Abstract
Objective
This study was undertaken to assess and evaluate adherence to secondary prevention recommendations and risk factor modifications among a patient cohort at a single-tertiary centre in Ireland, following coronary artery bypass grafting (CABG).
Methods
This is a retrospective observational study analysing patients who had CABG from 2015 to 2020, identified via the Adult Cardiac Surgery Database. Patients were asked a number of questions either over the phone or via postal survey, regarding blood pressure, cholesterol control, adherence to medication, attendance at cardiac-rehab and lifestyle factors. Any repeat interventions following CABG were noted.
Results
A total of 540 patients were invited to take part in this study. One hundred seventy-three patients consented to participate, ranging from 47 to 86 years old. Postoperatively, 59% of participants attended cardiac rehab. 90.2% of patients report taking a statin, 91.3% report taking an antiplatelet, 77.4% report taking a β-blocker and 75.7% take an antihypertensive. 93.1% of patients questioned in this study reported full compliance with their daily medications. Sixteen patients continue to have hypertension despite their current regimen. Thirteen patients continue to have hypercholesterolemia despite their current prescription. 62.4% of participants have quit smoking with only 4.6% remaining current smokers. No patients required re-operation, and eight patients required stenting. Compliance with diet and exercise modifications was suboptimal.
Conclusion
In this patient population, adherence to medication and control of risk factors is acceptable. However, there is room for improvement in terms of attendance at cardiac rehab (59%) and maintenance of a healthy lifestyle post-CABG.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Coronary artery disease (CAD) is a highly prevalent condition in Ireland today; affecting 1% of 45–54-year-olds, 4% of 55–64-year-olds, 5% of 65–74-year-olds and 8% of over 75 year olds in 2019 [1]. Since the early 2000s, there has been a dramatic decline in CAD mortality rates with ~ 60% of this decline being attributable to increased uptake of secondary prevention, with improvements in CAD risk factor modifications contributing to ~ 30% of the decline [2]. Despite this, diseases of the circulatory system continue to account for one in four deaths in Ireland today; 27.5% of total deaths in Ireland in 2020 [3].
Patients who have undergone coronary artery bypass grafting (CABG) by definition have more severe and diffuse CAD. In this cohort, secondary prevention is an important pillar in treatment postoperatively. Aggressive secondary prevention serves to slow down progression of native vessel disease [4] and has been shown to improve graft patency, especially in vein grafts [5]. The British Cardiac Society recommends a number of cardioprotective therapies for prevention of CAD progression in people with atherosclerotic cardiovascular disease as follows: aspirin 75 mg daily for all patients, a β-blocker for all patients following a myocardial infarction, an antihypertensive agent (such as an ACE inhibitor or calcium channel blocker) for all high-risk CAD patients whose blood pressure is not at target, a lipid-lowering agent (such as a statin) for all patients with symptomatic atherosclerotic disease and an anticoagulant in patients at high risk of systemic embolization [6]. The therapeutic target ranges are listed below in Table 1. A number of lifestyle changes are also recommended, including smoking cessation, undertaking 30 min of physical exercise most days of the week as well as dietary modifications. In addition to the risk modifications listed above, the British Cardiac Society also recommends that a comprehensive cardiovascular prevention and rehabilitation programme should be offered to all patients with atherosclerotic disease (Table 1).
This study was undertaken to assess and evaluate adherence to these secondary prevention recommendations and risk factor modifications among a patient cohort at a single-tertiary centre in Ireland.
Methods
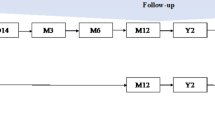
This study was a retrospective observational review of patients who had undergone CABG in an Irish tertiary centre, under two consultant surgeons (ZC & HJ), during a time period of 2015 to 2020. Ethical approval was sought, and this study was approved by the Institutional Review Board. Five hundred fifty-six patients were identified via the Adult Cardiac Surgery Database. Sixteen patients who had passed away, as per the hospital’s records and according to RIP.ie, were excluded (Fig. 1). The remaining 540 patients were each sent a letter of invitation via post. One hundred seventy-three patients (32%) consented to participation, ranging in age from 47 to 86 years old, 147 (85%) of whom were male and 26 (15%) of whom were female. The participants who had consented to participate in the study answered the questionnaire either over the phone or on a paper survey via post. The data was collected and analysed using Microsoft Excel (Microsoft Corp, Redmond, WA).
The questions encompassed adherence to cardioprotective therapies prescribed post-CABG. The prescription of a number of medications was assessed, namely antiplatelet, lipid-lowering, antihypertensive and rate control medications. The participants were also asked about attendance at primary care, diabetic status, blood pressure (as measured at their last GP check or indeed on home monitoring) and cholesterol control (as per their most recent blood test with their GP). Lifestyle factors such as smoking history, diet and exercise were discussed. Attendance at a cardiac rehabilitation programme and any re-interventions since their CABG operation were noted.
Patient involvement
The design of this study was informed by a participant preference to have a multitude of options for responding to the survey. Anxiety surrounding the recall or pronunciation of drug names was eliminated by the addition of the option to take part via paper questionnaire, allowing participants to transcribe drug names without undue stress.
Once the data from this study has been published, we intend to circulate the main results to participants via a patient information leaflet in the post or via email. We will seek patient involvement regarding which method would be most suitable for distribution of the results and to ensure the language used is pitched appropriately.
Results
Of the 540 patients who were invited to participate, 173 patients (32%) consented to the study. The age range of participants was 47–86 years old. There were 147 males (85%) and 26 females (15%) included in this study.
Adherence to cardioprotective therapies (Fig. 2)
93.1% (n = 161) of this patient group report full compliance with their cardioprotective therapies. Of the patients who did not report full medication compliance, 6.4% (n = 11) of the participants report taking their medications as prescribed less than seven but more than four days per week, with one patient (0.6%) taking their medications as prescribed between one and 3 days per week.
91.3% of this group (n = 158) take an anti-platelet agent. 90.2% (n = 156) take a lipid-lowering agent. 75.7% (n = 131) report taking a regular anti-hypertensive agent with 77.5% (n = 134) on a β-blocker. Two patients (1.2%) did not provide information regarding their prescription.
Attendance at primary care & cardiac rehabilitation
Attendance at primary care varied among the group with 11% (n = 19) participants attending within the week prior to taking part in the study, 23.7% (n = 41) attending within the previous month, 37.6% (n = 65) within the previous 6 months and 14.4% (n = 25) within the last year. This totals 86.7% of the group being seen in primary care within the previous 12 months.
9.2% (n = 16) of participants attended repeat follow-up visits at this tertiary centre within the 12 months prior to the study. The remaining majority of participants had not attended since their outpatient appointment ranging from 6 to 12 weeks postoperatively.
59% (n = 102) of this patient population attended a cardiac rehabilitation programme in the weeks following their CABG, and 38.2% (n = 66) did not. A further 2.9% (n = 5) patients were not sure.
Risk factor modification (Fig. 3)
Only 5.7% of this patient group (n = 10) had none of the following cardiovascular risk factors; hypertension, hypercholesterolemia, diabetes or smoking history. A further fourteen patients (8.1%) only had a smoking history as a risk factor for CAD.
9.2% (n = 16) of this group report ongoing hypertension, above target range, despite their current anti-hypertensive regimen, as measured at their last primary care appointment or indeed using home monitors. 53.2% (n = 92) report good control on their current regime. 10.4% (n = 18) do not know their hypertensive status, and 27.2% (n = 47) report never having had high blood pressure.
7.5% (n = 13) report ongoing hypercholesterolemia, above target range, despite their current lipid-lowering prescription, as measured on their last blood test. 59% (n = 102) report cholesterol levels within target range on their current regime. 16.8% (n = 29) do not know their cholesterol status, and a further 16.8% (n = 29) report never having been diagnosed with hypercholesterolemia or hyperlipidaemia.
Diabetic status (Fig. 4)
In terms of diabetic status, 47.2% of patients were diabetic. 2.3% (n = 4) had type 1 diabetics mellitus, on lifelong insulin. Of the remaining, 29.5% (n = 51) who had type 2 diabetes mellitus, fifteen of whom (8.7%) are diet- and exercise-controlled, and twenty-eight of whom (16.2%) take an antiglycemic agent alone with a further eight patients (4.6%) requiring both an antiglycemic agent and insulin. 14.5% (n = 25) did not know their diabetic status.
Smoking status
Of these 173 participants, 32.9% (n = 57) were never smokers. 62.4% (n = 108) were previous smokers but had quit either prior to or since their CABG. 4.6% (n = 8) participants remained current cigarette smokers.
Of those with a smoking pack year history, both the mean and median was 11.5 pack years. The average cigarettes smoked per day was 25, with a maximum of 60 cigarettes per day. The average duration of smoking history was 11 years with a maximum of 60 years. Of the subgroup who remain current smokers (4.6%, n = 8), the mean pack year history was 27.6 years with a median of 17.5 years. One patient (0.6%) has commenced vaping since quitting smoking.
Diet and exercise
38.2% (n = 66) of this patient group report exercising on a daily basis. 27.2% (n = 47) exercise between 3 and 4 times per week and 17.3% (n = 30) exercise 1 and 2 times per week. 9.2% (n = 16) of the group report exercising very infrequently (1–2 times per month) with 6.9% (n = 12) of the group not exercising at all. Two patients (1.2%) were not sure if any physical activity they were engaging in would be considered ‘exercise’.
56.6% (n = 98) report eating a healthy diet ‘most of the time’. 32.4% (n = 56) report eating a healthy diet ‘some of the time’. 6.9% (n = 12) report rarely making any effort in terms of dietary modifications, and 2.9% (n = 5) make no effort at all. Two participants (1.2%) were not sure.
Repeat interventions post-CABG
Following their CABG, eight patients (4.6%) required re-stenting. No patients required re-operation.
Discussion
Risk factor modification, adherence to cardioprotective therapies and therapeutic targets
Aggressive secondary prevention serves to slow down progression of native vessel disease [4] and has been shown to improve graft patency especially in vein grafts [5] which is particularly important among this patient cohort who by the very nature of requiring CABG are deemed to have high-risk atherosclerotic CAD.
Adherence to medication among this patient group is acceptable with 93.1% reporting full compliance. The British Cardiac Society recommend that all patients with atherosclerotic cardiovascular disease take aspirin 75 mg daily to reduce the incidence of vein graft occlusion, and this is true of 91.3% of this group.
Keeping in mind that lipid-lowering therapy is one of the mainstays of treatment in order to maintain graft patency following CABG, it is positive to note that three quarters of the patient group (75.7%) have cholesterol levels within the target range [7, 8]. Statin resistance has often been described in the literature [9,10,11] and perhaps has a role to play with the cohort of 7.5% of participants who report ongoing hypercholesterolemia despite current regimen. Additionally, of the eleven patients who report poor medication compliance (that is taking their medications as prescribed less than 7 days per week but more than 4 days per week), when asked the reason for missing doses, many of them note forgetting or skipping their night-time statin. Given that hyperlipidaemia following CABG has been shown to be an independent predictor of future coronary events [12], this should be addressed in all post-CABG patients.
Regarding the 9.2% of participants who report ongoing hypertension despite their current regimen, this may include those who were non-adherent, those with white coat hypertension and those with resistant hypertension, which is quoted as affecting 6.5–14.8% of treated hypertensives [13, 14]. Research has demonstrated that hypertension is associated with an increase in mortality after CABG [15]; thus, it remains an important pillar of secondary prevention.
In light of the current COVID-19 pandemic, a subgroup of participants reported not being able to attend their primary care for their annual review, thus resulting in a proportion of participants who did now know their hypertensive status (10.4%) or their lipid profile status (16.8%).
Attendance at cardiac rehabilitation
The British Cardiac Society recommends that a comprehensive cardiovascular prevention and rehabilitation programme should be offered to all patients with atherosclerotic disease [6]. Just over half of this group (59%) attended a cardiac rehabilitation programme in the weeks following their CABG. In the modern technological era, perhaps there is a possibility for some of the cardiac rehabilitation programme to be available online, thus increasing the availability of the rehabilitation programme material and potentially reducing the rates of non-attendance for those whose rehabilitation programme was cancelled due to COVID-19 pandemic (3.5%) or geographical distance (0.6%). This is supported by the fact that participation in cardiac rehabilitation post-CABG has been shown to lead to a better prognosis and reduced cardiovascular mortality [16, 17].
Lifestyle factors
Over half of this group (62.4%) had a smoking history, thus highlighting smoking as a potentiator for atherosclerosis, particularly in the subgroup of participants whose only risk factor was current cigarette smoking (14%) [18]. However, postoperatively, the majority of this patient group (95.4%) do not currently smoke which is a tribute to the excellent smoking cessation teams both at our tertiary centre and in primary care services. It is well described in the current literature that smoking cessation following CABG significantly reduces adverse outcomes and long-term mortality [19, 20].
Interestingly, of the subgroup of patients who have type 2 diabetes mellitus (29.5%), adherence to a daily exercise regime was lower than that of the group as a whole (31.1 vs 38.2%), as was compliance with eating a healthy diet (43.1 vs 56.6%). These lifestyle modifications are a mainstay of treatment of type 2 diabetes and are simultaneously key to preventing progression of atherosclerosis, thus leading to regression of native vessel disease [21,22,23]. There is room for improvement in this patient cohort, and a focus on improvement in lifestyle factors could be of benefit from both a postoperative surgical perspective as well as a general medical perspective.
Repeat interventions post-CABG
The number of patients who required re-intervention in the form of PCI (n = 8) is too small to meaningfully analyse any risk factors for reintervention in this study population. One patient had uncontrolled hypertension, and one was still smoking. Interestingly, none of the patients who needed PCI post-CABG adhered to a regular exercised regimen.
Conclusions, limitations, and recommendations
While adherence to cardioprotective therapies and control of risk factors such as blood pressure, cholesterol and smoking status among this patient group appears to be acceptable, there is room for patient education regarding lifestyle factors such as the importance of cardiac rehabilitation as well as diet and exercise modifications. This is particularly evident amongst those with type 2 diabetes. Primary preventative measures such as education in the community at a school level regarding the detrimental long-term effects of smoking on cardiovascular status should be initiated and encouraged.
8.7% of participants do not take an anti-platelet; however, it was not clarified during the study whether this cohort take an anti-coagulant instead, thus perhaps the percentage of participants on an anti-thrombotic regimen may in fact by higher than 91.3%. This should be accounted for if there were to be a follow up/part two of this study.
Of note that the participation rate among invited patients was 32% perhaps give way to some participation bias. This low response rate may be attributable to the fact that the study was done via postal survey, thus leading to a potential for selection bias. The question style format used also relies on participant honesty when responding which becomes particularly relevant regarding smoking status [24,25,26].
Abbreviations
- CABG:
-
Coronary artery bypass grafting
- CAD:
-
Coronary artery disease
References
IH238 Prevalence of Coronary Artery Disease or Angina Pectoris in 2019 [Internet] (2019) [cited 24/08/2021]
Marasigan V, Perry I, Bennett K et al (2020) Explaining the fall in Coronary Heart Disease mortality in the Republic of Ireland between 2000 and 2015 - IMPACT modelling study. Int J Cardiol 310:159–61
VSD09 Deaths Occuring in 2020; CSO statistical publication [Internet] (2020) [cited 24/08/2021]
O’Keefe JH, Carter MD, Lavie CJ (2009) Primary and secondary prevention of cardiovascular diseases: a practical evidence-based approach. Mayo Clin Proc 84(8):741–757
Kulik A, Ruel M, Jneid H et al (2015) Secondary prevention after coronary artery bypass graft surgery: a scientific statement from the American Heart Association. Circulation 131(10):927–964
British Cardiac Society BHS (2005) Diabetes UK, HEART UK, Primary Care Cardiovascular Society, The Stroke Association. JBS 2: Joint British Societies' guidelines on prevention of cardiovascular disease in clinical practice. 91(suppl 5):v1-v52
Kulik A, Abreu AM, Boronat V, Ruel M (2020) Impact of lipid levels and high-intensity statins on vein graft patency after CABG: Midterm results of the ACTIVE trial. J Card Surg 35(12):3286–3293
Kulik A, Voisine P, Mathieu P et al (2011) Statin therapy and saphenous vein graft disease after coronary bypass surgery: analysis from the CASCADE randomized trial. Ann Thorac Surg 92(4):1284–90; discussion 90–1
Reiner Z (2014) Resistance and intolerance to statins. Nutr Metab Cardiovasc Dis 24(10):1057–1066
Karr S (2017) Epidemiology and management of hyperlipidemia. Am J Manag Care 23(9 Suppl):S139–S148
Durrington P (2003) Dyslipidaemia. Lancet (London, England) 362(9385):717–731
Leviner DB, Zafrir B, Jaffe R et al (2020) Impact of Modifiable Risk Factors on Long-Term Outcomes after Coronary Artery Bypass Surgery. Ann Thorac Surg
Sinnott SJ, Smeeth L, Williamson E, Douglas IJ (2017) Trends for prevalence and incidence of resistant hypertension: population based cohort study in the UK 1995–2015. BMJ (Clinical research ed) 358:j3984
Judd E, Calhoun DA (2014) Apparent and true resistant hypertension: definition, prevalence and outcomes. J Hum Hypertens 28(8):463–468
Nalysnyk L, Fahrbach K, Reynolds MW et al (2003) Adverse events in coronary artery bypass graft (CABG) trials: a systematic review and analysis. Heart (British Cardiac Society) 89(7):767–772
Anderson L, Thompson DR, Oldridge N et al (2016) Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev 2016(1):Cd001800
Origuchi H, Itoh H, Momomura SI et al (2020) Active Participation in Outpatient Cardiac Rehabilitation Is Associated With Better Prognosis After Coronary Artery Bypass Graft Surgery - J-REHAB CABG Study. Circ J 84(3):427–435
Ambrose JA, Barua RS (2004) The pathophysiology of cigarette smoking and cardiovascular disease: an update. J Am Coll Cardiol 43(10):1731–1737
Masoudkabir F, Yavari N, Pashang M et al (2020) Smoking Cessation After Surgery and Midterm Outcomes of Surgical Revascularization. Ann Thorac Surg 109(6):1874–1879
Benedetto U, Albanese A, Kattach H et al (2014) Smoking cessation before coronary artery bypass grafting improves operative outcomes. J Thorac Cardiovasc Surg 148(2):468–474
Ornish D, Brown SE, Scherwitz LW et al (1990) Can lifestyle changes reverse coronary heart disease? The Lifestyle Heart Trial. Lancet (London, England) 336(8708):129–133
Kirwan JP, Sacks J, Nieuwoudt S (2017) The essential role of exercise in the management of type 2 diabetes. Clevel Clin J Med 84(7 Suppl 1):S15-s21
Magkos F, Hjorth MF, Astrup A (2020) Diet and exercise in the prevention and treatment of type 2 diabetes mellitus. Nat Rev Endocrinol 16(10):545–555
Williams J, Rakovac I, Loyola E et al (2020) A comparison of self-reported to cotinine-detected smoking status among adults in Georgia. Eur J Pub Health 30(5):1007–1012
Volk RJ, Mendoza TR, Hoover DS et al (2020) Reliability of self-reported smoking history and its implications for lung cancer screening. Preventive Med Reps 17
Stelmach R, Fernandes FL, Carvalho-Pinto RM et al (2015) Comparison between objective measures of smoking and self-reported smoking status in patients with asthma or COPD: are our patients telling us the truth? Jornal brasileiro de pneumologia : publicacao oficial da Sociedade Brasileira de Pneumologia e Tisilogia 41(2):124–132
Funding
This study did not receive any source of financial support and has no industry affiliations.
Author information
Authors and Affiliations
Contributions
I am extremely appreciative for the advice and direction from Mr. Seyed Hossein Javadpour during this research study. His advice and support were crucial to the successful completion of the project, and for that, I am very thankful. A special thank you to Mohammad AlAdalieh for his time and efforts during the data collection phase of this study as well as to Mr. Jehan Zeb Chughtai. I would like to also like to acknowledge and thank our participant group for their input and participation in this study. Their vital contribution to this project was much appreciated.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Questions
What is already known about this subject?
Aggressive secondary prevention after CABG serves to slow down progression of native vessel disease, maintain graft patency, and reduce cardiovascular mortality.
What does this study add?
This study describes adherence to secondary prevention recommendations among a patient cohort at a single tertiary centre in Ireland, highlighting which British Cardiac Society guidelines are being met and which areas need improvement.
How might this impact on clinical practice?
This study sheds the light on the fact that there is a need for increased patient education and involvement regarding modification of lifestyle factors and attendance at cardiac rehabilitation following CABG.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Keating, T., AlAdalieh, M., Chughtai, Z. et al. Adherence to secondary prevention recommendations after coronary artery bypass graft surgery. Ir J Med Sci 192, 1103–1108 (2023). https://doi.org/10.1007/s11845-022-03129-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-022-03129-0