Opinion statement
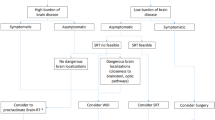
Management of non-small cell lung cancer (NSCLC) with brain metastasis (BrM) has been revolutionized by identification of molecular subsets that have targetable oncogenes. Historically, survival for NSCLC with symptomatic BrM was weeks to months. Now, many patients are surviving years with limited data to guide treatment decisions. Tumors with activating mutations in epidermal growth factor receptor (EGFRact+) have a higher incidence of BrM, but a longer overall survival. The high response rate of both systemic and BrM EGFRact+ NSCLC to tyrosine kinase inhibitors (TKIs) has led to the rapid incorporation of new therapies but is outpacing evidence-based decisions for BrM in NSCLC. While whole brain radiation therapy (WBRT) was the foundation of management of BrM, extended survival raises concerns for the subacute and late effects radiotherapy. We favor the use of TKIs and delaying the use of WBRT when able. At inevitable disease progression, we consider alternative dosing schedules to increase CNS penetration (such as pulse dosing of erlotinib) or advance to next generation TKI if available. We utilize local control options of surgery or stereotactic radiosurgery (SRS) for symptomatic accessible lesions based on size and edema. At progression despite available TKIs, we use pemetrexed-based platinum doublet chemotherapy or immunotherapy if the tumor has high expression of PDL-1. We reserve the use of WBRT for patients with more than 10 BrM and progression despite TKI and conventional chemotherapy, if performance status is appropriate.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Metastatic lung cancer remains a devastating diagnosis, due in part to the high incidence of brain involvement; however, advances in targeted therapy are prolonging survival [1••]. Lung cancer with brain metastasis (BrM) remains an incurable disease and the goals of care are optimizing quality of life (QOL) and maximizing duration of disease control. Unfortunately, given the toxicity of many treatments, the presence of neurologic symptoms limited the therapies that could be offered to patients. However, the availability of more tolerable and effective agents is changing the historical approach to BrM.
The treatment of non-small cell lung cancer (NSCLC), which accounts for 85% of lung cancer diagnosis, is being transformed by the identification of oncogenic driver mutations [2•]. Mutations are present in 60% of adenocarcinomas and the current standard of care is to evaluate molecular markers, particularly mutations in epidermal growth factor receptors (EGFR), in advanced disease. There is expanding evidence that these are unique tumors in regard to prognosis, incidence of metastases, and treatment response. While lower incidence, there are other clinically applicable driver mutations that have targeted therapies, including ALK, ROS-1, BRAF, MEF, and RET-1, that will not be addressed in this paper as it is uncommon for patients to express more than one driver mutation [3].
The feedback loop from bench to bedside has perhaps never been as productive as with EGFR in NSCLC. High expression of EGFR has been recognized in multiple malignancies with significant expression in lung cancer with BrM [4, 5]. Small molecules, tyrosine kinase inhibitors (TKIs) were developed to target these receptors. A subpopulation of Asian, female, non-smokers with adenocarcinoma had a striking sustained response rate (RR). Evaluation of EGFR genotype in the highly responsive subpopulation lead to identification of multiple mutations in the activating domain of EGFR (EGFRact+). These mutations have higher affinity for first generation TKIs than wildtype EGFR (EGFRwt) [6, 7]. With increased screening for EGFRact+ in NSCLC, it is clear that the phenotype of Asian, non-smoking women with adenocarcinoma only accounts for about 60% of patients. Overall frequency of EGFRact+ in Europe is 15% and 22% in North America [8•]. Up to 25% patients with EGFRact+ NSCLC are current smokers [9]. NSCLC expressing EGFRact+ are distinct with a higher incidence of BrM, greater overall survival and possibly increased response to radiotherapy [10]. Within the EGFRact+ mutations, retrospective studies have also suggested that specific mutations may be both predictive and prognostic marker for better outcome [11].
Despite changes in the treatment of systemic NSCLC, recommendations for management of BrM are based on mixed populations of solid tumors. While there is limited evidence to support whole brain radiation (WBRT) compared to best supportive care, it has been the foundation of management in patients with multiple BrM for many decades. Given advancements in systemic therapy as well as radiosurgery (SRS), the late cognitive effects associated with WBRT is of increasing significance on QOL [12•]. Additionally, the tolerability of TKIs enables these agents to be offered to most patients regardless of performance status, expanding the populations eligible for subsequent local therapy.
There remain multiple unanswered questions in the management of BrM in EGFRact+ NSCLC. This paper reflects our current practice based on the evidence available. The development of new therapies and ongoing clinical trials examining the combination of local and systemic therapies will continue to transform the management of BrM in EGFRact+ NSCLC in the coming years.
Systemic therapy
Traditionally, systemic therapy had a limited role in the management of BrM, largely due to limitations in blood-brain barrier (BBB) permeability as well as the risk of toxicity to surrounding healthy brain tissue. Advances in conventional chemotherapy as well as TKIs are changing the management of BrM. TKIs are first line therapy for advanced systemic EGFRact+ NSCLC and given tolerability and rapid action of these agents, we offer these medications to all EGFRact+ NSCLC patients regardless of performance status. We carefully monitor for CNS response and progression with MRIs. In our experience, response to these agents enables subsequent therapies that would not otherwise be tolerated. Platinum doublet chemotherapy utilizing pemetrexed is reserved for disease refractory to TKIs. We typically reserve immunotherapy until progression despite conventional chemotherapy, unless there is high tumor expression of PDL-1. We utilize bevacizumab (BEV) for the management of steroid refractory cerebral edema as well as radiation necrosis; recognizing it may also have an oncolytic effect.
EGFR tyrosine kinase inhibitors
Consideration of current use of EGFR TKIs requires greater understanding of their brief and transformative history. When initially studied, TKIs had less than 20% RR in an unselected population. Subsequent evaluation of tumor genomics lead to the identification of driver mutations in EGFR (EGFRact+) [6, 7]. Driver mutations are genetic alterations found within a tumor that result in constitutively active forms of signaling proteins and lead to sustained tumorgenesis. The most common EGFR activating mutations are deletions of exon 19 (exon19del) and point mutations of exon 21 (L858R) [13]. On exon 20, T790M is a resistance mutation that is seen in TKI naïve patients and in 60% of patients who develop resistance to TKIs [14]. This has led to a third generation of TKIs specifically targeting T790M. While there is data to support lower rates of CNS progression in EGFRact+ NSCLC treated with TKI compared to conventional chemotherapy, the brain is a frequent site of disease recurrence after an initial response to TKIs [15, 16]. Currently available agents were not designed for BBB penetration; however, there are multiple agents in the pipeline designed for increased CNS penetration.
The use of TKIs in patients with BrM is expanding without randomized trials to guide treatment strategies (Table 1). As with most early clinical trials, patients with active BrM were largely excluded from the initial trials of TKIs. The currently available studies are limited in that they are small and predominately single arm or retrospective studies with variable evaluation for EGFRact+. While CNS concentrations of all currently available agents are lower than plasma, CNS disease in EGFRact+ patients have high RR to TKIs. There are ongoing clinical trials to specifically evaluate the use of these agents in patients with BrM and active CNS disease as well as evaluations of new agents designed specifically for increased BBB penetration.
First and second generation TKIs
Gefitinib, a first generation TKI, has CSF concentration approximately 1% of serum; however, the concentration may increase with WBRT [17, 18]. The first prospective trial of gefitinib in NSCLC with BrM was conducted in Italy and had a low RR; however, they did find that patients who had previously received WBRT, had better disease control compared to radiation naïve patients [19]. As with all early studies, patients were not molecularly selected for EGFRact+ and gefitinib did not demonstrate a survival benefit [20]. While not molecularly selected, studies conducted in Asian countries enrolling predominately adenocarcinoma had high RR (60% in a Japanese study that had prior radiotherapy and 81% in a Chinese study treated in combination with WBRT) [21, 22]. Subsequent studies in EGFRact+ patients have demonstrated a RR of 87.8% as monotherapy with overall survival (OS) 21.9 months [23••]. Gefitinib is the most common first line TKI in Asian countries and retrospective studies of EGFRact+ enriched populations have supported the use of TKIs as monotherapy without radiation [24, 25•, 26].
Erlotinib is a first generation TKI that is more commonly used in the USA due in part to sustained FDA approval and increased CSF penetration (approximately 5% of serum in patients with BrM which is above the minimum inhibitory concentration) [27,28,29]. Early prospective trials failed to demonstrate a survival benefit with the addition of erlotinib to radiotherapy in patients with BrM; however, these trials did not screen for EGFRact+ [30,31,32, 33•]. A subsequent study with a small percentage of patients evaluated for EGFRact+ confirmed CNS response varied by genotype; EGFRwt patients survived 11.8 months; however, OS in EGFRact+ patients was 19.1 months [34]. Current dosing of erlotinib at 150 mg daily is based on inhibition of EGFRwt; however, mathematical modeling suggested pulse dosing strategy could delay development of resistance and CNS progression in EGFRact+ [35]. In 2011, retrospective case series of patients treated with weekly high-dose erlotinib supported a partial CNS response in six of nine patients [36]. Recently, an open-label study of 34 patients treated with a pulse of high-dose erlotinib for 2 days a week and otherwise 50 mg daily [37•]. While this did not prevent the development of T790M resistance, all patients with BrM had intracranial response and no patients with disease progression developed new BrM [37•]. This dosing strategy still needs to be studied in a randomized trial; however, it provides an additional treatment option for those patients with isolated intracranial disease progression. When considering dosing of erlotinib, it is also important to note that smoking decreases the bioavailability of erlotinib [9].
Icotinib, another first-generation TKI, is approved for use in China and has CSF concentration approximately 1% of serum that fluctuates with radiotherapy [38]. Dose escalation studies in combination with WBRT have confirmed safety and RR of 80% in a small phase II of 20 patients (at least 50% with EGFRact+) [39]. There are multiple ongoing trials further examining this agent in combination with radiotherapy for BrM (NCT01926171, NCT02726568, NCT01724801).
Afatinib, a second generation TKI, is unique as an irreversible inhibitor of EGFRact+, EGFRwt, Erb-2, and Erb-4. Likely secondary to its effects on EGFRwt, this agent is associated with greater toxicity; however, dose reduction in the first 6 months due to adverse events was not associated with decreased in progression-free survival (PFS) [40]. Subgroup analysis of LUX-Lung 3 and 6 confirmed CNS activity of this agent and superiority to conventional chemotherapy with increased intracranial PFS if patients had prior WBRT [41]. There is also a case study of five patients who declined WBRT and had complete intracranial response to afatinib [42].
While trials directly comparing first generation TKIs with BrM are ongoing (NCT2714010), retrospective analysis does not support significant survival difference between erlotinib and gefitinib [43,44,45]. LUX-Lung 7, a prospective comparison of afatinib to gefitinib did support improved time to treatment failure for the use of afatinib over gefitinib; however, there was no difference for 15% patients with asymptomatic BrM [46].
At the time of progression, there is a lack of prospective data to support transitioning between first and second generation TKIs. Current guidelines recommend re-biopsy or cell-free DNA testing at clinically significant disease progression to evaluate for T790M resistance which would guide transitioning to a third-generation TKI. The LUX-Lung 4 study prospectively evaluated transitioning to afatinib in patients progressing on a first-generation TKI and found a response rate of only 8.2%; however, this study excluded patients with active CNS disease [47]. There are reports of intracranial response to erlotinib after progressing on gefitinib [23••, 44, 48] and afatinib [49]. But, there are also retrospective studies of patients with active CNS disease, both of brain metastases and leptomeningeal disease, who progressed on prior treatments with erlotinib or gefitinib but had intracranial response to afatinib [50]. Additionally, there have been reports of patients responding to erlotinib even after development of the T790M [51, 52]. We utilized pulse dosing for isolated CNS progression, as there is evidence that T790M mutations are less common in BrM during pharmacokinetic failure than in systemic disease [51]. At systemic disease progression with identification of T790M resistance mutation, we transition to third-generation TKIs.
Third-generation TKIs
In 60% of cases, the development of resistance to a first- or second-generation TKI is due to the acquired point mutation T790M. This mutation is in the ATP binding pocket and prevents inhibition by first- and second-generations TKIs. Osimertinib is a potent irreversible inhibitor of T790M that demonstrated a response rate of over 60% in patients with T790M in early trials leading to the breakthrough designation. Supporting use of osimertinib over conventional chemotherapy, the AURA3 trial demonstrated an impressive PFS of 10.1 months for osimertinib compared to 4.4 months for pemetrexed containing platinum doublet chemotherapy [53••]. This PFS benefit was true even for the over 30% of patients with asymptomatic BrM at enrollment with a hazard ratio of 0.32 [53••]. Intracranial response has also been reported in patients with BrM as well as patients with leptomeningeal disease [54,55,56]. For patients with T790M, either primary or secondary, we favor the use of osimertinib for the use of EGFRact+ BrM.
Future agents
There are multiple TKIs in early clinical phases that are focusing on increased CNS penetration [57•]. One example, the ongoing phase I study of AZD3759, reported preliminary data that 11 of 21 patients had intracranial response [58]. Other ongoing clinical trials of new TKIs in NSCLC with BrM including tesevatinib (NCT02616393) and ASP 8273 (NCT02113813).
Platinum doublet chemotherapy
Conventional chemotherapy was thought to have a limited role in the treatment of BrM due to concerns about BBB penetration. While not equal to serum, pemetrexed, an antifolate chemotherapy, has CSF concentration only 2% lower than plasma [59]. Systemic RR are similar or lower than intracranial RR in a phase II trials with delayed or concurrent WBRT [60, 61]. Additionally, retrospective analysis found lower rate of symptomatic BrM in NSCLC patients treated with pemetrexed either in first or second line therapy [62]. For patients with advanced adenocarcinoma NSCLC with non-operable asymptomatic BrM, pemetrexed had similar intracranial and extracranial response of 80 and 70%, respectively [63]. While there was limited inclusion of patients with BrM in the large phase III trials, pemetrexed maintenance was shown to improve survival [64]. Based on data from IMPRESS trial, continuing TKI with conventional chemotherapy is not recommended [65]. There are multiple phase III trials to evaluate dose of pemetrexed and use in combination with radiotherapy and TKIs (NCT02284490, NCT02162537, NCT01951469). In patients with non-squamous NSCLC who do not respond to TKIs or at recurrence after osimertinib, platinum doublet chemotherapy of pemetrexed with carboplatin for four to six cycles is recommended for patients with performance status of 0–2. After completion of six cycles, or if side effects prevent further cycles, we utilize pemetrexed as maintenance therapy.
Immunotherapy
The three immune checkpoint inhibitors approved for use in NSCLC, nivolumab, pembrolizumab, and atezolizumab, have also revolutionized the treatment of NSCLC [66]. Preclinical work supports T cell exhaustion and decreased PDL-1 expression on EGFRact+ tumors [67]. Given the high RR of EGFRact+ tumors to TKIs, clinical trials of checkpoint inhibitors have excluded EGFRact+ patients, as well as patients with active CNS disease. Given these limitations, the use of immunotherapy in EGFRact+ NSCLC with BrM is limited to case series and small trials that have demonstrated efficacy [68••], although also with significant neurologic side effects [69]. There are ongoing trials combining immunotherapy with TKIs in EGFRact+ NSCLC (NCT02085070). At this time, checkpoint inhibitors are reserved for use after TKIs and usually not until progression on conventional chemotherapy unless there is high expression of PDL-1.
Antiangiogenic therapy
Bevacizumab (BEV) has demonstrated a survival benefit in combination with platinum doublet chemotherapy in non-squamous NSCLC, although these trials excluded patients with known CNS metastasis given concerns for intracranial hemorrhage [70]. Subsequently, the safety of the addition of BEV in patients with non-squamous NSCLC BrM, even in the setting of full anticoagulation, has been demonstrated [71•]. For this reason, addition of BEV to platinum doublet chemotherapy is recommended in non-squamous NSCLC. While it excluded patients with BrM, an open-label phase II study comparing the addition of BEV to erlotinib in first line therapy demonstrated a PFS benefit compared to erlotinib alone; survival data has not matured and a phase III study is ongoing [72]. At this time, the use of BEV in treatment of BrM is primarily in the management of steroid refractory vasogenic edema and for the management of radiation necrosis with recognition that there may be a benefit to tumor control as well.
Local therapy
Surgery
The survival and QOL benefits of surgery for treatment of a single symptomatic BrM are based on randomized trials from the 1990s with a population of primarily lung cancer patients. These trials were randomized to surgical resection and WBRT or WBRT alone and found not only a survival benefit to the surgical group, but also benefit in functionally independent survival [73, 74]. While a more recent retrospective study of patients with BrM at initial diagnosis of NSCLC did not demonstrate a survival benefit to surgery, surgery did improve QOL when presenting with neurologic symptoms [75]. Advances in neurosurgical techniques allow access to more lesions with low surgical complications and morbidity of only 1.8% at high volume centers [76]. Given the response of BrM to radiotherapy and systemic therapies, we reserve surgery for large (greater than 3 cm), symptomatic, accessible BrM or if additional histologic diagnosis is required.
Radiotherapy
Radiotherapy has been the foundation of treatment of solid tumor BrM for decades; however, the type and timing of radiotherapy remains highly variable in clinical practice. Given EGFRact+ is a positive prognostic factor with high RR to TKIs, we typically reserve the use of radiotherapy until after TKI response can be evaluated. The clinical evidence to support this decision is limited to multiple small studies of TKIs or conventional chemotherapy as monotherapy (Table 2). These studies have supported the use of systemic therapies to delay radiation therapy from 12.6 to 17.9 months [25•, 48, 77••]. A recently reported retrospective study suggests increased survival with combination of up-front SRS and TKI compared to salvage strategy [78••]. Review of this literature provides a foundation for our practice of delaying WBRT to evaluate for response to systemic agents.
Whole brain radiation therapy
Due to limited CNS penetration of older systemic therapies, WBRT, with or without surgery, was the cornerstone of management of BrM, based on evidence that patients were less likely to die of neurologic causes despite a lack of survival benefit [79]. Multiple studies evaluating the safety of chemotherapy in conjunction with WBRT demonstrated improved CNS control; however, there was no improvement in OS. No survival benefit has been demonstrated when comparing early WBRT to delayed following conventional chemotherapy [80]. Small studies examining the use of TKIs and WBRT have provided conflicting results and it remains unclear if addition of TKI to radiotherapy improved survival [81] or could possibly have deleterious effects [82]. In contrast, clinical trials have reported that patients were limited in receiving subsequent systemic treatment due to deteriorations in performance status after WBRT [26]. Meta-analysis also confirms more side effects with radiotherapy compared to TKIs alone [83•].
The benefits of radiation therapy must be weighed with not only the short-term side effects, but given survival of years for many patients with EGFRact+ NSCLC, the subacute and long-term cognitive effects of radiation [12]. For patients with poor functional status, WBRT has no significant survival or QOL benefit compared to best supportive care [84••]. Applications of these studies to the EGFRact+ NSCLC population are limited and there are multiple ongoing studies evaluating the use of WBRT in combination with TKIs [85]. We reserve WBRT for patients who have intracranial progression refractory to all systemic therapies that are not candidates for surgery or SRS, if performance status permits.
Stereotactic radiosurgery
SRS provides high-dose radiation to the target while minimizing exposure to surrounding normal brain tissue. The number of BrM that can be treated with SRS is expanding with a recent trial confirming non-inferiority with SRS for up to 10 metastases compared to WBRT [86]. The use of SRS is limited based on location and size of lesions as well as degree of vasogenic edema, so that it is primarily offered to patients with only a few, small BrM (<3 cm given decline in local control) [87].
Initially, clinical trials evaluated the addition of SRS to WBRT and found improved survival only for patients with a single BrM, but improved performance status of all patients [88]. Subsequent retrospective studies had mixed findings with some demonstrating improved CNS control however no improvement in OS and others actually finding that SRS following WBRT decreased survival [89, 90]. Recent post hoc analysis of the EORTC 22952 trial failed to find a benefit to adjuvant WBRT [91]. Additionally, combination SRS and WBRT has a significant impact on learning and memory at 4 months compared to SRS alone [92]. For these reasons, clinical practice has moved towards the use of SRS alone.
There are multiple hypotheses suggesting that radiation can increase the efficacy of TKIs possibly by improving BBB penetration or radiosensitizing the tumors with TKIs [93, 94]. There was a small phase III study that did not find a survival benefit to up-front SRS compared to conventional chemotherapy; however, this trial was closed early due to the approval of TKIs [77••]. Phase II and retrospective studies have supported the use of TKIs as monotherapy to delay radiation therapy, although these studies were primarily with WBRT or mixture of radiotherapy (Table 2). Retrospective studies of the use of up-front SRS with TKI support a survival benefit over the use of TKI monotherapy with salvage radiotherapy [78••, 95, 96]. A devastating long-term effect of radiation, leukoencephalopathy, radiographically presents as diffuse periventricular white matter changes [97]. The rate of leukoencephalopathy following SRS is lower than WBRT at all time points but is up to 84% at 4 years [98••]. Recognizing the risk of radiation, at this time, we favor the use of SRS in combination with TKIs for BrM <3 cm given appropriate performance status.
Management of subacute and late neurologic complications of radiotherapy
Radiation necrosis clinically presents with general and neurologic decline due to brain edema surrounding a growing necrotic core. In other brain tumor populations, radiation necrosis has been associated with similar survival as recurrent disease. Steroids are used as first line management of radiation necrosis. However, if there is no significant improvement with steroids, we transition to management with BEV utilizing a standard 6-week protocol [99].
Cognitive impairment can be seen as a result of radiation therapy with variable reversibility. Acute cognitive complaints within 1 month of radiation are most commonly related to fatigue or vasogenic cerebral edema and can be managed conservatively. Cognitive slowing, executive dysfunction, and short-term memory deficits seen in the 1 to 6 months following radiotherapy may resolve with time and lifestyle modification. There is limited data that memantine, an NMDA partial antagonist, hyperbaric oxygen and hippocampal sparing WBRT may prevent this impairment [100,101,102].
Late cognitive impairment, leukoencephalopathy, increases as a function of time following both SRS and WBRT [98]. These changes are irreversible and associated with both demyelinating and cerebrovascular pathology. For these reasons, it is more common in patients over the age of 70 with vascular disease or collagen disorders. This has been seen more commonly in WBRT and clinically is a driving force for delaying WBRT.
Hypopituitarism develops in virtually all patients with radiotherapy near the pituitary and 20% within 5 years. In long-term survivors, monitoring for pituitary function after radiation therapy is also important.
Emerging therapies
There are multiple ongoing trials as described above to clarify the use of currently available agents. In addition, for further development of TKIs, the National Lung Matrix Trial is using biomarkers to guide targeted drug therapies. The use of irinotecan, etoposide, and ATR kinase inhibitors is also under investigation. When patients progress on TKI and conventional chemotherapy, we encourage offering additional clinical trials to the patients.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
•• Sperduto PW, Yang TJ, Beal K, Pan H, Brown PD, Bangdiwala A, et al. Estimating survival in patients with lung cancer and brain metastases: an update of the graded prognostic assessment for lung cancer using molecular markers (lung-molGPA). JAMA Oncol. 2016; doi:10.1001/jamaoncol.2016.3834. Updated prognositc scale for BrM in lung cancer accounting for mutational status.
• Sholl LM. Biomarkers in lung adenocarcinoma: a decade of progress. Arch Pathol Lab Med. 2015;139(4):469–80. doi:10.5858/arpa.2014-0128-RA. Review of mutations in lung adenocardinoma.
Swanton C, Govindan R. Clinical implications of genomic discoveries in lung cancer. N Engl J Med. 2016;374(19):1864–73. doi:10.1056/NEJMra1504688.
Hendler FJ, Ozanne BW. Human squamous cell lung cancers express increased epidermal growth factor receptors. J Clin Invest. 1984;74(2):647–51. doi:10.1172/jci111463.
Di Carlo A, Mariano A, Coppa A, Macchia V, Maiuri F, Iaconetta G, et al. Epidermal growth factor receptor and tissue tumor markers in human intracranial neoplasms. J Neurosurg Sci. 1990;34(3–4):181–5.
Lynch TJ, Bell DW, Sordella R, Gurubhagavatula S, Okimoto RA, Brannigan BW, et al. Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib. N Engl J Med. 2004;350(21):2129–39. doi:10.1056/NEJMoa040938.
Paez JG, Janne PA, Lee JC, Tracy S, Greulich H, Gabriel S, et al. EGFR mutations in lung cancer: correlation with clinical response to gefitinib therapy. Science. 2004;304(5676):1497–500. doi:10.1126/science.1099314.
• Midha A, Dearden S, McCormack R. EGFR mutation incidence in non-small-cell lung cancer of adenocarcinoma histology: a systematic review and global map by ethnicity (mutMapII). Am J Cancer Res. 2015;5(9):2892–911. EGFRact+ worldwide incidence with maps for mutation frequency as well as reported ranges based on gender and smoking status.
Hughes AN, O’Brien ME, Petty WJ, Chick JB, Rankin E, Woll PJ, et al. Overcoming CYP1A1/1A2 mediated induction of metabolism by escalating erlotinib dose in current smokers. J Clin Oncol. 2009;27(8):1220–6. doi:10.1200/JCO.2008.19.3995.
Eichler AF, Kahle KT, Wang DL, Joshi VA, Willers H, Engelman JA, et al. EGFR mutation status and survival after diagnosis of brain metastasis in nonsmall cell lung cancer. Neuro-Oncology. 2010;12(11):1193–9. doi:10.1093/neuonc/noq076.
Porta R, Sanchez-Torres JM, Paz-Ares L, Massuti B, Reguart N, Mayo C, et al. Brain metastases from lung cancer responding to erlotinib: the importance of EGFR mutation. Eur Respir J. 2011;37(3):624–31. doi:10.1183/09031936.00195609.
• Peters S, Bexelius C, Munk V, Leighl N. The impact of brain metastasis on quality of life, resource utilization and survival in patients with non-small-cell lung cancer. Cancer Treat Rev. 2016;45:139–62. doi:10.1016/j.ctrv.2016.03.009. Systematic review of quality of life and survival in patients with NSCLC.
Shigematsu H, Gazdar AF. Somatic mutations of epidermal growth factor receptor signaling pathway in lung cancers. Int J Cancer. 2006;118(2):257–62. doi:10.1002/ijc.21496.
Sequist LV, Waltman BA, Dias-Santagata D, Digumarthy S, Turke AB, Fidias P, et al. Genotypic and histological evolution of lung cancers acquiring resistance to EGFR inhibitors. Sci Transl Med. 2011;3(75):75ra26. doi:10.1126/scitranslmed.3002003.
Omuro AM, Kris MG, Miller VA, Franceschi E, Shah N, Milton DT, et al. High incidence of disease recurrence in the brain and leptomeninges in patients with nonsmall cell lung carcinoma after response to gefitinib. Cancer. 2005;103(11):2344–8. doi:10.1002/cncr.21033.
Heon S, Yeap BY, Lindeman NI, Joshi VA, Butaney M, Britt GJ, et al. The impact of initial gefitinib or erlotinib versus chemotherapy on central nervous system progression in advanced non-small cell lung cancer with EGFR mutations. Clin Cancer Res. 2012;18(16):4406–14. doi:10.1158/1078-0432.CCR-12-0357.
Zeng YD, Liao H, Qin T, Zhang L, Wei WD, Liang JZ, et al. Blood-brain barrier permeability of gefitinib in patients with brain metastases from non-small-cell lung cancer before and during whole brain radiation therapy. Oncotarget. 2015;6(10):8366–76. doi:10.18632/oncotarget.3187.
Fang L, Sun X, Song Y, Zhang Y, Li F, Xu Y, et al. Whole-brain radiation fails to boost intracerebral gefitinib concentration in patients with brain metastatic non-small cell lung cancer: a self-controlled, pilot study. Cancer Chemother Pharmacol. 2015;76(4):873–7. doi:10.1007/s00280-015-2847-z.
Ceresoli GL, Cappuzzo F, Gregorc V, Bartolini S, Crino L, Villa E. Gefitinib in patients with brain metastases from non-small-cell lung cancer: a prospective trial. Ann Oncol. 2004;15(7):1042–7. doi:10.1093/annonc/mdh276.
Pesce GA, Klingbiel D, Ribi K, Zouhair A, von Moos R, Schlaeppi M, et al. Outcome, quality of life and cognitive function of patients with brain metastases from non-small cell lung cancer treated with whole brain radiotherapy combined with gefitinib or temozolomide. A randomised phase II trial of the Swiss Group for Clinical Cancer Research (SAKK 70/03). Eur J Cancer. 2012;48(3):377–84. doi:10.1016/j.ejca.2011.10.016.
Namba Y, Kijima T, Yokota S, Niinaka M, Kawamura S, Iwasaki T, et al. Gefitinib in patients with brain metastases from non–small-cell lung cancer: review of 15 clinical cases. Clinical Lung Cancer. 2004;6(2):123–8. doi:10.3816/CLC.2004.n.026.
Ma S, Xu Y, Deng Q, Yu X. Treatment of brain metastasis from non-small cell lung cancer with whole brain radiotherapy and gefitinib in a Chinese population. Lung Cancer. 2009;65(2):198–203. doi:10.1016/j.lungcan.2008.10.028.
•• Iuchi T, Shingyoji M, Sakaida T, Hatano K, Nagano O, Itakura M, et al. Phase II trial of gefitinib alone without radiation therapy for Japanese patients with brain metastases from EGFR-mutant lung adenocarcinoma. Lung Cancer. 2013;82(2):282–7. doi:10.1016/j.lungcan.2013.08.016. Trial design of advancing from gefitinib to erlotinib prior to salvage XRT that resulted in delayed XRT 17.9m.
Kim JE, Lee DH, Choi Y, Yoon DH, Kim SW, Suh C, et al. Epidermal growth factor receptor tyrosine kinase inhibitors as a first-line therapy for never-smokers with adenocarcinoma of the lung having asymptomatic synchronous brain metastasis. Lung Cancer. 2009;65(3):351–4. doi:10.1016/j.lungcan.2008.12.011.
• Zhang Q, Zhang X, Yan H, Jiang B, Xu C, Yang J, et al. Effects of epidermal growth factor receptor-tyrosine kinase inhibitors alone on EGFR-mutant non-small cell lung cancer with brain metastasis. Thorac Cancer. 2016;7(6):648–54. doi:10.1111/1759-7714.12379. Retrospective study of upfront TKI and salvage radiotherapy.
Byeon S, Ham JS, Sun JM, Lee SH, Ahn JS, Park K, et al. Analysis of the benefit of sequential cranial radiotherapy in patients with EGFR mutant non-small cell lung cancer and brain metastasis. Med Oncol. 2016;33(8):97. doi:10.1007/s12032-016-0811-3.
Togashi Y, Masago K, Fukudo M, Terada T, Fujita S, Irisa K, et al. Cerebrospinal fluid concentration of erlotinib and its active metabolite OSI-420 in patients with central nervous system metastases of non-small cell lung cancer. J Thorac Oncol. 2010;5(7):950–5. doi:10.1097/JTO.0b013e3181e2138b.
Deng Y, Feng W, Wu J, Chen Z, Tang Y, Zhang H, et al. The concentration of erlotinib in the cerebrospinal fluid of patients with brain metastasis from non-small-cell lung cancer. Mol Clin Oncol. 2014;2(1):116–20. doi:10.3892/mco.2013.190.
Weber B, Winterdahl M, Memon A, Sorensen BS, Keiding S, Sorensen L, et al. Erlotinib accumulation in brain metastases from non-small cell lung cancer: visualization by positron emission tomography in a patient harboring a mutation in the epidermal growth factor receptor. J Thorac Oncol. 2011;6(7):1287–9. doi:10.1097/JTO.0b013e318219ab87.
Olmez I, Donahue BR, Butler JS, Huang Y, Rubin P, Xu Y. Clinical outcomes in extracranial tumor sites and unusual toxicities with concurrent whole brain radiation (WBRT) and erlotinib treatment in patients with non-small cell lung cancer (NSCLC) with brain metastasis. Lung Cancer. 2010;70(2):174–9. doi:10.1016/j.lungcan.2010.01.018.
Sperduto PW, Kased N, Roberge D, Xu Z, Shanley R, Luo X, et al. Summary report on the graded prognostic assessment: an accurate and facile diagnosis-specific tool to estimate survival for patients with brain metastases. J Clin Oncol. 2011;30(4):419–25. doi:10.1200/jco.2011.38.0527.
Lind JS, Lagerwaard FJ, Smit EF, Senan S. Phase I study of concurrent whole brain radiotherapy and erlotinib for multiple brain metastases from non-small-cell lung cancer. Int J Radiat Oncol Biol Phys. 2009;74(5):1391–6. doi:10.1016/j.ijrobp.2008.10.026.
• Lee SM, Lewanski CR, Counsell N, Ottensmeier C, Bates A, Patel N, et al. Randomized trial of erlotinib plus whole-brain radiotherapy for NSCLC patients with multiple brain metastases. J Natl Cancer Inst. 2014;106(7) doi:10.1093/jnci/dju151. Prospective trial with no survival benefit to combination of eroltinib and WBRT in EGFRwt patients.
Welsh JW, Komaki R, Amini A, Munsell MF, Unger W, Allen PK, et al. Phase II trial of erlotinib plus concurrent whole-brain radiation therapy for patients with brain metastases from non-small-cell lung cancer. J Clin Oncol. 2013;31(7):895–902. doi:10.1200/JCO.2011.40.1174.
Chmielecki J, Foo J, Oxnard GR, Hutchinson K, Ohashi K, Somwar R, et al. Optimization of dosing for EGFR-mutant non-small cell lung cancer with evolutionary cancer modeling. Sci Transl Med. 2011;3(90):90ra59. doi:10.1126/scitranslmed.3002356.
Grommes C, Oxnard GR, Kris MG, Miller VA, Pao W, Holodny AI, et al. “Pulsatile” high-dose weekly erlotinib for CNS metastases from EGFR mutant non-small cell lung cancer. Neuro-Oncology. 2011;13(12):1364–9. doi:10.1093/neuonc/nor121.
• Yu HA, Sima C, Feldman D, Liu LL, Vaitheesvaran B, Cross J, et al. Phase 1 study of twice weekly pulse dose and daily low-dose erlotinib as initial treatment for patients with EGFR-mutant lung cancers. Ann Oncol. 2016; doi:10.1093/annonc/mdw556. Phase I pulse dosing of erlotinib with BrM response and no CNS progression.
Zhou L, He J, Xiong W, Liu Y, Xiang J, Yu Q, et al. Impact of whole brain radiation therapy on CSF penetration ability of icotinib in EGFR-mutated non-small cell lung cancer patients with brain metastases: results of phase I dose-escalation study. Lung Cancer. 2016;96:93–100. doi:10.1016/j.lungcan.2016.04.003.
Fan Y, Huang Z, Fang L, Miao L, Gong L, Yu H, et al. A phase II study of icotinib and whole-brain radiotherapy in Chinese patients with brain metastases from non-small cell lung cancer. Cancer Chemother Pharmacol. 2015;76(3):517–23. doi:10.1007/s00280-015-2760-5.
Yang JC, Sequist LV, Zhou C, Schuler M, Geater SL, Mok T, et al. Effect of dose adjustment on the safety and efficacy of afatinib for EGFR mutation-positive lung adenocarcinoma: post hoc analyses of the randomized LUX-Lung 3 and 6 trials. Ann Oncol. 2016; doi:10.1093/annonc/mdw322.
Schuler M, Wu YL, Hirsh V, O’Byrne K, Yamamoto N, Mok T, et al. First-line afatinib versus chemotherapy in patients with non-small cell lung cancer and common epidermal growth factor receptor gene mutations and brain metastases. J Thorac Oncol. 2016;11(3):380–90. doi:10.1016/j.jtho.2015.11.014.
Hochmair M, Holzer S, Burghuber OC. Complete remissions in afatinib-treated non-small-cell lung cancer patients with symptomatic brain metastases. Anti-Cancer Drugs. 2016;27(9):914–5. doi:10.1097/CAD.0000000000000410.
Kashima J, Okuma Y, Miwa M, Hosomi Y. Survival of patients with brain metastases from non-small cell lung cancer harboring EGFR mutations treated with epidermal growth factor receptor tyrosine kinase inhibitors. Med Oncol. 2016;33(11):129. doi:10.1007/s12032-016-0843-8.
Zheng MH, Sun HT, Xu JG, Yang G, Huo LM, Zhang P, et al. Combining whole-brain radiotherapy with gefitinib/erlotinib for brain metastases from non-small-cell lung cancer: a meta-analysis. Biomed Res Int. 2016;2016:5807346. doi:10.1155/2016/5807346.
Park SJ, Kim HT, Lee DH, Kim KP, Kim SW, Suh C, et al. Efficacy of epidermal growth factor receptor tyrosine kinase inhibitors for brain metastasis in non-small cell lung cancer patients harboring either exon 19 or 21 mutation. Lung Cancer. 2012;77(3):556–60. doi:10.1016/j.lungcan.2012.05.092.
Park K, Tan E-H, O’Byrne K, Zhang L, Boyer M, Mok T, et al. Afatinib versus gefitinib as first-line treatment of patients with EGFR mutation-positive non-small-cell lung cancer (LUX-Lung 7): a phase 2B, open-label, randomised controlled trial. Lancet Oncol. 2016;17(5):577–89. doi:10.1016/s1470-2045(16)30033-x.
Katakami N, Atagi S, Goto K, Hida T, Horai T, Inoue A, et al. LUX-Lung 4: a phase II trial of afatinib in patients with advanced non-small-cell lung cancer who progressed during prior treatment with erlotinib, gefitinib, or both. J Clin Oncol. 2013;31(27):3335–41. doi:10.1200/JCO.2012.45.0981.
Katayama T, Shimizu J, Suda K, Onozato R, Fukui T, Ito S, et al. Efficacy of erlotinib for brain and leptomeningeal metastases in patients with lung adenocarcinoma who showed initial good response to gefitinib. J Thorac Oncol. 2009;4(11):1415–9. doi:10.1097/JTO.0b013e3181b62572.
Nonagase Y, Okamoto K, Iwasa T, Yoshida T, Tanaka K, Takeda M, et al. Afatinib-refractory brain metastases from EGFR-mutant non-small-cell lung cancer successfully controlled with erlotinib: a case report. Anti-Cancer Drugs. 2016;27(3):251–3. doi:10.1097/CAD.0000000000000317.
Hoffknecht P, Tufman A, Wehler T, Pelzer T, Wiewrodt R, Schutz M, et al. Efficacy of the irreversible ErbB family blocker afatinib in epidermal growth factor receptor (EGFR) tyrosine kinase inhibitor (TKI)-pretreated non-small-cell lung cancer patients with brain metastases or leptomeningeal disease. J Thorac Oncol. 2015;10(1):156–63. doi:10.1097/JTO.0000000000000380.
Hata A, Katakami N, Yoshioka H, Takeshita J, Tanaka K, Nanjo S, et al. Rebiopsy of non-small cell lung cancer patients with acquired resistance to epidermal growth factor receptor-tyrosine kinase inhibitor: comparison between T790M mutation-positive and mutation-negative populations. Cancer. 2013;119(24):4325–32. doi:10.1002/cncr.28364.
Ohara S, Ushijima T, Gunji M, Tanai C, Tanaka Y, Noda H, et al. Brain metastasis effectively treated with erlotinib following the acquisition of resistance to gefitinib: a case report. J Med Case Rep. 2014;8:64. doi:10.1186/1752-1947-8-64.
Mok TS, Wu YL, Ahn MJ, Garassino MC, Kim HR, Ramalingam SS, et al. Osimertinib or platinum-pemetrexed in EGFR T790M-positive lung cancer. N Engl J Med. 2016; doi:10.1056/NEJMoa1612674. Randomized trial with benefit in PFS for osimertinib compared to conventional chemotherapy in EGFRact+ patients 30% of had asymptomtic BrM.
Reichegger H, Jochum W, Forbs D, Hader C, Fruh M. Rapid intracranial response to osimertinib in a patient with epidermal growth factor receptor T790M-positive adenocarcinoma of the lung. Oncol Res Treat. 2016;39(7–8):461–3. doi:10.1159/000446759.
Ricciuti B, Chiari R, Chiarini P, Crino L, Maiettini D, Ludovini V, et al. Osimertinib (AZD9291) and CNS response in two radiotherapy-naive patients with EGFR-mutant and T790M-positive advanced non-small cell lung cancer. Clin Drug Investig. 2016;36(8):683–6. doi:10.1007/s40261-016-0411-1.
Yang J, Kim DW, Kim SW, Cho BC, Lee J, Ye X, et al., editors. Osimertinib activity in patients with leptomeningeal disease from non-small cell lung cancer: updated results from the BLOOM study. Chicago, IL: ASCO Annual Meeting 2015; 2016.
• Tan CS, Cho BC, Soo RA. Next-generation epidermal growth factor receptor tyrosine kinase inhibitors in epidermal growth factor receptor -mutant non-small cell lung cancer. Lung Cancer. 2016;93:59–68. doi:10.1016/j.lungcan.2016.01.003. Review of currently available and pipline TKIs.
Ahn MJ, Kim DW, Kim TM, Lin C, Ratnayake J, Carlile DJ, et al., editors. Phase I study (BLOOM) of AZD3759, a CNS penetrable EGFR inhibitor, for the treatment of non-small-cell lung cancer (NSCLC) with brain metastasis (BM) and leptomeningeal metastasis (LM). Chicago, IL: ASCO Annual Meeting 2016; 2016.
Stapleton SL, Reid JM, Thompson PA, Ames MM, McGovern RM, McGuffey L, et al. Plasma and cerebrospinal fluid pharmacokinetics of pemetrexed after intravenous administration in non-human primates. Cancer Chemother Pharmacol. 2007;59(4):461–6. doi:10.1007/s00280-006-0285-7.
Dinglin XX, Huang Y, Liu H, Zeng YD, Hou X, Chen LK. Pemetrexed and cisplatin combination with concurrent whole brain radiotherapy in patients with brain metastases of lung adenocarcinoma: a single-arm phase II clinical trial. J Neuro-Oncol. 2013;112(3):461–6. doi:10.1007/s11060-013-1079-5.
Barlesi F, Gervais R, Lena H, Hureaux J, Berard H, Paillotin D, et al. Pemetrexed and cisplatin as first-line chemotherapy for advanced non-small-cell lung cancer (NSCLC) with asymptomatic inoperable brain metastases: a multicenter phase II trial (GFPC 07-01). Ann Oncol. 2011;22(11):2466–70. doi:10.1093/annonc/mdr003.
Ortuzar W, Hanna N, Pennella E, Peng G, Langer C, Monberg M, et al. Brain metastases as the primary site of relapse in two randomized phase III pemetrexed trials in advanced non-small-cell lung cancer. Clin Lung Cancer. 2012;13(1):24–30. doi:10.1016/j.cllc.2011.05.007.
Zhu W, Roe OD, Wu C, Li W, Guo R, Gu Y, et al. Activity of pemetrexed-based regimen as first-line chemotherapy for advanced non-small cell lung cancer with asymptomatic inoperable brain metastasis: a retrospective study. J Chemother. 2015;27(4):221–6. doi:10.1179/1973947815Y.0000000005.
Paz-Ares LG, de Marinis F, Dediu M, Thomas M, Pujol JL, Bidoli P, et al. PARAMOUNT: final overall survival results of the phase III study of maintenance pemetrexed versus placebo immediately after induction treatment with pemetrexed plus cisplatin for advanced nonsquamous non-small-cell lung cancer. J Clin Oncol. 2013;31(23):2895–902. doi:10.1200/JCO.2012.47.1102.
Soria JC, Wu Y-L, Nakagawa K, Kim S-W, Yang J-J, Ahn M-J, et al. Gefitinib plus chemotherapy versus placebo plus chemotherapy in EGFR-mutation-positive non-small-cell lung cancer after progression on first-line gefitinib (IMPRESS): a phase 3 randomised trial. Lancet Oncol. 2015;16(8):990–8. doi:10.1016/s1470-2045(15)00121-7.
Schvartsman G, Ferrarotto R, Massarelli E. Checkpoint inhibitors in lung cancer: latest developments and clinical potential. Ther Adv Med Oncol. 2016;8(6):460–73. doi:10.1177/1758834016661164.
Akbay EA, Koyama S, Carretero J, Altabef A, Tchaicha JH, Christensen CL, et al. Activation of the PD-1 pathway contributes to immune escape in EGFR-driven lung tumors. Cancer Discov. 2013;3(12):1355–63. doi:10.1158/2159-8290.CD-13-0310.
•• Goldberg SB, Gettinger SN, Mahajan A, Chiang AC, Herbst RS, Sznol M, et al. Pembrolizumab for patients with melanoma or non-small-cell lung cancer and untreated brain metastases: early analysis of a non-randomised, open-label, phase 2 trial. Lancet Oncol. 2016;17(7):976–83. doi:10.1016/S1470-2045(16)30053-5. Open label phase 2 of use of checkpoint inhibitor, pembrolizumab in NSCLC with brain metastasis.
Kanai O, Fujita K, Okamura M, Nakatani K, Mio T. Severe exacerbation or manifestation of primary disease related to nivolumab in non-small-cell lung cancer patients with poor performance status or brain metastases. Ann Oncol. 2016; doi:10.1093/annonc/mdw148.
Soria JC, Mauguen A, Reck M, Sandler AB, Saijo N, Johnson DH, et al. Systematic review and meta-analysis of randomised, phase II/III trials adding bevacizumab to platinum-based chemotherapy as first-line treatment in patients with advanced non-small-cell lung cancer. Ann Oncol. 2013;24(1):20–30. doi:10.1093/annonc/mds590.
• Besse B, Le Moulec S, Mazieres J, Senellart H, Barlesi F, Chouaid C, et al. Bevacizumab in patients with nonsquamous non-small cell lung cancer and asymptomatic, untreated brain metastases (BRAIN): a nonrandomized, phase II study. Clin Cancer Res. 2015;21(8):1896–903. doi:10.1158/1078-0432.CCR-14-2082. Phase II study of use of BEV in patients with untreated non-squamous NSCLC BrM.
Seto T, Kato T, Nishio M, Goto K, Atagi S, Hosomi Y, et al. Erlotinib alone or with bevacizumab as first-line therapy in patients with advanced non-squamous non-small-cell lung cancer harbouring EGFR mutations (JO25567): an open-label, randomised, multicentre, phase 2 study. Lancet Oncol. 2014;15(11):1236–44. doi:10.1016/s1470-2045(14)70381-x.
Patchell RA, Tibbs PA, Walsh JW, Dempsey RJ, Maruyama Y, Kryscio RJ, et al. A randomized trial of surgery in the treatment of single metastases to the brain. N Engl J Med. 1990;322(8):494–500. doi:10.1056/nejm199002223220802.
Vecht CJ, Haaxma-Reiche H, Noordijk EM, Padberg GW, Voormolen JH, Hoekstra FH, et al. Treatment of single brain metastasis: radiotherapy alone or combined with neurosurgery? Ann Neurol. 1993;33(6):583–90. doi:10.1002/ana.410330605.
Kim SY, Hong CK, Kim TH, Hong JB, Park CH, Chang YS, et al. Efficacy of surgical treatment for brain metastasis in patients with non-small cell lung cancer. Yonsei Med J. 2015;56(1):103–11. doi:10.3349/ymj.2015.56.1.103.
Barker 2nd FG. Craniotomy for the resection of metastatic brain tumors in the U.S., 1988-2000: decreasing mortality and the effect of provider caseload. Cancer. 2004;100(5):999–1007. doi:10.1002/cncr.20058.
•• Lim SH, Lee JY, Lee MY, Kim HS, Lee J, Sun JM, et al. A randomized phase III trial of stereotactic radiosurgery (SRS) versus observation for patients with asymptomatic cerebral oligo-metastases in non-small-cell lung cancer. Ann Oncol. 2015;26(4):762–8. doi:10.1093/annonc/mdu584. PhaseIII trial examining upfront SRS to conventional chemotherapy. Study was closed early due to approval of TKIs as first line, but did not show a benefit to early SRS.
•• Magnuson WJ, Yeung JT, Guillod PD, Gettinger SN, Yu JB, Chiang VL. Impact of deferring radiation therapy in patients with epidermal growth factor receptor-mutant non-small cell lung cancer who develop brain metastases. Int J Radiat Oncol Biol Phys. 2016;95(2):673–9. doi:10.1016/j.ijrobp.2016.01.037. Retrospective study with survival benefit to upfront SRS with TKI compared to salvage SRS.
Patchell RA, Tibbs PA, Regine WF, Dempsey RJ, Mohiuddin M, Kryscio RJ, et al. Postoperative radiotherapy in the treatment of single metastases to the brain: a randomized trial. JAMA. 1998;280(17):1485–9.
Robinet G, Thomas P, Breton JL, Lena H, Gouva S, Dabouis G, et al. Results of a phase III study of early versus delayed whole brain radiotherapy with concurrent cisplatin and vinorelbine combination in inoperable brain metastasis of non-small-cell lung cancer: Groupe Francais de Pneumo-Cancerologie (GFPC) Protocol 95-1. Ann Oncol. 2001;12(1):59–67.
Cai L, Zhu J-f, Zhang X-w, Lin S-x, Su X-d, Lin P, et al. A comparative analysis of EGFR mutation status in association with the efficacy of TKI in combination with WBRT/SRS/surgery plus chemotherapy in brain metastasis from non-small cell lung cancer. J Neuro-Oncol. 2014;120(2):423–30. doi:10.1007/s11060-014-1570-7.
Sperduto PW, Wang M, Robins HI, Schell MC, Werner-Wasik M, Komaki R, et al. A phase 3 trial of whole brain radiation therapy and stereotactic radiosurgery alone versus WBRT and SRS with temozolomide or erlotinib for non-small cell lung cancer and 1 to 3 brain metastases: radiation therapy oncology group 0320. Int J Radiat Oncol Biol Phys. 2013;85(5):1312–8. doi:10.1016/j.ijrobp.2012.11.042.
• Soon YY, Leong CN, Koh WY, Tham IW. EGFR tyrosine kinase inhibitors versus cranial radiation therapy for EGFR mutant non-small cell lung cancer with brain metastases: a systematic review and meta-analysis. Radiother Oncol. 2015;114(2):167–72. doi:10.1016/j.radonc.2014.12.011. Meta-analysis suggesting benefit to upfront radiotherapy compared to salvage stratedy.
•• Mulvenna P, Nankivell M, Barton R, Faivre-Finn C, Wilson P, McColl E, et al., editors. Dexamethasone and supportive care with or without whole brain radiotherapy in treating patients with non-small cell lung cancer with brain metastases unsuitable for resection or stereotactic radiotherapy (QUARTZ): results from a phase 3, non-inferiority, randomised trial. Lancet. 2016; doi:10.1016/s0140-6736(16)30825-x. No benefit to WBRT compared to steroids and best supportive care in patients who were not canidates for other local therapy. Study period largely pre-dated use of TKIs.
Gow CH, Chien CR, Chang YL, Chiu YH, Kuo SH, Shih JY, et al. Radiotherapy in lung adenocarcinoma with brain metastases: effects of activating epidermal growth factor receptor mutations on clinical response. Clin Cancer Res. 2008;14(1):162–8. doi:10.1158/1078-0432.ccr-07-1468.
Yamamoto M, Serizawa T, Shuto T, Akabane A, Higuchi Y, Kawagishi J, et al. Stereotactic radiosurgery for patients with multiple brain metastases (JLGK0901): a multi-institutional prospective observational study. Lancet Oncol. 2014;15(4):387–95. doi:10.1016/s1470-2045(14)70061-0.
Vogelbaum MA, Angelov L, Lee SY, Li L, Barnett GH, Suh JH. Local control of brain metastases by stereotactic radiosurgery in relation to dose to the tumor margin. J Neurosurg. 2006;104(6):907–12. doi:10.3171/jns.2006.104.6.907.
Andrews DW, Scott CB, Sperduto PW, Flanders AE, Gaspar LE, Schell MC, et al. Whole brain radiation therapy with or without stereotactic radiosurgery boost for patients with one to three brain metastases: phase III results of the RTOG 9508 randomised trial. Lancet. 2004;363(9422):1665–72. doi:10.1016/s0140-6736(04)16250-8.
Rades D, Huttenlocher S, Hornung D, Blanck O, Schild SE. Radiosurgery alone versus radiosurgery plus whole-brain irradiation for very few cerebral metastases from lung cancer. BMC Cancer. 2014;14:931. doi:10.1186/1471-2407-14-931.
Bowden G, Kano H, Caparosa E, Park S-H, Niranjan A, Flickinger J, et al. Gamma knife radiosurgery for the management of cerebral metastases from non–small cell lung cancer. J Neurosurg. 2015;122(4):766–72. doi:10.3171/2014.12.jns141111.
Churilla TM, Handorf E, Soffietti R, Kocher M, Aizer AA, Collette L, et al. Does whole-brain radiation therapy for oligometastatic brain metastases translate into a survival benefit for patients with a limited competing risk from extracranial disease? A secondary analysis of EORTC 22952-26001. Int J Radiat Oncol Biol Phys. 96(2):S56–S7. doi:10.1016/j.ijrobp.2016.06.147.
Chang EL, Wefel JS, Hess KR, Allen PK, Lang FF, Kornguth DG, et al. Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: a randomised controlled trial. Lancet Oncol. 2009;10(11):1037–44. doi:10.1016/s1470-2045(09)70263-3.
Zhuang H, Wang J, Zhao L, Yuan Z, Wang P. The theoretical foundation and research progress for WBRT combined with erlotinib for the treatment of multiple brain metastases in patients with lung adenocarcinoma. Int J Cancer. 2013;133(10):2277–83. doi:10.1002/ijc.28290.
Chinnaiyan P, Huang S, Vallabhaneni G, Armstrong E, Varambally S, Tomlins SA, et al. Mechanisms of enhanced radiation response following epidermal growth factor receptor signaling inhibition by erlotinib (Tarceva). Cancer Res. 2005;65(8):3328–35. doi:10.1158/0008-5472.can-04-3547.
Liu Y, Deng L, Zhou X, Zhou L, Xu Y, Gong Y, et al. Early radiation therapy combined with EGFR-TKI is associated with longer survival in EGFR-mutated non-small cell lung cancer patients with brain metastases. Int J Radiat Oncol Biol Phys. 2016;96(2):E436. doi:10.1016/j.ijrobp.2016.06.1725.
Magnuson WJ, Amini A, Patil T, Kavanagh BD, Camidge DR, Braunstein SE, et al. Deferring radiation therapy for brain metastases in patients with EGFR-mutant non-small cell lung cancer: a multi-institutional analysis. Int J Radiat Oncol Biol Phys. 2016;96(2S):S57–S8. doi:10.1016/j.ijrobp.2016.06.149.
Stokes TB, Niranjan A, Kano H, Choi PA, Kondziolka D, Dade Lunsford L, et al. White matter changes in breast cancer brain metastases patients who undergo radiosurgery alone compared to whole brain radiation therapy plus radiosurgery. J Neuro-Oncol. 2015;121(3):583–90. doi:10.1007/s11060-014-1670-4.
•• Cohen-Inbar O, Melmer P, Lee CC, Xu Z, Schlesinger D, Sheehan JP. Leukoencephalopathy in long term brain metastases survivors treated with radiosurgery. J Neuro-Oncol. 2016;126(2):289–98. doi:10.1007/s11060-015-1962-3. Study looking at rates of leukoencephalopathy in long term survivors for both SRS alone and SRS with history of WBRT.
Levin VA, Bidaut L, Hou P, Kumar AJ, Wefel JS, Bekele BN, et al. Randomized double-blind placebo-controlled trial of bevacizumab therapy for radiation necrosis of the central nervous system. Int J Radiat Oncol Biol Phys. 2011;79(5):1487–95. doi:10.1016/j.ijrobp.2009.12.061.
Brown PD, Pugh S, Laack NN, Wefel JS, Khuntia D, Meyers C, et al. Memantine for the prevention of cognitive dysfunction in patients receiving whole-brain radiotherapy: a randomized, double-blind, placebo-controlled trial. Neuro-Oncology. 2013;15(10):1429–37. doi:10.1093/neuonc/not114.
Marsh JC, Gielda BT, Herskovic AM, Abrams RA. Cognitive sparing during the administration of whole brain radiotherapy and prophylactic cranial irradiation: current concepts and approaches. J Oncol. 2010;2010:198208. doi:10.1155/2010/198208.
Gondi V, Hermann BP, Mehta MP, Tome WA. Hippocampal dosimetry predicts neurocognitive function impairment after fractionated stereotactic radiotherapy for benign or low-grade adult brain tumors. Int J Radiat Oncol Biol Phys. 2013;85(2):348–54. doi:10.1016/j.ijrobp.2012.11.031.
Wu YL, Zhou C, Cheng Y, Lu S, Chen GY, Huang C, et al. Erlotinib as second-line treatment in patients with advanced non-small-cell lung cancer and asymptomatic brain metastases: a phase II study (CTONG-0803). Ann Oncol. 2013;24(4):993–9. doi:10.1093/annonc/mds529.
Zhuang H, Yuan Z, Wang J, Zhao L, Pang Q, Wang P. Phase II study of whole brain radiotherapy with or without erlotinib in patients with multiple brain metastases from lung adenocarcinoma. Drug Des Devel Ther. 2013;7:1179–86. doi:10.2147/DDDT.S53011.
Wu C, Li YL, Wang ZM, Li Z, Zhang TX, Wei Z. Gefitinib as palliative therapy for lung adenocarcinoma metastatic to the brain. Lung Cancer. 2007;57(3):359–64. doi:10.1016/j.lungcan.2007.03.011.
Zeng Y-D, Zhang L, Liao H, Liang Y, Xu F, Liu J-L, et al. Gefitinib alone or with concomitant whole brain radiotherapy for patients with brain metastasis from non-small-cell lung cancer: a retrospective study. Asian Pac J Cancer Prev. 2012;13(3):909–14. doi:10.7314/apjcp.2012.13.3.909.
Ge H, Zhu Q, Sun Y. Comparing the clinical efficacy of TKI alone with TKI plus concomitant WBRT for EGFR mutation-positive lung adenocarcinoma patients with brain metastases: a retrospective study. Int J Radiat Oncol Biol Phys. 2016;96(2S):S132. doi:10.1016/j.ijrobp.2016.06.322.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Tresa McGranahan declares that she has no conflict of interest.
Seema Nagpal has received clinical trial funding from Nektar Therapeutics and has received consulting fees from Novartis.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Lung Cancer
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
McGranahan, T., Nagpal, S. A Neuro-oncologist’s Perspective on Management of Brain Metastases in Patients with EGFR Mutant Non-small Cell Lung Cancer. Curr. Treat. Options in Oncol. 18, 22 (2017). https://doi.org/10.1007/s11864-017-0466-0
Published:
DOI: https://doi.org/10.1007/s11864-017-0466-0