Abstract
Pelvic congestion syndrome (PCS) poses a significant health, diagnostic, and economic challenges. Transcatheter embolisation has emerged as a promising treatment for PCS. A systematic review was performed in order to assess the safety and efficacy of transcatheter embolisation in the treatment of PCS. A systematic search of electronic databases was performed using ‘PubMed’, ‘Embase’, ‘Medline (OVID)’, and ‘Web of Science’, for articles pertaining to efficacy of embolotherapy for the treatment of pelvic congestion syndrome. A total of 25 studies were included in this systematic review with a combined total of 2038 patients. All patients included were female with a mean average age of 37.65 (31–51). Of the 25 studies, 18/25 studies reported pre- and post-procedural pelvic pain outcomes using a visual analogue scale (VAS). All studies showed a reduction in VAS post-procedure. Transcatheter embolisation had a high technical success rate (94%) and an overall complication rate of 9.0%, of which 10.4% were major and 89.6% were minor. Fifteen out of 19 (78.9%) major complications required a subsequent intervention. Transcatheter embolisation using various techniques is effective and safe in treating PCS. A low quality of evidence limits the currently available literature; however, embolisation has shown to improve symptoms in the majority of patients with low complication rates and recurrence rates.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Chronic pelvic pain (CPP) is a common condition affecting up to a quarter of the female population worldwide [1]. It is characterised by pain originating from the pelvis that lasts more than 6 months and is associated with negative cognitive, behavioural, sexual and emotional consequences [12]. CPP accounts for up to 40% of gynaecological laparoscopies and approximately 20% of all gynaecology outpatient appointments, creating a significant economic burden on health systems [3, 4].
Thirty to 40% of cases of CPP are associated with pelvic congestion syndrome (PCS) [7]. PCS consists of a number of clinical symptoms associated with concomitant anatomical abnormalities secondary to pelvic venous insufficiency, usually reflux of the ovarian or internal iliac veins [2]. The aetiology of PCS is not completely understood but is hypothesised to involve hormonal, mechanical, and vasoactive factors leading to venous dilatation (>5 mm), insufficiency, and pelvic venous reflux [3]. Patients with PCS often present with non-cyclical chronic pelvic pain worsened by standing, associated with dyspareunia or lower urinary tract symptoms, and may have perineal, buttock, vulval, or vaginal varicosities on examination [4].
Several therapeutic options have been shown to successfully alleviate pain in patients suffering from PCS including medical, surgical, and endovascular therapies. Medical therapies range from simple analgesia to hormonal therapies (medroxyprogesterone acetate/gonadotropin receptor agonists) or venoactive therapies (micronised purified flavonoid fraction). Surgical options include open/laparoscopic ovarian vein embolisation or hysterectomy with salpingo-oophorectomy. Transcatheter embolisation has emerged as one of the effective treatments for PCS, with technical success rate of 98-100% and symptom improvement at 1-5 years of follow-up in 80-93% of patients [5,6,7,8,9]. This technique aims to occlude venous axes that have been proven to be insufficient with venography performed in the same procedure, and can be safely performed in an ambulatory outpatient clinic as a day procedure [10, 11].
PCS poses significant health, diagnostic, and economic challenges. A systematic review was performed in order to assess the efficacy and safety of transcatheter embolisation in the treatment of PCS.
Methods
Search strategy and data extraction
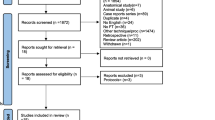
A systematic review was conducted in accordance to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. A formal systematic search was performed of the PubMed, Embase, Medline (OVID), and Web of Science databases using keywords and MeSH terms to identify relevant titles up to and including August 21st, 2022, for studies relating to the efficacy of embolotherapy for the treatment of pelvic congestion syndrome (Fig. 1). Grey literature and reference lists of relevant articles were reviewed for relevant studies. This study was prospectively registered with the International Prospective Register of Systematic Reviews in the PROSPERO platform with the reference number CRD42022374727.
The search was performed by two independent reviewers (JH and HT), using a predetermined search strategy that was designed by the senior authors. Details in relation to the search strategy can be found in Supplementary Appendix 1 (S1). Retrieved studies were reviewed to ensure studies met the predefined inclusion and exclusion criteria (see below). Discordances in opinion were resolved through consultation with a third author (NOS). Manual cross-referencing of reference lists from studies was undertaken to identify further potential articles for inclusion.
Two reviewers, JH and HT, independently extracted data from the studies identified. They recorded study details, basic patient clinicopathological characteristics, management strategies, and outcomes. The information was extracted based on the PICOTS framework, which includes population, intervention, comparator, outcomes, timing, and setting. GraphPad Prism (version 8.3.0) was used to analyse and create figures.
Eligibility criteria
The inclusion criteria were as follows: (1) published studies demonstrating the efficacy of embolotherapy for the treatment of pelvic congestion syndrome, (2) published in the English language, and (3) published after 1995.
The exclusion criteria were as follows: (1) abstract only, (2) studies failing to discuss or denote PCS, (3) paediatric cohorts aged less than 18 years, and (4) case reports.
Risk of bias
Assessment of potential biases within included RCTs was assessed using the Cochrane Collaboration (for randomised controlled trials (RCTs)) [12, 13]. This assessment tool grades each study as being high (red circle), low (green circle), or unclear (yellow) risk of bias across six categories. For non-RCT studies, Newcastle–Ottawa scale (NOS) risk of bias tool (2) and the results were tabulated. This assessment tool grades each study as being ‘satisfactory’ or ‘unsatisfactory’ across various categories. We assigned stars to evaluate study quality: 7 stars, ‘very good’; 5–6 stars ‘good’; 3–4 stars, ‘satisfactory’; and 0–2 stars, ‘unsatisfactory’. The critical appraisal was completed by two reviewers independently (JH and HT), where once again a third reviewer (NOS) was asked to arbitrate in cases of discrepancies in opinion.
Aims and objectives
The overall aims and objectives of this study were as follows:
-
Primary outcome:
-
1.
Improvement in pelvic pain measured subjectively or objectively using a 0 to 10 visual analogue score (VAS)
-
1.
-
Secondary outcomes:
-
1.
Other PCS symptom improvement measured subjectively or objectively using a 0 to 10 VAS, including dysmenorrhoea, lower limb pain, and dyspareunia
-
2.
Reintervention rate, which was defined as any subsequent intervention due to a sequelae of the patient’s symptoms
-
3.
Recurrence rate, which was defined as radiological or symptomatic recurrence of initial symptoms after index treatment.
-
4.
Complication rate, classified according to the Society of Interventional Radiology (SIR) classification system for complications by outcome [14]:
-
(a)
Post-embolisation syndrome, defined as the occurrence of gluteal and lumbar post-procedural pain, and/or abdominal pain in the area of the vessel embolised and/or pyrexia [15].
-
(b)
Access complications, defined as the presence of a haematoma at the procedural puncture site [16].
-
(c)
Coil migration, defined as entire or free fragment of coil deployed in a normal vessel, or any vessel other than the target vessel [17].
-
(d)
Reintervention, defined as a subsequent procedure required due to a complication from the index procedure
-
(a)
-
5.
Technical success, defined as successful occlusion of the target vein demonstrated to display reflux on venography or pre-operative imaging
-
1.
Results
Study selection/included studies
The systematic search strategy identified a total of 1773 studies, of which 491 duplicate studies were manually removed. The remaining 1282 studies were screened for relevance, before 54 full texts were reviewed. In total, 25 studies fulfilled our inclusion criteria and were included in this systematic review (Fig. 1) [6,7,8,9, 18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38]. Due to heterogeneity in study method and results presented, a meta-analysis was not performed, and a collative summary of findings was deemed appropriate.
Baseline characteristics
The data collected were highly heterogeneous and descriptive. The majority of studies had similar and consistent study population groups, with all 25 studies focusing on females undergoing pelvic venous embolisation for pelvic congestion syndrome. The study design was a retrospective cohort study in 13/25 reviews [8, 19, 23,24,25, 27, 29, 32,33,34,35,36], prospective cohort study in 8/25 reviews [7, 18, 20,21,22, 26, 28, 37, 38], and case series (with greater than 10 patients in 2/25 reviews) [30, 31], and 2/25 studies were randomised clinical trials (RCT) [6, 9]. The combined total of patients was 2038 across all 25 studies (range in sample size, 11–520). The mean average age 37.65 (range of reported means, 31–51). All patients were female, with no reported male cases. Of the 25 studies included in this analysis, the three most common countries of publication were Spain (5/25) [7, 9, 18, 19, 32], France (5/25) [8, 21, 23, 38], and the USA (3/25) [28, 31, 36]. The mean follow-up time was 23.54 months (range, 4.5–60). Publication dates ranged from 1997 to 2022. The primary outcome was improvement in VAS for CPP in 18/25 studies [6,7,8, 18,19,20, 23, 24, 26, 28, 29, 32,33,34,35,36,37,38]. A summary of study characteristics is presented in Table 1.
Risk of bias
Both of the included RCTs were ‘low risk’ of bias for most of the categories, using the Cochrane Collaboration risk of bias assessment for RCTs. The RCTs failed to provide detailed information in relation to their blinding process, rendering them ‘intermediate risk’ of bias. In regard to non-RCT studies, one study was ‘very good’, fourteen studies were ‘good’, seven studies were ‘satisfactory’, and one study was ‘unsatisfactory’. S1&2 summarises the results of our risk of bias assessment.
Intervention technique
The technique used for embolisation varied between studies. All 25 studies reported the access vessel(s) used. The most common access vessel utilised for vessel puncture was the left or right common femoral vein, which was accessed in 21 studies [6,7,8, 19,20,21,22, 24,25,26,27,28,29,30,31,32,33,34,35,36, 38]. All 25 studies reported the target vein embolised, of which there were 5126 veins embolised in 2038 patients. As seen in Table 2, the most common target vein was the left ovarian vein (LOV). Fluoroscopy time was reported in 8/25 studies, with a mean time of 33.3 min (SD 18.7, range 7.6–43.3) [7, 9, 18, 23, 25, 30, 32, 33]. The embolotherapy technique was reported in all studies. The most common embolotherapy was the use of coils only which was used in 9/25 studies [6, 7, 9, 19, 24, 29, 31, 32, 34]. PVE was predominantly performed by interventional radiology in 21/25 (84%) studies [7,8,9, 18,19,20,21,22,23,24,25,26,27,28, 30, 32, 33, 35,36,37,38], followed by vascular surgery in 3/25 (12%) studies [29, 31, 34].
Primary outcome
Overall, 18/25 studies reported pre- and post-procedural pain outcomes using a visual analogue scale (VAS) [6,7,8, 18,19,20, 23, 24, 26, 28, 29, 32,33,34,35,36,37,38]. As indicated in Table 3, all but one showed statistically significant reduction in VAS post-procedure. Pyra et al. did not report a p-value but demonstrated a reduction in VAS from 7.3 pre-procedure to 1.6 post-procedure [20]. Furthermore, 17/25 studies reported a qualitative improvement in pain. These findings are summarised in Table 4 [7,8,9, 19, 21,22,23,24, 26,27,28,29,30,31, 34,35,36]. Of note, 5/17 studies showed a proportion of patient who’s symptoms worsened at the time of follow-up [7, 8, 27, 29, 36].
Secondary outcome
Other symptoms of PCS
Other commonly reported outcomes were improvement in other symptoms such as dyspareunia and dysmenorrhoea; these are summarised in Table 3. Five studies (5/25) reported pre- and post-procedure VAS scores for dyspareunia [8, 18, 33, 36, 38]. Pre- and post-procedure VAS scores for dysmenorrhoea were reported in 4/25 studies [18, 33, 36, 38]. Qualitative improvements were recorded for a variety of symptoms amongst the studies, including dyspareunia (8/25) [9, 18, 23, 30, 31, 33, 36, 38], dysmenorrhoea (6/25) [9, 18, 31, 33, 36, 38], lower limb pain (2/25) [8, 38], post-coital pain (3/25) [8, 31, 38], and urinary symptoms (5/25) [9, 23, 31, 33, 36].
Symptom recurrence and reintervention
Symptom recurrence during the follow-up period was reported in 17/25 studies and ranged from 0 to 42% during the follow-up period [8, 18, 21, 23,24,25,26,27,28, 30,31,32,33,34, 36, 37]. The most common methods of reintervention were repeat embolisation procedure and hysterectomy. These findings are summarised in Table 5.
Technical success and complications
Technical success was reported in 20/25 studies and was achieved in 1583/1676 patients (94%). Complications were grouped according to the SIR classification system for complications by outcome as seen in Table 6 [14]. The most common complication was post-embolisation syndrome defined as mild abdominal pain immediately post-operatively which was self-resolving or treated with simple analgesia. There were 15 complications that required surgical or radiological intervention, including 13 migrated coils that required snaring, one common femoral artery injury that resulted in a false aneurysm and required embolisation, and one patient who developed salpingitis 1 month post-procedure requiring surgical intervention. There were no complications that led to permanent adverse sequelae, or death of a patient.
Discussion
This systematic review supports pelvic venous embolisation (PVE) as a safe and effective treatment modality for pelvic congestion syndrome (PCS), with all studies demonstrating improvement in symptoms in a majority of patients, and low complication and recurrence rates. This systematic review adds a contemporary analysis of the literature, incorporating several embolotherapy techniques such as various sclerotherapy agents, vascular plugs, and coils. Furthermore, by analysing VAS scores, this review provides a more uniform and objective way to quantify the efficacy of embolisation in the treatment in PCS.
In the symptom profile of PCS, chronic pelvic pain is the most commonly reported. All 25 studies analysed showed improvement in chronic pelvic pain in the majority of participants. There is currently a sparsity of validated quality of life tools available for CPP which has led to the VAS being widely used [39]. The VAS allows a more objective method to measure and compare pain scores and was used in 18 of the 25 studies. All 18 studies that reported VAS showed a significant improvement in pre-procedural vs. post-procedural scores for pelvic pain. The 7 studies that did not utilise VAS score demonstrated a subjective improvement in pain scores. In these studies, 67–100% of participants reported reduction in pelvic pain post treatment. This systematic review supports the previous literature which has demonstrated the efficacy of PVE in reducing chronic pelvic pain in PCS. Brown et al. also reported improvement in clinical symptoms in 68–100% of patients, although this review was performed in 2018, and only reported the results of 14 papers [2]. Sutanto et al. examined outcomes of isolated coil embolisation only and reported a 5.47 point improvement on the VAS scale at 2 years after PVE in a pooled analysis of eight studies and a qualitative improvement in pain in the majority (70–100%) of patients in four studies [40].
Although chronic pelvic pain is the most described symptom of PCS, it can present with a variety of other debilitating symptoms including dyspareunia and dysmenorrhoea [10]. Significant quantitative improvement in both dyspareunia and dysmenorrhoea was seen in studies reporting VAS scores for these symptoms, although pre-procedural VAS scores were generally lower for other symptoms compared to pelvic pain. Qualitative information collected measuring other symptoms such as lower limb pain, post-coital pain, and lower urinary tract symptoms (LUTS) also demonstrated high rates of subjective improvement.
PVE has become a widely accepted treatment modality for PCS as it is less invasive than open surgical or laparoscopic ligation techniques and has been shown to be safely performed in an ambulatory day clinic using local anaesthetic only [10, 11]. This was reflected in this review with low complication rates reported across studies. In total, 183 complications occurred across 2038 procedures. The majority of these complications (89%) were self-limiting and did not require pharmacological, radiological, or surgical treatment, including post-embolisation syndrome (PES) and access site haematomas. Of the 183 complications, 15 (8%) complications required surgical or radiological intervention. The most common of these was coil migration into the pulmonary vasculature requiring snaring, usually performed at the time of the index procedure through the same access, without any deleterious long-term sequelae. Proportionally, our review found a higher number of major and minor complications compared to the review by Sutanto et al., who investigated coil embolisation only (9.0% vs. 3.8%). Although the addition of other embolisation techniques (such as foam sclerotherapy, ethiodised oil, and Onyx) into our systematic review seemingly increased the complication rates, closer analysis of the data shows a higher rate of non-PES complications in studies that used coil embolisation. Of note, the 8 studies with the highest rates of complications (8–45%) used coil embolisation [7, 9, 29,30,31,32, 34, 37], and the 5 studies that reported no complications used other embolotherapy techniques such as Onyx, foam sclerotherapy, ethiodised oil, and Glubran-2 [18, 21, 26, 27, 35]. However, given the heterogeneity of the studies, it is difficult to draw meaningful conclusions from this.
Symptom recurrence (7.4%) and reintervention rates (3.9%) were low, despite widely variable follow-up periods amongst ranging from 4.5 months to 5 years. These rates were comparatively low compared to previous studies, such as that of Sutanto et al. who reported a 10–30% reintervention rate, predominantly due to recurrent pelvic pain or recurrent pelvic varices [40]. There was no clear pattern with regard to an embolotherapy technique associated with lower recurrence or reintervention rates.
The literature comparing different embolotherapy techniques in the treatment of PCS is scarce which has led to significant heterogeneity in clinical practice. In our review, there were two studies that directly compared the outcomes of coil embolotherapy and vascular plugs for pelvic vein embolisation. Guirola et al. performed a randomised trial comparing the use of Amplatzer vascular plugs to fibred platinum coils and did not find any difference in improvement of VAS scores or complication rates between the two devices [9]. De Gregorio et al. retrospectively analysed patients undergoing pelvic venous embolisation with either Amplatzer vascular plugs or coils and similarly did not find any significant difference in short and long-term outcomes. Although current guidelines recommend pelvic venous embolisation as a safe treatment for patients with CPP due to PCS, there is no evidence-based recommendation for the optimal embolic material used, and this decision is largely physician dependent [41]. Further research comparing the various embolisation techniques are required.
There were several limitations of our review including the small number of studies with quantitative comparative data and the heterogeneity of their study designs, which precluded collative meta-analysis and large volume analysis. Furthermore, the majority of studies were retrospective in design and did not control for other confounding factors. Robust prospective, randomised controlled trials and qualitative Delphi studies are needed to define treatment and diagnostic protocols. Finally, the studies included in this study span 25 years (1997–2022) which brings into question the comparability of these data provided. Nonetheless, our study will impact clinical practice by allowing interventionalists and surgeons to counsel patients on the optimal management’s options and inform patient on expected outcomes.
Conclusion
PCS is a prevalent condition that significantly impacts quality of life and poses a diagnostic and economic challenge to the public. According to current literature, PVE is a safe treatment option that effectively reduces symptom burden with relatively low complication rates. However, the studies reported in the literature were variable in sample size, follow-up period, and outcome description. Further research is required to draw conclusions about the longevity and optimal embolisation method, particularly regarding long-term follow-up and a head-to-head comparison of the embolotherapy technique.
References
Chronic Pelvic Pain (2020) ACOG Practice Bulletin Summary, Number 218. Obstet Gynecol 135(3):744–746. https://doi.org/10.1097/AOG.0000000000003717. PMID: 32080045
Brown CL, Rizer M, Alexander R et al (2018) Pelvic congestion syndrome: Systematic review of treatment success. Semin Intervent Radiol 35(1):35–40. https://doi.org/10.1055/s-0038-1636519. Epub 2018 Apr 5. PMID: 29628614; PMCID: PMC5886772
Phillips D, Deipolyi AR, Hesketh RL et al (2014) Pelvic congestion syndrome: etiology of pain, diagnosis, and clinical management. J Vasc Interv Radiol 25(5):725–733
Whiteley MS (2018) The current overview of pelvic congestion syndrome and pelvic vein reflux. Indian J Vasc Endovasc Surg 5(4):227
Borghi C, Dell’Atti L (2016) Pelvic congestion syndrome: the current state of the literature. Arch Gynecol Obstet 293(2):291–301
Chung M-H, Huh C-Y (2003) Comparison of treatments for pelvic congestion syndrome. Tohoku J Exp Med 201(3):131–138
Laborda A, Medrano J, de Blas I et al (2013) Endovascular treatment of pelvic congestion syndrome: visual analog scale (VAS) long-term follow-up clinical evaluation in 202 patients. Cardiovasc Intervent Radiol 36(4):1006–1014
Senechal Q, Echegut P, Bravetti M et al (2021) Endovascular treatment of pelvic congestion syndrome: Visual analog scale follow-up. Front Cardiovasc Med 8:751178. https://doi.org/10.3389/fcvm.2021.751178. PMID: 34869656; PMCID: PMC8635860
Guirola JA, Sánchez-Ballestin M, Sierre S et al (2018) A randomized trial of endovascular embolization treatment in pelvic congestion syndrome: fibered platinum coils versus vascular plugs with 1-year clinical outcomes. J Vasc Interv Radiol 29(1):45–53
Antignani P-L, Lazarashvili Z, Monedero JL et al (2019) Diagnosis and treatment of pelvic congestion syndrome: UIP consensus document. Int Angiol 38(4):265–283
Whiteley MS, Lewis-Shiell C, Bishop SI et al (2018) Pelvic vein embolisation of gonadal and internal iliac veins can be performed safely and with good technical results in an ambulatory vein clinic, under local anaesthetic alone–results from two years’ experience. Phlebology 33(8):575–579
Higgins JP, Altman DG, Gøtzsche PC et al (2011) The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 343:d5928. https://doi.org/10.1136/bmj.d5928. PMID: 22008217; PMCID: PMC3196245
Wells GA, Shea B, O’Connell et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Available at: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
Sacks D, McClenny TE, Cardella JF, Lewis CA (2003) Society of interventional radology clinical practice guidelines. J Vasc Interv Radiol 14:S199-202
Gavrilov SG, Krasavin GV, Mishakina NY, Kirsanov KV (2021) Postembolization syndrome in endovascular interventions on the gonadal veins. J Vasc Surg Venous Lymphat Disord 9(3):697–702
Ortiz D, Jahangir A, Singh M et al (2014) Access site complications after peripheral vascular interventions: incidence, predictors, and outcomes. Circ: Cardiovasc Interv 7(6):821–828
Skipworth JR, Morkane C, Raptis DA et al (2011) Coil migration--a rare complication of endovascular exclusion of visceral artery pseudoaneurysms and aneurysms. Ann R Coll Surg Engl 93(4):e19–23. https://doi.org/10.1308/003588411X13008844298652. PMID: 21944789; PMCID: PMC5827005
Lorenzo JIL, Madueño GG, Peral AA et al (2022) Bilateral ovarian vein embolisation from a unilateral basilic approach with n-2-butyl cyanoacrylate and crossover technique for pelvic congestion syndrome. Eur J Vasc Endovasc Surg 63(1):163–164
Nasser F, Cavalcante RN, Affonso BB et al (2014) Safety, efficacy, and prognostic factors in endovascular treatment of pelvic congestion syndrome. Int J Gynecol Obstet 125(1):65–68
Pyra K, Woźniak S, Drelich-Zbroja A et al (2016) Evaluation of effectiveness of embolization in pelvic congestion syndrome with the new vascular occlusion device (ArtVentive EOS™): preliminary results. Cardiovasc Intervent Radiol 39:1122–1127
Marcelin C, Izaaryene J, Castelli M et al (2017) Embolization of ovarian vein for pelvic congestion syndrome with ethylene vinyl alcohol copolymer (Onyx®). Diagn Interv Imaging 98(12):843–848
Maleux G, Stockx L, Wilms G, Marchal G (2000) Ovarian vein embolization for the treatment of pelvic congestion syndrome: long-term technical and clinical results. J Vasc Interv Radiol 11(7):859–864
Hocquelet A, Le Bras Y, Balian E et al (2014) Evaluation of the efficacy of endovascular treatment of pelvic congestion syndrome. Diagn Interv Imaging 95(3):301–306
Siqueira FM, Monsignore LM, Rosa-e-Silva JC et al (2016) Evaluation of embolization for periuterine varices involving chronic pelvic pain secondary to pelvic congestion syndrome. Clinics (Sao Paulo) 71:703–708. https://doi.org/10.6061/clinics/2016(12)05. PMID: 28076514; PMCID: PMC5175291
Tinelli A, Prudenzano R, Torsello M et al (2012) Suprapubic percutaneous sclero-embolization of symptomatic female pelvic varicocele under local anesthesia. Eur Rev Med Pharmacol Sci 16(1):111–117
Tropeano G, Di Stasi C, Amoroso S et al (2008) Ovarian vein incompetence: a potential cause of chronic pelvic pain in women. Eur J Obstet Gynecol Reprod Biol 139(2):215–221
van der Vleuten CJ, van Kempen JA, Schultze-Kool LJ (2012) Embolization to treat pelvic congestion syndrome and vulval varicose veins. Int J Gynecol Obstet 118(3):227–230
Venbrux AC, Chang AH, Kim HS et al (2002) Pelvic congestion syndrome (pelvic venous incompetence): impact of ovarian and internal iliac vein embolotherapy on menstrual cycle and chronic pelvic pain. J Vasc Interv Radiol 13(2):171–178
Asciutto G, Asciutto K, Mumme A, Geier B (2009) Pelvic venous incompetence: reflux patterns and treatment results. Eur J Vasc Endovasc Surg 38(3):381–386
Capasso P, Simons C, Trotteur G et al (1997) Treatment of symptomatic pelvic varices by ovarian vein embolization. Cardiovasc Intervent Radiol 20:107–111
Cordts PR, Eclavea A, Buckley PJ et al (1998) Pelvic congestion syndrome: early clinical results after transcatheter ovarian vein embolization. J Vasc Surg 28(5):862–868
De Gregorio MA, Guirola JA, Alvarez-Arranz E et al (2020) Pelvic venous disorders in women due to pelvic varices: treatment by embolization: experience in 520 patients. J Vasc Interv Radiol 31(10):1560–1569
Gandini R, Konda D, Abrignani S et al (2014) Treatment of symptomatic high-flow female varicoceles with stop-flow foam sclerotherapy. Cardiovasc Intervent Radiol 37:1259–1267
Gavrilov SG, Sazhin A, Krasavin G et al (2021) Comparative analysis of the efficacy and safety of endovascular and endoscopic interventions on the gonadal veins in the treatment of pelvic congestion syndrome. J Vasc Surg Venous Lymphat Disord 9(1):178–186
Gong M, He X, Zhao B et al (2021) Ovarian vein embolization with N-butyl-2 Cyanoacrylate Glubran-2® for the treatment of pelvic venous disorder. Front Surg 8:760600. https://doi.org/10.3389/fsurg.2021.760600. PMID: 34977140; PMCID: PMC8716375
Kim HS, Malhotra AD, Rowe PC et al (2006) Embolotherapy for pelvic congestion syndrome: long-term results. J Vasc Interv Radiol 17(2):289–297
Meneses L, Fava M, Diaz P et al (2013) Embolization of incompetent pelvic veins for the treatment of recurrent varicose veins in lower limbs and pelvic congestion syndrome. Cardiovasc Intervent Radiol 36:128–132
Jambon E, Le Bras Y, Coussy A et al (2022) Embolization in pelvic venous disorders using ethylene vinyl alcohol copolymer (Onyx®) and aetoxysclerol: a prospective evaluation of safety and long-term efficacy. Eur Radiol 32(7):4679–4686
Ghai V, Subramanian V, Jan H, Doumouchtsis SK (2022) A systematic review highlighting poor quality of evidence for content validity of quality of life instruments in female chronic pelvic pain. J Clin Epidemiol 149:1–11
Sutanto SA, Tan M, Onida S, Davies AH (2022) A systematic review on isolated coil embolization for pelvic venous reflux. J Vasc Surg Venous Lymphat Disord 10(1):224–232
De Maeseneer MG, Kakkos SK, Aherne T et al (2022) Editor’s Choice-European Society for Vascular Surgery (ESVS) 2022 clinical practice guidelines on the management of chronic venous disease of the lower limbs. Eur J Vasc Endovasc Surg 63(2):184–267
Funding
Open Access funding provided by the IReL Consortium
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1975 Helsinki Declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Consent to participate
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hanna, J., Bruinsma, J., Temperley, H.C. et al. Efficacy of embolotherapy for the treatment of pelvic congestion syndrome: A systematic review. Ir J Med Sci 193, 1441–1451 (2024). https://doi.org/10.1007/s11845-024-03608-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-024-03608-6