Abstract
Background
The major changes in the timing of meals during Ramadan may be challenging for hypothyroid patients on levothyroxine. We aimed to study the effect of Ramadan fasting on thyroid functions in hypothyroid patients taking levothyroxine.
Methods
We did a comprehensive search of 8 databases for Randomized controlled studies (RCTs) and observational studies investigating the effect of Ramadan fasting on thyroid functions in hypothyroid individuals taking levothyroxine. Relevant data was extracted and analyzed. Mean difference (MD) and standard deviation (SD) were used to evaluate the continuous data. Risk ratios (RR) with a 95% confidence interval were used for outcomes constituting dichotomous data. National Institutes of Health (NIH) tools were used to assess the risk of bias.
Results
Fourteen studies met our inclusion criteria, 3 RCTs, and 11 observational studies, all designed as pre-post studies. Ramadan fasting was associated with a statistically significant increase in TSH in patients who were euthyroid before Ramadan (MD = -0.76 [95% CI; -1.27, -0.25]). However, free thyroxine (FT4) was found to be stable (MD = 0.01, [95% CI; -0.03, 0.06]). All timing points were associated with a significant increase in TSH levels after Ramadan, pre-iftar (MD = -0.69 [95% CI; -1.03, -0.36]), post-iftar (MD = -0.76 [95% CI; -1.12, -0.39]), and pre-suhoor (MD = -1.19 [95% CI; -2.18, -0.19]).
Conclusion
TSH increases significantly after Ramadan. No timing point has superiority in maintaining thyroid control. However, choosing the timing should be individualized according to the patient’s preference to guarantee the most possible compliance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Millions of adult Muslims worldwide observe fasting during the holy month of Ramadan each year. Ramadan fasting is a type of intermittent fasting that is considered an obligatory Islamic tradition, as it is one of the five core pillars of Islam. During Ramadan, observant Muslims abstain from food, liquids, smoking, and sexual intercourse from dawn to dusk for 29–30 days annually. Ramadan, the ninth Islamic month, advances by 10 days each year according to the lunar calendar (355 days a year). Therefore, the number of fasting hours may vary depending on the season. During these fasting hours, Muslims often eat two meals a day: "Iftar", the meal that marks the conclusion of their fast at sunset, and "Suhoor", a quick supper eaten just before dawn [1,2,3].
The Quran exempts many cases from fasting, including those with chronic medical illnesses that fasting would worsen and those on drug regimens that might be harmed. Nevertheless, many people choose to observe the fast, often against medical advice, and frequently skip their midday doses since taking oral drugs during the fasting period invalidates the fast [4,5,6]. This has ramifications for a variety of chronic diseases, including the prevalent endocrine illness hypothyroidism [7].
Levothyroxine, the primary medication for hypothyroidism, is primarily absorbed in the small intestine, notably through the ileum [8]. The standard dose of levothyroxine is 1.5 µg / kilogram body weight to be taken 30–60 min before breakfast or 3 h or more after the evening meal on an empty stomach (usually at bedtime) to prevent interference with its intestinal uptake by food or medications [7, 9, 10]. These facts explain the low adherence of hypothyroid patients to the drug [11].
In Ramadan, hypothyroid patients, with the guidance of their medical care providers, have to choose the appropriate timing of levothyroxine intake to ensure full compliance, keeping in mind the precautions that must be taken, such as taking the drug on an empty stomach (no food or beverages for 3–4 h before, and 1 h after) [9]. They may take it before the iftar meal, after iftar, or before suhoor. Adhering to the recommended regimen during Ramadan represents a significant challenge to hypothyroid patients since it is notably difficult to delay the sunset meal (iftar), which is a significant social event and a time of acute hunger, for 30 to 60 min after levothyroxine administration. Additionally, they have relatively few hours in which they are allowed to eat and drink, making it challenging for them to abstain from eating for 3 to 4 h after the iftar meal or before the suhoor meal. Furthermore, most patients are not able to get up 30 min before each predawn suhoor meal for levothyroxine administration [12,13,14].
This issue has been a field of interest in the last decade, with several studies yielding considerable controversies in their results. Some studies have tested the effect of Ramadan fasting on thyroid functions, while others have compared different time points for levothyroxine intake to choose the optimal timing [12,13,14,15,16,17,18,19,20,21,22,23,24,25]. Although millions of Muslims with hypothyroidism often fast during Ramadan, there is a lack of high-quality evidence on how it affects thyroid functions (TF) and how to manage hypothyroid patients during Ramadan. To our knowledge, this is the first systematic review and meta-analysis pooling the current evidence in this area.
Methods
This systematic review was performed in accordance with the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) statement [26].
Data source and search terms
We searched 8 databases: PubMed, Scopus, Web Of Science (WOS), Ovid, Science Direct, Cochrane Library, Google Scholar, and ClinicalTrial.gov in October 2022. This search was supported by extensive manual searches till the end of November 2022. Without any restrictions or filters, we used these search terms; (Ramadan OR Islamic) AND (Levothyroxine [MeSH Terms] OR Thyroid [MeSH Terms] OR hypothyroidism OR TSH). The detailed search strategy and results can be found in the Supplementary Table 1.
Eligibility criteria
RCTs and observational studies written in English with the following PICO criteria were included: Population (P): hypothyroid patients taking thyroid hormone replacement; Intervention (I): Ramadan fasting;Control (C): No fasting;Outcome (O): the difference in serum TSH levels before and after Ramadan, and the effect of the drug timing (pre-iftar, post-iftar, and pre-suhoor) on the TSH level change (µIU/mL), the change in free thyroxine (FT4 ng/dl), and the difference in the number of patients with a TSH level above the reference range before and after Ramadan. Studies investigating fasting forms rather than Ramadan or Islamic fasting were not eligible. We excluded animal studies, reviews, pilot studies, post hoc analyses, and studies in a non-English language.
Study selection
We exported the studies to Rayyan software, removed duplicates, then started title and abstract screening [27]. Each study was assessed by 2 independent reviewers. Six reviewers participated in this step (MMB, ARY, NAE, HB, MAQ, and AAM). Studies that were found relevant after the title and abstract screening were subjected to a more detailed full-text screening according to our prespecified eligibility criteria. Any disputes were resolved by a third reviewer (EMR).
Data extraction and outcomes
Data from the final included studies were extracted into Microsoft Excel spreadsheets. The extracted data included the following: (a) Summary of the included studies (year, country, sample size, population, study design, and main outcomes measured), (b) Baseline characteristics of enrolled patients. (c) Details of regimens in studies comparing different time points of hormone intake, (d) The primary outcomes were the difference in serum TSH levels before and after Ramadan, and the effect of the drug timing (pre-iftar, post-iftar, and pre-suhoor) on the TSH level change (µIU/mL). The secondary outcomes were the change in FT4 (ng/dl), and the difference in the number of patients with a TSH level above the reference range before and after Ramadan. Each study was subjected to the data extraction step by two independent reviewers and rechecked by a third reviewer for any controversies.
Risk of bias and quality assessment
Each study was assessed for quality by two independent reviewers. Seven reviewers participated in this step (EMR, MMB, AAM, ARY, HB, NAE, and MAQ) using the National Institutes of Health (NIH) quality assessment tools for controlled intervention studies, pre-post studies, cohort, and cross-sectional studies, chosen according to their study designs [30]. The first tool was used for randomized controlled studies, the second tool for prospective cohort studies, and the last one for retrospective cohort studies.
Statistical analysis
We used the Review Manager Software (version 5.4) to perform the meta-analysis. Mean difference (MD) and standard deviation (SD) were used to evaluate continuous outcomes, while risk ratios (RR) with a 95% confidence interval were used to measure dichotomous outcomes. In the case of heterogeneity (I2 > 50% or p-value < 0.1), a random effect model was used; otherwise, a fixed-effect model was adopted, and when the heterogeneity persisted, the leave-one-out test was done [28, 29]. In the analysis of TSH change, a subgroup analysis was done based on the baseline thyroid control status of the patients (total sample (euthyroid & non-euthyroid) and euthyroid subgroup). The different TSH baselines and the different study designs were found to be sources of heterogeneity after sensitivity analysis. Studies had wide variability regarding the baseline TSH; that’s why we analyzed the euthyroid subgroup separately to compare the different time points. We used the data of studies which started with only well controlled (Euthyroid) patients [18, 21, 23, 24]. Three timing points of the drug intake were compared according to the change in TSH after Ramadan. “Pre-iftar” means taking the drug at sunset and waiting for 30–60 min before the iftar meal. “Post-iftar” means taking the drug at least 3 h after the iftar meal with no food or beverages during this period. “Pre-suhoor” means taking the drug 30–60 min before the suhoor meal while fasting for at least 3 h before the drug intake. El-Kaissi et al. [17] study was not included in the analysis of TSH change because of the unavailability of data, but it was included in the analysis of the number of patients with TSH levels above the reference ranges. A funnel plot was generated with Review Manager Software (version 5.4) to assess publication bias.
Results
Search results
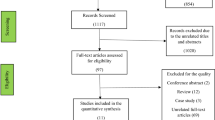
A total of 657 references were screened after removing the duplicates. Twenty studies were found relevant and sought for retrieval and full-text screening. Eight studies were found ineligible to our pre-specified criteria and were excluded. One study was excluded because of the unavailability of its full text [15]. 3 studies were added by manual search. A total of 14 studies were found eligible and included in our systematic review. The PRISMA flow chart is shown in Fig. 1.
Study characteristics
We included a total of 14 studies with a total of 1661 hypothyroid patients. All studies were comparing the thyroid functions before and after Ramadan (pre-post studies) with differences in the methodology (RCTs, prospective cohort, and retrospective cohort studies). Three studies were randomized controlled trials [17, 21, 23], 11 studies were observational [12,13,14, 16, 18,19,20, 22, 24, 25, 31]. Only 13 studies were included in the quantitative analysis as Karoli et al. did not report on any eligible data for this meta-analysis [20.]. All enrolled patients were hypothyroid and on daily levothyroxine doses. Five studies recruited only the well-controlled thyroid patients (euthyroid) [18, 21, 23,24,25], and the remaining studies didn’t specify a certain group of interest regarding the baseline thyroid status (Euthyroid and Non-euthyroid). Elsherbiny et al. is an extension of Elsherbiny et al. in which data from euthyroid patients only were included and analyzed [18, 19]. The dates of patient recruitment in the studies went from 2012 to 2020. Studies were conducted in different countries: Egypt, United Arab Emirates, Saudi Arabia, Pakistan, Qatar, Turkey, Iraq, Iran, India, and Morocco. The summary of the studies included is shown in Table 1. Most of the patients were females with a mean age of 43 years. Details of baseline characteristics of enrolled patients are provided in Table 2. Eight studies compared 2 or more timing points and investigated the effect of timing of levothyroxine intake on thyroid functions after Ramadan [14, 17,18,19, 21,22,23,24]. Definitions of time points in each group were slightly different among the studies which can be attributed to the variability in fasting hours, lifestyles, dietary habits, and prayer time. Details of these studies are shown in Table 3.
Quality assessment
By using NIH quality assessment tools [30], all studies were found to have fair quality. The details of each domain are provided in Supplementary Tables 2, 3, and 4.
Quantitative results
Change in TSH
The test for the overall effect of 12 studies showed a significant increase in TSH after Ramadan (MD = -0.72 [95% CI; -1.14, -0.31], p = 0.0006). The significance was attributed to the euthyroid subgroup (MD = -0.76 [95% CI; -1.27, -0.25], p = 0.003). Substantial heterogeneity was observed in both groups (I2 = 81%, and 65% respectively) (Fig. 2). No publication bias was observed, as shown in Supplementary Fig. 1. Another subgroup analysis was performed based on the mean baseline TSH level in the (euthyroid and non-euthyroid) group, studies with mean TSH > 3 at the baseline showed a significant decrease in the TSH after Ramadan (MD = 1.1 [95% CI; 0.09, 2.11], p = 0.03). However, studies with mean TSH < 3 at the baseline showed a significant increase in the TSH after Ramadan (MD = -1.13 [95% CI; -1.61, -0.66], p < 0.00001). No significant heterogeneity was observed in both groups (I2 = 24%, and 50% respectively) (Fig. 3A).
When examining the effect of study design on studies that included euthyroid patients only at the baseline, RCTs and observational studies showed a significant increase in the TSH after Ramadan in both groups (MD = -1.64 [95% CI; -2.32, -0.96], p < 0.00001), and (MD = -0.47 [95% CI; -0.69, -0.26], p < 0.0001) respectively. We observed no significant heterogeneity between the studies in both groups (I2 = 0%, and 0%) (Fig. 3B).
Comparison of 3 timing points of levothyroxine intake in euthyroid patients
The pooled effect of 4 studies showed that all time points of levothyroxine intake were associated with a significant increase in TSH levels after Ramadan in euthyroid patients [18, 21, 23, 24]. Pre-iftar (MD = -0.69 [95% CI; -1.03, -0.36], p < 0.0001), post-iftar (MD = -0.76 [95% CI; -1.12, -0.39], p < 0.0001), pre-suhoor (MD = -1.19 [95% CI; -2.18, -0.19], p = 0.02). No significant heterogeneity was observed (I2 = 12%, P = 0.33) (Fig. 4).
Number of patients with TSH above the reference range
The pooled effect of five studies [12, 14, 17, 22, 31] showed that the number of patients with TSH levels above the reference ranges was comparable with an insignificant increase after Ramadan (RR = 0.66, [95% CI; 0.41, 1.08], P = 0.1) with significant heterogeneity not solved by the random effects model or leave-one-out test (I2 = 80%, P = 0.0004) (Fig. 5).
Free Thyroxine (FT4) change
This analysis comprised six studies [13, 16, 21, 23, 24, 31]. Free thyroxine (FT4) was found to be stable after Ramadan with no significant difference (MD = 0.01, [95% CI; -0.03, 0.06], p = 0.59). Heterogeneity was addressed (I2 = 65%, P = 0.01), and also not resolved by the random effects model or leave-one-out test (Fig. 6).
Discussion
This study aimed to investigate the effect of Ramadan fasting on the thyroid status of patients taking levothyroxine, which was an area of interest for research, considering that Ramadan fasting is a month-long period of fasting experienced by millions of Muslims around the world each year. Our meta-analysis showed that Ramadan fasting significantly increases TSH levels in patients taking levothyroxine. However, subgroup analysis demonstrated this significant change specifically in patients with well-controlled baseline thyroid status (euthyroid) only. On the other hand, the meta-analysis of the studies that did not specify the thyroid status at baseline found an insignificant increase in TSH after Ramadan. Differences in baseline TSH and study designs were found to be the most important sources of the observed heterogeneity. Based on the sensitivity analysis, we further sub-grouped the studies accordingly. Studies with mean TSH > 3 at the baseline showed a significant decrease in the TSH after Ramadan, which can be explained by the fact that those patients might have gotten more care during Ramadan to control their thyroid status towards lower TSH levels. The meta-analysis of the studies that considered different time points of drug intake showed that timing, per se, did not affect the change in TSH levels. TSH increased in euthyroid patients after Ramadan to nearly the same degree, regardless of the time of drug intake. However, our analysis did not show a significant increase in the number of patients with TSH above the reference ranges. In addition, no significant effect of fasting on T4 levels was found.
Fasting during Ramadan causes some transient metabolic disturbances that can explain the changes in pharmacodynamics and pharmacokinetics of different drugs. Glucose increases mainly through increased gluconeogenesis in early fasting whereas triglycerides and cholesterol levels are affected by increased ketogenesis later [23,24,25,26,27,28,29,30,31,32,33]. Metabolism, especially carbohydrate and lipid metabolism, has a mutual influence relationship with TSH [34,35,36]. The nature of food consumed during Ramadan differs from other times according to Muslim customs and traditions [37]. The nature of diet can affect TSH levels [38]. Fasting, in addition, can affect body weight, which in turn has a mutual relationship with TSH levels [39]. Moreover, the physical and mental stress associated with fasting can affect TSH levels [40]. All these hypotheses can explain the changes in drug effectiveness during and after Ramadan, together with the fact that Ramadan fasting can affect patients’ compliance due to the limited hours in which they can eat and drink and the changes in their drug schedules, especially in patients taking multiple drugs. So, it has been a focus of research to study the effect of Ramadan fasting on thyroid functions, especially in hypothyroid patients, and to identify the measures by which they can maintain good thyroid control.
The most recent study, by Elsherbiny et al., found that Ramadan fasting was associated with a significant increase in TSH, which is consistent with the results of most studies included in this meta-analysis [18]. On the other hand, Zaboon et al., Dellal et al., and Pakdel et al. found that TSH levels were comparable before and after Ramadan [14, 16, 24]. Only Pakdel et al. showed a significant decrease in T4 levels. Oudgheri et al. and Elsherbiny et al., reported that 19–20% of the euthyroid patients before Ramadan turned into a dysthyroid state after Ramadan [18, 25]. This percentage was higher in other studies, including 32% in El-Kaissi et al., and 40% in Zaboon et al. [14, 15].
Choosing the optimal timing of drug intake, whether in “pre-iftar”, “post-iftar”, or “pre-suhoor” was shown to be a major controversy among the included studies. Al-Qahtani et al. concluded that taking the drug at sunset 30 min before iftar was found the least timing to affect TSH after Ramadan, which aligns with the conclusion of El-Kaissi et al., as they found no significant changes in TSH on “pre-iftar” regimen [17, 21]. In Elsherbiny et al., euthyroidism was more evident in patients who chose to take the drug 60 min before, or 3–4 h after the iftar meal. While Dabbous et al., and Sheikh et al. found that TSH change was not affected by the timing of LT4 intake, which is consistent with our finding in this meta-analysis [12, 23]. On the other hand, Dellal et al. and Zaboon et al. found no significant TSH change in all groups [14, 24]. These inconsistencies can be explained by different rates of adherence and compliance of the patients to the regimens and the precautions. Karoli et al. found that non-adherence in keeping at least a 2-h interval between meals and levothyroxine intake was significantly correlated to the variations in TSH [20]. Oudghiri et al. and Elsherbiny et al. reported the highest adherence rates and highlighted the significant association between adherence and maintaining euthyroid state [18, 19, 25]. This raises the concern of adherence as the most important factor to guarantee good thyroid control during and after Ramadan. This can be achieved by interplay between the caregiver and the patients, aiming to tailor the regimens according to their lifestyles and time schedules during Ramadan days. Other strategies have been postulated to increase compliance in patients, like changing the regimen from daily to weekly, especially in patients where compliance is a major issue [41]. Twice or thrice-per-week regimens were also compared with the standard daily dosing during Ramadan in a pilot study, and it showed promising results that should be investigated further in the future [42].
To our knowledge, this is the first systematic review and meta-analysis pooling the evidence on this point. There are a few limitations to our study; including the observational nature of most of the included studies, and the combination of RCTs and observational studies can represent a potential bias. The included studies were found to be of fair quality based on the risk of bias tools used, that’s why we cannot build a strong evidence in this area based on these results alone. Also, heterogeneity was noticed among the studies in different aspects like different TSH baselines, different indications of thyroid hormone replacement, different definitions of timing of the drug intake, different recommendations given to the patients, the different number of days fasted by the patients, different fasting hours, different TSH measuring time, and lastly and most importantly, different adherence rates. All these variabilities were supposed to be the source of the statistical heterogeneity observed in the results. We tried to address these issues by subgrouping and choosing the data that corresponds to the same baselines as much as possible. The hours of fasting can range from 10 to 20 h according to the country and the year. However, in our included studies, the maximal time difference is 4.5 h between the most eastern longitude (India) and the most western longitude (Morocco). So, the fasting hours did not differ that much, ranging from 14 to 16 h [20, 25].
In conclusion, Ramadan fasting is associated with a significant increase in TSH levels. However, achieving TSH levels above the reference range after Ramadan is not significant. Free thyroxine levels were also found to be stable after Ramadan. Timing per se (pre-iftar, post-iftar, or pre-suhoor) doesn't affect the change in TSH. No sufficient evidence supports increasing the dose of levothyroxine during or after Ramadan. However, management should be individualized. The compliance of the patients who intend to fast to the regimens and the precautions should be greatly emphasized by the medical care providers. Due to the small number of studies included, the fair quality, and the observational nature of most of the studies, more research efforts are still warranted to justify the management plan for the hypothyroid patients during Ramadan.
References
Pasha MC, Pasha HC (2016) The cardiac patient in Ramadan. Avicenna J Med 6(2):33–38. https://doi.org/10.4103/2231-0770.179547
Hassanein M, Al-Arouj M, Hamdy O et al (2017) Diabetes and Ramadan: Practical guidelines. Diabetes Res Clin Pract 126:303–316. https://doi.org/10.1016/j.diabres.2017.03.003
(2013) 9788178981413: The Holy Quran (7x4.8 Inches) - Abdullah Yusuf Ali (Translator): 8178981416 - AbeBooks [Internet]. [cited 2022 Dec 2]. Available from: https://www.abebooks.com/9788178981413/Holy-Quran-7x4.8-Inches-Abdullah-8178981416/plp
Al-Arouj M, Bouguerra R, Buse J et al (2005) Recommendations for Management of Diabetes During Ramadan. Diabetes Care 28(9):2305–2311. https://doi.org/10.2337/diacare.28.9.2305
Mughal F (2014) Ramadan: what it means for general practice. Br J Gen Pract 64(624):356–356. https://doi.org/10.3399/bjgp14X680605
Sherif I, Lakhdar A (2010) Ramadan fasting and the medical patient: Consensus is welcome but more evidence is needed. Ibnosina J Med Biomed Sci 2(05):237–239
Azizi F (2015) Islamic Fasting and Thyroid Hormones. Int J Endocrinol Metab 13(2) [Internet]. [cited 2022 Dec 2]. Available from: Environmental Factors Affecting Thyroid-Stimulating Hormone and Thyroid Hormone Levels. https://doi.org/10.5812/ijem.13(2)2015.29248
Hays MT (1988) Thyroid Hormone and the Gut. Endocr Res 14(2–3):203–224. https://doi.org/10.3109/07435808809032986
Parretti H, Okosieme O, Vanderpump M (2016) Current recommendations in the management of hypothyroidism: developed from a statement by the British Thyroid Association Executive. Br J Gen Pract 66(651):538–540. https://doi.org/10.3399/bjgp16X687493
Celi FS, Zemskova M, Linderman JD et al (2011) Metabolic Effects of Liothyronine Therapy in Hypothyroidism: A Randomized, Double-Blind, Crossover Trial of Liothyronine Versus Levothyroxine. J Clin Endocrinol Metab 96(11):3466–3474. https://doi.org/10.1210/jc.2011-1329
Hepp Z, Wyne K, Manthena SR et al (2018) Adherence to thyroid hormone replacement therapy: a retrospective, claims database analysis. Curr Med Res Opin 34(9):1673–1678. https://doi.org/10.1080/03007995.2018.1486293
Sheikh A, Mawani M, Mahar SA (2018) Impact of Ramadan Fasting on Thyroid Status and Quality of Life in Patients with Primary Hypothyroidism: a Prospective Cohort Study from Karachi, pakistan. Endocr Pract 24(10):882–888. https://doi.org/10.4158/ep-2018-0038
Koca A, Dağdevi̇Ren M, Altay M (2020) Should the dose of levothyroxine be changed in hypothyroidism patients fasting during Ramadan? Turk J Med Sci 50(4):784–788. https://doi.org/10.3906/sag-1911-28
Zaboon IA, Alidrisi HA, Hussein IH et al (2020) Best Time for Levothyroxine Intake in Ramadan (THYRAM): Basrah Experience. Int J Endocrinol Metab 18(2) [Internet]. [cited 2022 Dec 2]. https://doi.org/10.5812/ijem.94325
El-Kaissi S, Dajani R, John TJLS et al (2020) Impact of Lifestyle Changes During Ramadan on Thyroid Function Tests in Hypothyroid Patients Taking Levothyroxine. Endocr Pract 26(7):748–753. https://doi.org/10.4158/ep-2019-0505
Pakdel R, Mohebbi M, Rezaie N, Hadjzadeh M (2020) Ramadan Fasting and Thyroid Hormone Levels in Women with Hypothyroidism [Internet]. [cited 2022 Dec 2]. https://doi.org/10.22038/jnfh.2019.42779.1217
El-Kaissi S, Abdel Wareth L, Dajani R et al (2021) Levothyroxine Administration during Ramadan: A Prospective Randomized Controlled Trial. Eur Thyroid J 10(6):455–60. https://doi.org/10.1159/000517706
Elsherbiny TM (2022) Impact of fasting on thyrotropin and thyroid status during Ramadan in 292 previously well controlled hypothyroid patients. IFTAR study. Endocrine [Internet]. [cited 2022 Dec 2]. https://doi.org/10.1007/s12020-022-03242-1
Elsherbiny TM (2021) Preference, Adherence, and Maintenance of Euthyroidism Using 3 Different Regimens of Levothyroxine Intake during the Fasting Month of Ramadan. Dubai Diabetes Endocrinol J 27(1):6–13. https://doi.org/10.1159/000513927
Karoli R, Fatima J, Chandra A, Mishra P (2013) Levothyroxine replacement and Ramadan fasting. Indian J Endocrinol Metab 17(2):318. https://doi.org/10.4103/2230-8210.109700
Al-Qahtani KM, Aldeeri IA, Alshaibi AM et al (2022) Optimal Timing of Thyroid Hormone Replacement During Ramadan Fasting: A Randomized Controlled Trial in Patients with Prior Total Thyroidectomy. Thyroid 32(9):1029–1036. https://doi.org/10.1089/thy.2022.0110
Ghaffar T, Ahmad I, Bukhari AAS (2021) Effect of the Timing of Thyroxine Intake on Thyroid Stimulating Hormone Levels in Ramadan
Dabbous Z, Al Owainati B, Darwish S et al (2019) A Prospective Study Comparing Two-Time Points of Thyroid Hormone Replacement during the Holy Month of Ramadan. Int J Endocrinol 2019:1–5. https://doi.org/10.1155/2019/9843961
Dellal FD, Ogmen B, Ozdemir D et al (2020) Effect of Ramadan Fasting on Thyroid Hormone Levels in Patients on Levothyroxine Treatment. J Coll Physicians Surg Pak (JCPSP) 30(10):1009–1014. https://doi.org/10.29271/jcpsp.2020.10.1009
Oudghiri DM, Motaib I, Elamari S (2022) Ramadan and Hypothyroidism: Impact of Ramadan Fasting on Thyroid Status. Med Clin Res Open Access 3(1):1–5
Page MJ, McKenzie JE, Bossuyt PM et al (2020) statement: an updated guideline for reporting systematic reviews. BMJ 2021
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A (2016) Rayyan—a web and mobile app for systematic reviews. Syst Rev 5(1):210
(2022) Cochrane Handbook for Systematic Reviews of Interventions [Internet]. Version 6.3. [cited 2022 Dec 2]. Available from: https://training.cochrane.org/handbook
Higgins JPT (2003) Measuring inconsistency in meta-analyses. BMJ 327(7414):557–560
(2021) Study Quality Assessment Tools | NHLBI, NIH [Internet]. [cited 2022 Dec 2]. Available from: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools
Alkaf B, Siddiqui M, Ali T et al (2022) Ramadan Fasting and Changes in Thyroid Function in Hypothyroidism: Identifying Patients at Risk. Thyroid 32(4):368–375. https://doi.org/10.1089/thy.2021.0512
Beltaief K, Bouida W, Trabelsi I et al (2019) Metabolic effects of Ramadan fasting in patients at high risk of cardiovascular diseases. Int J Gen Med 12:247–254. https://doi.org/10.2147/IJGM.S172341
Maughan RJ, Fallah J, Coyle EF (2010) The effects of fasting on metabolism and performance. Br J Sports Med 44(7):490–494. https://doi.org/10.1136/bjsm.2010.072181
Wang JJ, Zhuang ZH, Shao CL et al (2021) Assessment of causal association between thyroid function and lipid metabolism: a Mendelian randomization study. Chin Med J (Eng) 134(9):1064–1069. https://doi.org/10.1097/CM9.0000000000001505
Korzeniowska KA, Brzeziński M, Szarejko K et al (2019) The association of thyroid-stimulating hormone (TSH) and free thyroxine (fT4) concentration levels with carbohydrate and lipid metabolism in obese and overweight teenagers. Endokrynolog Pol 70(2):172–178. https://doi.org/10.5603/ep.a2018.0090
Mullur R, Liu YY, Brent GA (2014) Thyroid Hormone Regulation of Metabolism. Physiol Rev 94(2):355–382. https://doi.org/10.1152/physrev.00030.2013
Shatila H, Baroudi M, El Sayed Ahmad R et al (2021) Impact of Ramadan Fasting on Dietary Intakes Among Healthy Adults: A Year-Round Comparative Study. Front Nutr 8:689788. https://doi.org/10.3389/fnut.2021.689788
Babić Leko M, Gunjača I, Pleić N, Zemunik T (2021) Environmental Factors Affecting Thyroid-Stimulating Hormone and Thyroid Hormone Levels. Int J Mol Sci 22(12):6521. https://doi.org/10.3390/ijms22126521
Liu G, Liang L, Bray GA et al (2017) Thyroid hormones and changes in body weight and metabolic parameters in response to weight loss diets: the POUNDS LOST trial. Int J Obes 41(6):878–886. https://doi.org/10.1038/ijo.2017.28
Tsigos C, Chrousos GP (2002) Hypothalamic–pituitary–adrenal axis, neuroendocrine factors and stress. J Psychosom Res 53(4):865–871. https://doi.org/10.1016/s0022-3999(02)00429-4
Rajput R, Pathak V (2017) The Effect of Daily versus Weekly Levothyroxine Replacement on Thyroid Function Test in Hypothyroid Patients at a Tertiary Care Centre in Haryana. Eur Thyroid J 6(5):250–254. https://doi.org/10.1159/000477348
Elsherbiny T (2022) Twice or thrice weekly versus daily thyroxine in hypothyroid fasting ramadan: A pilot study. Indian J Endocrinol Metab 26(3):265. https://doi.org/10.4103/ijem.ijem_1_22
Acknowledgements
All thanks and glory belong to Allah, who allows those whose health would be adversely affected by fasting to refrain from doing so. Also, we are grateful to Prophet Mohammed for inspiring us to provide free services to others that may lessen their suffering and save their lives.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Author information
Authors and Affiliations
Contributions
EMR, and MMB: conceptualization and methodology. MMB, ARY, NAE, HB, MAQ, AAM, and EMR: data collection, screening, and data extraction. EMR, MMB, ARY, NAE, HB, and MAQ: quality assessment. EMR, MMB, AAM, ARY, HB, NAE, and MAQ: writing - original draft. EMR: finalization, analysis, and supervision. All authors reviewed the manuscript and approved it for publication.
Corresponding author
Ethics declarations
Ethical approval
Not applicable.
Consent to participate
Not applicable.
Consent to publish
Not applicable.
Competing interests
The authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Belal, M.M., Youssef, A.R., Baker, H. et al. Effect of Ramadan fasting on thyroid functions in hypothyroid patients taking levothyroxine: a systematic review and meta-analysis. Ir J Med Sci 193, 741–753 (2024). https://doi.org/10.1007/s11845-023-03526-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-023-03526-z