Opinion Statement
The treatment landscape of renal cell carcinoma (RCC) has evolved significantly over the past three decades. Active surveillance and tumor ablation are alternatives to extirpative therapy in appropriately selected patients. Stereotactic body radiation therapy (SBRT) is an emerging noninvasive alternative to treat primary RCC tumors. The advent of immune checkpoint inhibitors (ICIs) has greatly improved the overall survival of advanced RCC, and now the ICI-based doublet (dual ICI-ICI doublet; or ICI in combination with a vascular endothelial growth factor tyrosine kinase inhibitor, ICI-TKI doublet) has become the standard frontline therapy. Based on unprecedented outcomes in the metastatic with ICIs, they are also being explored in the neoadjuvant and adjuvant setting for patients with high-risk disease. Adjuvant pembrolizumab has proven efficacy to reduce the risk of RCC recurrence after nephrectomy. Historically considered a radioresistant tumor, SBRT occupies an expanding role to treat RCC with oligometastasis or oligoprogression in combination with systemic therapy. Furthermore, SBRT is being investigated in combination with ICI-doublet in the advanced disease setting. Lastly, given the treatment paradigm is shifting to adopt ICIs at earlier disease course, the prospective studies guiding treatment sequencing in the post-ICI setting is maturing. The effort is ongoing in search of predictive biomarkers to guide optimal treatment option in RCC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Histologically, clear cell renal cell carcinoma (ccRCC) represents approximately 75–80% of RCC and the remainder of tumors classified as non-clear cell RCC (nccRCC). There have been tremendous advancements in understanding the biology of both ccRCC and nccRCC in the past three decades which has led to improved therapeutic options and prolonged survival. Despite this progress, it is estimated that there will be 81,800 new RCC cases diagnosed in the USA in 2023 and an estimated 14,890 deaths from RCC [1], suggesting an continued unmet need to improve outcomes in this disease. The current review aims to discuss the treatment modalities for localized and advanced RCC with a focus on assessing the landmark prospective studies.
Treatment of localized disease
The majority of patients with RCC are diagnosed with localized tumors. For patients with localized disease, the standard of care remains surgical excision, either through radical or partial nephrectomy. Active surveillance with or without tumor biopsy or tumor ablation are also options in appropriately selected patients. Despite definitive local therapy, a subgroup of patients will develop recurrent or advanced RCC with an estimated 5-year recurrence free survival ranged from 42 to 98% [2].
Risk stratification for localized disease
Risk stratification tools for localized disease have been developed over the years to identify patients with an increased likelihood of cancer recurrence and adverse outcomes. For localized RCC, tumor stage and nodal disease status in the TNM staging system are important prognostic factors. The tumor stage considers tumor size and disease extent. Nodal disease is infrequent but when present is invariably associated with poor prognosis [3]. In addition to the TNM staging, higher tumor grade is associated with increased disease recurrence independent of tumor stage [4]. Many nomograms have been developed combining the TNM staging system with additional clinical and pathologic factors (e.g., tumor grade, histologic features, performance status, tumor necrosis, clinical symptoms, and margin status) to aid in prognostication in the localized disease [5]. Currently, there is no validated biomarker beyond traditional clinical characteristics and histopathology in localized RCC.
Surgical management
Radical nephrectomy (RN) was historically served as the standard for management of all localized renal masses. However, partial nephrectomy (PN), using both open and robotic approaches, has now been recognized as the surgical standard for management of T1 (≤7 cm) renal masses. In T2 renal masses (>7 cm and limited to the kidney), PN is an acceptable approach in selected patients with the potential to preserve renal functional [6, 7]. In the setting of T3 disease, characterized by tumor extension beyond the renal cortex, RN has been viewed as the standard for definitive surgical management. However, recent literatures have examined the role of PN in this setting which showed acceptable outcomes in selected patients for which nephron-sparing surgery would be indicated [7,8,9].
Ablative approaches
Radiofrequency ablation (RFA) and cryoablation (CA) have been developed in recent years for selected patients with small renal masses [7]. Common indications include patients who are poor surgical candidates or who prefer a non-surgical approach. Current literature supports these ablative techniques as potential alternatives for patients with T1a masses (≤3 cm). A renal mass biopsy is recommended prior to or concomitant with ablation [10] to confirm histology and guide surveillance. Recent systematic review showed that ablation exhibited increased risk of local recurrence (5-year recurrent free rate: 94%) though this may be managed with repeat ablations with similar outcomes when treated with surgery [7, 11, 12].
Active surveillance
Increasing knowledge regarding the natural history of small renal masses, particularly in the context of competing patient comorbidities, led to interest in active surveillance as an initial management strategy for patients with small renal masses. Current guidelines endorse active surveillance as a part of the shared-decision making process in patients with small renal masses [13].
Adjuvant therapy
Cytokine therapy, vascular endothelial growth factor (VEGF) tyrosine kinase inhibitor (TKI), and mammalian target of rapamycin (mTOR) inhibitors were investigated in the adjuvant setting with mixed results [5, 14]. Sunitinib is the only FDA-approved VEGF TKI in resected high-risk ccRCC based on the positive phase III S-TRAC trial [15]. The primary endpoint was met which showed an improved disease-free survival (DFS) (6.8 years vs 5.6 years in placebo; p-value: 0.03). However, several other adjuvant studies (ASSURE, SORCE, PROTECT, ATLAS) [16,17,18,19] failed to demonstrate a clinical benefit of VEGF TKIs. Given the considerable toxicities and lack of proven overall survival (OS) benefit, adjuvant sunitinib has limited use in clinical practice.
Given the success of immune checkpoint inhibitor (ICIs) in the advanced disease setting, the efficacy of ICIs in the adjuvant/perioperative setting has also been evaluated. The KEYNOTE 564 was the first and the only positive adjuvant trial of ICIs in RCC. The study investigated 12-month pembrolizumab in patients with intermediate-high risk (pT2N0M0 grade 4 or sarcomatoid, or pT3N0M0 any grade) or high-risk (pT4N0M0 any grade, or pTxN1M0 any grade) ccRCC after definitive radical or partial nephrectomy [20••]. Patients with M1 disease rendered no evidence of disease (NED) ≤1 year from surgery were also included (brain or bone metastasis not eligible). At extended median follow-up of 30 months, adjuvant pembrolizumab continued to show improved DFS compared to placebo (78.3% vs 67.3% at 24 months, HR 0.63, 95% CI 0.50-0.80; p < 0.0001) [21••]. The OS data has not matured yet although the HR continued trending down. Of note, pembrolizumab generally has a favorable tolerability by patients but the toxicities are not negligible (20.7% patients in the pembrolizumab arm required treatment discontinuation due to adverse events and 7.4% patients required high-dose glucocorticoids). The judgement to offer adjuvant pembrolizumab should be based on individual’s disease recurrent risk and consider risk-benefit ratio through shared decision-making.
The promising results of KEYNOTE 564 was accompanied by a series of parallel negative adjuvant trials investigating other ICIs [5] (Table 1). The trials differed with regard to eligibility criteria, treatment, and design. These negative studies raised debates regarding whether the efficacy of ICIs exist in the adjuvant setting for RCC. There are many nuances that may explain the negative findings which are beyond the scope of this review [5]. In addition, cross-trial comparison is always challenging. Currently, adjuvant pembrolizumab is the only FDA-approved ICI in resected ccRCC. Highly sensitive biomarkers of minimal residual disease would identify patients most likely to benefit from adjuvant therapy while sparing those cured with surgery alone from unnecessary treatment-related toxicity with no oncologic benefit.
Neoadjuvant therapy
Neoadjuvant therapy with TKIs prior to nephrectomy has been shown to downstage the RCC tumors with high-risk features (e.g., large unresectable kidney mass, tumor thrombus invading the inferior vena cava) although currently there is no approved standard neoadjuvant therapy in RCC [22]. Given the success of ICI in the advanced disease setting, it has been hypothesized that neoadjuvant ICI could elicit robust immune response with the intact primary tumor providing high antigen load [23]. Two small studies investigating ICI monotherapy have showed safety/feasibility of neoadjuvant approach in RCC; however, radiographic response rate was low [24, 25]. There are several ongoing neoadjuvant RCC trials investigating ICI-based combinations [26].
Treatment of advanced or metastatic disease
Risk stratification for advanced disease
The Memorial Sloan Kettering Cancer Center (MSKCC) model was developed in the cytokine era and identified key prognostic factors [27] that are still pertinent to contemporary patients. The current widely used International Metastatic Renal Cell Carcinoma Database Consortium (IMDC) model was initially established in the targeted therapy era [28••] and is composed of two clinical factors (Karnofsky performance status/time from original RCC diagnosis to initiation of systemic therapy) and four laboratory factors from blood tests (hemoglobin/neutrophil/platelet/calcium). The IMDC model categorizes patients into favorable risk (0 factor), intermediate risk (1–2 factors), or poor risk (≥3 factors) based on the number of adverse prognostic factors and the risk groups are associated with differential OS. It was initially validated for patients with ccRCC and has subsequently been able to reliability predict survival for patients with nccRCC [29]. While initially developed as a prognostic model for patients initiating targeted therapy, the IMDC risk has been incorporated into landmark studies of immunotherapy combination regimens for baseline risk stratification. It has maintained relevance in the immunotherapy era given that front-line studies were specifically designed with endpoint in select IMDC risk-groups.
Frontline treatment for metastatic renal cell carcinoma (mccRCC)
The treatment paradigm for mccRCC has advanced remarkably in the past three decades. Up until 2005, treatment options for patients with mRCC were largely limited to cytokine-based therapies including interferon and interleukin-2. Given the advancements in our understanding of RCC pathogenesis, VEGF targeting agents entered the clinic in 2005 and remained the standard frontline treatment options until 2018. Currently, immune checkpoint inhibitor (ICI)–based doublets have significantly improved the OS of mccRCC and are now the new standard of care. There are two categories of ICI-based doublets: (1) the dual ICI combination targeting cytotoxic T lymphocyte-associated antigen 4 (CTLA-4) and programmed cell death 1 (PD-1) protein (ICI-ICI combination) and (2) the combination of an anti-PD1 ICI plus a vascular endothelial growth factor (VEGF) tyrosine kinase inhibitor (ICI-TKI combination). There are four ICI-based doublets that have demonstrated OS benefit compared to sunitinib in the intention-to-treatment population (ITT) (Table 2): ipilimumab/nivolumab (ICI-ICI combination) [30], pembrolizumab/axitinib (ICI-TKI combination) [31••], nivolumab/cabozantinib (ICI-TKI combination) [32••], and pembrolizumab/lenvatinib (ICI-TKI combination) [33••].
While these IO combination regimens are life prolonging, the two categories have distinct efficacy profile. One distinguishable feature of the ICI-ICI combination of ipilimumab/nivolumab is the long-term durable response: after a minimum follow-up of 5 years (median: 67.7 months), the duration of response (DOR) of ipilimumab/nivolumab had continued not been reached (NR) [34••]. For the ICI-TKI combinations, the median DOR ranged from 22 to 26.7 months (median follow-up time: 48–67.2 months) [35••, 36••, 37••]. On the contrary, the ICI-TKI combinations generally have longer PFS (median PFS range: 15.7–23.9 months vs 12.3 months in ipilimumab/nivolumab) and higher objective response rate (ORR) (range: 56–71% vs 39% in ipilimumab/nivolumab) [35••, 36••, 37••]. The primary disease progression (PD) rate also favors ICI-TKI combinations (range: 5.4–11.6% vs 17.6% in ipilimumab/nivolumab) [35••, 36••, 37••]. Lastly, given the potential persistent efficacy after ICI discontinuation, treatment-free survival (TFS), which was defined by the area between two Kaplan-Meier curves (time to protocol therapy cessation and time to subsequent systemic therapy), was investigated in the CheckMate 214. At 42-month follow-up, mean TFS was more than doubled in ipilimumab/nivolumab vs sunitinib (6.9 vs 3.1 months) in IMDC intermediate/poor risk and tripled in IMDC favorable risk (11.0 vs 3.7 months). Mean TFS with ≥grade 3 adverse events for ipilimumab/nivolumab were minor (0.6 months in intermediate/poor risk and 0.9 months in favorable risk). This analysis suggests that ipilimumab/nivolumab not only prolongs OS but patients also spend more time off therapy without toxicities with maintained disease control.
Currently, there is no level one evidence to suggest superiority of one combination over another and there are caveats in cross-trial comparisons. Decision making is empirically based on the treating physician’s interpretation of the existing data and considerations of burden of disease, toxicities, and patient fitness. Overall, the clinical efficacy of ipilimumab/nivolumab is mainly driven by the IMDC intermediate and poor risk patients, while the ICI-TKI combinations generally show efficacy across the three IMDC risk categories (Table 2).
IMDC intermediate/poor risk
-
ICI-ICI combination
The Food and Drug Administration (FDA) approved ipilimumab/nivolumab as a frontline therapy in the IMDC intermediate and poor risk patients based on the Checkmate 214 study [30]. The Co-primary endpoints (ORR/PFS/OS) were investigated among the IMDC intermediate and poor risk patients comparing ipilimumab/nivolumab versus sunitinib. After a minimum of 5-year follow-up [34••], the superior efficacy of ipilimumab/nivolumab were maintained (ORR: 42% vs 27%, PFS: 11.6 months vs 8.3 months, OS: 47 months vs 26.6 months) (Table 2). One recognizable hallmark of the dual ICI-ICI combination was the durable long-term efficacy as demonstrated at the tail of the PFS curve: the PFS had plateaued at 24 months (PFS at 24 months: 36.4%; PFS at 60 months: 31%) indicating that a subset of the patients had not progressed since randomization. In addition, the median DOR had not been reached (vs 19.7 months in sunitinib) [30].
-
ICI-TKI combination
The KEYNOTE 426 (pembrolizumab/axitinib) [31••], CheckMate 9ER (nivolumab/cabozantinib) [32••], and CLEAR (pembrolizumab/lenvatinib) [33••] investigated an anti-PD1 ICI plus an VEGF TKI in frontline mccRCC. The three ICI-TKI combinations all demonstrated OS benefit over sunitinib in the ITT population and received FDA approvals irrespective of IMDC risk. Subgroup analyses of the three ICI-TKI combinations all demonstrated superior ORR, PFS, and OS over sunitinib in the IMDC intermediate and poor risk and the efficacy were maintained after extended follow-up (Table 2) [35••, 36••, 37••].
IMDC favorable risk
-
ICI-ICI combination
Given the primary endpoint of CheckMate 214 was designed specifically in the intermediate-poor risk patients, the study was underpowered to assess statistically significant differences in OS in the favorable risk group (n). At 67.7 months of follow-up, ipilimumab/nivolumab demonstrated similar OS to sunitinib (median OS: 74.1 months vs 68.4 months, HR: 0.94, 95% CI: 0.65–1.37), shorter PFS (median PFS: 12.4 months vs 28.9 months, HR: 1.60, 95% CI: 1.13–2.26), and lower ORR (30% vs 52%) compared to sunitinib monotherapy [30]. Although the OS benefit was similar, the OS hazard ratios of ipilimumab/nivolumab had trended down over time (from 1.45 to 0.94; Table 3). Prolonged follow-up time would be required to formally investigate an OS benefit in this subgroup given the relatively indolent course of favorable risk disease and the OS would also be impacted by subsequent therapies. However, there was clearly a subset of favorable risk patients that benefited from ipilimumab/nivolumab as the median DOR was nearly doubled (61.5 months vs 33.2 months) among responders and the complete response (CR) rate was higher (13% vs 6%). Clinically, it is not unreasonable to consider ipilimumab/nivolumab in selected favorable risk patients (e.g., low volume disease) if the treatment goal is to prioritize long-term durable efficacy. Future studies are needed to identify biomarkers to select the ideal IMDC favorable risk patients to receive frontline ipilimumab/nivolumab combination.
-
ICI-TKI combination
Despite the higher ORR and numerically longer PFS with the ICI-TKI combinations over sunitinib (Table 2), whether the OS benefit of IO-TKI combinations also exists in the IMDC favorable risk subgroup has engendered debates. The disputes were due to the subgroup analyses of the three ICI-TKI trials (KEYNOTE-426, CheckMate 9ER, CLEAR) did not show a clear OS benefit over sunitinib after extended follow-up (Table 3). Of note, the landmark trials were not statistically powered to investigate the ICI-TKI combinations specifically in the IMDC favorable risk and the subgroup analyses should be interpreted as hypothesis-generating. In general, the efficacy of the three ICI-TKI doublets is considered superior to sunitinib and the NCCN guideline lists them as category 1 recommendation (but not sunitinib) for IMDC favorable risk disease [38]. Attention must be paid to the toxicities associated with the ICI-TKI doublets given the indolent biology of IMDC favorable disease and patients may stay on therapy for prolonged duration. The results from the subgroup analyses have also led to debates whether sequential approaches of systemic therapy (as opposed to ICI-doublets) in the IMDC favorable risk should be considered and this hypothesis can only be verified in prospective trials.
Triplet regimen: ICI-ICI-TKI
With the success of ICI-ICI and ICI-TKI in the frontline setting of mccRCC, it is rational to hypothesize that combining VEGF and dual ICI-ICI treatments would improve outcomes. COSMIC-313 was a phase III randomized placebo-controlled trial evaluating the triplet of ipilimumab/nivolumab/cabozantinib (40 mg daily) (ICI-ICI-TKI) vs ipilimumab/nivolumab (ICI-ICI) in the IMDC intermediate and poor risk patients [39••]. The primary endpoint of PFS was assessed in the first enrolled 550 patients, and the triplet regimen showed an improved PFS over ipilimumab/nivolumab (mPFS: NR vs 11.3; PFS at 12 months: 57% vs 49%, HR: 0.73, 95% CI: 0.57–0.94, p = 0.01). The ORR was numerically higher with the triplet: 43% (95% CI: 37–49%) vs 36% (95% CI: 30–42%). The OS data has not matured. When stratified by IMDC risk, ipilimumab/nivolumab/cabozantinib improved the PFS in the intermediate subgroup (HR: 0.63, 95% CI: 0.47–0.85) but interestingly not in the poor risk (HR: 1.04, 95% CI:0.65–1.69). In terms of toxicity profile, the triplet arm had higher grade 3/4 adverse events (79% vs 56%), more patients required dose holds of any medication (90% vs 70%), more patients required dose reduction of cabozantinib (54% vs 20%; average daily dose: 23.2 mg vs 36.1 mg of placebo), and less patients finished all four doses of ipilimumab (58% vs 73%). It is reasonable to postulate that the less than expected efficacy of this triplet regimen is the results of inadequate drug delivery due to significant toxicities.
Of note, the patient population in the COSMIC-313 was different from the aforementioned ICI-doublet trials. In addition to not including IMDC favorable risk disease, there were less patients who had radical nephrectomy (64% vs 74-83%) and less tumors with sarcomatoid features (6.3% vs 8–18%) [40].
Therefore, it is challenging to make comparisons across trials. Although not practice-changing, the COSMIC-313 should be accoladed as the first phase III trial that used a contemporary standard-of-care control (ipilimumab/nivolumab) and demonstrated the feasibility of triplet regimen in the frontline setting.
There is ongoing phase III study investigating the triplet regimen of pembrolizumab/belzutifan (HIF inhibitor)/lenvatinib or pembrolizumab/quavonlimab(anti-CTLA-4 antibody)/lenvatinib vs pembrolizumab/lenvatinib [41•]. Another phase III trial using an adaptive design (PDIGREE) that investigates maintenance nivolumab/cabozantinib vs nivolumab after ipilimumab/nivolumab induction among non-CR and non-PD patients and the results will provide additional information in the field [42•].
ICI monotherapy
Although not preferred, anti-PD-1 ICIs (pembrolizumab, nivolumab) have demonstrated anti-tumor activity as a single agent. The KEYNOTE 427 cohort A investigated pembrolizumab monotherapy in advanced ccRCC (N = 110) [43]. The ORR was 36% (95% CI: 27–46), disease control rate was 58% (95% CI: 45–68), and the median DOR was 19 months. The efficacy of nivolumab monotherapy in ccRCC was demonstrated in the HCRN GU 16-260 Part A (N = 123) [44]. The ORR was 34% (95% CI: 26–43), and the median DOR was 27.6 months. For patients who are less fit for ICI combinations, it is not unreasonable to offer ICI monotherapy to avoid additional toxicities.
Biomarker-driven trials in RCC
Tremendous efforts have been made to identify predictive biomarkers in mRCC to guide treatment selection [45]. BIONIKK was the first trial in mRCC which used gene expression signatures established in the TKI era and proved feasibility of such biomark-driven approach in prospective trial [46]. Currently, there is no available biomarker to guide decision between an ICI-ICI vs ICI-TKI combination in mRCC. A correlative study of the phase III IMmotion 151 used RNA-sequencing and categorized RCC tumors into seven biologically distinct clusters which had differential response to ICI [47]. An ongoing phase II OPTIC RCC trial adopts a biomarker-driven design and uses those clusters as predictive biomarker to assign protocol treatment between an ICI-TKI combination (nivolumab/cabozantinib) or an ICI-ICI combination (ipilimumab/nivolumab)[48]. RNA-sequencing will be performed on baseline tumor tissue to predict tumor cluster. The hypothesis is that the efficacy of the given ICI-doublet will be enhanced in biomarker selected patients compared to unselected patients in historical landmark trials.
Treatment options for refractory mccRCC
While ICI-based doublets have greatly improved OS in mccRCC, there is a subset of patients that exhibit primary resistance to ICI-doublets (PD rate: 5–18%) [30, 31••, 32••, 33••] and the majority of patients eventually progress despite initial response (mPFS : 12.3–23.9 months) [30, 31••, 32••, 33••]. Treatment options for subsequent therapies depends on the received first-line treatment, and the current evidence guiding treatment sequencing after frontline ICI-based combinations continues to evolve.
VEGF TKIs
Historical trials of VEGF TKIs (cabozantinib, axitinib, lenvatinib plus everolimus) [49,50,51] had demonstrated activities in the refractory setting after progression of prior TKIs although those trials included negligible patients who had prior ICIs. Recent studies of axitinib (NCT02579811) [52], cabozantinib (BREAKPOINT, CaboPoint) [53], and tivozanib (TIVO-3) [54••] either required progression after ICI therapy as trial eligibility or included a higher proportion of post-ICI patients. The prospective trials of VEGF TKIs in the refractory setting are summarized in Table 4.
-
Axitinib
The efficacy of axitinib in the second-line setting was established in the AXIS trial and the results demonstrated a PFS benefit over sorafenib [50, 55]. A single-arm phase II study (NCT02579811) investigated individualized dosing of axitinib in previously treated mccRCC with ICI being the most recent therapy (N = 40; 63% had nivolumab monotherapy; 15% had ipilimumab/nivolumab) [52]. The result showed a median PFS of 8.8 months which did not meet the prespecified PFS threshold (9.5 months), and the ORR was 45%. A post hoc analysis among patients who discontinued ICI due to disease progression (N = 37) showed a median PFS of 9.2 months (95% CI: 6.2–16.6).
-
Cabozantinib
In the phase III METEOR trial, cabozantinib demonstrated OS (median OS: 21.4 vs 16.5 months) and PFS (median PFS: 7.4 vs 3.9 months) benefit over everolimus after progression of prior VEGF TKIs [49] although only ≤5% patients had prior ICI treatment in this dataset [49].
Cabozantinib (60 mg daily) was evaluated in the phase II single-arm BREAKPOINT study which included contemporary patients progressed after adjuvant or first-line ICI [53]. Thirty patients were included for analysis (19 had ipilimumab/nivolumab, 7 had pembrolizumab/lenvatinib). The median PFS was 8.3 months (95% CI: 3.9–17.4) which met the prespecified threshold (mPFS: 7.4 months). Another on-going phase II trial, CaboPoint, is evaluating cabozantinib (60 mg daily) after frontline ipilimumab/nivolumab (cohort A, recruitment goal: N = 125) or ICI-TKI (cohort B, recruitment goal: N = 125) [56•]. An interim analysis was reported in February 2023: the ORR was 31.7% (95% CI: 20.3–45.0) and 25% (95% CI: 10.7–44.9) in cohort A (N = 60) and B (N = 28), respectively [57•].
The efficacy of cabozantinib in the post-ICI setting was also elucidated in two more recent randomized studies which used cabozantinib monotherapy as the control arm. In the CANTANA study [58] (62% had prior ICI; 29% had prior ipilimumab/nivolumab), the cabozantinib arm (N = 223) showed a median PFS of 9.3 months, ORR of 28%, and primary PD rate of 8%. In the Contact-3 study [59••] (100% had prior ICI), cabozantinib monotherapy (N = 254) showed a median PFS: 10.8 months, ORR of 41%, and primary PD rate of 5%.
-
Lenvatinib plus everolimus
A phase II three-arm study randomized mccRCC patients who previously treated with VEGF TKIs to lenvatinib (18 mg daily) plus everolimus (5 mg daily), lenvatinib monotherapy (24 mg daily), or everolimus monotherapy (10 mg/daily) [51]. Lenvatinib plus everolimus met primary endpoint (PFS) over everolimus (median PFS: 14.6 vs 5.5 months, HR: 0.40, 95% CI: 0.24–0.68), and OS was improved in the updated post hoc analysis (median OS: 25.5 vs 15.4 months, HR: 0.51, 95% CI: 0.30–0.88). Lenvatinib monotherapy also demonstrated activity with improved PFS over everolimus (median PFS: 7.4 vs 5.5 months, HR: 0.61, 95% CI: 0.38–0.98) and numerically longer OS (median OS: 19.1 vs 15.4 months, HR: 0.68, 95% CI: 0.41–1.14). Of note, only 5 patients included in this trial (N = 153) had prior ICI therapy.
-
Tivozanib
Tivo-3 is a phase III randomized trial which investigated tivozanib vs sorafenib in previously treated mccRCC (two or three previous systemic therapy; at least one VEGF TKI) [54••]. Patients (350) were included in this trial, and 26% had prior ICI-TKI combination. In the ITT population, tivozanib showed a PFS benefit over sorafenib (mPFS: 5.6 vs 3.9 months, HR: 0.73, 95% CI: 0.56–0.94) and met the trials primary endpoint. There was no OS difference (mOS: 16.4 vs 19.2 months, HR: 0.97, 95% CI: 0.75–1.24). The ORR was higher with tivozanib (18% vs 8%). In the ICI-treated subgroup, tivozanib showed improved PFS (mPFS: 7.3 vs 5.1 months, HR: 0.55, 95% CI: 0.32–0.94) but no OS difference (HR: 0.84, 95% CI: 0.50–1.40) [60•]. Tivozanib also showed a favorable toxicity profile with less diarrhea (any grade: 35% vs 57%; grade 3: 2% vs 9%), less hand foot syndrome (any grade: 17% vs 46%; grade 3: 1% vs 10%), and better tolerability (dose interruption due to treated-related adverse events: 48% vs 63%; dose reduction due to treated-related adverse events: 24% vs 38%).
Rechallenge of ICI
With the rapid adoptions of ICI-based combinations in the frontline setting, a clinically relevant question was whether there would be a role for ICI rechallenge after progression of prior ICIs. Small datasets from retrospective studies suggested the ORR were 23–25% [61, 62]. Recently, several prospective phase II trials investigated an adaptive approach (OMNIVORE, TITAN-RCC, HCRN GU16-260): nivolumab monotherapy was initiated as frontline therapy with ipilimumab/nivolumab as the salvage treatment for non-responders or stable disease. The ORRs for salvage approach were generally not encouraging (4% (OMNIVORE), 16% (TITAN-RCC), 11.4% (HCRN GU16-260)) and did not support such response-adaptive strategy [44, 63, 64] (Table 5).
Fraction-RCC is a signal-seeking randomized phase II trial which evaluated ICI combinations in advanced RCC who had previously progressed on ICI therapy (track 2) [65•]. For patients who were randomized to ipilimumab/nivolumab arm, eight patients (8/46) achieved partial response and zero patients had CR. The ORR was 17.4% (95% CI: 7.8–31.4). The median PFS was 3.7 months (95 CI: 2.0–7.3), and median OS was 23.8 months (95% CI: 13.2–not estimable). Of note, although the ORR was modest, the median DOR was 16.4 (95% CI: 2.1–27) suggesting a small subset of patients may derive benefit with ipilimumab/nivolumab after progression of prior PD-1/PD-L1 inhibitors, though data need to be interpreted with caution.
For ICI-TKI combination in the refractory setting, KEYNOTE-146 evaluated pembrolizumab/lenvatinib in a phase IB/II single-arm study [66•]. The ICI-treated subgroup required disease progression of prior anti-PD-1/PD-L1 regimens. After a median follow-up of 19.8 months, in the ICI-treated subgroup (N = 104; 65% had previous anti-VEGF therapies), the ORR was 55.8% (95 CI: 45.7–65.5) with a median DOR of 12.5 months (95% CI: 9.1–17.5). The median PFS was 12.2 months (95% CI: 9.5–17.7), and the OS was not reached. While these data are encouraging, it is difficult to isolate the effect of the component parts in this single arm study. The recently reported phase III CONTACT-03 study randomized ICI-treated mccRCC (N = 533) to atezolizumab (PD-L1 inhibitor)/cabozantinib vs cabozantinib [59••]. Patients who had disease progression during or after ICI (anti-PD-L1 or anti-PD-1) in the first-line or second-line setting and ICI being the immediately preceding line of therapy were eligible. The two-primary endpoints were PFS and OS. After a median follow-up of 15.2 months, there was neither a PFS (mPFS: 10.6 vs 10.8 months, HR: 1.03, 95% CI: 0.83–1.28) nor OS benefit (mOS: 25.7 vs NR months, HR: 0.94, 95% CI: 0.70–1.27) of atezolizumab/cabozantinib combination. More serious adverse events occurred in the atezolizumab/cabozantinib arm (48% vs 33%; adverse events leading to death: 6% vs 4%). The CONTACT-03 study did not support the PD-L1 inhibitor of atezolizumab/cabozantinib in previously ICI-treated mccRCC. A phase III randomized TiNiVO-2 study (NCT04987203) is on-going which investigates the PD-1 inhibitor of nivolumab in combination with tivozanib vs tivozanib monotherapy in ICI-treated mccRCC (recruitment goal: N = 326; primary endpoint: PFS) [67•].
Role of cytoreductive nephrectomy
The OS benefit of upfront cytoreductive nephrectomy (CN) in mRCC was supported by two landmark trials conducted in the cytokine era [68, 69]. Although there had been no available prospective data evaluating CN in the early targeted therapy era, the benefit of CN was extrapolated from the two landmark trials and retrospective data suggested OS benefit of CN in the context of VEGF TKIs [70]. This practice was formally challenged after the results from the landmark CARMENA trial. CARMENA was a phase III, noninferiority trial that investigated sunitinib alone vs CN followed by sunitinib (CN-sunitinib) in 450 MSKCC intermediate and poor risk mRCC [71]. The non-inferiority margin was set as the upper boundary of the 95% CI of the death hazard ratio ≤1.20. The initial results supported noninferiority of sunitinib alone compared to CN-sunitinib (median OS: 18.4 vs. 13.9 months, HR 0.89, 95% CI: 0.71 to 1.10) [71]. However, the results also engendered criticism for disproportionate accrual of poor risk patients (44%) which left unanswered question for the true role of CN in selected intermediate risk patients. An updated analysis with longer follow-up continued to show noninferiority of sunitinib alone (HR: 0.97, 95% CI, 0.79–1.19) and numerically longer OS (19.8 vs 15.6 months) compared to CN-sunitinib in the ITT population. Patients were further reclassified with the IMDC criteria in the post hoc analysis. Among IMDC intermediate risk, sunitinib alone had numerically longer OS (27.9 vs 19 months) although the results did not meet noninferiority (HR: 0.94, 95% CI: 0.70–1.24). When stratified by the number of risk factors (1 or 2), the OS favored CN-nephrectomy among patients with only one IMDC risk factor (31.4 vs 25.2 months) but not among patients with two IMDC risk factors (17.6 vs 31.2 months). Post hoc analysis was also conducted by the number of metastatic sites (1 vs ≥ 2). The OS favored upfront CN over sunitinib alone for patients with only one metastasis (OS: 23.2 vs 22.7 months) but not for patients with ≥2 metastasis (OS: 14.4 vs 16.7 months). Taken together the above analyses, CARMENA emphasized the importance of thorough patient selection (e.g., IMDC risk 0 or 1 and low-volume disease) in identifying patients for upfront CN. Another phase III SURTIME trial randomized mccRCC patients to immediate CN vs 3 cycles of sunitinib followed by CN (deferred CN). Due to poor trial accrual, the final study included 99 patients and there was no progression-free benefit (primary endpoint) of immediate CN vs deferred CN. Patients in the deferred CN arm had longer OS (32.4 vs 15 months, HR: 0.57, 95% CI: 0.34–0.95).
Based on the results from CARMENA and SURTIME, the utilization of upfront CN has been declining as reflected in the recent landmark ICI-doublet trials. However, the timing and eligibility for CN are still unclear in the contemporary kidney cancer patients receiving frontline ICI regimens. There are currently several prospective clinical trials that are evaluating the role of CN in the immunotherapy era including PROBE [72] (NCT04510597), NORDIC-SUN [73] (NCT03977571), and Cyto-KIK [73] (NCT04322955).
Role of radiation therapy
SBRT for primary RCC
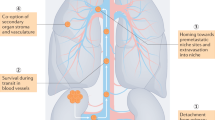
Historically, RCC was considered to be a radioresistant malignancy when utilized in the context of conventional fractionation. However, when human RCC cell lines were exposed to increased radiation doses, there are an exponential decrease in survival compared to the minimal survival effects from conventional radiation [74]. Stereotactic body radiation therapy (SBRT, dose ≥ 5 Gy delivered in five or fewer fractions) provides high-dose and precise conformal radiation, and its clinical efficacy in inoperable primary kidney cancer tumor has been reported since the early 2000s [75,76,77]. SBRT is an effective alternative and offers noninvasive cytoreduction to nonsurgical candidates while potentially preserving kidney function [78]. Additionally, SBRT has the potential to augment the anti-tumor immune response via increase in tumor-antigen presentation and immune-cell infiltration and therefore has the potential to increase the efficacy of ICI in mRCC [79,80,81]. This concept is currently being investigated in the phase II SAMURAI study which randomizes patients in a 2:1 ratio to receive SBRT (42 Gy in 3 fractions) plus ICI-doublet vs ICI-doublet alone (NCT05327686, NRG GU-012) in IMDC intermediate/poor risk patients [82•]. Another similar phase II study, CYTOSHRINK, randomizes patients (2:1 ratio) to SBRT (30–40 Gy in five fractions) plus ipilimumab/nivolumab vs ipilimumab/nivolumab in IMDC intermediate/poor RCC (NCT04090710) [83]. Both studies allow mRCC with any histology.
Oligometastatic
Oligometastatic (OM) disease involves metastatic lesions with limited spread; this is typically a maximum of five lesions, though criteria to define oligometastatic disease across solid tumor malignancies are evolving [84]. Metastatic-directed therapy (MDT) was historically performed through surgical measures, but has more recently expanded to include SBRT [85]. Several studies have investigated SBRT for OM RCC [86]. A single-arm study by Tang et el. studied oligometastatic RCC (≤5 metastases; with no more than one line of prior systemic therapy; IMDC favorable risk: 47%, intermediate risk: 50%) to receive SBRT to all lesions and maintained off systemic therapy. The median PFS was 22.7 months (1-year PFS of 64% (95% CI: 48–85)), and the 1-year adjusted systemic therapy-free survival was 86% [87•]. In another single-arm study of SBRT by Hannan et al. was investigated in treatment naïve OM RCC with ≤3 extracranial metastases (74% IMDC favorable and 26% intermediate risk). The median time to start of systemic therapy (primary endpoint) was 26.6 months (interquartile range: 16.3–30.3), the 1-year freedom from systemic therapy probability was 91.3% (95% CI: 69.5–97.8), and the 1-year PFS was 82.6% (95% CI, 60.1–93.1) [88•]. Shiva et al. investigated SBRT in OM RCC (≤5 metastases) with ≤ two lines of prior systemic therapy followed by eight cycles of pembrolizumab (200 mg, every 3 weeks). The ORR was 63%, and disease control rate was 83%. The 12-month and 24-month PFS were 60% and 45%, respectively, and the OS was 90% and 74%, respectively [89].
Oligoprogression
Oligoprogression (OP) in mRCC typically means an individual who has disease progression of a select number of metastatic lesions, while other metastatic sites remain responsive/stable to a given systemic therapy. SBRT to those progression sites could achieve desirable disease control while extending the duration of the given systemic agent [86]. A phase II single-arm study investigated SBRT in IMDC favorable/intermediate mRCC who had OP after ≥ 3 months of TKI therapy. This trial closed prematurely due to slow accrual after 38 patients were enrolled. The median PFS was 9.3 months (95% CI: 7.5–15.7), and the median time to change systemic therapy was 12.6 months (95% CI: 9.6–17.4). Another phase II single-arm study (N = 20) reported SBRT delayed new systemic therapy by >6 months in 70% patients with OP mRCC (median: 11 months, 95% CI: 4.5–19.3). Of note, patients on ICI in this trial had longer PFS compared to TKI, suggesting a synergistic effect of IO and SBRT combination [88•]. Ongoing prospective trials are investigating ICI and SBRT combination in OP RCC (NCT04974671, NCT04299646).
Special considerations for non-clear cell RCC
nccRCC represents a biologically heterogeneous disease entity and roughly 20–25% of the kidney cancer belongs to nccRCC, with papillary RCC being the most common (10–15%), followed by chromophobe RCC (5%). Other subtypes such as medullary RCC, collecting duct RCC, and unclassified RCC represent <1% of nccRCC. Of note, the WHO published the fifth edition classification of urogenital tumors in 2022. This version did not classify papillary RCC into type 1 or type 2. Additionally, it added a molecular-defined RCC category (e.g., fumarate hydratase-deficient RCC, succinate dehydrogenase-deficient RCC, SMARCB1-deficient RCC, ALK-rearranged RCC) in addition to morphology-based classification. Given the scarcity of nccRCC, it is challenging to conduct large trials in this disease space. The current available systemic agents such as TKIs and ICIs have various activities in nccRCC, but the efficacy is generally lower compared to ccRCC. In addition, most of the data is driven by papillary RCC with mixed representation of other subtypes in the datasets [90].
MET proto-oncogene alterations are commonly found in papillary RCC [91]. Cabozantinib, the multi-targeted (MET/VEGF/AXL/RET/KIT) TKI, has the most robust activity as a single agent in this histology. The phase II randomized PAMPET study investigated cabozantinib vs sunitinib in the papillary RCC which demonstrated longer PFS (median: 9 vs 5.6 months, HR: 0.60, 95% CI: 0.37–0.97) and higher ORR (23% vs 4%). For ICI monotherapy, the ORR of nivolumab in nccRCC was around 13–14% in two single-arm studies (CheckMate-374 cohort B, N = 44 (55% was papillary RCC); HCRN GU 16-260 cohort B (part A), N = 35 (54% was papillary RCC)) [92, 93]. Pembrolizumab had an ORR of 27% in the single-arm KEYNOTE-427 (cohort B, N = 165 (72% was papillary RCC)) with a median DOR of 29 months [94•]. In the papillary histology, the ORR was 29% (95% CI: 21–38%). With regard to the ICI-based doublets, ipilimumab/nivolumab was reported to have an ORR of 20% (95% CI: 9–34%) in the CheckMate 920 (N = 52; 42% was unclassified and 35% was papillary) [95]. Atezolizumab/bevacizumab was investigated in a phase II study of advanced RCC. Among the subgroup of nccRCC (N = 42, papillary: 35%, chromophobe: 29%; unclassified: 26%), the ORR was 26% [96]. Nivolumab/cabozantinib was investigated in a single-center study which included two cohorts of nccRCC [97]. Cohort A (N = 40 patients; papillary: 80%, unclassified: 15%, translocation-associated: 5%) reported an ORR of 48% (95% CI: 32–64%); cohort B included seven chromophobe patients, and none of them had response. This cohort was closed early for futility. Pembrolizumab/lenvatinib was investigated in a multi-center single-arm study (KEYNOTE-B61) in nccRCC (N = 158; papillary: 58%, chromophobe: 18%, unclassified: 13%) [98•]. The ORR was 49% (95% CI: 41–57) in all nccRCC and 54% (95% CI: 43-64) in papillary RCC including a CR rate of 9%. For chromophobe (N = 29), eight patients achieved partial response (ORR: 28%, 95% CI:13–47).
In summary, aside from papillary RCC, the contemporary ICI-based regimens have modest activity in other subtypes of nccRCC. In addition, evidence to support subsequent lines of therapy is elusive. Future prospective studies targeting novel mechanisms in nccRCC are warranted to fill the unmet needs.
Conclusions
With the advent of new treatment modalities including ablative techniques, SBRT, and ICIs, the OS of patients with RCC have prolonged significantly across the disease spectrum. ICIs have brought the possibilities of cure even in advanced disease. With improved understanding of the RCC biology and cancer immunology, the development of novel therapeutics is anticipated in near future. The knowledge of ideal treatment sequencing will continue to evolve.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
NCI SEER Program. Cancer stat facts: kidney and renal pelvis cancer. 2023.
Speed JM, Trinh QD, Choueiri TK, Sun M. Recurrence in localized renal cell carcinoma: a systematic review of contemporary data. Curr Urol Rep. 2017;18:15.
Terrone C, Cracco C, Porpiglia F, et al. Reassessing the current TNM lymph node staging for renal cell carcinoma. Eur Urol. 2006;49:324–31.
Tsui KH, Shvarts O, Smith RB, et al. Prognostic indicators for renal cell carcinoma: a multivariate analysis of 643 patients using the revised 1997 TNM staging criteria. J Urol. 2000;163:1090–5 quiz 1295.
Wang LL, Saidian A, Pan E, et al. Adjuvant therapy in renal cell carcinoma: are we ready for prime time? Kidney Cancer. 2023;7:1–11.
Mir MC, Derweesh I, Porpiglia F, et al. Partial nephrectomy versus radical nephrectomy for clinical T1b and T2 renal tumors: a systematic review and meta-analysis of comparative studies. Eur Urol. 2017;71:606–17.
Dhanji S, Wang L, Liu F, et al. Recent advances in the management of localized and locally advanced renal cell carcinoma: a narrative review. Res Rep Urol. 2023;15:99–108.
Yim K, Aron M, Rha KH, et al. Outcomes of robot-assisted partial nephrectomy for clinical T3a renal masses: a multicenter analysis. Eur Urol Focus. 2021;7:1107–14.
Andrade HS, Zargar H, Akca O, et al. Is robotic partial nephrectomy safe for T3a renal cell carcinoma? Experience of a high-volume center. J Endourol. 2017;31:153–7.
Campbell SC, Clark PE, Chang SS, et al. Renal mass and localized renal cancer: evaluation, management, and follow-up: AUA guideline: part I. J Urol. 2021;206:199–208.
Pierorazio PM, Johnson MH, Patel HD et al. AHRQ comparative effectiveness reviews. In Management of renal masses and localized renal cancer. Rockville (MD): Agency for Healthcare Research and Quality (US) 2016.
Pierorazio PM, Johnson MH, Patel HD, et al. Management of renal masses and localized renal cancer: systematic review and meta-analysis. J Urol. 2016;196:989–99.
Campbell SC, Uzzo RG, Karam JA, et al. Renal mass and localized renal cancer: evaluation, management, and follow-up: AUA guideline: part II. J Urol. 2021;206:209–18.
McKay RR. The promise of adjuvant immunotherapy in renal-cell carcinoma. N Engl J Med. 2021;385:756–8.
Ravaud A, Motzer RJ, Pandha HS, et al. Adjuvant sunitinib in high-risk renal-cell carcinoma after nephrectomy. N Engl J Med. 2016;375:2246–54.
Haas NB, Manola J, Uzzo RG, et al. Adjuvant sunitinib or sorafenib for high-risk, non-metastatic renal-cell carcinoma (ECOG-ACRIN E2805): a double-blind, placebo-controlled, randomised, phase 3 trial. Lancet. 2016;387:2008–16.
Eisen T, Frangou E, Oza B, et al. Adjuvant sorafenib for renal cell carcinoma at intermediate or high risk of relapse: results from the SORCE randomized phase III intergroup trial. J Clin Oncol. 2020;38:4064–75.
Motzer RJ, Russo P, Haas N, et al. Adjuvant pazopanib versus placebo after nephrectomy in patients with localized or locally advanced renal cell carcinoma: final overall survival analysis of the phase 3 PROTECT trial. Eur Urol. 2021;79:334–8.
Gross-Goupil M, Kwon TG, Eto M, et al. Axitinib versus placebo as an adjuvant treatment of renal cell carcinoma: results from the phase III, randomized ATLAS trial. Ann Oncol. 2018;29:2371–8.
Choueiri TK, Tomczak P, Park SH, et al. Adjuvant pembrolizumab after nephrectomy in renal-cell carcinoma. N Engl J Med. 2021;385:683–94. This landmark trial stablished the role of adjuvant pembrolizumab in RCC.
Choueiri T, Tomczak P, Park SH, et al. Pembrolizumab as post nephrectomy adjuvant therapy for patients with renal cell carcinoma: results from 30-month follow-up of KEYNOTE-564. J Clin Oncol. 2023;40:abstr 290. This reference showed the efficacy of adjuvant pembrolizumab in RCC after extended follow-up.
Borregales LD, Adibi M, Thomas AZ, et al. The role of neoadjuvant therapy in the management of locally advanced renal cell carcinoma. Ther Adv Urol. 2016;8:130–41.
Topalian SL, Taube JM, Pardoll DM. Neoadjuvant checkpoint blockade for cancer immunotherapy. Science. 2020;367:eaax0 182.
Gorin MA, Patel HD, Rowe SP, et al. Neoadjuvant nivolumab in patients with high-risk nonmetastatic renal cell carcinoma. Eur Urol Oncol. 2022;5:113–7.
Carlo MI, Attalla K, Mazaheri Y, et al. Phase II study of neoadjuvant nivolumab in patients with locally advanced clear cell renal cell carcinoma undergoing nephrectomy. Eur Urol. 2022;81:570–3.
Kaur J, Patil G, Geynisman DM, Ghatalia P. Role of perioperative immunotherapy in localized renal cell carcinoma. Ther Adv Med Oncol. 2023;15:17588359231181496.
Motzer RJ, Bacik J, Murphy BA, et al. Interferon-alfa as a comparative treatment for clinical trials of new therapies against advanced renal cell carcinoma. J Clin Oncol. 2002;20:289–96.
Heng DY, Xie W, Regan MM, et al. Prognostic factors for overall survival in patients with metastatic renal cell carcinoma treated with vascular endothelial growth factor-targeted agents: results from a large, multicenter study. J Clin Oncol. 2009;27:5794–9. This reference proposed the IMDC prognostic criteria in RCC.
Kroeger N, Xie W, Lee JL, et al. Metastatic non-clear cell renal cell carcinoma treated with targeted therapy agents: characterization of survival outcome and application of the International mRCC Database Consortium criteria. Cancer. 2013;119:2999–3006.
Motzer RJ, Tannir NM, McDermott DF, et al. Nivolumab plus ipilimumab versus sunitinib in advanced renal-cell carcinoma. N Engl J Med. 2018;378:1277–90 (Landmark CheckMate 214 trial).
Rini BI, Plimack ER, Stus V, et al. Pembrolizumab plus axitinib versus sunitinib for advanced renal-cell carcinoma. N Engl J Med. 2019;380:1116–27. This landmark trial established the role of pembrolizumab/axitinib in first-line RCC.
Choueiri TK, Powles T, Burotto M, et al. Nivolumab plus cabozantinib versus sunitinib for advanced renal-cell carcinoma. N Engl J Med. 2021;384:829–41. Landmark CheckMate 9ER trial.
Motzer R, Alekseev B, Rha SY, et al. Lenvatinib plus pembrolizumab or everolimus for advanced renal cell carcinoma. N Engl J Med. 2021;384:1289–300. Landmark CLEAR tria l.
Motzer RJ, McDermott DF, Escudier B, et al. Conditional survival and long-term efficacy with nivolumab plus ipilimumab versus sunitinib in patients with advanced renal cell carcinoma. Cancer. 2022;128:2085–97. This reference showed the extended follow-up of CheckMate 214 and continued to show the efficacy of ipilimumab/nivolumab in the first-line setting.
Rini BI, Plimack ER, Stus V, et al. Pembrolizumab plus axitinib versus sunitinib as first-line therapy for advanced clear cell renal cell carcinoma: 5-year analysis of KEYNOTE-426. J Clin Oncol. 2023;41:LBA4501–LBA4501. This reference showed the extended follow-up of KEYNOTE-426 and continued to show the efficacy of pembrolizumab/axitinib in the first-line setting.
Burotto M, Powles T, Escudier B, et al. Nivolumab plus cabozantinib vs sunitinib for first-line treatment of advanced renal cell carcinoma (aRCC): 3-year follow-up from the phase 3 CheckMate 9ER trial. J Clin Oncol. 2023;41:603–603. This reference showed the extended follow-up of CheckMate 9ER and continued to show the efficacy of nivolumab/cabozantinib in the first-line setting.
Motzer RJ, Porta C, Eto M, et al. Final prespecified overall survival (OS) analysis of CLEAR: 4-year follow-up of lenvatinib plus pembrolizumab (L+P) vs sunitinib (S) in patients (pts) with advanced renal cell carcinoma (aRCC). J Clin Oncol. 2023;41:4502–4502. This reference showed the extended follow-up of CLEAR and continued to show the efficacy of pembrolizumab/lenvatinib in the first-line setting.
National Comprehensive Cancer Network. Kidney Cancer 2023.
Choueiri TK, Powles T, Albiges L, et al. Cabozantinib plus nivolumab and ipilimumab in renal-cell carcinoma. N Engl J Med. 2023;388:1767–78. Triplet study which investigated ipilimumab/nivolumab/cabozantinib in first-line RCC.
Rini BI, Signoretti S, Choueiri TK, et al. Long-term outcomes with nivolumab plus ipilimumab versus sunitinib in first-line treatment of patients with advanced sarcomatoid renal cell carcinoma. J Immunother Cancer. 2022;10:e005445.
Choueiri T, Plimack ER, Powles T, et al. Phase 3 study of first-line treatment with pembrolizumab + belzutifan + lenvatinib or pembrolizumab/quavonlimab + lenvatinib versus pembrolizumab + lenvatinib for advanced renal cell carcinoma (RCC). J Clin Oncol. 2022;40:abstr TPS99. Ongoing trial of the triplet regimens in first-line RCC.
Zhang T, Ballman K, Choudhury A et al. PDIGREE: An adaptive phase III trial of PD-inhibitor nivolumab and ipilimumab (IPI-NIVO) with VEGF TKI cabozantinib (CABO) in metastatic untreated renal cell cancer (Alliance A031704). J Clin Oncol 2020; 366. Ongoing PDIGREE trial which uses a risk-adaptive design.
McDermott DF, Lee JL, Bjarnason GA, et al. Open-Label, Single-arm phase II study of pembrolizumab monotherapy as first-line therapy in patients with advanced clear cell renal cell carcinoma. J Clin Oncol. 2021;39:1020–8.
Atkins MB, Jegede OA, Haas NB, et al. Phase II study of nivolumab and salvage nivolumab/ipilimumab in treatment-naive patients with advanced clear cell renal cell carcinoma (HCRN GU16-260-Cohort A). J Clin Oncol. 2022;40:2913–23.
Tucker MD, Rini BI. Predicting response to immunotherapy in metastatic renal cell carcinoma. Cancers (Basel). 2020;12:2662.
Vano YA, Elaidi R, Bennamoun M, et al. Nivolumab, nivolumab-ipilimumab, and VEGFR-tyrosine kinase inhibitors as first-line treatment for metastatic clear-cell renal cell carcinoma (BIONIKK): a biomarker-driven, open-label, non-comparative, randomised, phase 2 trial. Lancet Oncol. 2022;23:612–24.
Motzer RJ, Banchereau R, Hamidi H, et al. Molecular subsets in renal cancer determine outcome to checkpoint and angiogenesis blockade. Cancer Cell. 2020;38:803-817.e804.
Chen Y, Beckermann K, Haake S, et al. Optimal treatment by invoking biologic clusters in renal cell carcinoma (OPTIC RCC). J Clin Oncol. 2023;41:742.
Choueiri TK, Escudier B, Powles T, et al. Cabozantinib versus everolimus in advanced renal cell carcinoma (METEOR): final results from a randomised, open-label, phase 3 trial. Lancet Oncol. 2016;17:917–27.
Rini BI, Escudier B, Tomczak P, et al. Comparative effectiveness of axitinib versus sorafenib in advanced renal cell carcinoma (AXIS): a randomised phase 3 trial. Lancet. 2011;378:1931–9.
Motzer RJ, Hutson TE, Glen H, et al. Lenvatinib, everolimus, and the combination in patients with metastatic renal cell carcinoma: a randomised, phase 2, open-label, multicentre trial. Lancet Oncol. 2015;16:1473–82.
Ornstein MC, Pal SK, Wood LS, et al. Individualised axitinib regimen for patients with metastatic renal cell carcinoma after treatment with checkpoint inhibitors: a multicentre, single-arm, phase 2 study. Lancet Oncol. 2019;20:1386–94.
Procopio G, Claps M, Pircher C, et al. A multicenter phase 2 single arm study of cabozantinib in patients with advanced or unresectable renal cell carcinoma pre-treated with one immune-checkpoint inhibitor: The BREAKPOINT trial (Meet-Uro trial 03). Tumori. 2023;109:129–37.
Rini BI, Pal SK, Escudier BJ, et al. Tivozanib versus sorafenib in patients with advanced renal cell carcinoma (TIVO-3): a phase 3, multicentre, randomised, controlled, open-label study. Lancet Oncol. 2020;21:95–104. This reference estabilished the role of tivozanib in the refractory RCC setting.
Motzer RJ, Escudier B, Tomczak P, et al. Axitinib versus sorafenib as second-line treatment for advanced renal cell carcinoma: overall survival analysis and updated results from a randomised phase 3 trial. Lancet Oncol. 2013;14:552–62.
Albiges L, Schmidinger M, Taguieva-Pioger N et al. CaboPoint: a phase II study of cabozantinib as second-line treatment in patients with metastatic renal cell carcinoma. Future Oncol 2022; 18: 915-926. Ongoing trial investigating cabozantinb in the second line setting.
Albiges L, Powles T, Sharma A, et al. CaboPoint: Interim results from a phase 2 study of cabozantinib after checkpoint inhibitor (CPI) therapy in patients with advanced renal cell carcinoma (RCC). J Clin Oncol. 2023;41:606–606. Interim analysis of the CaboPoint presented at the ASCO GU 2023.
Tannir NM, Agarwal N, Porta C, et al. Efficacy and safety of telaglenastat plus cabozantinib vs placebo plus cabozantinib in patients with advanced renal cell carcinoma: The CANTATA randomized clinical trial. JAMA Oncol. 2022;8:1411–8.
Pal SK, Albiges L, Tomczak P, et al. Atezolizumab plus cabozantinib versus cabozantinib monotherapy for patients with renal cell carcinoma after progression with previous immune checkpoint inhibitor treatment (CONTACT-03): a multicentre, randomised, open-label, phase 3 trial. Lancet. 2023;402:185–95. Important negative trial showing atezolizumab plus cabozantinib after disease progression of prior ICI did not provide improved efficacy compared to cabozantinib.
Pal SK, Escudier BJ, Atkins MB, et al. Final overall survival results from a phase 3 study to compare tivozanib to sorafenib as third- or fourth-line therapy in subjects with metastatic renal cell carcinoma. Eur Urol. 2020;78:783–5. Long-term follow-up of the Tivo3 study in the refractory RCC setting.
Gul A, Stewart TF, Mantia CM, et al. Salvage ipilimumab and nivolumab in patients with metastatic renal cell carcinoma after prior immune checkpoint inhibitors. J Clin Oncol. 2020;38:3088–94.
Ravi P, Mantia C, Su C, et al. Evaluation of the safety and efficacy of immunotherapy rechallenge in patients with renal cell carcinoma. JAMA Oncol. 2020;6:1606–10.
McKay RR, McGregor BA, Xie W, et al. Optimized management of nivolumab and ipilimumab in advanced renal cell carcinoma: a response-based phase II study (OMNIVORE). J Clin Oncol. 2020;38:4240–8.
Grimm MO, Esteban E, Barthélémy P, et al. Efficacy of nivolumab/ipilimumab in patients with initial or late progression with nivolumab: updated analysis of a tailored approach in advanced renal cell carcinoma (TITAN-RCC). J Clin Oncol. 2021;39:4576–4576.
Choueiri TK, Kluger H, George S, et al. FRACTION-RCC: nivolumab plus ipilimumab for advanced renal cell carcinoma after progression on immuno-oncology therapy. J Immunother Cancer. 2022;10:e005445. This trial investigated ipilimumab/nivoluamb in the second-line setting which showed modest activity
Lee CH, Shah AY, Rasco D, et al. Lenvatinib plus pembrolizumab in patients with either treatment-naive or previously treated metastatic renal cell carcinoma (Study 111/KEYNOTE-146): a phase 1b/2 study. Lancet Oncol. 2021;22:946–58. This single-arm study demonstrated the efficacy of pembrolizumab/lenvatinib in the second-line setting.
Choueiri T, Albiges L, Hammers HJ, et al. TiNivo-2: A phase 3, randomized, controlled, multicenter, open-label study to compare tivozanib in combination with nivolumab to tivozanib monotherapy in subjects with renal cell carcinoma who have progressed following one or two lines of therapy where one line has an immune checkpoint inhibitor. J Clin Oncol. 2022;40:TPS405. Trial-in-Progress abstract of the ongoing TiNivo-2 study.
Flanigan RC, Salmon SE, Blumenstein BA, et al. Nephrectomy followed by interferon alfa-2b compared with interferon alfa-2b alone for metastatic renal-cell cancer. N Engl J Med. 2001;345:1655–9.
Mickisch GH, Garin A, van Poppel H, et al. Radical nephrectomy plus interferon-alfa-based immunotherapy compared with interferon alfa alone in metastatic renal-cell carcinoma: a randomised trial. Lancet. 2001;358:966–70.
Hanna N, Sun M, Meyer CP, et al. Survival analyses of patients with metastatic renal cancer treated with targeted therapy with or without cytoreductive nephrectomy: a national cancer data base study. J Clin Oncol. 2016;34:3267–75.
Mejean A, Ravaud A, Thezenas S, et al. Sunitinib alone or after nephrectomy in metastatic renal-cell carcinoma. N Engl J Med. 2018;379:417–27.
Bell H, Cotta BH, Salami SS, et al. “PROBE”ing the role of cytoreductive nephrectomy in advanced renal cancer. Kidney Cancer J. 2022;6:3–9.
Meza L, Chawla NS, Giannarini G, Pal SK. Cytoreductive nephrectomy in 2021: Obsolete. Eur Urol Open Sci. 2022;36:44–6.
Ning S, Trisler K, Wessels BW, Knox SJ. Radiobiologic studies of radioimmunotherapy and external beam radiotherapy in vitro and in vivo in human renal cell carcinoma xenografts. Cancer. 1997;80:2519–28.
Hao C, Liu J, Ladbury C, et al. Stereotactic body radiation therapy to the kidney for metastatic renal cell carcinoma: a narrative review of an emerging concept. Cancer Treat Res Commun. 2023;35:100692.
Ponsky L, Lo SS, Zhang Y, et al. Phase I dose-escalation study of stereotactic body radiotherapy (SBRT) for poor surgical candidates with localized renal cell carcinoma. Radiother Oncol. 2015;117:183–7.
Sun MR, Brook A, Powell MF, et al. Effect of stereotactic body radiotherapy on the growth kinetics and enhancement pattern of primary renal tumors. AJR Am J Roentgenol. 2016;206:544–53.
Correa RJM, Louie AV, Zaorsky NG, et al. The emerging role of stereotactic ablative radiotherapy for primary renal cell carcinoma: a systematic review and meta-analysis. Eur Urol Focus. 2019;5:958–69.
Miljanic M, Montalvo S, Aliru M et al. The evolving interplay of SBRT and the immune system, along with future directions in the field. Cancers (Basel) 2022; 14.
Chow J, Hoffend NC, Abrams SI, et al. Radiation induces dynamic changes to the T cell repertoire in renal cell carcinoma patients. Proc Natl Acad Sci U S A. 2020;117:23721–9.
Zhang S, Zhang E, Long J, et al. Immune infiltration in renal cell carcinoma. Cancer Sci. 2019;110:1564–72.
Hall W, Karrison T, McGregor B et al. NRG-GU012: Randomized phase II stereotactic ablative radiation therapy (SABR) for patients with metastatic unresected renal cell carcinoma (RCC) receiving immunotherapy (SAMURAI). J Clin Oncol 2023; 41: abstr TPS4604. Trial-in-Progress abstract of the ongoing SAMURI study.
Lalani A, Swaminath A, Pond G et al. Phase II trial of cytoreductive stereotactic hypofractionated radiotherapy with combination ipilimumab/nivolumab for metastatic kidney cancer (CYTOSHRINK). J Clin Oncol 2023; 41: abstr TPS750.
Dason S, Lacuna K, Hannan R, et al. State of the art: multidisciplinary management of oligometastatic renal cell carcinoma. Am Soc Clin Oncol Educ Book. 2023;43:e390038.
Rathmell WK, Rumble RB, Van Veldhuizen PJ, et al. Management of metastatic clear cell renal cell carcinoma: ASCO guideline. J Clin Oncol. 2022;40:2957–95.
Christensen M, Hannan R. The emerging role of radiation therapy in renal cell carcinoma. Cancers (Basel). 2022;14:4693.
Tang C, Msaouel P, Hara K, et al. Definitive radiotherapy in lieu of systemic therapy for oligometastatic renal cell carcinoma: a single-arm, single-centre, feasibility, phase 2 trial. Lancet Oncol. 2021;22:1732–9. Important trial showing the efficacy of definiteive radiation in oligometastatic RCC.
Hannan R, Christensen M, Christie A, et al. Stereotactic ablative radiation for systemic therapy-naïve oligometastatic kidney cancer. Eur Urol Oncol. 2022;5:695–703. Important study showing the efficacy of stereotactic ablative radiation in treatment-naive oligometastatic RCC.
Siva S, Bressel M, Wood ST, et al. Stereotactic radiotherapy and short-course pembrolizumab for oligometastatic renal cell carcinoma—the RAPPORT trial. Eur Urol. 2022;81:364–72.
John A, Spain L, Hamid AA. Navigating the current landscape of non-clear cell renal cell carcinoma: a review of the literature. Curr Oncol. 2023;30:923–37.
Albiges L, Guegan J, Le Formal A, et al. MET is a potential target across all papillary renal cell carcinomas: result from a large molecular study of pRCC with CGH array and matching gene expression array. Clin Cancer Res. 2014;20:3411–21.
Atkins MB, Jegede OA, Haas NB et al. Phase II study of nivolumab and salvage nivolumab/ipilimumab in treatment-naïve patients with advanced non-clear cell renal cell carcinoma (HCRN GU16-260-Cohort B). J Immunother Cancer 2023; 11.
Vogelzang NJ, Olsen MR, McFarlane JJ, et al. Safety and efficacy of nivolumab in patients with advanced non-clear cell renal cell carcinoma: results from the phase IIIb/IV CheckMate 374 study. Clin Genitourin Cancer. 2020;18:461-468.e463.
McDermott DF, Lee JL, Ziobro M, et al. Open-label, single-arm, phase II study of pembrolizumab monotherapy as first-line therapy in patients with advanced non-clear cell renal cell carcinoma. J Clin Oncol. 2021;39:1029–39. Important single-arm study of pembrolizumab monotherapy in nccRCC.
Tykodi SS, Gordan LN, Alter RS et al. Safety and efficacy of nivolumab plus ipilimumab in patients with advanced non-clear cell renal cell carcinoma: results from the phase 3b/4 CheckMate 920 trial. J Immunother Cancer 2022; 10.
McGregor BA, McKay RR, Braun DA, et al. Results of a multicenter phase II study of atezolizumab and bevacizumab for patients with metastatic renal cell carcinoma with variant histology and/or sarcomatoid features. J Clin Oncol. 2020;38:63–70.
Lee CH, Voss MH, Carlo MI, et al. Phase II trial of cabozantinib plus nivolumab in patients with non-clear-cell renal cell carcinoma and genomic correlates. J Clin Oncol. 2022;40:2333–41.
Albiges L, Gurney H, Atduev V, et al. Pembrolizumab plus lenvatinib as first-line therapy for advanced non-clear-cell renal cell carcinoma (KEYNOTE-B61): a single-arm, multicentre, phase 2 trial. Lancet Oncol. 2023;24:881–91. Important study showing the efficacy of pembrolizumab/lenvatinib in advanced non-clear cell RCC.
Author information
Authors and Affiliations
Contributions
Yu-Wei Chen, Luke Wang, Justine Panian and Rana McKay drafted the initial manuscript text. Sohail Dhanji, Ithaar Derweesh, Brent Rose, and Aditya Bagrodia critically reviewed and edited the draft. All authors of this manuscript have reviewed and approved the final version submitted
Corresponding author
Ethics declarations
Conflict of Interest
Yu-Wei Chen has an immediate family member who has been employed by Amgen and owned stock. Luke Wang reported no conflict of interest. Justine Panian reported no conflict of interest. Sohail Dhanji reported no conflict of interest. Ithaar Deerweesh reported no conflict of interest. Brent Rose reported no conflict of interest. Aditya Bagrodia reported no conflict of interest. Rana R McKay has served on the consulting/advisory board for Aveo, AstraZeneca, Bayer, Bristol Myers Squib, Blue Earth Diagnostics, Calithera, Caris, Denderon, Exelixis, Janssen, Merck, Myovant, Pfizer, Sanofi, SeaGen, Sorrento Therapeutics, Tempus and has received Institutional Research Funding from AstraZeneca, BMS, Exelixis, Artera, Oncternal, Bayer, Tempus.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chen, YW., Wang, L., Panian, J. et al. Treatment Landscape of Renal Cell Carcinoma. Curr. Treat. Options in Oncol. 24, 1889–1916 (2023). https://doi.org/10.1007/s11864-023-01161-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11864-023-01161-5