Abstract
Background
The global healthcare activity including neurosurgical services has been significantly impacted by the COVID-19 pandemic.
Aim
Compare neurosurgical theatre activity from 2019 (pre-pandemic) to that of the subsequent pandemic years (2020–2021) and explore how each wave of COVID-19 infection impacted activity levels.
Methods
A retrospective analysis of neurosurgical theatre activity at the National Neurosurgical Centre of Ireland was performed from 1 January 2019 till 31 December 2021. The extracted data included date, surgical procedure, demographics of the patient and case scheduling (elective or emergency).
Results
In total, 6139 neurosurgical procedures were recorded throughout the study period. Two thousand one hundred forty-four neurosurgical procedures were recorded in 2019, 2052 in 2020 and 1943 in 2021 corresponding to a reduction in theatre activity by 4.3% and 9.4% in 2020 and 2021 respectively. The lowest number of monthly caseloads was recorded in April 2020 during the first wave of the pandemic. The first quarter of 2021 recorded the lowest number of quarterly surgical procedures over the entire 3-year period contributing to just 19.4% of 2021 caseload. Subgroup analysis showed a significant reduction in trans-sphenoidal pituitary surgeries post-pandemic by 36% and 44% in 2020 and 2021 respectively.
Conclusions
Despite the exceptional stress imposed on our institution by COVID-19, the neurosurgical service managed to maintain comparable activity levels to 2019. The 2021 activity levels were more significantly impacted with 9.4% reduction when compared with pre-pandemic figures in 2019. Institutions need to develop a robust emergency plan to reduce the impact of any subsequent pandemics on healthcare delivery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
COVID-19 has had an un-precedented impact on global healthcare activity resulting in the postponement of many elective services during successive waves of infection This has been compounded by the fact that some services were unable to return to full levels of pre-pandemic activity in the intervening period between waves [1].
In Ireland, the first PCR-positive case of COVID-19 was reported on 26 February 2020 and the first national public health restrictions were introduced on 12 March 2020, a day after the WHO declared COVID-19 to be a global pandemic [2, 3].
Given the potential consequences of delayed surgery, we sought to examine and compare neurosurgical theatre activity from 2019 (pre-pandemic) to that of the subsequent pandemic years (2020–2021) and explore how each wave of COVID-19 infection impacted activity levels.
Materials and methods
We conducted a retrospective, single institution, observational cohort study. The institution is the Irish National Neurosurgical Centre in Beaumont Hospital, Dublin. It is a large tertiary referral centre with over 2,000 neurosurgical procedures typically performed per annum. We reviewed the neurosurgical theatre activity from 1 January 2019 to 31 December 2021 and examined the total number of operations performed daily throughout the study period. Theatre activity is electronically recorded on a specific operating theatre computer system. Data was obtained from this system, with assistance from the IT Department. The extracted data included date of surgery, type of surgical procedure, age and gender of the patient and case scheduling (elective or emergency).
All patients who underwent neurosurgical procedures in the Operating Theatre Department during the study period were included. Patients who underwent interventional neuroradiology procedures were excluded, as different booking systems used in the Radiology Department meant the reliability of capturing accurate data in this patient cohort was not guaranteed. Neurosurgical patients who underwent non-neurosurgical procedures were also excluded.
Subgroup analysis was performed on the type of neurosurgical procedure completed, i.e. craniotomy for space occupying lesions (SOL), brain biopsy, intracranial vascular procedures, spinal surgery, CSF diversion surgery, trans-sphenoidal pituitary resections and vagal nerve stimulator implantation surgery.
Statistical analysis
Statistical analysis was performed using IBM SPSS (Statistical Package for the Social Science; IBM Corp, Armonk, NY, USA) release 22 for Microsoft Windows. Data were described in terms of frequencies (number of cases) and percentages and compared using Chi-square (χ2) test. Two-sided p values less than 0.05 were considered statistically significant.
Results
In total, 6,139 neurosurgical procedures were recorded throughout the study period. Patient demographics are listed in Table 1. Two thousand one hundred forty-four neurosurgical procedures were recorded in 2019. This was pre-pandemic and served as baseline activity levels. Two thousand fifty-two neurosurgical procedures were performed in 2020, with 1943 neurosurgical procedures performed in 2021. Theatre activity was reduced by 4.3% in 2020, with a reduction of 9.4% in 2021 when compared with pre-pandemic baseline figures in 2019. The downward trend in the total number of neurosurgical operations performed following the onset of the pandemic included both elective and emergency procedures.
Subanalysis of quarterly periods showed that the first quarter of 2021 recorded the lowest number of neurosurgical procedures over the entire 3-year period, contributing to just 19.4% of the total cases performed in 2021. In 2020, the second quarter recorded 22.6% of the total activity for that year, while the third quarter recorded 27.9% (Table 2).
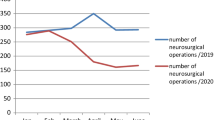
Analysis of the monthly activity showed a sharp reduction in the number of procedures performed in April 2020 (Fig. 1). This coincided with the first wave of the pandemic. However, activity levels returned to normal in May 2020, with an increase in activity observed over the following months. Activity again reduced progressively from December 2020 to April 2021, before returning to pre-pandemic levels again in May 2021. This reduction coincided with the third wave of the pandemic. The median number of the monthly neurosurgical procedures performed decreased from 177 (164–191) in 2019 to 176 (84–216) in 2020 and 169 (84–216) in 2021.
Subspeciality analysis showed that spinal surgeries accounted for 20.5% of the total activity in 2019. Spinal surgeries constituted 24.8% of cases in 2020 and 21.2% in 2021 (Table 3). Craniotomy for SOL was the indication for surgery in 19.1% of cases in 2019, 19.2% in 2020 and 20.9% in 2021 (P = 0.273). There was a notable and statistically significant reduction in trans-sphenoidal pituitary surgeries performed post-pandemic onset, decreasing by 36% and 44% (P = 0.015) in 2020 and 2021 respectively. Brain biopsy surgeries were also reduced, by 15.9% in 2020 and 25.5% in 2021 (P = 0.228).
Discussion
Our institution endeavoured to maintain full neurosurgical theatre activity throughout the pandemic. The data showed that this was almost achieved throughout 2020 with statistically insignificant reduction of 4.3% on 2019 activity levels. However, the service was more significantly impacted in 2021 with a 9.4% reduction on pre-pandemic activity levels. The reasons for this are multifactorial with lack of beds being the most significant. Other reasons are the introduction of COVID-19 theatre policies, invalid COVID-19 swab results, staff illness or self-isolation, on the day cancellation of elective surgery due to patients contracting COVID-19 and lack of ICU capacity.
In line with general theatre practice, the neurosurgical theatres introduced several measures in response to COVID-19 with the aim of minimizing risk of infection while still running the service. These measures evolved with our evolving understanding of COVID-19 transmission and the fluctuation in community burden of disease (Figs. 2, 3).
In order to minimize risk of infection from aerosol generating procedures (AGPs), our institution mandated the use of full PPE, minimal staff in the room and a 10-min pause after intubating or extubating a patient before further staff were allowed to enter the room [4]. This was the case regardless of the patient COVID status. This has since been revised to the use of full PPE for COVID-positive or COVID-unknown patients only and the 10-min pause has been eliminated.
There was a statistically significant reduction in trans-sphenoidal pituitary surgery performed during the pandemic. This might be, at least partially, explained by the hypervigilance surrounding potential AGPs. Cases that may include the opening of an air sinus, such as trans-sphenoidal pituitary surgery or skull base surgery, are considered aerosol generating, and thus require all theatre staff to wear full PPE throughout the surgery [5]. These cases were assessed on a case-by-case basis and were postponed if there was no risk of neurological deterioration in the interim, and the risks of aerosol generation outweighed the potential benefits of proceeding.
A theatre policy on COVID-19 testing of patients was also introduced. All patients are required to have a valid COVID test result within the 72 h prior to induction. This has been the policy since March 2020. If the COVID result is unavailable, the case is either postponed or proceeds as COVID unknown. If on the COVID unknown pathway, full PPE is required by everyone in theatre throughout the procedure and the patient must be recovered in theatre before being transferred to a suitable isolation bed.
Emergency cases proceed as COVID unknown. All emergency patients are swabbed prior to induction but the procedure is not delayed awaiting results. Consequently, full PPE is required throughout emergency cases or until the pre-induction swab is reported. Swab results initially took up to 12 h to be reported but the introduction of rapid testing has reduced this timeframe to 1 h. We anticipated that the additional time required to complete these necessary measures would impact on theatre productivity and reduce overall throughput.
The two most significant periods during which service provision was impaired were in April 2020 when only 84 cases were performed and again during the first quarter of 2021.
The 84 cases performed in April 2020 constituted a reduction of 52.5% when compared to April 2019. By observing emerging trends in China, Italy and Spain, the National Health Service (Health Service Executive) prioritized the rapid expansion of hospital and ICU capacity amid very real fears that demand would outstrip supply [6]. All resources were re-directed at the expense of existing services. By the third quarter of 2020, COVID hospitalization rates had improved, and the monthly theatre throughput increased to address the backlog.
A further significant impact on service provision was seen during the period of Jan 2021 to Feb 2021. This correlates with peak COVID-19 demands on hospital resources, resulting in usage of surge capacity and a consequent lack of both ICU beds and general hospital beds. This surge followed the easing of restrictions over the 2020 Christmas period and January 24 is reported as having the highest number of COVID hospitalizations. On this day, there were 221 COVID patients admitted to the intensive care unit (ICU) nationwide, accounting for about 70% of the national ICU capacity. In addition, COVID rosters were adopted with most anaesthetic personnel relocated to the ICU. During this period, a total of 377 neurosurgical cases were completed. This was significantly less than the number of cases completed during the same timeframe in 2019 (553 cases) and 2020 (516 cases).
Regarding emergency cases, they are often time critical and thus proceeded, often being performed in full PPE. However, there was a reduction in the emergency caseload after the pandemic. This reduced demand likely reflects a reduction in the number of traumatic brain injuries (TBIs). A 17.1% reduction in trauma referrals occurred between 2019 and 2020 [7]. Interestingly, the number of road traffic accidents and head injuries secondary to interpersonal violence remained constant despite the many restrictions limiting both social interactions and the movement of people [7]. All other forms of TBIs showed a reduction in incidence with a notable 70% reduction in head injuries secondary to sports [7]. The emergency caseload peaked in the second half of 2021, surpassing even the caseload over the same period in 2019. This perhaps reflects a delay in the management of neurosurgical conditions in the first half of the year resulting in the clinical deterioration and emergent presentation of some patients.
Despite the reduction in activity levels recorded in this study, our data compares favourably with other institutions. Some neurosurgical units in London experienced a reduction in neurosurgical referrals by 33.6% and in operations by 55.6% during the first wave of COVID-19 [8]. The Veneto region in Italy reported a 30% deficit in the average number of neurosurgical procedures in March 2020 when compared with the previous year [9]. There was a reduction of 33.6% in the overall volume of all surgical activity in England and Wales in 2020 [10].
Limitations to this study include the fact that this is a retrospective, single institution, and observational study. It does not include outcome data and it does not capture data on excess neurosurgical morbidity due to delayed presentation to hospital. Presentation delays have been seen worldwide in many other emergency and time-critical events such as ischaemic stroke and myocardial infarction [11, 12]. Arising from this, one could conclude similar behaviour must be true to neurosurgical population. One study in Germany reported that patients with spinal injuries presented 48 h later in 2020 compared to the previous year, even when complaining of similar symptoms [13]. Irish GPs and emergency department consultants have also recognized this issue and have warned of the dangers of delayed presentations, imploring patients not to delay in seeking help for urgent conditions [14].
In conclusion, despite the exceptional stress imposed on our institution by COVID-19, the neurosurgical service managed to maintain activity levels to within 10% of baseline pre-pandemic levels in 2019. Although significant differences were observed on the monthly timeframe, 2020 saw a modest overall impact with results showing a 4.3% reduction in activity when compared to 2019. However, the 2021 activity levels were more significantly impacted, with results demonstrating a 9.4% reduction in activity on 2019. The causes for this are multifactorial. However, the reductions observed closely mirrored the identifiable waves of COVID-19 infection, with the largest reduction correlating with peak demands on ICU beds, which occurred during first quarter of 2021. A robust emergency plan needs to be developed to prevent the impact of any subsequent pandemic on ordinary healthcare service delivery.
Availability of data and material
Data is available for review from the corresponding author on reasonable request.
References
Cantor J, Sood N, Bravata DM et al (2022) The impact of the COVID-19 pandemic and policy response on health care utilization: evidence from county-level medical claims and cellphone data. J Health Econ 102581. https://doi.org/10.1016/j.jhealeco.2022.102581
Perumal V, Curran T, Hunter M (2020) First case of COVID-19 in Ireland. Ulster Med J 89(2):128
Fahmi I (2019) World Health Organization coronavirus disease 2019 (Covid-19) situation report. DroneEmprit. https://apps.who.int/iris/handle/10665/331475. Accessed 10 Mar 2022
Cook T, El-Boghdadly K, McGuire B et al (2020) Consensus guidelines for managing the airway in patients with COVID-19: guidelines from the Difficult Airway Society, the Association of Anaesthetists the Intensive Care Society, the Faculty of Intensive Care Medicine and the Royal College of Anaesthetists. Anaesthesia 75(6):785–799. https://doi.org/10.1111/anae.15054
Workman AD, Jafari A, Welling DB et al (2020) Airborne aerosol generation during endonasal procedures in the era of COVID-19: risks and recommendations. Otolaryngol Head Neck Surg 163(3):465–470. https://doi.org/10.1177/0194599820931805
Remuzzi A, Remuzzi G (2020) COVID-19 and Italy: what next? Lancet 395(10231):1225–1228. https://doi.org/10.1016/S0140-6736(20)30627-9
Horan J, Duddy JC, Gilmartin B et al (2021) The impact of COVID-19 on trauma referrals to a National Neurosurgical Centre. Ir J Med Sci 190(4):1281–1293. https://doi.org/10.1007/s11845-021-02504-7
Ashkan K, Jung J, Velicu AM et al (2021) Neurosurgery and coronavirus: impact and challenges—lessons learnt from the first wave of a global pandemic. Acta Neurochir 163(2):317–329. https://doi.org/10.1007/s00701-020-04652-8
Raneri F, Rustemi O, Zambon G et al (2020) Neurosurgery in times of a pandemic: a survey of neurosurgical services during the COVID-19 outbreak in the Veneto region in Italy. Neurosurg Focus 49(6):E9. https://doi.org/10.3171/2020.9.FOCUS20691
Dobbs TD, Gibson JA, Fowler AJ et al (2021) Surgical activity in England and Wales during the COVID-19 pandemic: a nationwide observational cohort study. Br J Anaesth 127(2):196–204. https://doi.org/10.1016/j.bja.2021.05.001
Schirmer CM, Ringer AJ, Arthur AS et al (2020) Delayed presentation of acute ischemic strokes during the COVID-19 crisis. J Neurointerv Surg 12(7):639–642. https://doi.org/10.1136/neurintsurg-2020-016299
Moroni F, Gramegna M, Ajello S et al (2020) Collateral damage: medical care avoidance behavior among patients with myocardial infarction during the COVID-19 pandemic. JACC Case Rep 2(10):1620–1624. https://doi.org/10.1016/j.jaccas.2020.04.010
Hecht N, Wessels L, Werft F-O et al (2020) Need for ensuring care for neuro-emergencies—lessons learned from the COVID-19 pandemic. Acta Neurochir 162:1795–1801. https://doi.org/10.1007/s00701-020-04437-z
Irish Medical Organisation (2020) IMO warns that patients may be ignoring serious ailments as a result of #Covid19. Available at. https://www.imo.ie/news-media/news-press-releases/2020/imo-warns-that-patients-m/index.xml. Accessed 10 Mar 2022
Author information
Authors and Affiliations
Contributions
K Hussein: data collection and analysis, manuscript writing. A Geoghegan: data analysis, manuscript writing. M Hassan: data collection. M Moore: protocol development, data analysis and manuscript editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hussein, K., Geoghegan, A., Hassan, M. et al. The impact of COVID-19 on neurosurgical theatre activity in the National Neurosurgical Centre of Ireland. Ir J Med Sci 192, 823–827 (2023). https://doi.org/10.1007/s11845-022-03028-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-022-03028-4