Indoor Air 16(4):296–312. https://doi.org/10.1111/j.1600-0668.2006.00426.x
Chao CYH, Wan MP, Sze To GN (2008) Transport and removal of expiratory droplets in hospital ward environment. Aerosol Sci Technol 42(5):377–394. https://doi.org/10.1080/02786820802104973
Chau OKY, Liu CH, Leung MKH (2006) CFD analysis of the performance of a local exhaust ventilation system in a hospital ward. Indoor and Built Environment 15(3):257–271. https://doi.org/10.1177/1420326X06066123
Chen C, Zhao B (2010) Some questions on dispersion of human exhaled droplets in ventilation room: answers from numerical investigation. Indoor Air 20(2):95–111. https://doi.org/10.1111/j.1600-0668.2009.00626.x
Chen C, Zhao B, Yang X, Li Y (2011) Role of two-way airflow owing to temperature difference in severe acute respiratory syndrome transmission: revisiting the largest nosocomial severe acute respiratory syndrome outbreak in Hong Kong. J R Soc Interface 8(58):699–710. https://doi.org/10.1098/rsif.2010.0486
Chen C, Zhu J, Qu Z, Lin CH, Jiang Z, Chen Q (2014) Systematic study of person-to-person contaminant transport in mechanically ventilated spaces (RP-1458). HVAC R Res 20(1):80–91. https://doi.org/10.1080/10789669.2013.834778
Cheng YH, Wang CH, You SH, Hsieh NH, Chen WY, Chio CP, Liao CM (2016) Assessing coughing-induced influenza droplet transmission and implications for infection risk control. Epidemiol Infect 144(2):333–345. https://doi.org/10.1017/S0950268815001739
Choi J, Kang M, Jung JH (2015) Integrated micro-optofluidic platform for real-time detection of airborne microorganisms. Sci Rep 5:15983. https://doi.org/10.1038/srep15983
Choi JI, Edwards JR (2008) Large eddy simulation and zonal modeling of human-induced contaminant transport. Indoor Air 18(3):233–249. https://doi.org/10.1111/j.1600-0668.2008.00527.x
Choi JI, Edwards JR (2012) Large-eddy simulation of human-induced contaminant transport in room compartments. Indoor Air 22(1):77–87. https://doi.org/10.1111/j.1600-0668.2011.00741.x
Choi N, Yamanaka T, Sagara K, Momoi Y, Suzuki T (2019) Displacement ventilation with radiant panel for hospital wards: measurement and prediction of the temperature and contaminant concentration profiles. Build Environ 160:106197. https://doi.org/10.1016/j.buildenv.2019.106197
Choudoir MJ, Barberán A, Menninger HL, Dunn RR, Fierer N (2018) Variation in range size and dispersal capabilities of microbial taxa. Ecology 99(2):322–334. https://doi.org/10.1002/ecy.2094
Chow WK (1996) Application of computational fluid dynamics in building services engineering. Build Environ 31(5):425–436. https://doi.org/10.1016/0360-1323(96)00012-1
Cole EC, Cook CE (1998) Characterization of infectious aerosols in health care facilities: an aid to effective engineering controls and preventive strategies. Am J Infect Control 26(4):453–464. https://doi.org/10.1016/S0196-6553(98)70046-X
Coleman KK, Sigler WV (2020) Airborne influenza A virus exposure in an elementary school. Sci Rep 10(1):1859. https://doi.org/10.1038/s41598-020-58588-1
Collier LH, Oxford JS, Pipkin J (2000) Human virology: a text for students of medicine, dentistry, and microbiology. Oxford University Press, Oxford
Collins CH, Lyne PM, Grange JM (1989) Collins and lyne’s microbiological methods. Butterworths, London
Cooke TF (1991) Indoor air pollutants a literature review. Rev Environ Health 9(3):137–160. https://doi.org/10.1515/REVEH.1991.9.3.137
Crameri R, Weichel M, Flückiger S, Glaser AG, Rhyner C (2006) Fungal allergies: a yet unsolved problem. Chem Immunol Allergy 91:121–133. https://doi.org/10.1159/000090276
Crowe CT, Troutt TR, Chung JN (1996) Numerical models for two-phase turbulent flows. Annu Rev Fluid Mech 28:11–43
Cui D, Ai Z, Mak CM, Kwok K, Xue P (2018) The influence of envelope features on interunit dispersion around a naturally ventilated multi-story building. Build Simul 11(6):1245–1253. https://doi.org/10.1007/s12273-018-0460-x
Cutting SM, Ricca E (2014) Bacterial spore-formers: friends and foes. FEMS Microbiol Lett 358(2):107–109. https://doi.org/10.1111/1574-6968.12572
D’Amato G, Liccardi G, Frenguelli G (2007) Thunderstorm-asthma and pollen allergy. Allergy 62(1):11–16. https://doi.org/10.1111/j.1398-9995.2006.01271.x
D’Amato G, Spieksma FT, Liccardi G, Jäger S, Russo M, Kontou-Fili K, Nikkels H, Wüthrich B, Bonini S (1998) Pollen-related allergy in Europe. Allergy 53(6):567–578. https://doi.org/10.1111/j.1398-9995.1998.tb03932.x
Dannemiller KC, Weschler CJ, Peccia J (2017) Fungal and bacterial growth in floor dust at elevated relative humidity levels. Indoor Air 27(2):354–363. https://doi.org/10.1111/ina.12313
Davidson S (2018) Treating Influenza infection, from now and into the future. Front Immunol 9:1946. https://doi.org/10.3389/fimmu.2018.01946
Dbouk T, Drikakis D (2020a) On coughing and airborne droplet transmission to humans. Phys Fluids 32(5):053310. https://doi.org/10.1063/5.0011960
Dbouk T, Drikakis D (2020b) On respiratory droplets and face masks. Phys Fluids 32(6):063303. https://doi.org/10.1063/5.0015044
Dbouk T, Drikakis D (2020c) Weather impact on airborne coronavirus survival. Phys Fluids 32(9):093312. https://doi.org/10.1063/5.0024272
De Dear RJ, Brager GS (2002) Thermal comfort in naturally ventilated buildings: revisions to ASHRAE standard 55. Energy Build 34(6):549–561. https://doi.org/10.1016/S0378-7788(02)00005-1
de Oliveira PM, Mesquita LCC, Gkantonas S, Giusti A, Mastorakos E (2021) Evolution of spray and aerosol from respiratory releases: theoretical estimates for insight on viral transmission. Proc R Soc A Math Phys Eng Sci 477(2245):20200584. https://doi.org/10.1098/rspa.2020.0584
de Wit E, van Doremalen N, Falzarano D, Munster VJ (2016) SARS and MERS: recent insights into emerging coronaviruses. Nat Rev Microbiol 14(8):523–534. https://doi.org/10.1038/nrmicro.2016.81
Deacon JW (2006) Fungal biology. Blackwell Publishing, Malden
Dedesko S, Siegel JA (2015) Moisture parameters and fungal communities associated with gypsum drywall in buildings. Microbiome 3:71. https://doi.org/10.1186/s40168-015-0137-y
Dhama K, Khan S, Tiwari R, Sircar S, Bhat S, Malik YS, Singh KP, Chaicumpa W, Bonilla-Aldana K, Rodriguez-Morales AJ (2020) Coronavirus disease 2019-COVID-19. Clin Microbiol Revi 33(4):e00028–00020. https://doi.org/10.1128/CMR.00028-20
Dhand R, Li J (2020) Coughs and sneezes: their role in transmission of respiratory viral infections, including SARS-CoV-2. Am J Respir Crit Care Med 202(5):651–659. https://doi.org/10.1164/rccm.202004-1263PP
Dietert K, Gutbier B, Wienhold SM, Reppe K, Jiang X, Yao L, Chaput C, Naujoks J, Brack M, Kupke A, Peteranderl C, Becker S, Lachner C, Baal N, Slevogt H, Hocke AC, Witzenrath M, Opitz B, Herold S, Hackstein H, Sander LE, Suttorp N, Gruber AD (2017) Spectrum of pathogen- and model-specific histopathologies in mouse models of acute pneumonia. Plos One 12(11):e0188251–e0188251. https://doi.org/10.1371/journal.pone.0188251
Dijksterhuis J (2019) Fungal spores: highly variable and stress-resistant vehicles for distribution and spoilage. Food Microbiol 81:2–11. https://doi.org/10.1016/j.fm.2018.11.006
Dimitroulopoulou C, Ashmore MR, Byrne MA, Kinnersley RP (2001) Modelling of indoor exposure to nitrogen dioxide in the UK. Atmos Environ 35(2):269–279. https://doi.org/10.1016/S1352-2310(00)00176-X
Dimitroulopoulou C, Ashmore MR, Hill MTR, Byrne MA, Kinnersley R (2006) INDAIR: a probabilistic model of indoor air pollution in UK homes. Atmos Environ 40(33):6362–6379. https://doi.org/10.1016/j.atmosenv.2006.05.047
Dingle TC, Butler-Wu SM (2013) Maldi-tof mass spectrometry for microorganism identification. Clin Lab Med 33(3):589–609. https://doi.org/10.1016/j.cll.2013.03.001
Diwan SS, Ravichandran S, Govindarajan R, Narasimha R (2020) Understanding transmission dynamics of COVID-19-Type infections by direct numerical simulations of cough/sneeze flows. Trans Indian Natl Acad Eng 5(2):255–261. https://doi.org/10.1007/s41403-020-00106-w
Dols WS, Polidoro BJ (2015) CONTAM user guide and program documentation. National Institute of Standards and Technology. https://nvlpubs.nist.gov/nistpubs/TechnicalNotes/NIST.TN.1887r1.pdf. Accessed 24 Nov 2022
Dols WS, Walton GN, Denton KR (2000) CONTAMW 1.0 user manual. National Institute of Standards and Technology, Gaithersburg
Domingo JL, Marquès M, Rovira J (2020) Influence of airborne transmission of SARS-CoV-2 on COVID-19 pandemic. A Review. Environ Res 188:109861. https://doi.org/10.1016/j.envres.2020.109861
Douglas MG, Kocher JF, Scobey T, Baric RS, Cockrell AS (2018) Adaptive evolution influences the infectious dose of MERS-CoV necessary to achieve severe respiratory disease. Virology 517:98–107. https://doi.org/10.1016/j.virol.2017.12.006
Drossinos Y, Stilianakis NI (2020) What aerosol physics tells us about airborne pathogen transmission. Aerosol Sci Technol 54(6):639–643. https://doi.org/10.1080/02786826.2020.1751055
Duan N (1982) Indoor Air Pollution Models for human exposure to air pollution. Environ Int 8(1):305–309. https://doi.org/10.1016/0160-4120(82)90041-1
Dudalski N, Mohamed A, Mubareka S, Bi R, Zhang C, Savory E (2020) Experimental investigation of far-field human cough airflows from healthy and influenza-infected subjects. Indoor Air 30(5):966–977. https://doi.org/10.1111/ina.12680
Duquenne P (2017) On the identification of culturable microorganisms for the assessment of biodiversity in bioaerosols. Ann Work Expo Health 62(2):139–146. https://doi.org/10.1093/annweh/wxx096
Efthimiou GC, Kovalets IV, Argyropoulos CD, Venetsanos A, Andronopoulos S, Kakosimos KE (2018) Evaluation of an inverse modelling methodology for the prediction of a stationary point pollutant source in complex urban environments. Build Environ 143:107–119. https://doi.org/10.1016/j.buildenv.2018.07.003
Emmerich SJ (2001) Validation of multizone IAQ modeling of residential-scale buildings: a review. Trans Am Soc Heat Refrigerating Air Cond Eng 107(2):619–628
Emmerich SJ, Heinzerling D, Choi J-I, Persily AK (2013) Multizone modeling of strategies to reduce the spread of airborne infectious agents in healthcare facilities. Build Environ 60:105–115. https://doi.org/10.1016/j.buildenv.2012.11.013
Engin AB, Engin ED, Engin A (2020) Two important controversial risk factors in SARS-CoV-2 infection: obesity and smoking. Environ Toxicol Pharmacol 78:103411. https://doi.org/10.1016/j.etap.2020.103411
Escombe AR, Oeser CC, Gilman RH, Navincopa M, Ticona E, Pan W, Martínez C, Chacaltana J, Rodríguez R, Moore DAJ, Friedland JS, Evans CA (2007) Natural ventilation for the prevention of airborne contagion. PLoS Med 4(2):309–317. https://doi.org/10.1371/journal.pmed.0040068
Escombe AR, Ticona E, Chávez-Pérez V, Espinoza M, Moore DAJ (2019) Improving natural ventilation in hospital waiting and consulting rooms to reduce nosocomial tuberculosis transmission risk in a low resource setting. BMC Infect Dis 19(1). https://doi.org/10.1186/s12879-019-3717-9
Evers E, Waterhouse A (1978) A computer model for analysing smoke movement in Buildings. Building Research Establishment (BRE), Borehamwood
Faridi S, Niazi S, Sadeghi K, Naddafi K, Yavarian J, Shamsipour M, Jandaghi NZS, Sadeghniiat K, Nabizadeh R, Yunesian M, Momeniha F, Mokamel A, Hassanvand, MS, MokhtariAzad T (2020) A field indoor air measurement of SARS-CoV-2 in the patient rooms of the largest hospital in Iran. Sci Total Environ 725:138401. https://doi.org/10.1016/j.scitotenv.2020.138401
Faulkner WB, Memarzadeh F, Riskowski G, Kalbasi A, Ching-Zu Chang A (2015) Effects of air exchange rate, particle size and injection place on particle concentrations within a reduced-scale room. Build Environ 92:246–255. https://doi.org/10.1016/j.buildenv.2015.04.034
Feldman C, Anderson R (2016) The role of Streptococcus pneumoniae in Community-acquired pneumonia. Semin Respir Crit Care Med 37(6):806–818. https://doi.org/10.1055/s-0036-1592074
Feng G, Bi Y, Zhang Y, Cai Y, Huang K (2020a) Study on the motion law of aerosols produced by human respiration under the action of thermal plume of different intensities. Sustain Cities Soc 54:101935. https://doi.org/10.1016/j.scs.2019.101935
Feng Y, Marchal T, Sperry T, Yi H (2020b) Influence of wind and relative humidity on the social distancing effectiveness to prevent COVID-19 airborne transmission: a numerical study. J Aerosol Sci 147:105585. https://doi.org/10.1016/j.jaerosci.2020.105585
Feng Y, Zhao J, Hayati H, Sperry T, Yi H (2021) Tutorial: understanding the transport, deposition, and translocation of particles in human respiratory systems using computational fluid-particle dynamics and physiologically based toxicokinetic models. J Aerosol Sci 151:105672. https://doi.org/10.1016/j.jaerosci.2020.105672
Fennelly KP, Nardell EA (1998) The relative efficacy of respirators and room ventilation in preventing occupational tuberculosis. Infect Control Hosp Epidemiol 19(10):754–759. https://doi.org/10.2307/30141420
Ferguson RMW, Garcia-Alcega S, Coulon F, Dumbrell AJ, Whitby C, Colbeck I (2019) Bioaerosol biomonitoring: sampling optimization for molecular microbial ecology. Mol Ecol Resour 19(3):672–690. https://doi.org/10.1111/1755-0998.13002
Fernstrom A, Goldblatt M (2013) Aerobiology and its role in the transmission of infectious diseases. Journal of Pathogens 2013:493960. https://doi.org/10.1155/2013/493960
Feustel HE (1999) COMIS—an international multizone air-flow and contaminant transport model. Energy and Buildings 30(1):3–18. https://doi.org/10.1016/S0378-7788(98)00043-7
Feustel HE, Allard F, Dorer VB, Grosso M, Herrlin M, Mingsheng L, Phaff JC, Utsumi Y, Yoshino H (1989) The COMIS infiltration model. U.S. Department of Energy. https://www.osti.gov/servlets/purl/7259831. Accessed 24 Nov 2022
Feustel HE, Dieris J (1992) A survey of airflow models for multizone structures. Energy Build 18(2):79–100. https://doi.org/10.1016/0378-7788(92)90040-N
Fontes D, Reyes J, Ahmed K, Kinzel M (2020) A study of fluid dynamics and human physiology factors driving droplet dispersion from a human sneeze. Phys Fluids 32(11):111904. https://doi.org/10.1063/5.0032006
Foster A, Kinzel M (2021) Estimating COVID-19 exposure in a classroom setting: a comparison between mathematical and numerical models. Phys Fluids 33(2):021904. https://doi.org/10.1063/5.0040755
Foster KN, Chundu KR, Lal S, Caruso DM (2017) Invasive aspergillus infection leading to vascular thrombosis and amputation in a severely burned child. J Burn Care Res 38(1):e464–e468. https://doi.org/10.1097/bcr.0000000000000366
Friberg B, Friberg S, Burman LG, Lundholm R, Östensson R (1996) Inefficiency of upward displacement operating theatre ventilation. J Hosp Infect 33(4):263–272. https://doi.org/10.1016/S0195-6701(96)90012-2
Gadsby NJ, McHugh MP, Forbes C, MacKenzie L, Hamilton SKD, Griffith DM, Templeton KE (2019) Comparison of Unyvero P55 Pneumonia Cartridge, in-house PCR and culture for the identification of respiratory pathogens and antibiotic resistance in bronchoalveolar lavage fluids in the critical care setting. Eur J Clin Microbiol Infect Dis 38(6):1171–1178. https://doi.org/10.1007/s10096-019-03526-x
Galvin CJ, Li YCJ, Malwade S, Syed-Abdul S (2020) COVID-19 preventive measures showing an unintended decline in infectious diseases in Taiwan. Int J Infect Dis 98:18–20. https://doi.org/10.1016/j.ijid.2020.06.062
Gama JA, Abby SS, Vieira-Silva S, Dionisio F, Rocha EP (2012) Immune subversion and quorum-sensing shape the variation in infectious dose among bacterial pathogens. PLoS Pathog 8(2):e1002503. https://doi.org/10.1371/journal.ppat.1002503
Gao N, He Q, Niu J (2012a) Numerical study of the lock-up phenomenon of human exhaled droplets under a displacement ventilated room. Build Simul 5(1):51–60. https://doi.org/10.1007/s12273-012-0068-5
Gao N, Niu J, Morawska L (2008a) Distribution of respiratory droplets in enclosed environments under different air distribution methods. Build Simul 1(4):326–335. https://doi.org/10.1007/s12273-008-8328-0
Gao NP, Niu JL (2005) CFD Study of the thermal environment around a human body: a review. Indoor Built Environ 14(1):5–16. https://doi.org/10.1177/1420326X05050132
Gao NP, Niu JL, Perino M, Heiselberg P (2008b) The airborne transmission of infection between flats in high-rise residential buildings: tracer gas simulation. Build Environ 43(11):1805–1817. https://doi.org/10.1016/j.buildenv.2007.10.023
Gao NP, Niu JL, Perino M, Heiselberg P (2009a) The airborne transmission of infection between flats in high-rise residential buildings: particle simulation. Build Environ 44(2):402–410. https://doi.org/10.1016/j.buildenv.2008.03.016
Gao X, Li Y, Leung GM (2009b) Ventilation control of indoor transmission of airborne diseases in an Urban community. Indoor Built Environ 18(3):205–218. https://doi.org/10.1177/1420326X09104141
Gao X, Li Y, Xu P, Cowling BJ (2012b) Evaluation of intervention strategies in schools including ventilation for influenza transmission control. Build Simul 5(1):29–37. https://doi.org/10.1007/s12273-011-0034-7
Gao X, Wei J, Cowling BJ, Li Y (2016) Potential impact of a ventilation intervention for influenza in the context of a dense indoor contact network in Hong Kong. Sci Total Environ 569–570:373–381. https://doi.org/10.1016/j.scitotenv.2016.06.179
Gerharz LE, Krüger A, Klemm O (2009) Applying indoor and outdoor modeling techniques to estimate individual exposure to PM2.5 from personal GPS profiles and diaries: a pilot study. Sci Total Environ 407(18):5184–5193. https://doi.org/10.1016/j.scitotenv.2009.06.006
Ghosh B, Lal H, Srivastava A (2015) Review of bioaerosols in indoor environment with special reference to sampling, analysis and control mechanisms. Environ Int 85:254–272. https://doi.org/10.1016/j.envint.2015.09.018
Gilkeson CA, Camargo-Valero MA, Pickin LE, Noakes CJ (2013) Measurement of ventilation and airborne infection risk in large naturally ventilated hospital wards. Build Environ 65:35–48. https://doi.org/10.1016/j.buildenv.2013.03.006
Glanville N, Johnston SL (2015) Challenges in developing a cross-serotype rhinovirus vaccine. Curr Opin Virol 11:83–88. https://doi.org/10.1016/j.coviro.2015.03.004
Godri Pollitt KJ, Peccia J, Ko AI, Kaminski N, Dela Cruz CS, Nebert DW, Reichardt JKV, Thompson DC, Vasiliou V (2020) COVID-19 vulnerability: the potential impact of genetic susceptibility and airborne transmission. Hum Genomics 14(1):17. https://doi.org/10.1186/s40246-020-00267-3
Gralton J, Tovey E, McLaws M-L, Rawlinson WD (2011) The role of particle size in aerosolised pathogen transmission: a review. J Infect 62(1):1–13. https://doi.org/10.1016/j.jinf.2010.11.010
Green BJ, Tovey ER, Sercombe JK, Blachere FM, Beezhold DH, Schmechel D (2006) Airborne fungal fragments and allergenicity. Med Mycol 44(Suppl 1):S245-255. https://doi.org/10.1080/13693780600776308
Griffin DW (2007) Atmospheric Movement of microorganisms in clouds of desert dust and implications for human health. Clin Microbiol Rev 20(3):459. https://doi.org/10.1128/CMR.00039-06
Grishkan I (2018) Thermotolerant mycobiota of Israeli soils. J Basic Microbiol 58(1):30–40. https://doi.org/10.1002/jobm.201700517
Gu D, Zheng Z, Zhao P, Xie L, Xu Z, Lu X (2020) High-Efficiency simulation framework to analyze the impact of exhaust air from COVID-19 Temporary hospitals and its typical applications. Appl Sci 10(11):3949. https://doi.org/10.3390/app10113949
Gu W, Miller S, Chiu CY (2019) Clinical metagenomic next-generation sequencing for pathogen detection. Annu Rev Pathol 14:319–338. https://doi.org/10.1146/annurev-pathmechdis-012418-012751
Guzman M (2020) Bioaerosol size effect in COVID-19 transmission. Preprints org. https://www.preprints.org/manuscript/202004.0093/v2. Accessed 24 Nov 2022
Habchi C, Ghali K, Ghaddar N, Chakroun W, Alotaibi S (2016) Ceiling personalized ventilation combined with desk fans for reduced direct and indirect cross-contamination and efficient use of office space. Energy Convers Manag 111:158–173. https://doi.org/10.1016/j.enconman.2015.12.067
Hageman JR (2020) The Coronavirus Disease 2019 (COVID-19). Pediatr Ann 49(3):e99–e100. https://doi.org/10.3928/19382359-20200219-01
Haghighat F, Megri AC (1996) A comprehensive validation of two airflow models - COMIS and CONTAM. Indoor Air 6:278–288
Haghighat F, Rao J (1991) Computer-aided building ventilation system design — a system-theoretic approach. Energy Build 17(2):147–155. https://doi.org/10.1016/0378-7788(91)90007-P
Haghnegahdar A, Zhao J, Feng Y (2019a) Lung aerosol dynamics of airborne influenza A virus-laden droplets and the resultant immune system responses: an in silico study. J Aerosol Sci 134:34–55. https://doi.org/10.1016/j.jaerosci.2019.04.009
Haghnegahdar A, Zhao J, Kozak M, Williamson P, Feng Y (2019b) Development of a hybrid CFD-PBPK model to predict the transport of xenon gas around a human respiratory system to systemic regions. Heliyon 5(4):e01461. https://doi.org/10.1016/j.heliyon.2019.e01461
Haines SR, Adams RI, Boor BE, Bruton TA, Downey J, Ferro AR, Gall E,Green BJ, Hegarty B, Horner E, Jacobs DE, Lemieux P, Misztal PK, Morrison G, Perzanowski M, Reponen T, Rush RE, Virgo T, Alkhayri C, Bope A, Cochran S, Cox J, Donohue A, May AA, Nastasi N, Nishioka M, Renninger N, Tian Y, Uebel-Niemeier C, Wilkinson D, Wu T, Zambrana J, Dannemiller KC (2020) Ten questions concerning the implications of carpet on indoor chemistry and microbiology. Build Environ 170:106589. https://doi.org/10.1016/j.buildenv.2019.106589
Hajjar SA, Memish ZA, McIntosh K (2013) Middle East Respiratory syndrome coronavirus (MERS-CoV): a perpetual challenge. Ann Saudi Med 33(5):427–436. https://doi.org/10.5144/0256-4947.2013.427
Hall-Stoodley L, Costerton JW, Stoodley P (2004) Bacterial biofilms: from the natural environment to infectious diseases. Nat Rev Microbiol 2(2):95–108. https://doi.org/10.1038/nrmicro821
Han B, Weiss LM (2017) Microsporidia: obligate intracellular pathogens within the fungal kingdom. Microbiol Spectr 5(2):1–26. https://doi.org/10.1128/microbiolspec.FUNK-0018-2016
Han H, Wang P, Li Y, Liu R, Tian C (2020) Effect of water supply pressure on atomization characteristics and dust-reduction efficiency of internal mixing air atomizing nozzle. Adv Powder Technol 31(1):252–268. https://doi.org/10.1016/j.apt.2019.10.017
Haun N, Hooper-Lane C, Safdar N (2016) Healthcare personnel attire and devices as fomites: a systematic review. Infect Control Hosp Epidemiol 37(11):1367–1373. https://doi.org/10.1017/ice.2016.192
He Q, Niu J, Gao N, Zhu T, Wu J (2011) CFD study of exhaled droplet transmission between occupants under different ventilation strategies in a typical office room. Build Environ 46(2):397–408. https://doi.org/10.1016/j.buildenv.2010.08.003
Henrickson KJ (2003) Parainfluenza viruses. Clin Microbiol Rev 16(2):242–264. https://doi.org/10.1128/cmr.16.2.242-264.2003
Hicklin W, Farrugia PS, Sinagra E (2018) Investigations of VOCs in and around buildings close to service stations. Atmos Environ 172:93–101. https://doi.org/10.1016/j.atmosenv.2017.10.012
Hirose R, Ikegaya H, Naito Y, Watanabe N, Yoshida T, Bandou R, Daidoji T, Itoh Y, Nakaya T (2020) Survival of SARS-CoV-2 and influenza virus on the human skin: importance of hand hygiene in COVID-19. Clin Infect Dis. https://doi.org/10.1093/cid/ciaa1517
Hobday RA, Dancer SJ (2013) Roles of sunlight and natural ventilation for controlling infection: historical and current perspectives. J Hosp Infect 84(4):271–282. https://doi.org/10.1016/j.jhin.2013.04.011
Huang J, Jiang E, Yang D, Wei J, Zhao M, Feng J, Cao J (2020) Metagenomic next-generation sequencing versus traditional pathogen detection in the diagnosis of peripheral pulmonary infectious lesions. Infect Drug Resist 13:567–576. https://doi.org/10.2147/idr.s235182
Huang J-M, Tsao S-M (2005) The Influence of air motion on bacteria removal in negative pressure isolation rooms. HVAC&R Res 11(4):563–585. https://doi.org/10.1080/10789669.2005.10391155
Huffman JA, Perring AE, Savage NJ, Clot B, Crouzy B, Tummon F, Shoshanim O, Damit B, Schneider J, Sivaprakasam V, Zawadowicz MA, Crawford I, Gallagher M, Topping D, Doughty DC, Hill SC, Pan Y (2020) Real-time sensing of bioaerosols: review and current perspectives. Aerosol Sci Technol 54(5):465–495. https://doi.org/10.1080/02786826.2019.1664724
Hunter RL (2016) Tuberculosis as a three-act play: a new paradigm for the pathogenesis of pulmonary tuberculosis. Tuberculosis (Edinb) 97:8–17. https://doi.org/10.1016/j.tube.2015.11.010
Hunter RL (2018) The Pathogenesis of tuberculosis: the early infiltrate of post-primary (adult pulmonary) tuberculosis: a distinct disease entity. Front Immunol 9:2108. https://doi.org/10.3389/fimmu.2018.02108
Husman T (1996) Health effects of indoor-air microorganisms. Scand J Work Environ Health 22(1):5–13. https://doi.org/10.5271/sjweh.103
Hussain S, Parker S, Edwards K, Finch J, Jeanjean A, Leigh R, Gonem S (2019) Effects of indoor particulate matter exposure on daily asthma control. Ann Allergy Asthma Immunol 123(4):375-380.e373. https://doi.org/10.1016/j.anai.2019.07.020
Islam MS, Paul G, Ong HX, Young PM, Gu YT, Saha SC (2020) A review of respiratory anatomical development, air flow characterization and particle deposition. Int J Environ Res Public Health 17(2):380. https://doi.org/10.3390/ijerph17020380
Ito K (2014) Integrated numerical approach of computational fluid dynamics and epidemiological model for multi-scale transmission analysis in indoor spaces. Indoor Built Environ 23(7):1029–1049. https://doi.org/10.1177/1420326X13516658
Iwasaki A, Pillai PS (2014) Innate immunity to influenza virus infection. Nat Rev Immunol 14(5):315–328. https://doi.org/10.1038/nri3665
Jang KS, Kim YH (2018) Rapid and robust MALDI-TOF MS techniques for microbial identification: a brief overview of their diverse applications. J Microbiol 56(4):209–216. https://doi.org/10.1007/s12275-018-7457-0
Järvinen AK, Laakso S, Piiparinen P, Aittakorpi A, Lindfors M, Huopaniemi L, Piiparinen H, Mäki M (2009) Rapid identification of bacterial pathogens using a PCR- and microarray-based assay. BMC Microbiol 9:161. https://doi.org/10.1186/1471-2180-9-161
Jayaweera M, Perera H, Gunawardana B, Manatunge J (2020) Transmission of COVID-19 virus by droplets and aerosols: A CRITICAL review on the unresolved dichotomy. Environ Res 188:109819. https://doi.org/10.1016/j.envres.2020.109819
Ji Y, Qian H, Ye J, Zheng X (2018) The impact of ambient humidity on the evaporation and dispersion of exhaled breathing droplets: a numerical investigation. J Aerosol Sci 115:164–172. https://doi.org/10.1016/j.jaerosci.2017.10.009
Jiang Y, Zhao B, Li X, Yang X, Zhang Z, Zhang Y (2009) Investigating a safe ventilation rate for the prevention of indoor SARS transmission: an attempt based on a simulation approach. Build Simul 2(4):281–289. https://doi.org/10.1007/s12273-009-9325-7
Jones AP (1999) Indoor air quality and health. Atmos Environ 33(28):4535–4564. https://doi.org/10.1016/S1352-2310(99)00272-1
Jurelionis A, Gagyte L, Prasauskas T, Čiužas D, Krugly E, Šeduikyte L, Martuzevičius D (2015) The impact of the air distribution method in ventilated rooms on the aerosol particle dispersion and removal: the experimental approach. Energy Build 86:305–313. https://doi.org/10.1016/j.enbuild.2014.10.014
Jurelionis A, Gagyte L, Seduikyte L, Prasauskas T, Ciuzas D, Martuzevicius D (2016) Combined air heating and ventilation increases risk of personal exposure to airborne pollutants released at the floor level. Energy Build 116:263–273. https://doi.org/10.1016/j.enbuild.2016.01.011
Jurelionis A, Stasiuliene L, Prasauskas T, Martuzevicius D (2018) Dispersion of indoor air pollutants emitted at near-floor levels in rooms with floor heating and mixing ventilation. Indoor Built Environ 27(2):205–218. https://doi.org/10.1177/1420326X16669975
Kampf G, Todt D, Pfaender S, Steinmann E (2020) Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J Hosp Infect 104(3):246–251. https://doi.org/10.1016/j.jhin.2020.01.022
Kang Z, Zhang Y, Fan H, Feng G (2015) Numerical Simulation of coughed droplets in the air-conditioning room. Procedia Eng 121:114–121. https://doi.org/10.1016/j.proeng.2015.08.1031
Karakitsios S, Busker R, Tjärnhage T, Armand P, Dybwad M, Nielsen MF, Burman J, Burke J, Brinek J, Bartzis J, Maggos T, Theocharidou M, Gattinesi P, Giannopoulos G, Sarigiannis D (2020) Challenges on detection, identification and monitoring of indoor airborne chemical-biological agents. Saf Sci 129:104789. https://doi.org/10.1016/j.ssci.2020.104789
Katramiz E, Al Assaad D, Ghaddar N, Ghali K (2020) The effect of human breathing on the effectiveness of intermittent personalized ventilation coupled with mixing ventilation. Build Environ 174:106755. https://doi.org/10.1016/j.buildenv.2020.106755
Katz SM, Hammel JM (1987) The effect of drying, heat, and pH on the survival of Legionella pneumophila. Ann Clin Lab Sci 17(3):150–156
Keshavarz SA, Salmanzadeh M, Ahmadi G (2017) Computational modeling of time resolved exposure level analysis of a heated breathing manikin with rotation in a room. J Aerosol Sci 103:117–131. https://doi.org/10.1016/j.jaerosci.2016.09.005
Khan RK, Strand MA (2018) Road dust and its effect on human health: a literature review. Epidemiol Health 40:e2018013. https://doi.org/10.4178/epih.e2018013
Khosronejad A, Santoni C, Flora K, Zhang Z, Kang S, Payabvash S, Sotiropoulos F (2020) Fluid dynamics simulations show that facial masks can suppress the spread of COVID-19 in indoor environments. AIP Adv 10(12):125109. https://doi.org/10.1063/5.0035414
Kim H, Webster RG, Webby RJ (2018) Influenza Virus: dealing with a drifting and shifting pathogen. Viral Immunol 31(2):174–183. https://doi.org/10.1089/vim.2017.0141
King MF, Noakes CJ, Sleigh PA (2015) Modeling environmental contamination in hospital single- and four-bed rooms. Indoor Air 25(6):694–707. https://doi.org/10.1111/ina.12186
King N, Auger P (2002) Indoor air quality, fungi, and health. How do we stand? Can Fam Physician 48:298–302
Knibbs LD, Johnson GR, Kidd TJ, Cheney J, Grimwood K, Kattenbelt JA, O'Rourke P, Ramsay KA, Sly PD, Wainwright CE, Wood ME, Morawska L, Bell SC (2014) Viability of Pseudomonas aeruginosa in cough aerosols generated by persons with cystic fibrosis. Thorax 69(8):740–745. https://doi.org/10.1136/thoraxjnl-2014-205213
Knibbs LD, Morawska L, Bell SC, Grzybowski P (2011) Room ventilation and the risk of airborne infection transmission in 3 health care settings within a large teaching hospital. Am J Infect Control 39(10):866–872. https://doi.org/10.1016/j.ajic.2011.02.014
Kornartit C, Sokhi RS, Burton MA, Ravindra K (2010) Activity pattern and personal exposure to nitrogen dioxide in indoor and outdoor microenvironments. Environ Int 36(1):36–45. https://doi.org/10.1016/j.envint.2009.09.004
Kovalets IV, Efthimiou GC, Andronopoulos S, Venetsanos AG, Argyropoulos CD, Kakosimos KE (2018) Inverse identification of unknown finite-duration air pollutant release from a point source in urban environment. Atmos Environ 181:82–96. https://doi.org/10.1016/j.atmosenv.2018.03.028
Kowalski W, Bahnfleth W, Musser A (2003) Modeling immune building systems for bioterrorism defense. J Archit Eng 9(2):86–96. https://doi.org/10.1061/(ASCE)1076-0431(2003)9:2(86)
Kralik P, Ricchi M (2017) A Basic guide to real time PCR in microbial diagnostics: definitions, parameters, and everything. Front Microbiol 8:108. https://doi.org/10.3389/fmicb.2017.00108
Kramer A, Schwebke I, Kampf G (2006) How long do nosocomial pathogens persist on inanimate surfaces? A systematic review. BMC Infect Dis 6:130–130. https://doi.org/10.1186/1471-2334-6-130
Kumar V (2017) Influenza in children. Indian J Pediatr 84(2):139–143. https://doi.org/10.1007/s12098-016-2232-x
Kurgat EK, Sexton JD, Garavito F, Reynolds A, Contreras RD, Gerba CP, Leslie RA, Edmonds-Wilson SL, Reynolds KA (2019) Impact of a hygiene intervention on virus spread in an office building. Int J Hyg Environ Health 222(3):479–485. https://doi.org/10.1016/j.ijheh.2019.01.001
Kuznetsov GV, Shlegel NE, Solomatin Y, Strizhak PA (2019) Combined techniques of secondary atomization of multi-component droplets. Chem Eng Sci 209:115199. https://doi.org/10.1016/j.ces.2019.115199
Lacoma A, Mateo L, Blanco I, Méndez MJ, Rodrigo C, Latorre I, Villar-Hernandez R, Domínguez J, Prat C (2019) Impact of host genetics and biological response modifiers on respiratory tract infections. Front Immunol 10:1013. https://doi.org/10.3389/fimmu.2019.01013
Lai ACK, Cheng YC (2007) Study of expiratory droplet dispersion and transport using a new Eulerian modeling approach. Atmos Environ 41(35):7473–7484. https://doi.org/10.1016/j.atmosenv.2007.05.045
Lai ACK, Wong SL (2011) Expiratory aerosol transport in a scaled chamber under a variety of emission characteristics: an experimental study. Aerosol Sci Technol 45(8):909–917. https://doi.org/10.1080/02786826.2011.571308
Lai MYY, Cheng PKC, Lim WWL (2005) Survival of severe acute respiratory syndrome coronavirus. Clin Infect Dis 41(7):67–71. https://doi.org/10.1086/433186
Lanzerstorfer C (2017) Variations in the composition of house dust by particle size. J Environ Sci Health A Tox Hazard Subst Environ Eng 52(8):770–777. https://doi.org/10.1080/10934529.2017.1303316
Latgé JP, Chamilos G (2019) Aspergillus fumigatus and Aspergillosis in 2019. Clin Microbiol Rev 33(1):e00140-18. https://doi.org/10.1128/cmr.00140-18
Lauxmann MA, Santucci NE, Autrán-Gómez AM (2020) The SARS-CoV-2 coronavirus and the COVID-19 outbreak. Int Braz J Urol 46(1):6–18. https://doi.org/10.1590/s1677-5538.ibju.2020.s101
Lee C, Park S, Cho K, Yoo JE, Lee S, Ko G (2018) Comparison of swab sampling methods for norovirus recovery on surfaces. Food Environ Virol 10(4):378–385. https://doi.org/10.1007/s12560-018-9353-5
Lee K, Parkhurst WJ, Xue J, Ozkaynak AH, Neuberg D, Spengler JD (2004) Outdoor/indoor/personal ozone exposures of children in Nashville, Tennessee. J Air Waste Manag Assoc 54(3):352–359. https://doi.org/10.1080/10473289.2004.10470904
Leggett MJ, McDonnell G, Denyer SP, Setlow P, Maillard JY (2012) Bacterial spore structures and their protective role in biocide resistance. J Appl Microbiol 113(3):485–498. https://doi.org/10.1111/j.1365-2672.2012.05336.x
Lei Z, Yang J, Zhuang Z (2012a) Headform and N95 filtering facepiece respirator interaction: contact pressure simulation and validation. J Occup Environ Hyg 9(1):46–58. https://doi.org/10.1080/15459624.2011.635130
Lei Z, Yang J, Zhuang Z, Roberge R (2012b) Simulation and evaluation of respirator faceseal leaks using computational fluid dynamics and infrared imaging. Ann Occup Hyg 57(4):493–506. https://doi.org/10.1093/annhyg/mes085
Leskiewicz M, Kaliszewski M, Włodarski M, Młynczak J, Mierczyk Z, Kopczynski K (2018) Improved real-time bio-aerosol classification using artificial neural networks. Atmos Meas Tech 11:6259–6270. https://doi.org/10.5194/amt-11-6259-2018
Li C-C (2009) Aerodynamic behavior of a gas mask canister containing two porous media. Chem Eng Sci 64(8):1832–1843. https://doi.org/10.1016/j.ces.2009.01.009
Li F, Niu J (2007) Control of volatile organic compounds indoors—development of an integrated mass-transfer-based model and its application. Atmos Environ 41(11):2344–2354. https://doi.org/10.1016/j.atmosenv.2006.11.022
Li X, Niu J, Gao N (2013) Co-occupant’s exposure to exhaled pollutants with two types of personalized ventilation strategies under mixing and displacement ventilation systems. Indoor Air 23(2):162–171. https://doi.org/10.1111/ina.12005
Li X, Shang Y, Yan Y, Yang L, Tu J (2018) Modelling of evaporation of cough droplets in inhomogeneous humidity fields using the multi-component Eulerian-Lagrangian approach. Build Environ 128:68–76. https://doi.org/10.1016/j.buildenv.2017.11.025
Li X-P, Niu J-L, Gao N-P (2012) Characteristics of physical blocking on co-occupant’s exposure to respiratory droplet residuals. J Cent South Univ 19(3):645–650. https://doi.org/10.1007/s11771-012-1051-0
Li Y, Duan S, Yu ITS, Wong TW (2004a) Multi-zone modeling of probable SARS virus transmission by airflow between flats in Block E, Amoy Gardens. Indoor Air 15(2):96–111. https://doi.org/10.1111/j.1600-0668.2004.00318.x
Li Y, Duan S, Yu ITS, Wong TW (2005) Multi-zone modeling of probable SARS virus transmission by airflow between flats in Block E, Amoy Gardens. Indoor Air 15(2):96–111. https://doi.org/10.1111/j.1600-0668.2004.00318.x
Li Y, Huang X, Yu ITS, Wong TW, Qian H (2004b) Role of air distribution in SARS transmission during the largest nosocomial outbreak in Hong Kong. Indoor Air 15(2):83–95. https://doi.org/10.1111/j.1600-0668.2004.00317.x
Li Y, Leung GM, Tang JW, Yang X, Chao CYH, Lin JZ, Lu JW, Nielsen PV, Niu J, Qian H, Sleigh AC, Su H-JJ, Sundell J, Wong TW,Yuen PL (2007) Role of ventilation in airborne transmission of infectious agents in the built environment – a multidisciplinary systematic review. Indoor Air 17(1):2–18. https://doi.org/10.1111/j.1600-0668.2006.00445.x
Li X, Niu J, Gao N (2011) Spatial distribution of human respiratory droplet residuals and exposure risk for the co-occupant under different ventilation methods. HVAC R Res 17(4):432–445. https://doi.org/10.1080/10789669.2011.578699
Li Z, Wang H, Zhang X, Wu T, Yang X (2020) Effects of space sizes on the dispersion of cough-generated droplets from a walking person. Phys Fluids 32(12):121705. https://doi.org/10.1063/5.0034874
Licina D, Melikov A, Pantelic J, Sekhar C, Tham KW (2015) Human convection flow in spaces with and without ventilation: personal exposure to floor-released particles and cough-released droplets. Indoor Air 25(6):672–682. https://doi.org/10.1111/ina.12177
Lim T, Cho J, Kim BS (2010) The predictions of infection risk of indoor airborne transmission of diseases in high-rise hospitals: tracer gas simulation. Energy Build 42(8):1172–1181. https://doi.org/10.1016/j.enbuild.2010.02.008
Lim T, Cho J, Kim BS (2011) Predictions and measurements of the stack effect on indoor airborne virus transmission in a high-rise hospital building. Build Environ 46(12):2413–2424. https://doi.org/10.1016/j.buildenv.2011.04.015
Lin Y, Wang BX, Zhang NN, Zhang L, Gao ZB, Tian J, Jiang X (2019) Metagenomic analysis identified Stenotrophomonas maltophilia Pneumonia in an infant suffering from unexplained very severe pneumonia. Front Pediatr 7:380. https://doi.org/10.3389/fped.2019.00380
Lin Z, Wang J, Yao T, Chow TT (2012) Investigation into anti-airborne infection performance of stratum ventilation. Build Environ 54:29–38. https://doi.org/10.1016/j.buildenv.2012.01.017
Lin Z, Wang J, Yao T, Chow TT, Fong KF (2013) Numerical comparison of dispersion of human exhaled droplets under different ventilation methods. World Rev Sci Technol Sustain Dev 10(1–3):142–161. https://doi.org/10.1504/WRSTSD.2013.050790
Lindsley WG, King WP, Thewlis RE, Reynolds JS, Panday K, Cao G, Szalajda JV (2012) Dispersion and exposure to a cough-generated aerosol in a simulated medical examination room. J Occup Environ Hyg 9(12):681–690. https://doi.org/10.1080/15459624.2012.725986
Lipczynska A, Kaczmarczyk J, Melikov AK (2015) Thermal environment and air quality in office with personalized ventilation combined with chilled ceiling. Build Environ 92:603–614. https://doi.org/10.1016/j.buildenv.2015.05.035
Liu F, Qian H, Zheng X, Song J, Cao G, Liu Z (2019a) Evaporation and dispersion of exhaled droplets in stratified environment. IOP Conf Ser Mater Sci Eng 609:042059. https://doi.org/10.1088/1757-899x/609/4/042059
Liu HY, Hopping GC, Vaidyanathan U, Ronquillo YC, Hoopes PC, Moshirfar M (2019b) Polymerase chain reaction and its application in the diagnosis of infectious keratitis. Med Hypothesis Discov Innov Ophthalmol 8(3):152–155
Liu J, Dalgo DA, Zhu S, Li H, Zhang L, Srebric J (2019c) Performance analysis of a ductless personalized ventilation combined with radiant floor cooling system and displacement ventilation. Build Simul 12(5):905–919. https://doi.org/10.1007/s12273-019-0521-9
Liu J, Zhu S, Kim MK, Srebric J (2019d) A review of CFD analysis methods for personalized ventilation (PV) in indoor built environments. Sustainability 11(15):4166. https://doi.org/10.3390/su11154166
Liu L, Li Y, Nielsen PV, Wei J, Jensen RL (2016a) Short-range airborne transmission of expiratory droplets between two people. Indoor Air 27(2):452–462. https://doi.org/10.1111/ina.12314
Liu L, Wei J, Li Y, Ooi A (2017) Evaporation and dispersion of respiratory droplets from coughing. Indoor Air 27(1):179–190. https://doi.org/10.1111/ina.12297
Liu W, You X-Y (2011) Transportation and risk analysis of influenza indoor and outdoor transportation and exposure risk analysis of influenza aerosol. Indoor Built Environ 21(5):614–621. https://doi.org/10.1177/1420326X11426164
Liu X, Niu J (2011) Wind tunnel test of indoor air pollutant dispersion around high-rise building. ASHRAE IAQ 2010:1–6
Liu X, Niu J, Gao N, Perino M, Heiselberg P (2007) Cfd simulation of inter-flat air cross-contamination-A possible transmission path of infectious diseases. Air infiltration and Ventilation Centre. https://www.aivc.org/sites/default/files/p646_final.pdf. Accessed 24 Nov 2022
Liu X, Niu J, Perino M, Heiselberg P (2008) Numerical simulation of inter-flat air cross-contamination under the condition of single-sided natural ventilation. J Build Perform Simul 1(2):133–147. https://doi.org/10.1080/19401490802250462
Liu X, Zhang X, Min J (2019e) Spreading of droplets impacting different wettable surfaces at a Weber number close to zero. Chem Eng Sci 207:495–503. https://doi.org/10.1016/j.ces.2019.06.058
Liu XP, Niu JL, Kwok KCS (2011a) Analysis of concentration fluctuations in gas dispersion around high-rise building for different incident wind directions. J Hazard Mater 192(3):1623–1632. https://doi.org/10.1016/j.jhazmat.2011.06.090
Liu XP, Niu JL, Kwok KCS, Wang JH, Li BZ (2010) Investigation of indoor air pollutant dispersion and cross-contamination around a typical high-rise residential building: Wind tunnel tests. Build Environ 45(8):1769–1778. https://doi.org/10.1016/j.buildenv.2010.02.003
Liu XP, Niu JL, Kwok KCS, Wang JH, Li BZ (2011b) Local characteristics of cross-unit contamination around high-rise building due to wind effect: mean concentration and infection risk assessment. J Hazard Mater 192(1):160–167. https://doi.org/10.1016/j.jhazmat.2011.04.106
Liu Y, Zhao Y, Liu Z, Luo J (2016b) Numerical investigation of the unsteady flow characteristics of human body thermal plume. Build Simul 9(6):677–687. https://doi.org/10.1007/s12273-016-0296-1
Löhner R, Antil H (2020) High fidelity modeling of aerosol pathogen propagation in built environments with moving pedestrians. Int J Numer Meth in Biomed Eng 37:e3428. https://doi.org/10.1002/cnm.3428
Löhner R, Antil H, Idelsohn S, Oñate E (2020) Detailed simulation of viral propagation in the built environment. Comput Mech 66(5):1093–1107. https://doi.org/10.1007/s00466-020-01881-7
Loures FV, Röhm M, Lee CK, Santos E, Wang JP, Specht CA, Calich VLG, Urban CF, Levitz SM (2015) Recognition of Aspergillus fumigatus hyphae by human plasmacytoid dendritic cells is mediated by dectin-2 and results in formation of extracellular traps. PLoS Pathog 11(2):e1004643–e1004643. https://doi.org/10.1371/journal.ppat.1004643
Luengas A, Barona A, Hort C, Gallastegui G, Platel V, Elias A (2015) A review of indoor air treatment technologies. Rev Environ Sci Biotechnol 14(3):499–522. https://doi.org/10.1007/s11157-015-9363-9
Luksamijarulkul P, Pipitsangjan S (2015) Microbial air quality and bacterial surface contamination in ambulances during patient services. Oman Med J 30(2):104–110. https://doi.org/10.5001/omj.2015.23
Lunden MM, Revzan KL, Fischer ML, Thatcher TL, Littlejohn D, Hering SV, Brown NJ (2003a) The transformation of outdoor ammonium nitrate aerosols in the indoor environment. Atmos Environ 37(39):5633–5644. https://doi.org/10.1016/j.atmosenv.2003.09.035
Lunden MM, Thatcher TL, Hering SV, Brown NJ (2003b) Use of Time- and chemically resolved particulate data to characterize the infiltration of outdoor PM2.5 into a residence in the San Joaquin valley. Environ Sci Technol 37:4724–4732
Luongo JC, Fennelly KP, Keen JA, Zhai ZJ, Jones BW, Miller SL (2016) Role of mechanical ventilation in the airborne transmission of infectious agents in buildings. Indoor Air 26(5):666–678. https://doi.org/10.1111/ina.12267
Lv Y, Wang H, Wei S (2018) The transmission characteristics of indoor particles under two ventilation modes. Energy Build 163:1–9. https://doi.org/10.1016/j.enbuild.2017.12.028
Lyons DM, Lauring AS (2018) Mutation and epistasis in influenza virus evolution. Viruses 10:407. https://doi.org/10.3390/v10080407
Madigan MT (2009) Brock Biology of microorganisms. Pearson/Benjamin Cummings, San Francisco
Madsen AM, Larsen ST, Koponen IK, Kling KI, Barooni A, Karottki DG, Tendal K, Wolkoff P (2016) Generation and characterization of indoor fungal aerosols for inhalation studies. Appl Environ Microbiol 82(8):2479–2493. https://doi.org/10.1128/aem.04063-15
Madsen AM, Zervas A, Tendal K, Nielsen JL (2015) Microbial diversity in bioaerosol samples causing ODTS compared to reference bioaerosol samples as measured using Illumina sequencing and MALDI-TOF. Environ Res 140:255–267. https://doi.org/10.1016/j.envres.2015.03.027
Mandato S, Rondet E, Delaplace G, Barkouti A, Galet L, Accart P, Ruiz T, Cuq B (2012) Liquids’ atomization with two different nozzles: modeling of the effects of some processing and formulation conditions by dimensional analysis. Powder Technol 224:323–330. https://doi.org/10.1016/j.powtec.2012.03.014
Mander L (2016) A combinatorial approach to angiosperm pollen morphology. Proc Biol Sci. https://doi.org/10.1098/rspb.2016.2033
Marshall JW, Vincent JH, Kuehn TH, Brosseau LM (1996) Studies of ventilation efficiency in a protective isolation room by the use of a scale model. Infect Control Hosp Epidemiol 17(1):5–10. https://doi.org/10.2307/30142358
Marui VC, Souto MLS, Rovai ES, Romito GA, Chambrone L, Pannuti CM (2019) Efficacy of preprocedural mouthrinses in the reduction of microorganisms in aerosol: A systematic review. J Am Dent Assoc 150(12):1015-1026e1. https://doi.org/10.1016/j.adaj.2019.06.024
Mazej M, Butala V (2012) Investigation in the characteristics of the personal ventilation using computational fluid dynamics. Indoor Built Environ 21(6):749–771. https://doi.org/10.1177/1420326X11420456
Mazumdar S, Yin Y, Guity A, Marmion P, Gulick B, Chen Q (2010) Impact of moving objects oncontaminant concentration distributions in an inpatient ward with displacement ventilation. HVAC R Res 16(5):545–563. https://doi.org/10.1080/10789669.2010.10390921
Megri AC, Haghighat F (2007) Zonal modeling for simulating indoor environment of buildings: review, recent developments, and applications. HVAC&R Res 13(6):887–905. https://doi.org/10.1080/10789669.2007.10391461
Melikov AK (2004) Personalized ventilation. Indoor Air Supplement, 14(SUPPL. 7):157–167. https://doi.org/10.1111/j.1600-0668.2004.00284.x
Melikov AK, Skwarczynski MA, Kaczmarczyk J, Zabecky J (2013) Use of personalized ventilation for improving health, comfort, and performance at high room temperature and humidity. Indoor Air 23(3):250–263. https://doi.org/10.1111/ina.12012
Memarzadeh F, Xu W (2012) Role of air changes per hour (ACH) in possible transmission of airborne infections. Build Simul 5(1):15–28. https://doi.org/10.1007/s12273-011-0053-4
Mendell MJ, Macher JM, Kumagai K (2018) Measured moisture in buildings and adverse health effects: a review. Indoor Air 28(4):488–499. https://doi.org/10.1111/ina.12464
Menzies D, Fanning A, Yuan L, Fitzgerald JM, Blanchette G, Boldiic Ph, Brassard P, Gharbonneau M, Déry S, Libman M, Miller M, Robiliard P, Schwartzman K, Tannenbaum TN, Tremblay J, Avandano M, Gonly J, Simor A, Naus M, Taylor G, Ma M, Montaner J (2000) Hospital ventilation and risk for tuberculous infection in Canadian health care workers. Ann Intern Med 133(10):779–789. https://doi.org/10.7326/0003-4819-133-10-200011210-00010
Milner J, Vardoulakis S, Chalabi Z, Wilkinson P (2011) Modelling inhalation exposure to combustion-related air pollutants in residential buildings: application to health impact assessment. Environ Int 37(1):268–279. https://doi.org/10.1016/j.envint.2010.08.015
Milton DK, Fabian MP, Cowling BJ, Grantham ML, McDevitt JJ (2013) Influenza virus aerosols in human exhaled breath: particle size, culturability, and effect of surgical masks. PLoS Pathog 9(3):e1003205. https://doi.org/10.1371/journal.ppat.1003205
Milton DK, Glencross MP, Walters MD (2000) Risk of sick leave associated with outdoor air supply rate, humidification, and occupant complaints. Indoor Air 10(4):212–221. https://doi.org/10.1034/j.1600-0668.2000.010004212.x
Mittal R, Ni R, Seo J-H (2020) The flow physics of COVID-19. J Fluid Mech 894:F2. https://doi.org/10.1017/jfm.2020.330
Mölter A, Lindley S, de Vocht F, Agius R, Kerry G, Johnson K, Ashmore M, Terry A, Dimitroulopoulou S, Simpson A (2012) Performance of a microenviromental model for estimating personal NO2 exposure in children. Atmos Environ 51:225–233. https://doi.org/10.1016/j.atmosenv.2012.01.030
Monn C (2001) Exposure assessment of air pollutants: a review on spatial heterogeneity and indoor/outdoor/personal exposure to suspended particulate matter, nitrogen dioxide and ozone. Atmos Environ 35(1):1–32. https://doi.org/10.1016/S1352-2310(00)00330-7
Morawska L (2006) Droplet fate in indoor environments, or can we prevent the spread of infection? Indoor Air 16(5):335–347. https://doi.org/10.1111/j.1600-0668.2006.00432.x
Morawska L, Johnson GR, Ristovski ZD, Hargreaves M, Mengersen K, Corbett S, Chao CYH, Li Y, Katoshevski D (2009) Size distribution and sites of origin of droplets expelled from the human respiratory tract during expiratory activities. J Aerosol Sci 40(3):256–269. https://doi.org/10.1016/j.jaerosci.2008.11.002
Mothes N, Valenta R (2004) Biology of tree pollen allergens. Curr Allergy Asthma Rep 4(5):384–390. https://doi.org/10.1007/s11882-004-0089-y
Mousavi ES, Grosskopf KR (2015) Ventilation rates and airflow pathways in patient rooms: a case study of bioaerosol containment and removal. Ann Occup Hyg 59(9):1190–1199. https://doi.org/10.1093/annhyg/mev048
Mu D, Gao N, Zhu T (2016) Wind tunnel tests of inter-flat pollutant transmission characteristics in a rectangular multi-storey residential building, part A: effect of wind direction. Build Environ 108:159–170. https://doi.org/10.1016/j.buildenv.2016.08.032
Mu D, Shu C, Gao N, Zhu T (2017) Wind tunnel tests of inter-flat pollutant transmission characteristics in a rectangular multi-storey residential building, part B: Effect of source location. Build Environ 114:281–292. https://doi.org/10.1016/j.buildenv.2016.12.031
Mui KW, Wong LT, Wu CL, Lai ACK (2009) Numerical modeling of exhaled droplet nuclei dispersion and mixing in indoor environments. J Hazard Mater 167(1–3):736–744. https://doi.org/10.1016/j.jhazmat.2009.01.041
Muller MP, MacDougall C, Lim M (2016) Antimicrobial surfaces to prevent healthcare-associated infections: a systematic review. J Hosp Infect 92(1):7–13. https://doi.org/10.1016/j.jhin.2015.09.008
Mumtaz M, Fisher J, Blount B, Ruiz P (2012) Application of physiologically based pharmacokinetic models in chemical risk assessment. Journal of Toxicology 2012:904603. https://doi.org/10.1155/2012/904603
Murga A, Kuga K, Yoo S-J, Ito K (2019) Personal inhalation risk assessment based on a hybrid method using CFD-CSP-PBTK modelling: quantification of time-averaged and peak concentration differences. IOP Conf Ser Mater Sci Eng 609:042003. https://doi.org/10.1088/1757-899x/609/4/042003
Murga A, Long Z, Yoo S-J, Sumiyoshi E, Ito K (2020) Decreasing inhaled contaminant dose of a factory worker through a hybrid emergency ventilation system: performance evaluation in worst-case scenario. Energy Built Environ 1(3):319–326. https://doi.org/10.1016/j.enbenv.2020.04.007
Murray PR (2012) What is new in clinical microbiology-microbial identification by MALDI-TOF mass spectrometry: a paper from the 2011 William Beaumont Hospital Symposium on molecular pathology. J Mol Diagn 14(5):419–423. https://doi.org/10.1016/j.jmoldx.2012.03.007
Murray PR, Rosenthal KS, Pfaller MA (2013) Medical microbiology. Elsevier Saunders, Philadelphia
Mutuku JK, Hou W-C, Chen W-H (2020a) An overview of experiments and numerical simulations on airflow and aerosols deposition in human airways and the role of bioaerosol motion in COVID-19 transmission. Aerosol Air Qual Res 20(6):1172–1196. https://doi.org/10.4209/aaqr.2020.04.0185
Mutuku JK, Hou W-C, Chen W-H (2020b) Two-phase flow dynamics and PM2.5 Deposition in healthy and obstructed human airways during inhalation. Aerosol Air Qual Res 20:1094–1110. https://doi.org/10.4209/aaqr.2020.03.0107
Myatt TA, Johnston SL, Zuo Z, Wand M, Kebadze T, Rudnick S, Milton DK (2004) Detection of airborne rhinovirus and its relation to outdoor air supply in office environments. Am J Respir Crit Care Med 169(11):1187–1190. https://doi.org/10.1164/rccm.200306-760OC
Napoli C, Marcotrigiano V, Montagna MT (2012) Air sampling procedures to evaluate microbial contamination: a comparison between active and passive methods in operating theatres. BMC Public Health 12:594. https://doi.org/10.1186/1471-2458-12-594
Nardell EA, Keegan J, Cheney SA, Etkind SC (1991) Airborne Infection: Theoretical limits of protection achievable by building ventilation. Am Rev Respir Dis 144(2):302–306. https://doi.org/10.1164/ajrccm/144.2.302
Nasir ZA, Hayes E, Williams B, Gladding T, Rolph C, Khera S, Jackson S, Bennett A, Collins S, Parks S, Attwood A, Kinnersley RP, Walsh K, Alcega SG, Pollard SJT, Drew G, Coulon F, Tyrrel S (2019) Scoping studies to establish the capability and utility of a real-time bioaerosol sensor to characterise emissions from environmental sources. Sci Total Environ 648:25–32. https://doi.org/10.1016/j.scitotenv.2018.08.120
Nasir ZA, Rolph CA, Collins S, Stevenson DW, Gladding TL, Hayes ET, Williams B, Khera S, Jackson S, Bennett A, Parks S, Kinnersley RP, Walsh K, Pollard SJT, Drew G, Alcega SG, Coulon F, Tyrrel SF (2018) A Controlled study on the characterisation of bioaerosols emissions from compost. Atmosphere 9(10):379. https://doi.org/10.3390/atmos9100379
Nazaroff WW (2004) Indoor particle dynamics. Indoor Air 14(Suppl 7):175–183. https://doi.org/10.1111/j.1600-0668.2004.00286.x
Nazaroff WW (2016) Indoor bioaerosol dynamics. Indoor Air 26(1):61–78. https://doi.org/10.1111/ina.12174
Neely AN, Orloff MM (2001) Survival of some medically important fungi on hospital fabrics and plastics. J Clin Microbiol 39(9):3360–3361. https://doi.org/10.1128/jcm.39.9.3360-3361.2001
Netz RR (2020) Mechanisms of airborne infection via evaporating and sedimenting droplets produced by speaking. J Phys Chem B. https://doi.org/10.1021/acs.jpcb.0c05229
Ni Y, Shi G, Qu J (2020) Indoor PM2.5, tobacco smoking and chronic lung diseases: a narrative review. Environ Res 181:108910. https://doi.org/10.1016/j.envres.2019.108910
Nicas M (1996) An analytical framework for relating dose, risk, and incidence: an application to occupational tuberculosis infection. Risk Anal 16(4):527–538. https://doi.org/10.1111/j.1539-6924.1996.tb01098.x
Nielsen PV (2009) Control of airborne infectious diseases in ventilated spaces. J R Soc Interface 6(suppl_6):S747–S755. https://doi.org/10.1098/rsif.2009.0228.focus
Nielsen PV (2015) Fifty years of CFD for room air distribution. Build Environ 91:78–90. https://doi.org/10.1016/j.buildenv.2015.02.035
Nielsen PV, Bartholomaeussen NM, Jakubowska E, Jiang H, Jonsson OT, Krawiecka K,Mierzejewski A, Jessica SJ, Trampczynska K, Polak M, Soennichsen M (2007a) Chair with integrated personalized ventilation for minimizing cross infection. Aalborg University. https://vbn.aau.dk/ws/portalfiles/portal/13819115/Chair_with_Integrated_Personalized_Ventilation_for_Minimizing_Cross_Infection. Accessed 24 Nov 2022
Nielsen PV, Hyldgaard CE, Melikov A, Andersen H, Soennichsen M (2007b) Personal exposure between people in a room ventilated by textile terminals—with and without personalized ventilation. HVAC R Res 13(4):635–643. https://doi.org/10.1080/10789669.2007.10390976
Nielsen PV, Li Y, Buus M, Winther FV (2010) Risk of cross-infection in a hospital ward with downward ventilation. Build Environ 45(9):2008–2014. https://doi.org/10.1016/j.buildenv.2010.02.017
Nigro OD, Steward GF (2015) Differential specificity of selective culture media for enumeration of pathogenic vibrios: advantages and limitations of multi-plating methods. J Microbiol Methods 111:24–30. https://doi.org/10.1016/j.mimet.2015.01.014
Niu J, Tung C, Wan J, Cheng J (2005) CFD simulation of interflat air flow for the study of the spread of aerosol transmitted infectious diseases. International Building Performance Simulation Association. http://www.ibpsa.org/proceedings/BS2005/BS05_0853_858.pdf. Accessed 24 Nov 2022
Niu J, Tung TCW (2008) On-site quantification of re-entry ratio of ventilation exhausts in multi-family residential buildings and implications. Indoor Air 18(1):12–26. https://doi.org/10.1111/j.1600-0668.2007.00500.x
Noakes CJ, Andrew Sleigh P (2009) Mathematical models for assessing the role of airflow on the risk of airborne infection in hospital wards. J R Soc Interface 6(SUPPL. 6):S791–S800. https://doi.org/10.1098/rsif.2009.0305.focus
Novozhilov V (2007) Fire suppression studies. Therm Sci 11(2):161–180. https://doi.org/10.2298/TSCI0702161N
Olesen BW, Simone A, Krajčík M, Causone F, De Carli M (2011) Experimental study of air distribution and ventilation effectiveness in a room with a combination of different mechanical ventilation and heating/cooling systems. Int J Vent 9(4):371–383. https://doi.org/10.1080/14733315.2011.11683895
Olmedo I, Nielsen PV, Ruiz de Adana M, Jensen RL, Grzelecki P (2012) Distribution of exhaled contaminants and personal exposure in a room using three different air distribution strategies. Indoor Air 22(1):64–76. https://doi.org/10.1111/j.1600-0668.2011.00736.x
Ouazia B, Macdonald I, Tardif M, Thompson A, Booth D (2012) Contaminant removal effectiveness of displacement ventilationsystems during heating season; summary results from three field studies. ASHRAE Trans 118(2):292–299
Ouazia B, Tardif M, Macdonald I, Thompson A, Booth D (2011) In-situ performance of displacement ventilation system in Canadian schools with radiant heating systems. ASHRAE Annual Conference, Montreal, Quebec, pp 1–13
Ozkaynak H, Palma T, Touma JS, Thurman J (2007) Modeling population exposures to outdoor sources of hazardous air pollutants. J Expos Sci Environ Epidemiol 18(1):45–58. https://doi.org/10.1038/sj.jes.7500612
Özkaynak H, Palma T, Touma JS, Thurman J (2008) Modeling population exposures to outdoor sources of hazardous air pollutants. J Eposure Sci Environ Epidemiol 18(1):45–58. https://doi.org/10.1038/sj.jes.7500612
Pablos I, Wildner S, Asam C, Wallner M, Gadermaier G (2016) Pollen allergens for molecular diagnosis. Curr Allergy Asthma Rep 16(4):31. https://doi.org/10.1007/s11882-016-0603-z
Pantelic J, Sze-To GN, Tham KW, Chao CYH, Khoo YCM (2009) Personalized ventilation as a control measure for airborne transmissible disease spread. J R Soc Interface 6(SUPPL. 6):S715–S726. https://doi.org/10.1098/rsif.2009.0311.focus
Pantelic J, Tham KW (2011) Assessment of the ability of different ventilation systems to serve as a control measure against airborne infectious disease transmission using Wells-Riley approach. American Society of Heating Refrigeration and Airconditioning Engineers. https://scholarbank.nus.edu.sg/handle/10635/45912. Accessed 24 Nov 2022
Pantelic J, Tham KW (2013) Adequacy of air change rate as the sole indicator of an air distribution system’s effectiveness to mitigate airborne infectious disease transmission caused by a cough release in the room with overhead mixing ventilation: a case study. HVAC R Res 19(8):947–961. https://doi.org/10.1080/10789669.2013.842447
Pantelic J, Tham KW, Licina D (2015) Effectiveness of a personalized ventilation system in reducing personal exposure against directly released simulated cough droplets. Indoor Air 25(6):683–693. https://doi.org/10.1111/ina.12187
Pantelic J, Wai TK (2009) Effect of the room air motion on the dispersion of expiratory droplets in the personalized ventilated room. International Society of Indoor Air Quality and Climate. https://scholarbank.nus.edu.sg/handle/10635/45936. Accessed 24 Nov 2022
Park DY, Chang S (2019) Numerical investigation of thermal comfort and transport of expiratory contaminants in a ventilated office with an air curtain system. Indoor Built Environ 28(3):401–421. https://doi.org/10.1177/1420326x18770238
Park JW, Kim HR, Hwang J (2016) Continuous and real-time bioaerosol monitoring by combined aerosol-to-hydrosol sampling and ATP bioluminescence assay. Anal Chim Acta 941:101–107. https://doi.org/10.1016/j.aca.2016.08.039
Patankar SV (1980) Numerical heat transfer and fluid flow. Hemisphere Publishing Corporation, New York
Penconek A, Michalczuk U, Sienkiewicz A, Moskal A (2019) The effect of desert dust particles on rheological properties of saliva and mucus. Environ Sci Pollut Res Int 26(12):12150–12157. https://doi.org/10.1007/s11356-019-04628-x
Pendar M-R, Páscoa JC (2020) Numerical modeling of the distribution of virus carrying saliva droplets during sneeze and cough. Phys Fluids 32(8):083305. https://doi.org/10.1063/5.0018432
Peng S, Chen Q, Liu E (2020) The role of computational fluid dynamics tools on investigation of pathogen transmission: prevention and control. Sci Total Environ 746:142090. https://doi.org/10.1016/j.scitotenv.2020.142090
Peteranderl C, Herold S, Schmoldt C (2016) Human Influenza virus infections. Semin Respir Crit Care Med 37(4):487–500. https://doi.org/10.1055/s-0036-1584801
Phu H-T, Park Y, Andrews AJ, Marabella I, Abraham A, Mimmack R, Olson BA, Chaika J, Floersch E, Remskar M, Hume JR, Fischer GA, Belani K, Hogan CJ (2020) Design and evaluation of a portable negative pressure hood with HEPA filtration to protect health care workers treating patients with transmissible respiratory infections. Am J Infect Control. https://doi.org/10.1016/j.ajic.2020.06.203
Phuong NL, Ito K (2015) Investigation of flow pattern in upper human airway including oral and nasal inhalation by PIV and CFD. Build Environ 94:504–515. https://doi.org/10.1016/j.buildenv.2015.10.002
Phuong NL, Khoa ND, Ito K (2020) Comparative numerical simulation of inhaled particle dispersion in upper human airway to analyse intersubject differences. Indoor Built Environ 29(6):793–809. https://doi.org/10.1177/1420326x19894128
Pitt JI, Christian JH (1970) Heat resistance of xerophilic fungi based on microscopical assessment of spore survival. Appl Microbiol 20(5):682–686
Pleschka S (2013) Overview of influenza viruses. Curr Top Microbiol Immunol 370:1–20. https://doi.org/10.1007/82_2012_272
Pomeranz G, Pando R, Hindiyeh M, Sherbany H, Meningher T, Sharabi S, Kolet L, Pomeranz A, Mendelson E, Mandelboim M (2019) Rhinovirus infections in infants suggest that early detection can prevent unnecessary treatment. J Clin Virol 115:11–17. https://doi.org/10.1016/j.jcv.2019.03.012
Poon WCK, Brown AT, Direito SOL, Hodgson DJM, Le Nagard L, Lips A, MacPhee CA, Marenduzzo D, Royer JR, Silva AF, Thijssen JH, Titmuss S (2020) Soft matter science and the COVID-19 pandemic. Soft Matter 16(36):8310–8324. https://doi.org/10.1039/D0SM01223H
Prat C, Lacoma A (2016) Bacteria in the respiratory tract-how to treat? Or do not treat? Int J Infect Dis 51:113–122. https://doi.org/10.1016/j.ijid.2016.09.005
Predicala BZ, Urban JE, Maghirang RG, Jerez SB, Goodband RD (2002) Assessment of bioaerosols in swine barns by filtration and impaction. Curr Microbiol 44(2):136–140. https://doi.org/10.1007/s00284-001-0064-y
Prussin AJ, Belser JA, Bischoff W, Kelley ST, Lin K, Lindsley WG, Nshimyimana JP, Schuit M, Wu Z, Bibby K, Marr LC (2020) Viruses in the Built Environment (VIBE) meeting report. Microbiome 8(1):1. https://doi.org/10.1186/s40168-019-0777-4
Prussin AJ, Schwake DO, Marr LC (2017) Ten questions concerning the aerosolization and transmission of Legionella in the built environment. Build Environ 123:684–695. https://doi.org/10.1016/j.buildenv.2017.06.024
Pyankov OV, Bodnev SA, Pyankova OG, Agranovski IE (2018) Survival of aerosolized coronavirus in the ambient air. J Aerosol Sci 115:158–163. https://doi.org/10.1016/j.jaerosci.2017.09.009
Qian H, Li Y (2010) Removal of exhaled particles by ventilation and deposition in a multibed airborne infection isolation room. Indoor Air 20(4):284–297. https://doi.org/10.1111/j.1600-0668.2010.00653.x
Qian H, Li Y, Nielsen PV, Hyldgaard CE (2008) Dispersion of exhalation pollutants in a two-bed hospital ward with a downward ventilation system. Build Environ 43(3):344–354. https://doi.org/10.1016/j.buildenv.2006.03.025
Qian H, Li Y, Nielsen PV, Hyldgaard CE, Wong TW, Chwang ATY (2006) Dispersion of exhaled droplet nuclei in a two-bed hospital ward with three different ventilation systems. Indoor Air 16(2):111–128. https://doi.org/10.1111/j.1600-0668.2005.00407.x
Qian H, Li Y, Seto WH, Ching P, Ching WH, Sun HQ (2010) Natural ventilation for reducing airborne infection in hospitals. Build Environ 45(3):559–565. https://doi.org/10.1016/j.buildenv.2009.07.011
Qian H, Zheng X (2018) Ventilation control for airborne transmission of human exhaled bio-aerosols in buildings. J Thorac Dis 10:S2295–S2304. https://doi.org/10.21037/jtd.2018.01.24
Rantio-Lehtimäki A, Viander M, Koivikko A (1994) Airborne birch pollen antigens in different particle sizes. Clin Exp Allergy 24(1):23–28. https://doi.org/10.1111/j.1365-2222.1994.tb00912.x
Rath B, Conrad T, Myles P, Alchikh M, Ma X, Hoppe C, Tief F, Chen X, Obermeier P, Kisler B, Schweiger B (2017) Influenza and other respiratory viruses: standardizing disease severity in surveillance and clinical trials. Expert Rev Anti Infect Ther 15(6):545–568. https://doi.org/10.1080/14787210.2017.1295847
Razzini K, Castrica M, Menchetti L, Maggi L, Negroni L, Orfeo NV, Pizzoccheri A, Stocco M, Muttini S, Balzaretti CM (2020) SARS-CoV-2 RNA detection in the air and on surfaces in the COVID-19 ward of a hospital in Milan, Italy. Sci Total Environ 742:140540. https://doi.org/10.1016/j.scitotenv.2020.140540
Reddy MS, Vedamuthu ER, Washam CJ, Reinbold GW (1972) Agar medium for differential enumeration of lactic streptococci. Appl Microbiol 24(6):947–952
Ren Z, Stewart J (2005) Prediction of personal exposure to contaminant sources in industrial buildings using a sub-zonal model. Environ Model Softw 20(5):623–638. https://doi.org/10.1016/j.envsoft.2004.03.007
Rhodes M (2008) Introduction to particle technology. John Wiley & Sons, Ltd, Chichester
Rodríguez R, Villalba M, Batanero E, Palomares O, Salamanca G (2007) Emerging pollen allergens. Biomed Pharmacother 61(1):1–7. https://doi.org/10.1016/j.biopha.2006.09.014
Rothan HA, Byrareddy SN (2020) The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmun 109:102433. https://doi.org/10.1016/j.jaut.2020.102433
Rui Z, Guangbei T, Jihong L (2008) Study on biological contaminant control strategies under different ventilation models in hospital operating room. Build Environ 43(5):793–803. https://doi.org/10.1016/j.buildenv.2007.01.018
Ryan KA, Bewley KR, Fotheringham SA, Brown P, Hall Y, Marriott AC, Cavell BE, Tree JA, Allen L, Aram MJ, Bean TJ, Brunt E, Buttigieg KR, Carter DP, Cobb R, Coombes NS, Findlay-Wilson SJ, Godwin KJ, Gooch KE, Gouriet J, Halkerston R, Harris DJ, Hender TH, Humphries HE, Hunter L, Ho CMK, Kennard CL, Leung S, Longet S, Ngabo D, Osman KL, Paterson J, Penn EJ, Steven T. Pullan, Emma Rayner, Oliver Skinner, Kimberley Steeds, Irene Taylor, Tipton T, Thomas S, Turner C, Watson RJ, Wiblin NR, Charlton S, Hallis B, Hiscox JA, Funnell S, Dennis MJ, Whittaker CJ, Catton MG, Druce J, Salguero FJ, Carroll MW (2020) Dose-dependent response to infection with SARS-CoV-2 in the ferret model: evidence of protection to re-challenge. bioRxiv, 2020.2005.2029.123810. https://doi.org/10.1101/2020.05.29.123810
Saarinen PE, Kalliomäki P, Tang JW, Koskela H (2015) Large eddy simulation of air escape through a hospital isolation room single hinged doorway—validation by using tracer gases and simulated smoke videos. PLoS One 10(7):e0130667. https://doi.org/10.1371/journal.pone.0130667
Sadrizadeh S, Holmberg S, Tammelin A (2014a) A numerical investigation of vertical and horizontal laminar airflow ventilation in an operating room. Build Environ 82:517–525. https://doi.org/10.1016/j.buildenv.2014.09.013
Sadrizadeh S, Pantelic J, Sherman M, Clark J, Abouali O (2018) Airborne particle dispersion to an operating room environment during sliding and hinged door opening. J Infect Public Health 11(5):631–635. https://doi.org/10.1016/j.jiph.2018.02.007
Sadrizadeh S, Tammelin A, Ekolind P, Holmberg S (2014b) Influence of staff number and internal constellation on surgical site infection in an operating room. Particuology 13:42–51. https://doi.org/10.1016/j.partic.2013.10.006
Sajjadi H, Salmanzadeh M, Ahmadi G, Jafari S (2016) Simulations of indoor airflow and particle dispersion and deposition by the lattice Boltzmann method using LES and RANS approaches. Build Environ 102:1–12. https://doi.org/10.1016/j.buildenv.2016.03.006
Sakharov AS, Zhukov K (2020) Study of an air curtain in the context of individual protection from exposure to coronavirus (SARS-CoV-2) contained in cough-generated fluid particles. Physics 2(3):340–351. https://doi.org/10.3390/physics2030018
Salmanzadeh M, Zahedi G, Ahmadi G, Marr DR, Glauser M (2012) Computational modeling of effects of thermal plume adjacent to the body on the indoor airflow and particle transport. J Aerosol Sci 53:29–39. https://doi.org/10.1016/j.jaerosci.2012.05.005
Salthammer T (2020) Emerging indoor pollutants. Int J Hyg Environ Health 224:113423. https://doi.org/10.1016/j.ijheh.2019.113423
Sarkar A, Xu F, Lee S (2019) Human saliva and model saliva at bulk to adsorbed phases – similarities and differences. Adv Coll Interface Sci 273:102034. https://doi.org/10.1016/j.cis.2019.102034
Satheesan MK, Mui KW, Wong LT (2020) A numerical study of ventilation strategies for infection risk mitigation in general inpatient wards. Build Simul 13(4):887–896. https://doi.org/10.1007/s12273-020-0623-4
Scharfman BE, Techet AH, Bush JWM, Bourouiba L (2016) Visualization of sneeze ejecta: steps of fluid fragmentation leading to respiratory droplets. Exp Fluids 57(2):24. https://doi.org/10.1007/s00348-015-2078-4
Scheuch G (2020) Breathing is enough: for the spread of influenza virus and SARS-CoV-2 by breathing only. J Aerosol Med Pulm Drug Deliv. https://doi.org/10.1089/jamp.2020.1616
Schiavon S, Bauman FS, Tully B, Rimmer J (2015) Chilled ceiling and displacement ventilation system: laboratory study with high cooling load. Sci Technol Built Environ 21(7):944–956. https://doi.org/10.1080/23744731.2015.1034061
Schroeter JD, Kimbell JS, Asgharian B, Tewksbury EW, Singal M (2012) Computational fluid dynamics simulations of submicrometer and micrometer particle deposition in the nasal passages of a Sprague-Dawley rat. J Aerosol Sci 43(1):31–44. https://doi.org/10.1016/j.jaerosci.2011.08.008
Schuijs MJ, Willart MA, Vergote K, Gras D, Deswarte K, Ege MJ, Madeira FB, Beyaert R, Loo G, Bracher F, Mutius E, Chanez P, Lambrecht BN, Hammad H (2015) Farm dust and endotoxin protect against allergy through A20 induction in lung epithelial cells. Science 349(6252):1106–1110. https://doi.org/10.1126/science.aac6623
Seepana S, Lai ACK (2012) Experimental and numerical investigation of interpersonal exposure of sneezing in a full-scale chamber. Aerosol Sci Technol 46(5):485–493. https://doi.org/10.1080/02786826.2011.640365
Seymour MJ, Alani A, Manning A, Jiang J (2000) CFD based airflow modelling to investigate the effectiveness of control methods intended to prevent the transmission of airborne organisms. Paper presented at the Air Distribution in Rooms: Ventilation for Health and Sustainable Environment, Reading, UK
Shajahan A, Culp CH, Williamson B (2019) Effects of indoor environmental parameters related to building heating, ventilation, and air conditioning systems on patients’ medical outcomes: a review of scientific research on hospital buildings. Indoor Air 29(2):161–176. https://doi.org/10.1111/ina.12531
Shao S, Zhou D, He R, Li J, Zou S, Mallery K, Kumar S, Yang S, Hong J (2021) Risk assessment of airborne transmission of COVID-19 by asymptomatic individuals under different practical settings. J Aerosol Sci 151:105661. https://doi.org/10.1016/j.jaerosci.2020.105661
Shao X, Liang S, Li X, Liang C, Yan S (2020) Quantitative effects of supply air and contaminant sources on steady contaminant distribution in ventilated space with air recirculation. Build Environ 171:106672. https://doi.org/10.1016/j.buildenv.2020.106672
Shi H, Tarabara VV (2018) Charge, size distribution and hydrophobicity of viruses: Effect of propagation and purification methods. J Virol Methods 256:123–132. https://doi.org/10.1016/j.jviromet.2018.02.008
Shi Z, Lu Z, Chen Q (2019) Indoor airflow and contaminant transport in a room with coupled displacement ventilation and passive-chilled-beam systems. Build Environ 161:106244. https://doi.org/10.1016/j.buildenv.2019.106244
Short CA, Al-Maiyah S (2009) Design strategy for low-energy ventilation and cooling of hospitals. Build Res Inf 37(3):264–292. https://doi.org/10.1080/09613210902885156
Shrubsole C, Ridley I, Biddulph P, Milner J, Vardoulakis S, Ucci M, Wilkinson P, Chalabi Z, Davies M (2012) Indoor PM2.5 exposure in London’s domestic stock: modelling current and future exposures following energy efficient refurbishment. Atmos Environ 62:336–343
Singh SK (2016) Middle East respiratory syndrome virus pathogenesis. Semin Respir Crit Care Med 37(4):572–577. https://doi.org/10.1055/s-0036-1584796
Singhal N, Kumar M, Kanaujia PK, Virdi JS (2015) MALDI-TOF mass spectrometry: an emerging technology for microbial identification and diagnosis. Front Microbiol 6:791. https://doi.org/10.3389/fmicb.2015.00791
Siqueira JF Jr, Rôças IN (2003) PCR methodology as a valuable tool for identification of endodontic pathogens. J Dent 31(5):333–339. https://doi.org/10.1016/s0300-5712(03)00051-4
Smith M, Berger U, Behrendt H, Bergmann KC (2014) Pollen and pollinosis. Chem Immunol Allergy 100:228–233. https://doi.org/10.1159/000358743
Snyder H (2019) Literature review as a research methodology: an overview and guidelines. J Bus Res 104:333–339. https://doi.org/10.1016/j.jbusres.2019.07.039
Soares TL, Jesus ON, Souza EH, Rossi ML, Oliveira EJ (2018) Comparative pollen morphological analysis in the subgenera Passiflora and Decaloba. An Acad Bras Cienc 90(2 suppl 1):2381–2396. https://doi.org/10.1590/0001-3765201720170248
Soni SK, Kirar PK, Kolhe P, Sahu KC (2020) Deformation and breakup of droplets in an oblique continuous air stream. Int J Multiph Flow 122:103141. https://doi.org/10.1016/j.ijmultiphaseflow.2019.103141
Spalding DB (1981) A general purpose computer program for multi-dimensional one- and two-phase flow. Math Comput Simul 23(3):267–276. https://doi.org/10.1016/0378-4754(81)90083-5
Spiegelman D, Whissell G, Greer CW (2005) A survey of the methods for the characterization of microbial consortia and communities. Can J Microbiol 51(5):355–386. https://doi.org/10.1139/w05-003
Srebric J, Yuan J, Novoselac A (2008) On-site experimental validation of a coupled multizone and CFD model for building contaminant transport simulations. ASHRAE Transactions, 14(1):273–281
Srivastav A, Santibanez TA, Lu PJ, Stringer MC, Dever JA, Bostwick M, Stanley-Kurtz M, Qualls NL, Williams WW (2018) Preventive behaviors adults report using to avoid catching or spreading influenza, United States, 2015-16 influenza season. Plos One 13(3):e0195085. https://doi.org/10.1371/journal.pone.0195085
Stadnytskyi V, Bax CE, Bax A, Anfinrud P (2020) The airborne lifetime of small speech droplets and their potential importance in SARS-CoV-2 transmission. Proc Natl Acad Sci 117(22):11875. https://doi.org/10.1073/pnas.2006874117
Steiner S, Herve P, Pak C, Majeed S, Sandoz A, Kuczaj A, Hoeng J (2020) Development and testing of a new-generation aerosol exposure system: the independent holistic air-liquid exposure system (InHALES). Toxicol in Vitro 67:104909. https://doi.org/10.1016/j.tiv.2020.104909
Stewart J, Ren Z (2006) COwZ—a subzonal indoor airflow, temperature and contaminant dispersion model. Build Environ 41(12):1631–1648. https://doi.org/10.1016/j.buildenv.2005.06.015
Stilianakis NI, Drossinos Y (2010) Dynamics of infectious disease transmission by inhalable respiratory droplets. J R Soc Interface 7(50):1355–1366. https://doi.org/10.1098/rsif.2010.0026
Stockwell RE, Ballard EL, O’Rourke P, Knibbs LD, Morawska L, Bell SC (2019) Indoor hospital air and the impact of ventilation on bioaerosols: a systematic review. J Hosp Infect 103(2):175–184. https://doi.org/10.1016/j.jhin.2019.06.016
Sun W, Ji J (2007) Transport of droplets expelled by coughing in ventilated rooms. Indoor Built Environ 16(6):493–504. https://doi.org/10.1177/1420326X07084290
Sun Y, Wang Z, Zhang Y, Sundell J (2011) In China, students in crowded dormitories with a low ventilation rate have more common colds: evidence for airborne transmission. Plos One 6(11):27140. https://doi.org/10.1371/journal.pone.0027140
Sundell J, Levin H, Nazaroff WW, Cain WS, Fisk WJ, Grimsrud DT, Gyntelberg F, Li Y, Persily AK, Pickering AC, Samet JM, Spengler JD, Taylor ST, Weschler CJ (2011) Ventilation rates and health: multidisciplinary review of the scientific literature. Indoor Air 21(3):191–204. https://doi.org/10.1111/j.1600-0668.2010.00703.x
Sung JY, Hwang Y, Shin MH, Park MS, Lee SH, Yong D, Lee K (2018) Utility of conventional culture and MALDI-TOF MS for identification of microbial communities in bronchoalveolar lavage fluid in comparison with the GS junior next generation sequencing system. Ann Lab Med 38(2):110–118. https://doi.org/10.3343/alm.2018.38.2.110
Tang JW, Li Y, Eames I, Chan PKS, Ridgway GL (2006) Factors involved in the aerosol transmission of infection and control of ventilation in healthcare premises. J Hosp Infect 64(2):100–114. https://doi.org/10.1016/j.jhin.2006.05.022
Tang JW, Liebner TJ, Craven BA, Settles GS (2009) A schlieren optical study of the human cough with and without wearing masks for aerosol infection control. J R Soc Interface 6(suppl_6):S727-S736. https://doi.org/10.1098/rsif.2009.0295.focus
Tao Y, Inthavong K, Petersen P, Mohanarangam K, Yang W, Tu J (2020) Vortex structures and wake flow analysis from moving manikin models. Indoor Built Environ 30(3):347–362. https://doi.org/10.1177/1420326x19893013
Tao Y, Yang W, Ito K, Inthavong K (2019) Computational fluid dynamics investigation of particle intake for nasal breathing by a moving body. Exp Comput Multiph Flow 1(3):212–218. https://doi.org/10.1007/s42757-019-0014-1
Taylor J, Lai KM, Nasir ZA (2012) Human factors and bioagent transmission following an indoor bioterror attack. J Bioterror Biodef 3(1):1000116. https://doi.org/10.4172/2157-2526.1000116
Taylor-Robinson D, Tyrrell DA (1962) Serotypes of viruses (rhinoviruses) isolated from common colds. Lancet 1(7227):452–454. https://doi.org/10.1016/s0140-6736(62)91418-6
Tham KW, Pantelic J (2011) Cough released airborne infection disease transmission control with ventilation at various infectorsusceptible distances. Paper presented at the IAQ Conference
Thompson KA, Bennett AM (2017) Persistence of influenza on surfaces. J Hosp Infect 95(2):194–199. https://doi.org/10.1016/j.jhin.2016.12.003
Tian ZF, Tu JY, Yeoh GH, Yuen RKK (2007) Numerical studies of indoor airflow and particle dispersion by large Eddy simulation. Build Environ 42(10):3483–3492. https://doi.org/10.1016/j.buildenv.2006.10.047
To KKW, Yip CCY, Yuen KY (2017) Rhinovirus - from bench to bedside. J Formos Med Assoc 116(7):496–504. https://doi.org/10.1016/j.jfma.2017.04.009
Tran K, Cimon K, Severn M, Pessoa-Silva CL, Conly J (2012) Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: a systematic review. PLoS One 7(4):e35797. https://doi.org/10.1371/journal.pone.0035797
Tung YC, Hu SC (2008) Infection risk of indoor airborne transmission of diseases in multiple spaces. Archit Sci Rev 51(1):14–20. https://doi.org/10.3763/asre.2008.5103
Urbán A, Zaremba M, Malý M, Józsa V, Jedelský J (2017) Droplet dynamics and size characterization of high-velocity airblast atomization. Int J Multiph Flow 95:1–11. https://doi.org/10.1016/j.ijmultiphaseflow.2017.02.001
Usachev EV, Usacheva OV, Agranovski IE (2013) Surface plasmon resonance-based real-time bioaerosol detection. J Appl Microbiol 115(3):766–773. https://doi.org/10.1111/jam.12267
Vadivukkarasan M, Dhivyaraja K, Panchagnula MV (2020) Breakup morphology of expelled respiratory liquid: from the perspective of hydrodynamic instabilities. Phys Fluids 32(9):094101. https://doi.org/10.1063/5.0022858
Valero N, Aguilera I, Llop S, Esplugues A, de Nazelle A, Ballester F, Sunyer J (2009) Concentrations and determinants of outdoor, indoor and personal nitrogen dioxide in pregnant women from two Spanish birth cohorts. Environ Int 35(8):1196–1201. https://doi.org/10.1016/j.envint.2009.08.002
Verijkazemi K, Mansouri N, Moattar F, Khezri SM (2018) Evaluation of indoor PM distribution by CONTAM Airflow model and real time measuring: model description and validation. Avicenna J Environ Health Eng 5(1):42–49. https://doi.org/10.15171/ajehe.2018.06
Vianello A, Jensen RL, Liu L, Vollertsen J (2019) Simulating human exposure to indoor airborne microplastics using a breathing thermal manikin. Sci Rep 9(1):8670. https://doi.org/10.1038/s41598-019-45054-w
Vidlak D, Kielian T (2016) Infectious dose dictates the host response during Staphylococcus aureus orthopedic-implant biofilminfection. Infect Immun 84(7):1957. https://doi.org/10.1128/IAI.00117-16
Villafruela JM, Olmedo I, Berlanga FA, Ruiz de Adana M (2019) Assessment of displacement ventilation systems in airborne infection risk in hospital rooms. PLoS One 14(1):e0211390. https://doi.org/10.1371/journal.pone.0211390
Viswanathan H (2019) Breakup and coalescence of drops during transition from dripping to jetting in a Newtonian fluid. Int J Multiph Flow 112:269–285. https://doi.org/10.1016/j.ijmultiphaseflow.2018.09.016
Vogazianos P, Argyropoulos CD, Haralambous C, Mikellidou CV, Boustras G, Andreou M, Silvestros V, Theofanous F, Soteriou S, Gregoriou I, Jaber-Apostolidou A, Demetriou A, Athanasiadou M, Stylianou C, Michael M, Herodotou H, Alexandrou D, Kalakouta O, Pana ZD (2021) Impact assessment of COVID-19 non-pharmaceutical interventions in long term care facilities in Cyprus: Safety improvement strategy. Saf Sci 143:105415. https://doi.org/10.1016/j.ssci.2021.105415
Vuorinen V, Aarnio M, Alava M, Alopaeus V, Atanasova N, Auvinen M, Balasubramanian N, Bordbar H, Erästö P, Grande R, Hayward N, Hellsten A, Hostikka S, Hokkanen J, Kaario O, Karvinen A, Kivistö I, Korhonen M, Kosonen R, Kuusela J, Lestinen S, Laurila E, Nieminen HJ, Peltonen P, PokkJ i, Puisto A, Råback P, Salmenjoki H, Sironen T, Österberg M (2020) Modelling aerosol transport and virus exposure with numerical simulations in relation to SARS-CoV-2 transmission by inhalation indoors. Saf Sci 130:104866. https://doi.org/10.1016/j.ssci.2020.104866
Wady L, Larsson L (2005) Determination of microbial volatile organic compounds adsorbed on house dust particles and gypsum board using SPME/GC-MS. Indoor Air 15(Suppl 9):27–32. https://doi.org/10.1111/j.1600-0668.2005.00293.x
Wai TK, Pantelic J (2009) Influence of different personalized air terminal Devices on the motion of expiratory droplets released in the closed vicinity of the occupant. Paper presented at the 9th International Conference and Exhibition - Healthy Buildings 2009, HB 2009
Walsh RL, Camilli A (2011) Streptococcus pneumoniae is desiccation tolerant and infectious upon rehydration. mBio 2(3):e00092–00011. https://doi.org/10.1128/mBio.00092-11
Walton GN (1989) AIRNET - a computer program for building airflow network modeling. U.S. Department of Commerce. https://nvlpubs.nist.gov/nistpubs/Legacy/IR/nistir89-4072.pdf. Accessed 24 Nov 2022
Walton GN, Dols WS (2005) CONTAM 2.4 User Guide and Program Documentation. National Institute of Standards and Technology. https://nvlpubs.nist.gov/nistpubs/Legacy/IR/nistir7251.pdf. Accessed 24 Nov 2022
Wan MP, Chao CYH, Ng YD, Sze To GN, Yu WC (2007) Dispersion of expiratory droplets in a general hospital ward with ceiling mixing type mechanical ventilation system. Aerosol Sci Technol 41(3):244–258. https://doi.org/10.1080/02786820601146985
Wang C, Holmberg S, Sadrizadeh S (2019a) Impact of door opening on the risk of surgical site infections in an operating room with mixing ventilation. Indoor Built Environ 0(0):1420326X19888276. https://doi.org/10.1177/1420326x19888276
Wang CT (1999) Diagnosing and treating asymptomatic tuberculosis infection. Can Fam Physician 45:2397–2404
Wang H, Zhai Z (2016) Advances in building simulation and computational techniques: a review between 1987 and 2014. Energy and Buildings 128:319–335. https://doi.org/10.1016/j.enbuild.2016.06.080
Wang J, Huo Q, Zhang T, Wang S, Battaglia F (2020) Numerical investigation of gaseous pollutant cross-transmission for single-sided natural ventilation driven by buoyancy and wind. Build Environ 172:106705. https://doi.org/10.1016/j.buildenv.2020.106705
Wang J-X, Cao X, Chen Y-P (2021) An air distribution optimization of hospital wards for minimizing cross-infection. J Clean Prod 279:123431. https://doi.org/10.1016/j.jclepro.2020.123431
Wang JH, Niu JL, Liu XP, Yu CWF (2010a) Assessment of pollutant dispersion in the re-entrance space of a high-rise residential building, using wind tunnel simulations. Indoor Built Environ 19(6):638–647. https://doi.org/10.1177/1420326X10386669
Wang L, Chen Q (2007) Theoretical and numerical studies of coupling multizone and CFD models for building air distribution simulations. Indoor Air 17(5):348–361. https://doi.org/10.1111/j.1600-0668.2007.00481.x
Wang L, Chen Q (2008a) Applications of a coupled multizone-CFD model to calculate airflow and contaminant dispersion in built environments for emergency management. HVAC&R Res 14(6):925–939. https://doi.org/10.1080/10789669.2008.10391047
Wang L, Chen Q (2008b) Evaluation of some assumptions used in multizone airflow network models. Build Environ 43(10):1671–1677. https://doi.org/10.1016/j.buildenv.2007.10.010
Wang LL, Dols WS, Chen Q (2010b) Using CFD capabilities of CONTAM 3.0 for simulating airflow and contaminant transport in and around buildings. HVAC&R Res 16:749–763
Wang W, Yoneda M (2020) Determination of the optimal penetration factor for evaluating the invasion process of aerosols from a confined source space to an uncontaminated area. Sci Total Environ 740:140113. https://doi.org/10.1016/j.scitotenv.2020.140113
Wang Y, Wu S, Yang Y, Yang X, Song H, Cao Z, Huang Y (2019b) Evaporation and movement of fine droplets in non-uniform temperature and humidity field. Build Environ 150:75–87. https://doi.org/10.1016/j.buildenv.2019.01.003
Watanabe T, Bartrand TA, Weir MH, Omura T, Haas CN (2010) Development of a dose-response model for SARS coronavirus. Risk Anal 30(7):1129–1138. https://doi.org/10.1111/j.1539-6924.2010.01427.x
Weber DJ, Rutala WA, Sickbert-Bennett EE, Kanamori H, Anderson D (2019) Continuous room decontamination technologies. Am J Infect Control 47s:A72–a78. https://doi.org/10.1016/j.ajic.2019.03.016
Weber TP, Stilianakis NI (2008) Inactivation of influenza A viruses in the environment and modes of transmission: a critical review. J Infect 57(5):361–373. https://doi.org/10.1016/j.jinf.2008.08.013
Webster RG, Govorkova EA (2014) Continuing challenges in influenza. Ann N Y Acad Sci 1323(1):115–139. https://doi.org/10.1111/nyas.12462
Wei J, Li Y (2015) Enhanced spread of expiratory droplets by turbulence in a cough jet. Build Environ 93:86–96. https://doi.org/10.1016/j.buildenv.2015.06.018
Wei J, Li Y (2016a) Airborne spread of infectious agents in the indoor environment. Am J Infect Control 44(9, Supplement):S102-S108. https://doi.org/10.1016/j.ajic.2016.06.003
Wei J, Li Y (2016b) Airborne spread of infectious agents in the indoor environment. Am J Infect Control 44(9 Suppl):S102-108. https://doi.org/10.1016/j.ajic.2016.06.003
Weiser JN (2013) The battle with the host over microbial size. Curr Opin Microbiol 16(1):59–62. https://doi.org/10.1016/j.mib.2013.01.001
Weiss P, Murdoch DR (2020) Clinical course and mortality risk of severe COVID-19. Lancet 395(10229):1014–1015. https://doi.org/10.1016/s0140-6736(20)30633-4
Wells WF (1934) On air-borne infection: Study II. Droplets and droplet nuclei. Am J Epidemiol 20(3):611–618. https://doi.org/10.1093/oxfordjournals.aje.a118097
White JF, Bernstein DI (2003) Key pollen allergens in North America. Ann Allergy Asthma Immunol 91(5):425–435. https://doi.org/10.1016/s1081-1206(10)61509-8
White JK, Nielsen JL, Madsen AM (2019) Microbial species and biodiversity in settling dust within and between pig farms. Environ Res 171:558–567. https://doi.org/10.1016/j.envres.2019.01.008
Wiegand I, Hilpert K, Hancock RE (2008) Agar and broth dilution methods to determine the minimal inhibitory concentration (MIC) of antimicrobial substances. Nat Protoc 3(2):163–175. https://doi.org/10.1038/nprot.2007.521
Wilson JM, Platts-Mills TAE (2018) Home environmental interventions for house dust mite. J Allergy Clin Immunol Pract 6(1):1–7. https://doi.org/10.1016/j.jaip.2017.10.003
Wu W, Lin Z (2015) Experimental study of the influence of a moving manikin on temperature profile and carbon dioxide distribution under three air distribution methods. Build Environ 87:142–153. https://doi.org/10.1016/j.buildenv.2015.01.027
Wu X, Fang L, Olesen BW, Zhao J (2014) Air distribution and ventilation effectiveness in a room with floor/ceiling heating and mixing/displacement ventilation. In: Vol. 261 LNEE. Lecture Notes in Electrical Engineering, p 59–67
Wu X, Fang L, Olesen BW, Zhao J, Wang F (2015) Air distribution in a multi-occupant room with mixing or displacement ventilation with or without floor or ceiling heating. Sci Technol Built Environ 21(8):1109–1116. https://doi.org/10.1080/23744731.2015.1090255
Wu X, Gao J, Wang H, Fang L, Olesen BW (2019a) Indoor thermal environment and air distribution in a floor-ceiling heating room with mixing or displacement ventilation. Sci Technol Built Environ 25(3):346–355. https://doi.org/10.1080/23744731.2018.1527138
Wu X, Wang H, Gao J, Wang F (2020) Influence of sensible cooling load on indoor air distribution in an office room with ceiling cooling and mixing ventilation. Indoor Built Environ. https://doi.org/10.1177/1420326X20924819
Wu Y, Niu J, Liu X (2018) Air infiltration induced inter-unit dispersion and infectious risk assessment in a high-rise residential building. Build Simul 11(1):193–202. https://doi.org/10.1007/s12273-017-0388-6
Wu Y, Tung TCW, Niu J (2019b) Experimental analysis of driving forces and impact factors of horizontal inter-unit airborne dispersion in a residential building. Build Environ 151:88–96. https://doi.org/10.1016/j.buildenv.2019.01.028
Xiao S, Li Y, Lei H, Lin C-H, Norris SL, Yang X, Zhao P (2018) Characterizing dynamic transmission of contaminants on a surface touch network. Build Environ 129:107–116. https://doi.org/10.1016/j.buildenv.2017.12.015
Xie X, Li Y, Chwang ATY, Ho PL, Seto WH (2007) How far droplets can move in indoor environments – revisiting the Wells evaporation–falling curve. Indoor Air 17(3):211–225. https://doi.org/10.1111/j.1600-0668.2007.00469.x
Xie X, Li Y, Sun H, Liu L (2009) Exhaled droplets due to talking and coughing. J R Soc Interface 6 Suppl 6(Suppl 6):S703–714.https://doi.org/10.1098/rsif.2009.0388.focus
Yan Y, Li X, Ito K (2020) Numerical investigation of indoor particulate contaminant transport using the Eulerian-Eulerian and Eulerian-Lagrangian two-phase flow models. Exp Comput Multiph Flow 2(1):31–40. https://doi.org/10.1007/s42757-019-0016-z
Yan Y, Li X, Tu J (2019) Thermal effect of human body on cough droplets evaporation and dispersion in an enclosed space. Build Environ 148:96–106. https://doi.org/10.1016/j.buildenv.2018.10.039
Yang C, Yang X, Zhao B (2016) Person to person droplets transmission characteristics in unidirectional ventilated protective isolation room: the impact of initial droplet size. Build Simul 9(5):597–606. https://doi.org/10.1007/s12273-016-0290-7
Yang J, Sekhar SC, Cheong KWD, Raphael B (2015) Performance evaluation of a novel personalized ventilation-personalized exhaust system for airborne infection control. Indoor Air 25(2):176–187. https://doi.org/10.1111/ina.12127
Yang JH (2013) CFD analysis of the inhaled-air quality for the inpatients in a four-bed sickroom. J Asian Archit Build Eng 12(1):109–116. https://doi.org/10.3130/jaabe.12.109
Yang Y, Wang Y, Song B, Fan J, Cao Y (2018) Stability and accuracy of numerical investigation of droplet motion under local ventilation airflow. Build Environ 140:32–42. https://doi.org/10.1016/j.buildenv.2018.05.023
Yasmeen R, Ali Z, Afzal N, Safdar S, Nasir ZA (2020) Characterization of bioaerosols in controlled environment broiler houses at different stages of growth. JAPS J Anim Plant Sci 30(1):81–91. https://doi.org/10.36899/JAPS.2020.1.0010
Ye J, Qian H, Ma J, Zhou R, Zheng X (2020) Using air curtains to reduce short-range infection risk in consulting ward: a numerical investigation. Build Simul. https://doi.org/10.1007/s12273-020-0649-7
Yeoh GH, Tu J (2010) Computational techniques for multiphase flows. Butterworth - Heinemann, Amsterdam
Yezli S, Otter JA (2011) Minimum infective dose of the major human respiratory and enteric viruses transmitted through food and the environment. Food Environ Virol 3(1):1–30. https://doi.org/10.1007/s12560-011-9056-7
Yin D, Gao Q, Zhu H, Li J (2020) Public perception of urban companion animals during the COVID-19 outbreak in China. Health Place 65:102399. https://doi.org/10.1016/j.healthplace.2020.102399
Yin Y, Gupta JK, Zhang X, Liu J, Chen Q (2011) Distributions of respiratory contaminants from a patient with different postures and exhaling modes in a single-bed inpatient room. Build Environ 46(1):75–81. https://doi.org/10.1016/j.buildenv.2010.07.003
Yin Y, Wunderink RG (2018) MERS, SARS and other coronaviruses as causes of pneumonia. Respirology 23(2):130–137. https://doi.org/10.1111/resp.13196
Yin Y, Xu W, Gupta J, Guity A, Marmion P, Manning A, Gulick B, Zhang X, Chen Q (2009) Experimental study on displacement and mixing ventilation systems for a patient ward. HVAC R Res 15(6):1175–1191. https://doi.org/10.1080/10789669.2009.10390885
Yoo JH, Choi NY, Bae YM, Lee JS, Lee SY (2014) Development of a selective agar plate for the detection of Campylobacter spp. in fresh produce. Int J Food Microbiol 189:67–74. https://doi.org/10.1016/j.ijfoodmicro.2014.07.032
Yoo S-J, Ito K (2018) Assessment of transient inhalation exposure using in silico human model integrated with PBPK-CFD hybrid analysis. Sustain Cities Soc 40:317–325. https://doi.org/10.1016/j.scs.2018.04.023
You S, Wan MP (2014) Particle concentration dynamics in the ventilation duct after an artificial release: For countering potential bioterrorist attack. J Hazard Mater 267:183–193. https://doi.org/10.1016/j.jhazmat.2013.12.058
Yu ITS, Li Y, Wong TW, Tam W, Chan AT, Lee JHW, Leung DYC, Ho T (2004) Evidence of airborne transmission of the severe acute respiratory syndrome virus. N Eng J Med 350(17):1731–1739. https://doi.org/10.1056/NEJMoa032867
Zayas G, Chiang MC, Wong E, MacDonald F, Lange CF, Senthilselvan A, King M (2012) Cough aerosol in healthy participants: fundamental knowledge to optimize droplet-spread infectious respiratory disease management. BMC Pulm Med 12(1):11. https://doi.org/10.1186/1471-2466-12-11
Zhai ZJ, Metzger ID (2019) Insights on critical parameters and conditions for personalized ventilation. Sustain Cities Soc 48:101584. https://doi.org/10.1016/j.scs.2019.101584
Zhai ZJ, Zhang Z, Zhang W, Chen QY (2007) Evaluation of various turbulence models in predicting airflow and turbulence in enclosed environments by CFD: Part 1—summary of prevalent turbulence models. HVAC&R Res 13(6):853–870. https://doi.org/10.1080/10789669.2007.10391459
Zhang B, Guo G, Zhu C, Ji Z, Lin C-H (2020a) Transport and trajectory of cough-induced bimodal aerosol in an air-conditioned space. Indoor Built Enviro 30(9):1546–1567. https://doi.org/10.1177/1420326x20941166
Zhang C, Pomianowski M, Heiselberg PK, Yu T (2020b) A review of integrated radiant heating/cooling with ventilation systems- thermal comfort and indoor air quality. Energy Build 223:110094. https://doi.org/10.1016/j.enbuild.2020.110094
Zhang N, Chen W, Chan PT, Yen HL, Tang JW, Li Y (2020c) Close contact behavior in indoor environment and transmission of respiratory infection. Indoor Air 30(4):645–661. https://doi.org/10.1111/ina.12673
Zhang R, Li Y, Zhang AL, Wang Y, Molina MJ (2020d) Identifying airborne transmission as the dominant route for the spread of COVID-19. Proc Natl Acad Sci 117(26):14857. https://doi.org/10.1073/pnas.2009637117
Zhang Y, Feng G, Bi Y, Cai Y, Zhang Z, Cao G (2019) Distribution of droplet aerosols generated by mouth coughing and nose breathing in an air-conditioned room. Sustain Cities Soc 51:101721. https://doi.org/10.1016/j.scs.2019.101721
Zhang Z, Chen Q (2007) Comparison of the Eulerian and Lagrangian methods for predicting particle transport in enclosed spaces. Atmos Environ 41(25):5236–5248. https://doi.org/10.1016/j.atmosenv.2006.05.086
Zhang Z, Zhang W, Zhai ZJ, Chen QY (2007) Evaluation of various turbulence models in predicting airflow and turbulence in enclosed environments by CFD: Part 2—comparison with experimental data from literature. HVAC&R Res 13(6):871–886. https://doi.org/10.1080/10789669.2007.10391460
Zhao B, Zhang Z, Li X (2005) Numerical study of the transport of droplets or particles generated by respiratory system indoors. Build Environ 40(8):1032–1039. https://doi.org/10.1016/j.buildenv.2004.09.018
Zheng XH, Qian H, Liu L (2011) Numerical study on a new personalized ventilation system application in cross infection prevention. J Cent South Univ 42(12):3905–39114307
Zhou Q, Gao N, Qian H (2014) CFD study on the wind-induced transmission of gaseous pollutants between flats in multistory residential buildings. Paper presented at the Indoor Air 2014, Hong Kong, China
Zhou Y, Deng Y, Wu P, Cao S-J (2017) The effects of ventilation and floor heating systems on the dispersion and deposition of fine particles in an enclosed environment. Build Environ 125:192–205. https://doi.org/10.1016/j.buildenv.2017.08.049
Zhu S, Jenkins S, Addo K, Heidarinejad M, Romo SA, Layne A, Ehizibolo J, Dalgo D, Mattise NW, Hong F, Adenaiye OO, Bueno de Mesquita JP, Albert BJ, Washington-Lewis R, German J, Tai S, Youssefi S, Milton DK, Srebric J (2020) Ventilation and laboratory confirmed acute respiratory infection (ARI) rates in college residence halls in College Park, Maryland. Environ Int 137:105537. https://doi.org/10.1016/j.envint.2020.105537
Zhu S, Kato S, Yang J-H (2006) Study on transport characteristics of saliva droplets produced by coughing in a calm indoor environment. Build Environ 41(12):1691–1702. https://doi.org/10.1016/j.buildenv.2005.06.024
Acknowledgements
The authors gratefully acknowledge Mrs. Eirini Kyritsi and Mr. Christos Italos for the visualisation of the enclosed figures, and the anonymous reviewers for their valuable recommendations and efforts.
Funding
Dr. Skoulou received partial support from the European Commission H2020 MSCA programme (DEW-COOL-4-CDC project, Grant agreement ID: 734340).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Argyropoulos, C.D., Skoulou, V., Efthimiou, G. et al. Airborne transmission of biological agents within the indoor built environment: a multidisciplinary review. Air Qual Atmos Health 16, 477–533 (2023). https://doi.org/10.1007/s11869-022-01286-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11869-022-01286-w