Opinion Statement
This perspective underscores the evolution and significance of neoadjuvant therapy in breast cancer, tracing its history and efficacy in improving outcomes. It delves into the correlation between achieving complete response and long-term survival, emphasizing the predictive value of treatment response estimation. Neoadjuvant chemotherapy in HER2-positive early breast cancer, particularly with taxanes and anti-HER2 therapies, emerges as a cornerstone, offering enhanced breast conservation rates and prognostic insights. The focus on individualized care, tailored to treatment response, underscores the need for adaptive strategies. Additionally, the article discusses the ongoing debate surrounding anthracyclines' role and the benefits of dual HER2 blockade. Ultimately, advocating for a personalized approach, guided by treatment response assessment, ensures optimal outcomes in HER2-positive breast cancer management.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neoadjuvant treatment refers to the administration of anticancer therapy before surgery, with the goal of reducing the risk of recurrence in conjunction with surgical intervention. Initially employed for locally advanced and inoperable breast cancers, neoadjuvant chemotherapy (NAC) has experienced significant expansion in recent years, particularly for cases where a conservative approach is not feasible [1]. Despite comprehensive randomized trials and meta-analyses, there is currently no demonstrated improvement in relapse-free or overall survival (OS) with neoadjuvant compared to the same adjuvant regimen [1, 2]. Nonetheless, this strategy presents several advantages.
Tumor regression induced by neoadjuvant chemotherapy enables breast preservation in patients for whom initial conservative surgery was not feasible. Additionally, for patients eligible for initial conservative surgery, preoperative treatment can enhance cosmetic outcome [3]. Neoadjuvant treatment facilitates the assessment of tumor response to standard or new therapies, acting as a research platform for evaluating novel treatments and predictive markers. Furthermore, neoadjuvant treatment provides the opportunity to customize post-neoadjuvant treatment based on pathologic tumor response, allowing for the proposal of escalation strategies (with impacts on survival) or de-escalation in patients with curative intent and potential long-term risks. This article provides a comprehensive overview of the history, advancements, and future perspectives in neoadjuvant treatment for breast cancer, focusing on HER2-positive phenotypic subtype.
Efficacy and Breast Conservation
Evolution of Surgical Practices
Initially proposed as the primary treatment for locally advanced, inoperable tumors [4], primary chemotherapy has proven transformative in managing conditions such as inflammatory breast cancer (BC), traditionally treated with surgery alone with disappointing results [5]. The advent of NAC has significantly improved the prognosis for this clinical entity [6]. Further studies revealed the efficacy of NAC in enhancing the rate of breast conservation for initially operable tumors. In the U.S. study NSABP B18 [7], 1523 patients were randomized between primary surgery followed by 4 cycles of AC and the same chemotherapy administered preoperatively. This strategy increased the rate of breast-conserving surgery from 59.8% to 67.8%, with a comparable local recurrence rate (5.8% vs. 7.9%, p = 0.23). Even for patients eligible for initial conservative treatment, NAC allows for surgery with less breast volume removal, leading to a better cosmetic result [8]. A meta-analysis incorporating data from 4756 patients across 10 major NAC trials confirmed this benefit, reporting a breast conservation rate of 49% to 64.8% [2]. However, this meta-analysis revealed an increased risk of local recurrence with NAC, reaching 21.4% at 15 years compared to 15.9%. It is noteworthy that these results are not fully explained by the two trials allowing omission of surgery in case of a complete clinical response. Despite these findings, caution is warranted in interpreting older data, as they may not consistently reflect the impact of modern chemotherapies, anti-HER2 agents, and recent advancements in imaging, surgery and radiotherapy.
Avoiding Surgery?
Given the increasing efficacy of neoadjuvant medical strategies and the consequential physical and psychological impact of surgery, numerous research teams have explored the prospect of forgoing surgery in instances of clinical complete response (cCR) [9,10,11,12,13,14]. Several retrospective studies have assessed the viability of radiotherapy (RT) as a standalone approach post-NAC, though some exhibit notable biases by comparing RT alone following a cCR (as determined by mammography and breast ultrasound) to surgery followed by RT in cases of residual tumor. [9, 10]
Despite these biases, these studies highlight an elevated risk of locoregional recurrence. In a retrospective British study involving 136 patients with a cCR by ultrasound, comparable survival parameters were reported between groups, but the RT-alone cohort exhibited a higher locoregional recurrence rate at 5 years compared to the surgery-plus-RT group (21% vs. 10%, p = 0.09) [11]. A French series of 100 patients adopting a similar strategy reported analogous findings, with a local recurrence rate of 23% versus 10% at 5 years and 31% versus 17% at 10 years (p = 0.06) [12]. Another retrospective British study investigated the local strategy in 101 patients post-NAC with AC + paclitaxel [13]. In cases of cCR, histologically confirmed by biopsy (16 patients), RT alone was offered. No significant differences were observed in overall or recurrence-free survival (RFS) compared to surgery ± RT, and the locoregional recurrence rates were comparable (12.5% with radiotherapy alone versus 9.5% with surgery).
A non-comparative phase 2 prospective trial conducted at MD Anderson explored the omission of surgery in cases of cCR, confirmed by biopsy. After a 26-month follow-up, none of the 31 patients with TN or HER2-positive BC experienced locoregional recurrence [14]. These small retrospective series and current prospective data do not support considering this strategy as routine, and surgery remains the standard of care. These studies collectively underscore that the principal challenges lie in the duration of follow-up and the assessment of tumor response.
Tumor Response: Assessing and Predicting
Conventional imaging modalities, such as mammography and breast ultrasound, exhibit a modest correlation with pathologic response, demonstrating an accuracy ranging from approximately 30 to 60% [15, 16]. The role of MRI appears to be pivotal in gauging the response to NAC. Numerous publications assert that MRI currently stands as the most effective modality for assessing chemotherapy response, although its predictive value for pathologic response remains suboptimal [17]. Notably, the positive predictive value is significantly lower for hormone receptor-positive tumors (33% versus 61%, p = 0.004) [18]. Breast MRI allows for better staging and patient selection for NAC, especially for invasive lobular carcinomas [19]. MRI helps exclude multifocality, which occurs in up to half of HER2-positive tumors [20]. Early monitoring of systemic therapy efficacy can identify unresponsive tumors, allowing for therapy adjustments. MRI correlates more accurately with pathological tumor size after NAC compared to physical examination, mammography, or ultrasonography [21]. MRI-assessed tumor volume changes have a strong association with RFS [22]. A precise assessment of residual disease before surgery, following NAC, help determine the potential of breast-conserving surgery and guide the surgical strategy [23]. A PET scan may be proposed for staging in locally advanced tumors [24, 25] and proves valuable for monitoring treatment response. Early metabolic response, as evaluated by PET scan, appears to be predictive of pathologic response, particularly in TN and HER2-positive BC [26, 27]. While the widespread adoption of this practice is not yet acknowledged as a definitive predictor of pathological complete response (pCR), it is gradually being incorporated into the framework of prospective trials. [28,29,30,31]
Circulating tumor DNA (ctDNA) in plasma reflects the mutational signatures of the primary tumor and serves as a minimally invasive marker for monitoring response, progression, or recurrence. The detection of ctDNA appears predictive of relapse during surveillance [32]. Its identification during NAC, either early in the course or just before surgery, predicts poor pathologic response and relapse [33,34,35]. Early clearance of ctDNA appears to predict a favorable response to NAC in TNBC only [36]. In cases of residual disease, the presence of ctDNA independently signifies an adverse factor for recurrence (RR > 10). Conversely, even in the presence of residual disease, RFS in patients without detectable ctDNA during NAC is comparable to those achieving pCR [34, 36]. The effectiveness of ctDNA detection in guiding therapeutic interventions is uncertain, and studies are ongoing. The optimal strategy for detecting ctDNA in early-stage BC patients remains undetermined, including the most suitable assays, whether tumor-agnostic or tumor-informed [37]. The HER2DX pCR-score is designed to predict treatment response in HER2-positive early BC, based on a 27-gene expression signature combined with clinical features [38]. While the pCR-score, as a continuous variable, appears to be associated with pCR [39], it may not be sufficiently discriminative to warrant its integration into current clinical practice [40]. At last, increased tumour-infiltrating lymphocytes (TILs) concentration predict response to neoadjuvant chemotherapy in all molecular subtypes [41]. This positive predictive value seems to be more nuanced for HER2-positive, HR-negative tumors undergoing dual anti-HER2 blockade, although the presence of TILs remains a major prognostic factor. [42]
Efficacy and Survival
Data from Major NAC Trials
Designed before the anti-HER2 era, major NAC trials like the U.S. NSABP B181 and B27 trials1 failed to demonstrate a difference in terms of survival. The EBCTCG meta-analysis, incorporating individual data from 4756 patients across 10 trials, also indicates no survival advantage for administering the same chemotherapy before surgery rather than after.2 The distant recurrence rate slightly increased to 38.2% compared to 38%, and overall mortality reached 40.9% compared to 41.2% with neoadjuvant and adjuvant treatments, respectively. The key takeaway from these studies is that pCR emerges as a prognostic factor associated with increased DFS and OS at 5 and 9 years.
Pathologic Response: Definitions
Pathologic response stands as the primary evaluation criterion in most contemporary studies. However, diverse assessments of pathologic response across studies sometimes complicate direct comparisons. The definition of pathologic complete response (pCR) varies both over time and among studies. The most stringent definition is the complete absence of tumor cells in both the breast and lymph nodes (ypT0 ypN0), aligning with Chevallier's class 1 in France. Chevallier's prognostic classification includes three other groups based on the presence of residual in situ lesions (Ch-2), infiltrating residuals with traces of post-therapeutic remodeling (Ch-3), or those without apparent modification (Ch-4) [43]. While complete response has historically been considered even with lymph node residue (ypT0 ypN0/ +), recent evidence has established that lymph node status independently impacts prognosis [44, 45]. Some teams have regarded the presence of in situ residues as indicative of complete response (ypT0/is ypN0) [46,47,48]. Retrospective data from MD Anderson have provided reassurance in this context, demonstrating no discernible difference in survival based on the persistence or absence of in situ lesions [49]. However, a more extensive analysis by the German Breast Group (GBG) has revealed a negative impact of in situ residue on RFS (HR 1.74, p < 0.001), though not on OS (HR 1.41, p = 0.166) [45]. The rate of pCR in NAC has been shown to vary significantly across molecular subtypes, approximated through the immunohistochemical status of ER, PR, and HER2 [49]. Multiple meta-analyses [45, 46, 48] have indicated that pCR rates are lower in luminal A and even B tumors (pCR rates < 20%), but higher in TN and HER2-positive tumors patients treated with chemotherapy and trastuzumab (30 to 70%). It's noteworthy that NAC often alters the immunohistochemical evaluation of surgical specimens [50], particularly impacting prognosis in cases of ER-negative biopsy and ER-positive specimen [51]. The occurrence of a positive HER2 status after NAC is rare when the initial biopsy is negative [52]. However, the incidence of losing HER2-positive status on IHC after NAC is estimated to be between 17 and 43%, [53,54,55] and possibly even higher with dual anti-HER2 blockade [56]. The clinical significance of HER2 loss is unclear, but the prognostic impact appears to be limited. [57]
Pathologic Response and Survival
The association between achieving pCR and its impact on RFS or OS remains a subject of ongoing debate [48, 58,59,60]. The GBG observed that in the HER2-positive population, the attainment of pCR was not correlated with an increase in RFS [45] among patients with estrogen receptor-positive (ER +) tumors, whereas such a correlation was evident in ER-negative tumors. Patricia Cortazar, in collaboration with the FDA, spearheaded the CTNeoBC international working group, which conducted a comprehensive analysis of the relationship between pCR and long-term outcomes by pooling data from various neoadjuvant trials [48]. Their findings indicated that pCR (ypT0/is ypN0) was associated with enhanced RFS and OS across all BC subgroups. These results revealed a 68% reduction in the risk of death in cases of pCR, with decreasing correlation between pCR and survival across populations with TN, HER2-positive, and ER + /HER2- cancers. However, at the trial level, statistical associations between the increase in pCR and the treatment effect on survival parameters were not conclusively demonstrated [48]. This has been confirmed in a recent CTNeoBC meta-analysis of eleven neoadjuvant anti-HER2 therapy trials encompassing 3,980 patients. [46]
To add nuance, the treatment effect on pCR was modest and, therefore, may not have induced statistically significant differences in terms of EFS and OS. Indeed, only the NOAH and GeparQuinto trials showed significant results for pCR. Additionally, the impact of salvage strategies in the absence of pCR could obscure the statistical association between pCR and survival at the trial level. Finally, the use of unadjusted regression models may have led to an underestimation of this statistical association. This may explains why these findings do not currently challenge the FDA's decision [61] to utilize pCR as a surrogate endpoint for the registration of new molecules.
Recent data have been published, encompassing the same 11 neoadjuvant chemotherapy trials that include anti-HER2 therapies. It remains confirmed at the patient level that pCR is a powerful predictive factor for EFS and OS. The objective of this analysis was also to identify risk factors for recurrence with or without pCR. In cases of residual disease, tumor size, lymph node involvement, and negative hormone receptors remain independent prognostic factors for EFS and OS. Even in cases of pCR, tumor size and lymph node involvement continue to be independent prognostic factors for EFS (HR 0.67, p = 0.007 and HR 0.72, p = 0.039, respectively). For OS in cases of pCR, only tumor size remains an independent prognostic factor (cT1-2 vs. cT3-4, HR 0.55; 95% CI: 0.34 to 0.87, p = 0.011). In other words, some patients who achieve a complete response but have additional risk factors are potentially at a higher risk of recurrence and death than those with residual disease but no additional risk factors (cT1-2 cN0 HR +). This information can be instrumental in tailoring post-neoadjuvant strategies at the patient level or in prospective clinical trials, even in cases of pCR [60]. A classification introduced a decade ago [62], known as "Residual Cancer Burden" (RCB), has become commonplace in routine clinical practice. The score is contingent on the size of the residual cancer and the cellularity of the invasive primary cancer, resulting in RCB scores of I for minimal residual tumor, II for moderate residue, and III for extended residue. A publication demonstrated the predictive value of this classification for RFS across all BC subgroups [63]. A recent analysis, utilizing pooled individual data from 5161 patients participating in prospective trials, affirms RCB as an independent prognostic factor in all BC subtypes [64]. An online tool provided by MD Anderson enables the calculation of the RCB score.
Optimization of Neoadjuvant Treatment: HER2-Positive Breast Cancer
Role of Trastuzumab
Similar to its impact in metastatic and adjuvant settings, trastuzumab has significantly revolutionized neoadjuvant treatment for HER2-positive BC. A multitude of phase II studies have explored diverse chemotherapy regimens in combination with trastuzumab, revealing promising pCR rates ranging from 18 to 47%. The initial evaluation of trastuzumab in the neoadjuvant setting occurred in a randomized phase II study at the MD Anderson Cancer Center [65]. In this trial, patients with HER2-positive T2-T3 tumors received a sequential combination of 4 cycles of paclitaxel followed by 4 cycles of FEC, either with or without concurrent trastuzumab. The study was prematurely terminated due to a significantly higher pCR rate in the trastuzumab arm (65% vs. 25%, p = 0.02). Breast conservation rates were comparable (56% in the trastuzumab arm vs. 52% in the NAC-only arm). Published survival data revealed a DFS of 100% at 3 years in the NAC and trastuzumab group compared to 85% in the control arm (p = 0.041) [66]. The GeparQuattro study [67], involving 1509 patients with locally advanced tumors requiring neoadjuvant treatment, included both HER2-positive and HER2-negative cases. HER2-positive patients (n = 445) received a regimen of 4 cycles of EC followed by 4 cycles of docetaxel ± capecitabine, combined with trastuzumab for 1 year. Without a control arm, an indirect comparison was made with HER2-negative patients (n = 1050) receiving the same treatment without trastuzumab. The pCR rate (ypT0/ pN0) was notably higher in HER2-positive tumors receiving NAC with trastuzumab compared to HER2-negative tumors treated with NAC alone (31.7% vs. 15.7%).
In the NOAH study (n = 235), patients with locally advanced or inflammatory tumors featuring HER2 amplification were randomized between a sequential combination of doxorubicin-paclitaxel followed by paclitaxel then CMF, with or without trastuzumab every 3 weeks, initiated from the beginning of chemotherapy and extending for a total duration of 1 year. Trastuzumab doubled the pCR rate (38% vs. 19%, p = 0.001). In this trial, a control cohort of 99 patients with HER2-negative tumors received the same treatment without trastuzumab, resulting in a pCR rate of 16%. Response rates varied based on ER/PR expression, with higher rates in HER2 + /ER- compared to HER2 + /ER + . Breast conservation rates favored the trastuzumab group (23% vs. 13%). With a median follow-up of 5.4 years, event-free survival significantly prolonged in the trastuzumab arm (58% vs. 43%; HR = 0.64, 95% CI = 0.44–0.93; p = 0.016). However, OS differences were not statistically significant (74% vs. 63%). Based on these findings, it is recommended that NAC for HER2-positive BC be combined with trastuzumab, continued into the adjuvant phase for a total duration of 1 year. The optimal choice of cytotoxics, particularly the role of anthracyclines, remains a subject of controversy.
Role of Pertuzumab
Pertuzumab, a monoclonal antibody targeting a distinct HER2 epitope implicated in the heterodimerization of HER family molecules, offers significant synergy with trastuzumab in metastatic HER2-positive BC. It stands as the first-line standard of treatment in metastatic BC, employed alongside chemotherapy and trastuzumab. The efficacy of pertuzumab in the early phase was thoroughly examined in the APHINITY trial [68], with recent reporting of its 6-year results. In this study, 4805 patients underwent randomization between pertuzumab and placebo, in addition to standard adjuvant treatment involving chemotherapy and trastuzumab. OS rates were comparable, at 95% for pertuzumab and 94% for placebo. Pertuzumab demonstrated a notable improvement in RFS, recording 91% in the pertuzumab arm versus 88% in the placebo arm (HR 0.76, 95% CI = 0.64–0.91). This benefit was particularly prominent in the node-positive cohort, as no RFS advantage was observed in the absence of lymph node involvement. Importantly, the benefit of pertuzumab remained consistent across hormonal statuses. Several prospective trials have evaluated the role of pertuzumab and chemotherapy backbones in the neoadjuvant setting, as summarized in Table 1.
The NeoSphere study, a phase II trial, allocated 427 patients across four treatment arms before surgery: trastuzumab-docetaxel, pertuzumab-docetaxel, trastuzumab-pertuzumab-docetaxel, or trastuzumab-pertuzumab without chemotherapy [69]. Post-surgery, patients underwent adjuvant treatment with 3 FEC cycles and trastuzumab, spanning a total duration of one year. Notably, the group receiving docetaxel in conjunction with the double blockade of trastuzumab-pertuzumab exhibited the highest pCR rate (46%), nearly double the rates observed in other arms employing docetaxel with either trastuzumab (29%) or pertuzumab (24%) alone (p = 0.0141). The double blockade without chemotherapy yielded a pCR of 16%. pCR rates were higher in HR- tumors compared to HR + tumors. Cardiac tolerance showed comparable profiles between the two arms and proved relatively satisfactory. An update on the 3-year survival data [78] revealed a DFS rate of 92% in the docetaxel-trastuzumab-pertuzumab group, compared to 85% (HR 0.60, 95% CI = 0.28–1.27) in the docetaxel-trastuzumab group.
The randomized phase II TRYPHAENA study assessed the cardiac tolerance of various trastuzumab and pertuzumab-based regimens in 225 patients with HER2-positive BC (67). Patients received 3 cycles of FEC100 followed by 3 cycles of docetaxel, with trastuzumab-pertuzumab initiated from the beginning of chemotherapy and thus concomitant with anthracyclines (arm A), or only docetaxel (arm B), or 6 cycles of a docetaxel-carboplatin-trastuzumab-pertuzumab combination (without anthracyclines) (arm C). The incidence of LVEF alterations during neoadjuvant treatment remained low and continued to be so in the adjuvant phase with trastuzumab alone or in the follow-up phase after treatment cessation. Considering LVEF alterations below 50% (a decrease of 10 points or more compared to baseline), 11 patients (4 in arm A, 4 in arm B, and 3 in arm C) were affected in the neoadjuvant phase, 15 patients (4 in arm A, 8 in arm B, and 3 in arm C) in the adjuvant phase, and 9 patients (3 in arm A, 4 in arm B, and 2 in arm C) in the follow-up phase. The majority of these decreases were reversible. The main but indirect conclusion is that pertuzumab in each of these three regimens does not appear to alter the rate of cardiac dysfunction. In terms of pCR, there were no significant differences between the various regimens (50%, 45%, and 51% for arms A, B, and C, respectively).
Drawing from these two studies and metastatic data, both the FDA and EMA have granted marketing authorization for pertuzumab's use in the neoadjuvant setting, in conjunction with docetaxel and trastuzumab. The reimbursement decisions regarding pertuzumab in the neoadjuvant context vary from one EU country to another, and the final decisions will depend on their impact on overall survival. In summary, neoadjuvant strategies employing dual HER2 blockade appear to significantly increase pCR rates compared to trastuzumab alone. A meta-analysis, encompassing 6 trials with 1820 HER2-positive BC patients treated in the neoadjuvant setting, assessed dual blockade versus single HER2 blockade [79]. Despite considerable trial heterogeneity, dual blockade demonstrated a notable increase in pCR rates, particularly impactful in HR-negative tumors. It's noteworthy that regimens combining anthracyclines and taxanes (with either single or dual blockade) were associated with higher pCR rates and increased breast conservation (potentially with a slight uptick in cardiac events) compared to regimens without anthracyclines. Another meta-analysis, involving 2247 patients from seven trials evaluating neoadjuvant chemotherapy with one or more anti-HER2 agents, employed an analysis enabling indirect comparisons across different regimens [80]. This analysis affirmed that dual blockade heightened the pCR rate in comparison to single blockade. These findings are corroborated by a recent meta-analysis covering 11 studies and 2836 patients, revealing an odds ratio of 2.8 (95% CI = 2.0–4.1), yet without discernible impacts on survival. [81]
Anthracyclines and Anti-HER2 Combination
The debate on whether to use anthracyclines concomitantly or sequentially with anti-HER2 treatments is ongoing. Traditionally, concomitant administration has been prohibited due to identified cardiac risks in metastatic setup [82]. However, in some neoadjuvant trials, including those mentioned above, trastuzumab was administered from the beginning of chemotherapy and concurrently with anthracyclines, revealing no clinically significant cardiac toxicity. Nevertheless, the limited follow-up and not always comprehensive cardiac monitoring warrant caution [83]. A comparative study explored [84] the concomitant administration of anthracycline and trastuzumab: 282 patients with HER2-positive BC were randomized between sequential chemotherapy with 4 cycles of FEC75 followed by 12 weekly paclitaxel-trastuzumab infusions, versus 12 weekly paclitaxel infusions followed by 4 cycles of FEC75 with concomitant weekly trastuzumab from the beginning of chemotherapy. It's noteworthy that the chemotherapy administration order differed. Comparable pCR rates were observed in both arms: 56% in the sequential arm and 54% in the concomitant arm. At 12 weeks, LVEF decreased in 1 out of 130 patients (0.8%) in the sequential treatment arm and in 4 out of 137 patients in the concomitant treatment arm (2.9%). By week 24, 9/137 patients (6.6%) experienced a decrease in LVEF, compared to 6/130 (4.6%) in the sequential arm. Given the absence of detectable benefits in terms of pCR, it can be concluded that there is no merit in the concomitant administration of trastuzumab and anthracyclines in the neoadjuvant treatment of HER2-positive BC.
In light of the increasing interest in limiting the long-term consequences of curative treatments, several de-escalation studies have explored regimens without anthracyclines. The phase III TRAIN-2 trial randomized 438 patients with HER2-positive BC between a regimen with anthracyclines (3 FEC90 followed by 3 carboplatin-paclitaxel) and a regimen without anthracyclines (9 carboplatin-paclitaxel) [73]. All patients received dual HER2 blockade with trastuzumab-pertuzumab concomitantly. The pCR rate was 67% and 68% in the anthracycline and non-anthracycline groups, respectively (p = 0.95). With a 3-year follow-up, RFS and OS rates were comparable, but the anthracycline regimen was associated with an increased risk of febrile neutropenia, acute leukemia, and cardiac toxicity (7.7% vs. 3.2%, p = 0.04) [85]. The TRYPHAENA trial also investigated dual HER2 blockade in combination with chemotherapy containing or not containing anthracyclines [70]. The pCR rate was high, with or without anthracyclines, ranging from 57 to 66%, and up to 84% in the ER-negative subgroup. These trials, along with the long-term results of the BCIRG006 trial by Slamon et al. in the adjuvant setting with the docetaxel-carboplatin regimen [86], form the basis for the U.S. NCCN recommendations favoring a regimen without anthracyclines but dual HER2 blockade for HER2-positive tumors.
Perspectives
Therapeutic de-escalation has become a prominent concern since the introduction of anti-HER2 therapies and the implementation of adaptive strategies based on the response to neoadjuvant treatment. Initially explored in adjuvant trials, chemotherapy-free regimens were primarily proposed for the frailest patients [87, 88]. It is worth noting that in NeoSphere, the pCR rate with the double-blockade of trastuzumab-pertuzumab alone was 16.8% in a population with 70% N + and 40% initially inoperable.
The phase II WSG-ADAPT trial, involving 134 patients with HER2-positive and ER-negative tumors and 43% with lymph node involvement, randomized patients for 12 weeks of neoadjuvant double-blockade ± neoadjuvant paclitaxel [71]. Remarkably, the pCR rate without chemotherapy reached 34.4%. In the WSG-ADAPT-TP trial, focusing on HER2-positive luminal tumors with ER + , 375 patients were randomized between T-DM1, T-DM1-Endocrine therapy (ET), and trastuzumab-ET [89]. In the chemo-free arm, the pCR rate was 15%. Notably, these ADAPT trials, allowing the omission of chemotherapy in case of pCR, did not seem to compromise RFS, paving the way for entirely chemotherapy-free strategies.
The single-arm phase II de-escalation trial, DAPHNe, reported a remarkable pCR rate of 56.7% with neoadjuvant paclitaxel-trastuzumab-pertuzumab in 98 patients [90]. Going further, the ongoing phase II CompassHER2-pCR trial (NCT04266249) is designed for cT2-3 N0-2 tumors, investigating the neoadjuvant combination of taxanes-trastuzumab-pertuzumab with the aim of sparing carboplatin and anthracyclines. A similar design is employed in the ongoing phase II trial DECRESCENDO (NCT04675827), incorporating an adaptive adjuvant strategy based on the RCB.
Escalation studies are also underway, particularly for patients with residual disease after NAC, following the KATHERINE trial model, which will be discussed later. The CompassHER2-RD trial (NCT04457596) follows the aforementioned CompassHER2 trial, addressing residual disease after double-blockade alone, with randomization between T-DM1-placebo and T-DM1-tucatinib. The phase III DESTINY-Breast05 trial (NCT04622319) randomizes T-DM1 and trastuzumab-deruxtecan in the adjuvant setting, in the absence of pCR. In case of positivity, it will be necessary to discuss in each case the magnitude of benefit, considering the differences in toxicity between these two antibody–drug conjugates. Trastuzumab-deruxtecan is also being studied as monotherapy in the neoadjuvant setting in the DESTINY-Breast11 trial (NCT05113251).
Immunotherapy with immune checkpoint inhibitors (ICI) is also under investigation in the HER2-positive population. This approach is based on the rationale of potentiating chemotherapy by inducing immunogenicity and anti-HER2 action through antibody-dependent cell-mediated cytotoxicity. Immunotherapy is integrated into neoadjuvant strategies, as seen in the neoHIP phase II trial (NCT03747120), where pembrolizumab is randomized alongside paclitaxel and anti-HER2 therapies. Similarly, the phase III IMpassion050 trial (NCT03726879) tests atezolizumab in combination with chemotherapy and dual blockade. Although the initial results are disappointing and do not show a benefit in pCR [91], more follow-up is needed. Immunotherapy is also explored in a post-neoadjuvant strategy, as evidenced by the phase III ASTEFANIA trial (NCT04873362), randomizing T-DM1 with or without atezolizumab in cases of residual disease.
Recovery Strategies
Trastuzumab-Emtansine
Trastuzumab-emtansine (T-DM1), an antibody–drug conjugate amalgamating trastuzumab with a potent microtubule-targeted cytotoxic agent via a linker, has demonstrated efficacy in HER2-positive metastatic BC resistant to trastuzumab. In the neoadjuvant context, T-DM1 has exhibited favorable cardiac tolerance [92], but its superiority in terms of toxicity or efficacy remains unproven. Conversely, there is a noted risk of progression during neoadjuvant chemotherapy [72]. However, the assessment of neoadjuvant treatment response has facilitated the tailoring of adjuvant treatment for HER2-positive tumors. The KATHERINE trial randomized 1486 patients with stage II HER2-positive BC (tumor size > 2 cm), with or without nodal involvement, who did not achieve pCR after neoadjuvant treatment, including trastuzumab (and pertuzumab for 18% of patients). Participants were randomized between continuing trastuzumab or escalating to T-DM1. Results revealed a 3-year locoregional or distant RFS of 88.3% in the T-DM1 arm versus 77% in the trastuzumab arm (HR 0.50, 95% CI = 0.39–0.64; p < 0.001). Notably, there was no significant deterioration in quality of life, as assessed by patient-reported outcomes. After a median follow-up of 8.4 years, T-DM1 significantly improved OS, reducing the risk of death by 34% compared to trastuzumab.93 This study has influenced clinical practices by reinforcing the value of a neoadjuvant strategy for HER2-positive tumors larger than 2 cm, with the objective of proposing an adaptive strategy based on tumor response.
Conclusion
Neoadjuvant chemotherapy offers the prospect of enhancing breast conservation rates, albeit with an increased risk of local recurrence. The primary challenge in adopting a surgery-avoidance strategy lies in the precise evaluation of tumor response. Despite lacking direct and objective evidence demonstrating improved survival with neoadjuvant over adjuvant approaches, it is crucial to note that statistical power in most neoadjuvant trials is geared towards pathological complete response (pCR) rather than long-term survival.
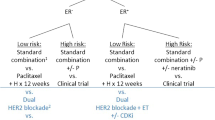
Nevertheless, neoadjuvant chemotherapy remains a standard therapeutic approach, particularly in HER2-positive and triple-negative breast cancers. At an individual level, achieving or not achieving pCR serves as a significant prognostic indicator, especially in triple-negative breast cancers. This informs the development of adaptive strategies based on response, allowing therapeutic escalation in cases of residual disease with potential impacts on survival or therapeutic de-escalation in selected patients. Early evaluation of response, whether metabolic or histo-molecular, facilitates timely therapeutic adjustments in patients at high risk of recurrence due to incomplete pathologic response.
For HER2-positive breast cancers, neoadjuvant chemotherapy incorporating taxanes and trastuzumab, with or without prior anthracyclines, is recommended. Concomitant administration of anthracyclines and anti-HER2 agents is not favored. Dual blockade with trastuzumab and pertuzumab enhances pCR, but its impact on survival is yet to be fully demonstrated, making it more relevant in cases of nodal involvement or when sparing anthracyclines is desired. Salvage treatment with trastuzumab-emtansine for residual disease has proven effective in improving recurrence-free survival.
Disclosure
HB, ME and TP had no conflict of interest associated with this publication.
Key References
-
Kuerer HM, Smith BD, Krishnamurthy S, et al. Eliminating breast surgery for invasive breast cancer in exceptional responders to neoadjuvant systemic therapy: a multicentre, single-arm, phase 2 trial. Lancet Oncol. 2022;23(12):1517-1524. doi:10.1016/S1470-2045(22)00613-1
-
In selected patients with triple-negative or HER2-positive breast cancer showing a complete response to neoadjuvant therapy, omitting surgery for radiotherapy alone, guided by image-assisted biopsy, yields promising low recurrence rates, suggesting feasibility for further study.
-
-
Squifflet P, Saad ED, Loibl S, et al. Re-Evaluation of Pathologic Complete Response as a Surrogate for Event-Free and Overall Survival in Human Epidermal Growth Factor Receptor 2-Positive, Early Breast Cancer Treated With Neoadjuvant Therapy Including Anti-Human Epidermal Growth Factor Receptor 2 Therapy. J Clin Oncol. 2023;41(16):2988-2997. doi:10.1200/JCO.22.02363
-
In HER2-positive breast cancer trials, individual patients achieving a pathologic complete response (pCR) show better event-free survival (EFS) and overall survival (OS), but this correlation is weak at the trial level.
-
-
van Mackelenbergh MT, Loibl S, Untch M, et al. Pathologic Complete Response and Individual Patient Prognosis After Neoadjuvant Chemotherapy Plus Anti-Human Epidermal Growth Factor Receptor 2 Therapy of Human Epidermal Growth Factor Receptor 2-Positive Early Breast Cancer. J Clin Oncol. 2023;41(16):2998-3008. doi:10.1200/JCO.22.02241
-
In early breast cancer, achieving pathologic complete response (pCR) after neoadjuvant therapy improves survival, especially in HER2-positive disease. Tumor size and nodal status remain key prognostic factors regardless of pCR status, underscoring their ongoing significance in outcome prediction.
-
-
Yau C, Osdoit M, van der Noordaa M, et al. Residual cancer burden after neoadjuvant chemotherapy and long-term survival outcomes in breast cancer: a multicentre pooled analysis of 5161 patients. Lancet Oncol. 2022;23(1):149-160. doi:10.1016/S1470-2045(21)00589-1
-
Residual cancer burden (RCB) after neoadjuvant chemotherapy independently predicts event-free survival across various breast cancer subtypes, indicating its potential as a standard pathology reporting measure post-therapy.
-
-
Waks AG, Desai NV, Li T, et al. A prospective trial of treatment de-escalation following neoadjuvant paclitaxel/trastuzumab/pertuzumab in HER2-positive breast cancer. NPJ Breast Cancer. 2022;8(1):63. doi:10.1038/s41523-022-00429-7
-
In HER2-positive breast cancer patients achieving pathologic complete response (pCR) after neoadjuvant paclitaxel/HP regimen, adherence to de-escalated adjuvant antibody-only therapy (HP) was high (98.2%), indicating feasibility and patient/provider acceptability. This approach is under further investigation for long-term efficacy in ongoing trials.
-
Data Availability
No datasets were generated or analysed during the current study.
Abbreviations
- AC:
-
Doxorubicine + Cyclophosphamide
- BC:
-
Breast Cancer
- cCR:
-
Clinical Complete Response
- CMF:
-
Cyclophosphamide, methotrexate and 5-fluorouracil
- ctDNA:
-
Circulating tumor Deoxyribonucleic Acid
- CTNeoBC:
-
Collaborative Trials in Neoadjuvant Breast Cancer
- EBCTCG:
-
Early Breast Cancer Trialists' Collaborative Group
- EC:
-
Epirubicin and Cyclophosphamide
- EMA:
-
European Medicines Agency
- ER:
-
Estrogen Receptors
- ET:
-
Endocrine therapy
- FEC:
-
5-Fluorouracil, epirubicin and cyclophosphamide
- FDA:
-
Food and Drug Administration
- GBG:
-
German Breast Group
- HR:
-
Hormone Receptors
- ICI:
-
Immune Checkpoints Inhibitors
- MRI:
-
Magnetic Resonance Imaging
- NAC:
-
Neoadjuvant chemotherapy
- NCCN:
-
National Comprehensive Cancer Network
- NSABP:
-
National Surgical Adjuvant Breast and Bowel Project
- OS:
-
Overall survival
- pCR:
-
Pathological Complete Response
- RCB:
-
Residual Cancer Burden
- RFS:
-
Recurrence-free survival
- RR:
-
Relative risk
- RS:
-
Recurrence Score
- RT:
-
Radiotherapy
- T-DM1:
-
Trastuzumab-emtansine
- TN:
-
Triple-negative
References and Recommended Reading
Rastogi P, Anderson SJ, Bear HD, et al. Preoperative chemotherapy: updates of national surgical adjuvant breast and bowel project protocols B-18 and B-27. J Clin Oncol. 2008;26(5):778–85. https://doi.org/10.1200/JCO.2007.15.0235.
Early Breast Cancer Trialists’ Collaborative Group (EBCTCG). Long-term outcomes for neoadjuvant versus adjuvant chemotherapy in early breast cancer: meta-analysis of individual patient data from ten randomised trials. Lancet Oncol. 2018;19(1):27–39. https://doi.org/10.1016/S1470-2045(17)30777-5.
Ademuyiwa FO, Ellis MJ, Ma CX. Neoadjuvant therapy in operable breast cancer: application to triple negative breast cancer. J Oncol. 2013;2013:219869. https://doi.org/10.1155/2013/219869.
Rubens RD, Sexton S, Tong D, Winter PJ, Knight RK, Hayward JL. Combined chemotherapy and radiotherapy for locally advanced breast cancer. Eur J Cancer (1965). 1980;16(3):351–6. https://doi.org/10.1016/0014-2964(80)90352-7.
Taylor GW, Meltzer A. “Inflammatory Carcinoma” of the breast. Am J Cancer. 1938;33(1):33–49. https://doi.org/10.1158/ajc.1938.33.
Jaiyesimi IA, Buzdar AU, Hortobagyi G. Inflammatory breast cancer: a review. JCO. 1992;10(6):1014–24. https://doi.org/10.1200/JCO.1992.10.6.1014.
Fisher B, Bryant J, Wolmark N, et al. Effect of preoperative chemotherapy on the outcome of women with operable breast cancer. J Clin Oncol. 2023;41(10):1795–808. https://doi.org/10.1200/JCO.22.02571.
Boughey JC, Peintinger F, Meric-Bernstam F, et al. Impact of preoperative versus postoperative chemotherapy on the extent and number of surgical procedures in patients treated in randomized clinical trials for breast cancer. Ann Surg. 2006;244(3):464–70. https://doi.org/10.1097/01.sla.0000234897.38950.5c.
Scholl SM, Fourquet A, Asselain B, et al. Neoadjuvant versus adjuvant chemotherapy in premenopausal patients with tumours considered too large for breast conserving surgery: preliminary results of a randomised trial: S6. Eur J Cancer. 1994;30A(5):645–52. https://doi.org/10.1016/0959-8049(94)90537-1.
Mauriac L, MacGrogan G, Avril A, et al. Neoadjuvant chemotherapy for operable breast carcinoma larger than 3 cm: a unicentre randomized trial with a 124-month median follow-up. Institut bergonié bordeaux groupe sein (IBBGS). Ann Oncol. 1999;10(1):47–52. https://doi.org/10.1023/a:1008337009350.
Ring A, Webb A, Ashley S, et al. Is surgery necessary after complete clinical remission following neoadjuvant chemotherapy for early breast cancer? J Clin Oncol. 2003;21(24):4540–5. https://doi.org/10.1200/JCO.2003.05.208.
Daveau C, Savignoni A, Abrous-Anane S, et al. Is radiotherapy an option for early breast cancers with complete clinical response after neoadjuvant chemotherapy? Int J Radiat Oncol Biol Phys. 2011;79(5):1452–9. https://doi.org/10.1016/j.ijrobp.2010.01.003.
Clouth B, Chandrasekharan S, Inwang R, Smith S, Davidson N, Sauven P. The surgical management of patients who achieve a complete pathological response after primary chemotherapy for locally advanced breast cancer. Eur J Surg Oncol. 2007;33(8):961–6. https://doi.org/10.1016/j.ejso.2006.12.006.
Kuerer HM, Smith BD, Krishnamurthy S, et al. Eliminating breast surgery for invasive breast cancer in exceptional responders to neoadjuvant systemic therapy: a multicentre, single-arm, phase 2 trial. Lancet Oncol. 2022;23(12):1517–24. https://doi.org/10.1016/S1470-2045(22)00613-1.
Baumgartner A, Tausch C, Hosch S, et al. Ultrasound-based prediction of pathologic response to neoadjuvant chemotherapy in breast cancer patients. Breast. 2018;39:19–23. https://doi.org/10.1016/j.breast.2018.02.028.
Zhang K, Li J, Zhu Q, Chang C. Prediction of pathologic complete response by ultrasonography and magnetic resonance imaging after neoadjuvant chemotherapy in patients with breast cancer. Cancer Manag Res. 2020;12:2603–12. https://doi.org/10.2147/CMAR.S247279.
Gu YL, Pan SM, Ren J, Yang ZX, Jiang GQ. Role of magnetic resonance imaging in detection of pathologic complete remission in breast cancer patients treated with neoadjuvant chemotherapy: A Meta-analysis. Clin Breast Cancer. 2017;17(4):245–55. https://doi.org/10.1016/j.clbc.2016.12.010.
Gampenrieder SP, Peer A, Weismann C, et al. Radiologic complete response (rCR) in contrast-enhanced magnetic resonance imaging (CE-MRI) after neoadjuvant chemotherapy for early breast cancer predicts recurrence-free survival but not pathologic complete response (pCR). Breast Cancer Res. 2019;21(1):19. https://doi.org/10.1186/s13058-018-1091-y.
Le-Petross HT, Lim B. Role of MR imaging in neoadjuvant therapy monitoring. Magn Reson Imaging Clin N Am. 2018;26(2):207–20. https://doi.org/10.1016/j.mric.2017.12.011.
Loo CE, Straver ME, Rodenhuis S, et al. Magnetic resonance imaging response monitoring of breast cancer during neoadjuvant chemotherapy: relevance of breast cancer subtype. J Clin Oncol. 2011;29(6):660–6. https://doi.org/10.1200/JCO.2010.31.1258.
Scheel JR, Kim E, Partridge SC, et al. MRI, clinical examination, and mammography for preoperative assessment of residual disease and pathologic complete response after neoadjuvant chemotherapy for breast cancer: ACRIN 6657 trial. AJR Am J Roentgenol. 2018;210(6):1376–85. https://doi.org/10.2214/AJR.17.18323.
Hylton NM, Gatsonis CA, Rosen MA, et al. Neoadjuvant chemotherapy for breast cancer: functional tumor volume by MR imaging predicts recurrence-free survival-results from the ACRIN 6657/CALGB 150007 I-SPY 1 TRIAL. Radiology. 2016;279(1):44–55. https://doi.org/10.1148/radiol.2015150013.
Mann RM, Cho N, Moy L. Breast MRI: State of the art. Radiology. 2019;292(3):520–36. https://doi.org/10.1148/radiol.2019182947.
Groheux D, Cochet A, Humbert O, Alberini JL, Hindié E, Mankoff D. 18F-FDG PET/CT for staging and restaging of breast cancer. J Nucl Med. 2016;57(Suppl 1):17S-26S. https://doi.org/10.2967/jnumed.115.157859.
Groheux D. FDG-PET/CT for systemic staging of patients with newly diagnosed breast cancer. Eur J Nucl Med Mol Imaging. 2017;44(9):1417–9. https://doi.org/10.1007/s00259-017-3731-3.
Groheux D, Biard L, Giacchetti S, et al. 18F-FDG PET/CT for the early evaluation of response to neoadjuvant treatment in triple-negative breast cancer: influence of the chemotherapy regimen. J Nucl Med. 2016;57(4):536–43. https://doi.org/10.2967/jnumed.115.163907.
Groheux D, Mankoff D, Espié M, Hindié E. 18F-FDG PET/CT in the early prediction of pathological response in aggressive subtypes of breast cancer: review of the literature and recommendations for use in clinical trials. Eur J Nucl Med Mol Imaging. 2016;43(5):983–93. https://doi.org/10.1007/s00259-015-3295-z.
Coudert B, Pierga JY, Mouret-Reynier MA, et al. Use of [(18)F]-FDG PET to predict response to neoadjuvant trastuzumab and docetaxel in patients with HER2-positive breast cancer, and addition of bevacizumab to neoadjuvant trastuzumab and docetaxel in [(18)F]-FDG PET-predicted non-responders (AVATAXHER): an open-label, randomised phase 2 trial. Lancet Oncol. 2014;15(13):1493–502. https://doi.org/10.1016/S1470-2045(14)70475-9.
Pérez-García JM, Gebhart G, Ruiz Borrego M, et al. Chemotherapy de-escalation using an 18F-FDG-PET-based pathological response-adapted strategy in patients with HER2-positive early breast cancer (PHERGain): a multicentre, randomised, open-label, non-comparative, phase 2 trial. Lancet Oncol. 2021;22(6):858–71. https://doi.org/10.1016/S1470-2045(21)00122-4.
Lin NU, Guo H, Yap JT, et al. Phase ii study of lapatinib in combination with trastuzumab in patients with human epidermal growth factor receptor 2-positive metastatic breast cancer: clinical outcomes and predictive value of early [18F]fluorodeoxyglucose positron emission tomography imaging (TBCRC 003). J Clin Oncol. 2015;33(24):2623–31. https://doi.org/10.1200/JCO.2014.60.0353.
Gebhart G, Gámez C, Holmes E, et al. 18F-FDG PET/CT for early prediction of response to neoadjuvant lapatinib, trastuzumab, and their combination in HER2-positive breast cancer: results from Neo-ALTTO. J Nucl Med. 2013;54(11):1862–8. https://doi.org/10.2967/jnumed.112.119271.
Coombes RC, Page K, Salari R, et al. Personalized detection of circulating tumor DNA antedates breast cancer metastatic recurrence. Clin Cancer Res. 2019;25(14):4255–63. https://doi.org/10.1158/1078-0432.CCR-18-3663.
Moss J, Zick A, Grinshpun A, et al. Circulating breast-derived DNA allows universal detection and monitoring of localized breast cancer. Ann Oncol. 2020;31(3):395–403. https://doi.org/10.1016/j.annonc.2019.11.014.
Magbanua MJM, Swigart LB, Wu HT, et al. Circulating tumor DNA in neoadjuvant-treated breast cancer reflects response and survival. Ann Oncol. 2021;32(2):229–39. https://doi.org/10.1016/j.annonc.2020.11.007.
Radovich M, Jiang G, Hancock BA, et al. Association of circulating tumor dna and circulating tumor cells after neoadjuvant chemotherapy with disease recurrence in patients with triple-negative breast cancer: preplanned secondary analysis of the BRE12-158 randomized clinical trial. JAMA Oncol. 2020;6(9):1410–5. https://doi.org/10.1001/jamaoncol.2020.2295.
Magbanua MJM, Brown Swigart L, Ahmed Z, et al. Clinical significance and biology of circulating tumor DNA in high-risk early-stage HER2-negative breast cancer receiving neoadjuvant chemotherapy. Cancer Cell. 2023;41(6):1091-1102.e4. https://doi.org/10.1016/j.ccell.2023.04.008.
Pascual J, Attard G, Bidard FC, et al. ESMO recommendations on the use of circulating tumour DNA assays for patients with cancer: a report from the ESMO precision medicine working group. Ann Oncol. 2022;33(8):750–68. https://doi.org/10.1016/j.annonc.2022.05.520.
Prat A, Guarneri V, Pascual T, et al. Development and validation of the new HER2DX assay for predicting pathological response and survival outcome in early-stage HER2-positive breast cancer. EBioMedicine. 2022;75:103801. https://doi.org/10.1016/j.ebiom.2021.103801.
Llombart-Cussac A, Pérez-García J, Brasó-Maristany F, et al. HER2DX genomic assay in HER2-positive early breast cancer treated with trastuzumab and pertuzumab: a correlative analysis from PHERGain Phase II trial. Clin Cancer Res. Published online July 12, 2024. https://doi.org/10.1158/1078-0432.CCR-24-0464.
Villacampa G, Tung NM, Pernas S, et al. Association of HER2DX with pathological complete response and survival outcomes in HER2-positive breast cancer. Ann Oncol. 2023;34(9):783–95. https://doi.org/10.1016/j.annonc.2023.05.012.
Denkert C, von Minckwitz G, Darb-Esfahani S, et al. Tumour-infiltrating lymphocytes and prognosis in different subtypes of breast cancer: a pooled analysis of 3771 patients treated with neoadjuvant therapy. Lancet Oncol. 2018;19(1):40–50. https://doi.org/10.1016/S1470-2045(17)30904-X.
Liefaard MC, Van Der Voort A, Van Seijen M, et al. Tumor-infiltrating lymphocytes in HER2-positive breast cancer treated with neoadjuvant chemotherapy and dual HER2-blockade. npj Breast Cancer. 2024;10(1):29. https://doi.org/10.1038/s41523-024-00636-4.
Chevallier B, Roche H, Olivier JP, Chollet P, Hurteloup P. Inflammatory breast cancer. Pilot study of intensive induction chemotherapy (FEC-HD) results in a high histologic response rate. Am J Clin Oncol. 1993;16(3):223–8.
Rouzier R, Extra JM, Klijanienko J, et al. Incidence and prognostic significance of complete axillary downstaging after primary chemotherapy in breast cancer patients with T1 to T3 tumors and cytologically proven axillary metastatic lymph nodes. J Clin Oncol. 2002;20(5):1304–10. https://doi.org/10.1200/JCO.2002.20.5.1304.
von Minckwitz G, Untch M, Blohmer JU, et al. Definition and impact of pathologic complete response on prognosis after neoadjuvant chemotherapy in various intrinsic breast cancer subtypes. J Clin Oncol. 2012;30(15):1796–804. https://doi.org/10.1200/JCO.2011.38.8595.
Squifflet P, Saad ED, Loibl S, et al. Re-evaluation of pathologic complete response as a surrogate for event-free and overall survival in human epidermal growth factor receptor 2-positive, early breast cancer treated with neoadjuvant therapy including anti-human epidermal growth factor receptor 2 therapy. J Clin Oncol. 2023;41(16):2988–97. https://doi.org/10.1200/JCO.22.02363.
Baselga J, Bradbury I, Eidtmann H, et al. Lapatinib with trastuzumab for HER2-positive early breast cancer (NeoALTTO): a randomised, open-label, multicentre, phase 3 trial. Lancet. 2012;379(9816):633–40. https://doi.org/10.1016/S0140-6736(11)61847-3.
Cortazar P, Zhang L, Untch M, et al. Pathological complete response and long-term clinical benefit in breast cancer: the CTNeoBC pooled analysis. Lancet. 2014;384(9938):164–72. https://doi.org/10.1016/S0140-6736(13)62422-8.
Mazouni C, Peintinger F, Wan-Kau S, et al. Residual ductal carcinoma in situ in patients with complete eradication of invasive breast cancer after neoadjuvant chemotherapy does not adversely affect patient outcome. J Clin Oncol. 2007;25(19):2650–5. https://doi.org/10.1200/JCO.2006.08.2271.
Valent A, Penault-Llorca F, Cayre A, Kroemer G. Change in HER2 (ERBB2) gene status after taxane-based chemotherapy for breast cancer: polyploidization can lead to diagnostic pitfalls with potential impact for clinical management. Cancer Genet. 2013;206(1–2):37–41. https://doi.org/10.1016/j.cancergen.2012.12.001.
Tacca O, Penault-Llorca F, Abrial C, et al. Changes in and prognostic value of hormone receptor status in a series of operable breast cancer patients treated with neoadjuvant chemotherapy. Oncologist. 2007;12(6):636–43. https://doi.org/10.1634/theoncologist.12-6-636.
Kang S, Lee SH, Lee HJ, et al. Prognostic implications of HER2 changes after neoadjuvant chemotherapy in patients with HER2-zero and HER2-low breast cancer. Eur J Cancer. 2023;191:112956. https://doi.org/10.1016/j.ejca.2023.112956.
Bo J, Yu B, Bi R, et al. Conversion of ER and HER2 status after neoadjuvant therapy in chinese breast cancer patients. Clin Breast Cancer. 2023;23(4):436–46. https://doi.org/10.1016/j.clbc.2023.03.002.
Niikura N, Tomotaki A, Miyata H, et al. Changes in tumor expression of HER2 and hormone receptors status after neoadjuvant chemotherapy in 21 755 patients from the Japanese breast cancer registry. Ann Oncol. 2016;27(3):480–7. https://doi.org/10.1093/annonc/mdv611.
Van De Ven S, Smit VTHBM, Dekker TJA, Nortier JWR, Kroep JR. Discordances in ER, PR and HER2 receptors after neoadjuvant chemotherapy in breast cancer. Cancer Treatment Rev. Published online December 21, 2010:S0305737210002070.https://doi.org/10.1016/j.ctrv.2010.11.006.
Ferraro E, Razavi P, Chandarlapaty S, et al. Change in HER2 status after neoadjuvant chemotherapy (NAC) with trastuzumab and pertuzumab (HP) in patients with HER2-positive early-stage breast cancer. JCO. 2021;39(15_suppl):e12614–e12614. https://doi.org/10.1200/JCO.2021.39.15_suppl.e12614.
Yoshida A, Hayashi N, Suzuki K, Takimoto M, Nakamura S, Yamauchi H. Change in HER2 status after neoadjuvant chemotherapy and the prognostic impact in patients with primary breast cancer. J Surg Oncol. 2017;116(8):1021–8. https://doi.org/10.1002/jso.24762.
Berruti A, Amoroso V, Gallo F, et al. Pathologic complete response as a potential surrogate for the clinical outcome in patients with breast cancer after neoadjuvant therapy: a meta-regression of 29 randomized prospective studies. J Clin Oncol. 2014;32(34):3883–91. https://doi.org/10.1200/JCO.2014.55.2836.
Broglio KR, Quintana M, Foster M, et al. Association of pathologic complete response to neoadjuvant therapy in HER2-positive breast cancer with long-term outcomes: a meta-analysis. JAMA Oncol. 2016;2(6):751–60. https://doi.org/10.1001/jamaoncol.2015.6113.
van Mackelenbergh MT, Loibl S, Untch M, et al. Pathologic complete response and individual patient prognosis after neoadjuvant chemotherapy plus anti-human epidermal growth factor receptor 2 therapy of human epidermal growth factor receptor 2-positive early breast cancer. J Clin Oncol. 2023;41(16):2998–3008. https://doi.org/10.1200/JCO.22.02241.
Cortazar P, Kluetz PG. Neoadjuvant breast cancer therapy and drug development. Clin Adv Hematol Oncol. 2015;13(11):755–61.
Symmans WF, Peintinger F, Hatzis C, et al. Measurement of residual breast cancer burden to predict survival after neoadjuvant chemotherapy. J Clin Oncol. 2007;25(28):4414–22. https://doi.org/10.1200/JCO.2007.10.6823.
Symmans WF, Wei C, Gould R, et al. Long-term prognostic risk after neoadjuvant chemotherapy associated with residual cancer burden and breast cancer subtype. J Clin Oncol. 2017;35(10):1049–60. https://doi.org/10.1200/JCO.2015.63.1010.
Yau C, Osdoit M, van der Noordaa M, et al. Residual cancer burden after neoadjuvant chemotherapy and long-term survival outcomes in breast cancer: a multicentre pooled analysis of 5161 patients. Lancet Oncol. 2022;23(1):149–60. https://doi.org/10.1016/S1470-2045(21)00589-1.
Buzdar AU, Ibrahim NK, Francis D, et al. Significantly higher pathologic complete remission rate after neoadjuvant therapy with trastuzumab, paclitaxel, and epirubicin chemotherapy: results of a randomized trial in human epidermal growth factor receptor 2-positive operable breast cancer. J Clin Oncol. 2005;23(16):3676–85. https://doi.org/10.1200/JCO.2005.07.032.
Buzdar AU, Valero V, Ibrahim NK, et al. Neoadjuvant therapy with paclitaxel followed by 5-fluorouracil, epirubicin, and cyclophosphamide chemotherapy and concurrent trastuzumab in human epidermal growth factor receptor 2-positive operable breast cancer: an update of the initial randomized study population and data of additional patients treated with the same regimen. Clin Cancer Res. 2007;13(1):228–33. https://doi.org/10.1158/1078-0432.CCR-06-1345.
Untch M, Rezai M, Loibl S, et al. Neoadjuvant treatment with trastuzumab in HER2-positive breast cancer: results from the GeparQuattro study. J Clin Oncol. 2010;28(12):2024–31. https://doi.org/10.1200/JCO.2009.23.8451.
Piccart M, Procter M, Fumagalli D, et al. Adjuvant pertuzumab and trastuzumab in early HER2-positive breast cancer in the APHINITY trial: 6 years’ follow-up. J Clin Oncol. 2021;39(13):1448–57. https://doi.org/10.1200/JCO.20.01204.
Gianni L, Pienkowski T, Im YH, et al. Efficacy and safety of neoadjuvant pertuzumab and trastuzumab in women with locally advanced, inflammatory, or early HER2-positive breast cancer (NeoSphere): a randomised multicentre, open-label, phase 2 trial. Lancet Oncol. 2012;13(1):25–32. https://doi.org/10.1016/S1470-2045(11)70336-9.
Schneeweiss A, Chia S, Hickish T, et al. Pertuzumab plus trastuzumab in combination with standard neoadjuvant anthracycline-containing and anthracycline-free chemotherapy regimens in patients with HER2-positive early breast cancer: a randomized phase II cardiac safety study (TRYPHAENA). Ann Oncol. 2013;24(9):2278–84. https://doi.org/10.1093/annonc/mdt182.
Nitz U, Gluz O, Graeser M, et al. De-escalated neoadjuvant pertuzumab plus trastuzumab therapy with or without weekly paclitaxel in HER2-positive, hormone receptor-negative, early breast cancer (WSG-ADAPT-HER2+/HR-): survival outcomes from a multicentre, open-label, randomised, phase 2 trial. Lancet Oncol. 2022;23(5):625–35. https://doi.org/10.1016/S1470-2045(22)00159-0.
Hurvitz SA, Martin M, Symmans WF, et al. Neoadjuvant trastuzumab, pertuzumab, and chemotherapy versus trastuzumab emtansine plus pertuzumab in patients with HER2-positive breast cancer (KRISTINE): a randomised, open-label, multicentre, phase 3 trial. Lancet Oncol. 2018;19(1):115–26. https://doi.org/10.1016/S1470-2045(17)30716-7.
van Ramshorst MS, van der Voort A, van Werkhoven ED, et al. Neoadjuvant chemotherapy with or without anthracyclines in the presence of dual HER2 blockade for HER2-positive breast cancer (TRAIN-2): a multicentre, open-label, randomised, phase 3 trial. Lancet Oncol. 2018;19(12):1630–40. https://doi.org/10.1016/S1470-2045(18)30570-9.
Swain SM, Ewer MS, Viale G, et al. Pertuzumab, trastuzumab, and standard anthracycline- and taxane-based chemotherapy for the neoadjuvant treatment of patients with HER2-positive localized breast cancer (BERENICE): a phase II, open-label, multicenter, multinational cardiac safety study. Ann Oncol. 2018;29(3):646–53. https://doi.org/10.1093/annonc/mdx773.
Shao Z, Pang D, Yang H, et al. Efficacy, safety, and tolerability of pertuzumab, trastuzumab, and docetaxel for patients with early or locally advanced ERBB2-positive breast cancer in asia: the PEONY Phase 3 randomized clinical trial. JAMA Oncol. 2020;6(3):e193692. https://doi.org/10.1001/jamaoncol.2019.3692.
Clark AS, Yau C, Wolf DM, et al. Neoadjuvant T-DM1/pertuzumab and paclitaxel/trastuzumab/pertuzumab for HER2+ breast cancer in the adaptively randomized I-SPY2 trial. Nat Commun. 2021;12(1):6428. https://doi.org/10.1038/s41467-021-26019-y.
Tan AR, Im SA, Mattar A, et al. Fixed-dose combination of pertuzumab and trastuzumab for subcutaneous injection plus chemotherapy in HER2-positive early breast cancer (FeDeriCa): a randomised, open-label, multicentre, non-inferiority, phase 3 study. Lancet Oncol. 2021;22(1):85–97. https://doi.org/10.1016/S1470-2045(20)30536-2.
Gianni L, Pienkowski T, Im YH, et al. 5-year analysis of neoadjuvant pertuzumab and trastuzumab in patients with locally advanced, inflammatory, or early-stage HER2-positive breast cancer (NeoSphere): a multicentre, open-label, phase 2 randomised trial. Lancet Oncol. 2016;17(6):791–800. https://doi.org/10.1016/S1470-2045(16)00163-7.
Bria E, Carbognin L, Furlanetto J, et al. Impact of neoadjuvant single or dual HER2 inhibition and chemotherapy backbone upon pathological complete response in operable and locally advanced breast cancer: Sensitivity analysis of randomized trials. Cancer Treat Rev. 2014;40(7):847–56. https://doi.org/10.1016/j.ctrv.2014.05.001.
Nagayama A, Hayashida T, Jinno H, et al. Comparative effectiveness of neoadjuvant therapy for HER2-positive breast cancer: a network meta-analysis. J Natl Cancer Inst. 2014;106(9):dju203. https://doi.org/10.1093/jnci/dju203.
Vazquez JC, Antolin S, Ruiz-Borrego M, et al. Dual neoadjuvant blockade plus chemotherapy versus monotherapy for the treatment of women with non-metastatic HER2-positive breast cancer: a systematic review and meta-analysis. Clin Transl Oncol. 2023;25(4):941–58. https://doi.org/10.1007/s12094-022-02998-2.
Slamon DJ, Leyland-Jones B, Shak S, et al. Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N Engl J Med. 2001;344(11):783–92. https://doi.org/10.1056/NEJM200103153441101.
Bozovic-Spasojevic I, Azim HA, Paesmans M, Suter T, Piccart MJ, de Azambuja E. Neoadjuvant anthracycline and trastuzumab for breast cancer: is concurrent treatment safe? Lancet Oncol. 2011;12(3):209–11. https://doi.org/10.1016/S1470-2045(11)70013-4.
Buzdar AU, Suman VJ, Meric-Bernstam F, et al. Fluorouracil, epirubicin, and cyclophosphamide (FEC-75) followed by paclitaxel plus trastuzumab versus paclitaxel plus trastuzumab followed by FEC-75 plus trastuzumab as neoadjuvant treatment for patients with HER2-positive breast cancer (Z1041): a randomised, controlled, phase 3 trial. Lancet Oncol. 2013;14(13):1317–25. https://doi.org/10.1016/S1470-2045(13)70502-3.
van der Voort A, van Ramshorst MS, van Werkhoven ED, et al. Three-year follow-up of neoadjuvant chemotherapy with or without anthracyclines in the presence of dual ERBB2 blockade in patients with ERBB2-positive breast cancer: a secondary analysis of the TRAIN-2 randomized, Phase 3 trial. JAMA Oncol. 2021;7(7):978–84. https://doi.org/10.1001/jamaoncol.2021.1371.
Slamon D, Eiermann W, Robert N, et al. Adjuvant trastuzumab in HER2-positive breast cancer. N Engl J Med. 2011;365(14):1273–83. https://doi.org/10.1056/NEJMoa0910383.
Sawaki M, Taira N, Uemura Y, et al. Randomized controlled trial of trastuzumab with or without chemotherapy for HER2-positive early breast cancer in older patients. JCO. 2020;38(32):3743–52. https://doi.org/10.1200/JCO.20.00184.
Gligorov J, Pivot X, Ataseven B, et al. Safety and efficacy of adjuvant subcutaneous trastuzumab in human epidermal growth factor receptor 2-positive early breast cancer: final results of the SafeHER study. The Breast. 2022;64:151–8. https://doi.org/10.1016/j.breast.2022.03.001.
Harbeck N, Nitz UA, Christgen M, et al. De-Escalated neoadjuvant trastuzumab-emtansine with or without endocrine therapy versus trastuzumab with endocrine therapy in HR+/HER2+ early breast cancer: 5-year survival in the WSG-ADAPT-TP trial. J Clin Oncol. 2023;41(22):3796–804. https://doi.org/10.1200/JCO.22.01816.
Waks AG, Desai NV, Li T, et al. A prospective trial of treatment de-escalation following neoadjuvant paclitaxel/trastuzumab/pertuzumab in HER2-positive breast cancer. NPJ Breast Cancer. 2022;8(1):63. https://doi.org/10.1038/s41523-022-00429-7.
Huober J, Barrios CH, Niikura N, et al. Atezolizumab with neoadjuvant anti-human epidermal growth factor receptor 2 therapy and chemotherapy in human epidermal growth factor receptor 2-positive early breast cancer: primary results of the randomized Phase III IMpassion050 trial. J Clin Oncol. 2022;40(25):2946–56. https://doi.org/10.1200/JCO.21.02772.
Krop IE, Suter TM, Dang CT, et al. Feasibility and cardiac safety of trastuzumab emtansine after anthracycline-based chemotherapy as (neo)adjuvant therapy for human epidermal growth factor receptor 2-positive early-stage breast cancer. J Clin Oncol. 2015;33(10):1136–42. https://doi.org/10.1200/JCO.2014.58.7782.
Loibl S, Mano M, Untch M, et al. Abstract GS03–12: Phase III study of adjuvant ado-trastuzumab emtansine vs trastuzumab for residual invasive HER2-positive early breast cancer after neoadjuvant chemotherapy and HER2-targeted therapy: KATHERINE final IDFS and updated OS analysis. Cancer Res. 2024;84(9_Supplement):GS03-12-GS03-12. https://doi.org/10.1158/1538-7445.SABCS23-GS03-12.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. H.B wrote the first draft of the manuscript. T.P. supervised the course of the article. M.E. critically reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Bischoff, H., Espié, M. & Petit, T. Unveiling Neoadjuvant Therapy: Insights and Outlooks for HER2-Positive Early Breast Cancer. Curr. Treat. Options in Oncol. (2024). https://doi.org/10.1007/s11864-024-01252-x
Accepted:
Published:
DOI: https://doi.org/10.1007/s11864-024-01252-x