Abstract
Background
Advanced clinical prioritisation (ACP) pathways could potentially improve the interface between primary and secondary care, instigating appropriate treatment pathways with improved efficiencies. Telemedicine is a key component of ACP pathways.
Aims
Telephone consultations for new referrals (as part of a pilot ACP pathway for chronic pain) were trialled to try (a) improve efficiency of outpatient clinics, (b) expedite assessment/treatment, and (c) reduce the number of face-to-face attendances. An audit of this activity was undertaken.
Methods
The 100 longest waiting new referrals were identified. Over a 9-month period patients were contacted via telephone, undergoing an initial assessment. Treatment plans were initiated and outcomes (≥ 1) were documented.
Results
Average length of time on waiting list was 35.37 months. 40% patients were discharged with advice back to referrer, 8% were referred for diagnostics/imaging, 32% were offered pharmacological management, 30% were scheduled for interventional management, 9% were referred for further MDT assessment/treatment, 4% were referred directly for a pain management programme (PMP), 6% were referred for assessment by other specialist services, 9% were brought in for face-to-face consultation in our pain management OPD, 2% were uncontactable, and 1% had died before assessment could be made.
Conclusions
Telemedicine as part of ACP represents an opportunity to improve speed of access to care, reducing the number of patients and time spent on waiting lists. Future studies should be directed at assessing efficacy of treatment plans initiated in telemedicine clinics whilst also looking at cost effectiveness and patient satisfaction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The full impact of COVID-19 on chronic disease in the context of altered elective/scheduled care delivery remains to be seen [1]. Hospital footfall is down with healthcare providers keen to avoid exposing patients unnecessarily to risks of hospital acquired COVID-19 infection. In Ireland, one study cited in person attendance to outpatient appointments at the height of lockdown restrictions as having fallen to 10% of pre-COVID-19 pandemic levels [2]. Additionally, patients themselves are reluctant to present to healthcare facilities for similar concerns; in the USA, the CDC has stated that up to 40% of Americans delayed presenting to hospital for emergency or elective care due to perceived risk of COVID-19 [1].
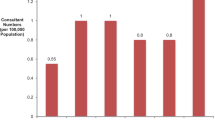
What is clear is that in Ireland, in a system with pre-existing prolonged waiting lists to access specialist care, cancellations have only meant longer wait times [2]. Evidently, solutions to this problem are needed. Manpower has always been an issue. At the time of writing, with 0.55 consultants per 100,000 population, Ireland has almost half the number of pain management consultants per 100,000 population compared to our neighbours in the UK [3]. Telemedicine may provide some part of the solution to this problem. Only with the advent of COVID-19-related attendance restrictions did telemedicine come to the forefront of Irish healthcare systems. One estimate cited a five-fold increase in the utilisation of telemedicine for elective healthcare in the period following the emergence of the COVID-19 pandemic in Ireland [4]. In pain medicine in Ireland, we have seen the vast majority of services increase their utilisation of this tool; prior to COVID-19, 13% of Irish pain management services were utilising telemedicine; this increased to 46% during the pandemic [2].
The return to normal delivery of elective, scheduled care and normal out-patient services forms part of the Health Service Executive’s (HSE) national service plan for 2021. In this, the development of advanced clinical prioritisation (ACP) processes as a “priority area for action” in 2021 are discussed [5]. Advanced clinical prioritisation (ACP) is defined as a process (or processes) for streamlining access to care, to ensure needs of patients are met as efficiently and effectively as possible. They are envisaged as being a key interface between primary and secondary care. While the concept of triage services is not a new one in Irish healthcare, it has been suggested that ACP should be built into the reform of scheduled care pathways generally. The aims of ACP is to improve efficacy of outpatient clinics, reduce the number of hospital attendances necessary (including for people who might have difficulty attending hospital locations), improve overall patient experience, reduce the number of patients attending clinics without necessary diagnostic examinations, and help clinic staff feel more productive within each patient interaction [6].
The aims of this study were to devise, implement/trial a clinical prioritisation pathway for new patient referrals to our chronic pain management clinic using telemedicine and to audit outcomes. The ultimate goal of the project was to develop a system for new referrals (as part of a pilot ACP pathway for chronic pain) to try (a) improve efficiency of outpatient clinics, (b) expedite assessment/treatment, and (c) reduce the number of face-to-face attendances in the context of an ongoing global pandemic.
Methods
We identified 100 patients who as new referrals to our OPD service were waiting the longest for an initial assessment. On the basis of the information given in the initial referral letters, the patients were triaged to several categories (those for potential intervention, potential MDT rehabilitation patients, those over 70 years of age, and miscellaneous — i.e. not initially assignable into any of the other categories). Patient demographics and waiting time between initial referral and assessment were examined. Over a 9-month period (June 2020 to February 2021), patients were contacted via telephone by a member of our multidisciplinary pain management team and underwent an initial assessment. If relevant, treatment plans were put in place and outcomes were documented. Where it was not possible to direct treatment via telephone, consultation patients were brought in for face-to-face consultation in our out-patient department. Documented outcomes included Discharged to Referrer (GP), Discharged to Referrer (Specialist), Referred for Diagnostics/Imaging, Pharmacological Management, Referred for Interventional Management, Referred for Further MDT Assessment/Treatment (Physiotherapy/Psychology), Referred for inclusion in Pain Management Programme (PMP), Referred for Further Specialist Assessment, Pain OPD (in-person) Follow up (Psychology/Physiotherapy/Medical/Nursing), Uncontactable (DNA), and Deceased by time of assessment (RIP). Patients could have more than one documented outcome. This was performed without any additional funding, using pre-existing departmental resources.
Statistical analysis
Standard, descriptive statistics including frequencies, means (averages), medians, and ranges were calculated using Microsoft® Excel® for Mac (Version 14.7.7).
Results
Of the 100 patients included in our patient cohort for this project, 68% (n = 68) were female with 32% (n = 32) male. The average age of patient was 58.9 years (SD = 17.02 years; mean = 58.96 years; median = 59.5 years; range 17–88 years). The average length of time for a patient to have been waiting on our out-patient waiting list for initial assessment/consultation was 35.37 months (SD = 11.57 months; median = 35 months; range = 14–46 months). With respect to outcomes, following initial telephone consultation, 34% (n = 34) of patients were discharged with advice back to the referrer (general practitioner), 6% (n = 6) were discharged with advice back to the referrer (other specialist), 8% (n = 8) were referred for further diagnostics/imaging, 32% (n = 32) were offered pharmacological management, 30% (n = 30) were scheduled for interventional management, 7% (n = 7) were referred for further chronic pain MDT assessment/treatment (physiotherapy), 2% (n = 2) were referred for further chronic pain MDT assessment/treatment (clinical psychology), 4% (n = 4) were referred directly for a multi-disciplinary pain management programme (PMP), 6% (n = 6) were referred for assessment by other specialist services (e.g. spinal orthopaedics), 9% (n = 9) were brought in for face to face consultation in our multidisciplinary pain management OPD, 2% (n = 2) were uncontactable and categorised as “Did Not Attend” (DNA), while unfortunately 1% (n = 1) had died in the intervening time from initial referral. These results are represented graphically in chart format in Fig. 1. Patients could have more than one documented outcome; in fact, 44% of patients (n = 44) had more than one, with 29% (n = 29) having two, 13% (n = 13) having three, and 2% (n = 2) having four different outcomes as a result of their consultation. This is represented graphically in Fig. 2.
Percentage of patients with given outcomes. It should be noted that patients could have more than one possible outcome as detailed in Fig. 2
Discussion
While telemedicine use is not a new development in chronic pain management in Ireland, this project has shown that it is possible to utilise an advanced clinical prioritisation (ACP) model to implement care plans for new referrals to a chronic pain management outpatient clinic. By removing the barrier of in person attendance, we increased our access (as evidenced by a low “Did Not Attend” (DNA) rate by national standards), maintained clinical activity and expedited treatment plans while reducing outpatient-related hospital footfall during a global pandemic. In the context of the widely reported waiting list crisis faced by Irish patients in need of specialist services, this represents a positive step forward.
The wait for chronic pain management in Ireland
In December 2020, there were over 600,000 people waiting for referral to secondary care, with over half of this number waiting over 9 months [6]. As of January 2020, based on data available publicly available from the national treatment purchase fund (NTPF) (https://www.ntpf.ie), there were almost 12,000 patients on a waiting list for a chronic pain management outpatient clinic appointment. Of these, almost 2000 had been waiting between 12 and 18 months with over 3000 waiting greater than 18 months for an appointment [3]. The length of time that patients have been waiting has only been exacerbated by COVID-19-related postponement of elective/scheduled care.
Telemedicine for chronic pain management
The ability to roll out telemedicine services in the delivery of scheduled, outpatient health care services has been improved significantly by dramatic technical innovations in recent years. Telemedicine can improve quality of care when access to pain medicine specialists is limited or indeed in situations where in person attendances should/can be avoided [7]. On an international level, telemedicine in pain management services has been previously reviewed [8] and shown to have the capacity to improve access to care [9], improve opioid discontinuation rates [10], provide improved management in chronic cancer pain [11], improve psychosocial outcomes in patients with chronic primary pain (e.g. fibromyalgia) [12], improve patient satisfaction, and decrease overall health care costs [13].
In Dec 2020, the Irish Medical Council published a guide about telemedicine for patients in Irish healthcare settings [14]. At the time of writing, there was currently no legislation specifically regulating telemedicine in Ireland. The current Irish Medical Council Professional Conduct and Ethics for Registered Medical Practitioners document states that telemedicine can pre provided in Irish health care settings subject to the presence of strong security measures, services being safe and suitable for patients, patients being informed that aspects of telemedicine consultations are different to traditional in-person consultations (e.g. lack of physical examination) and any additional risks that this can convey and providing consent to proceed. information policies being clear to users, patients’ primary care providers being informed of consultations, and compliance with data protections principles [15].
Advanced clinical prioritisation schemes
While formal plans to introduce ACP schemes were not published until July 2021 [6], we devised and piloted what would transpire to be a prototype version of an ACP triage scheme, albeit deploying it without the additional funding. The key components of this ACP triage scheme included clinically assessing the patient through a telemedicine consultation and identifying/implementing the most appropriate step(s) in the pathway to care for each patient. Taking 100 new patient referrals off our outpatient waiting list was ultimately achieved, with treatment pathways initiated for 57% (n = 57) patients directly from this telemedicine assessment.
Demographics
Chronic pain affects women more than men. One European wide study showed that in those with chronic pain, 56% were female with 44% being male [16]. From an Irish perspective, the PRIME study from 2011 corroborated this, finding that 57% chronic pain sufferers in Ireland were female, with 43% being male [17]. While the gender distribution of our sample of 100 patients did not reflect this (62% female, 48% male), it was consistent with the theme of chronic pain affecting women more than men. The average age (standard deviation) of our 100 patients was 58.96 (17.02) years. We know from Breivik et al. that in 2006, the European wide average age (standard deviation) of a chronic pain patient was 49.9 (17.4) years [16]. When their data was examined on an individual country basis, the average age of a chronic pain patient in Ireland in 2006 was cited as 60 years, a figure that is largely consistent with our own patient group.
Outcome implications
We saw a 40% (n = 36 back to primary care/GP, n = 4 back to other specialist referrers) discharge rate from our patient cohort. Reasons for discharge included patients having received treatment from another speciality (neurosurgery, interventional radiology, orthopaedics, rheumatology), symptoms had resolved or symptoms had improved with initiating treatment from primary care. A number of patients had sought care from the private healthcare sector in the time since initial referral and as such no longer required our services. In other instances, patients were discharged with advice (e.g. pharmacological, physiotherapy) to both themselves and the referrer. The multi-modal, multidisciplinary nature of chronic pain management bears out in the fact that 44% (n = 44) had more than one treatment outcome. Whilst the majority had some medical management of their pain in their treatment plan (32% (n = 32) pharmacological; 30% (n = 30) interventional), this included 7% (n = 7) of patients who were referred for specialist physiotherapy assessment/treatment, 2% (n = 2) being referred for specialist clinical psychology assessment/treatment, and 4% (n = 4) who were referred directly to inclusion in a pain management programme (PMP). The fact that 30% (n = 30) of patients could be referred directly for diagnostic or therapeutic intervention was important as it meant that further waiting times between traditional face-to-face OPD review and intervention would be shortened via removing the former from the equation. Similarly time was saved for the 8% (n = 8) of patients who required further diagnostics/imaging and 6% (n = 6) who needed further specialist assessment (neurosurgery, orthopaedics, rheumatology, neurology) as part of the workup for their painful symptoms. Only 9% (n = 9) of patients were identified as needing face-to-face assessment. Reasons that warranted such assessments included patients with hearing impairments, cognitive dysfunction, language barrier necessitating translator services, and ambiguous history necessitating a formal clinical examination that could not be undertaken with a telemedicine consultation. In 2016, the reported DNA rate overall within the HSE was 13%; the HSE has cited a target DNA rate of 5–8% in line with international best practice [18]. The observed DNA rate of 2% (n = 2) with the telemedicine pathway was much improved on our face-to-face OPD clinic DNA rate (12%). This is potentially explained by the fact that it is easier for patients with mobility, transport, or indeed carer issues to engage with a telemedicine clinic rather than the logistics of a face-to-face clinic. There is a cost incurred by DNAs in outpatient clinics and a rate reduction, while improving waiting list efficiency has positive financial implications for departments.
Limitations
While our study has demonstrated that ACP-type telemedicine assessment in multi-disciplinary pain management can be successfully undertaken in Irish hospitals. The limitations of this project include the fact that the results represent an audit of clinical activity, not a trial comparing telemedicine assessment to face-to-face clinic assessment. Our data consists only of baseline demographic data and clinic outcomes. We did not examine treatment outcomes nor were we able to compare the results to those of patients who attended face-to-face OPD appointments. Cost of implementation was not assessed. Any future study should seek to establish equivalence of treatment outcomes from telemedicine consultations compared to those from face-to-face assessments while also examining patient satisfaction with telemedicine services in chronic pain management.
Conclusions
With over 12,000 patients waiting for chronic pain management services in Ireland, new approaches are needed to improve access to specialist care. The use of telemedicine in Irish healthcare since the onset of the COVID-19 global pandemic has increased dramatically; it would appear to be here to stay. The use of telemedicine as part of ACP represents an opportunity to deploy telemedicine as a means to improving speed of access to tertiary care, reducing the number of patients on waiting lists and the time spent on them. Future studies should be directed at assessing efficacy of treatment plans initiated in telemedicine clinics whilst also looking at cost effectiveness and patient satisfaction.
Availability of data and material
All data and material collected are presented in the manuscript. Clarification on any matter can be made through the corresponding author.
Code availability
N/A.
References
Hacker KA, Briss PA, Richardson L et al (2021) COVID-19 and chronic disease: the impact now and in the future. Prev Chronic Dis 18:210086. https://doi.org/10.5888/pcd18.210086
Mullins CF, Harmon D, O’Connor T (2021) Quantifying the impact of COVID-19 on chronic pain services in the Republic of Ireland. Ir J Med Sci. https://doi.org/10.1007/s11845-021-02509-2
Purcell A, Channappa K, Moore D, Harmon D (2021) A national survey of publicly funded chronic pain management services in Ireland. Ir J Med Sci 10:1–9. https://doi.org/10.1007/s11845-021-02673-5
B&A (2020) Medical Council Press Release: five-fold increase in use of Telemedicine in Ireland since start of Pandemic. https://banda.ie/press-release-medical-council/. Accessed 1 Sept 2021
HSE (2021) National Service Plan 2021. https://www.hse.ie/eng/services/publications/serviceplans/national-service-plan-2021.pdf. Accessed 1 Sept 2021
HSE (2021) Advanced Clinical Prioritisation. In:Advanced Clinical Prioritisation (ACP) Handbook version 1. Department of Health (In press)
Kevin E, Vorenkamp MD (2016) Improving pain care through telemedicine: future or folly? Pain Med 17(6):997–998. https://doi.org/10.1093/pm/pnw035
McGeary DD, McGeary CA, Gatchel RJ (2013) A comprehensive review of telehealth for pain management: where we are and the way ahead. Pain Pract 12(7):570–577
Liddy C, Smyth C, Poulin PA et al (2016) Improving access to chronic pain services through econsultation: a cross-sectional study of the Champlain BASE eConsult Service. Pain Med. https://doi.org/10.1093/pm/pnw038
Naylor MR, Naud S, Keefe FJ, Helzer JE (2010) Therapeutic interactive voice response (TIVR) to reduce analgesic medication use for chronic pain management. J Pain 11:1410–1419
Kroenke K, Theobald E, Wu J et al (2010) Effect of telecare management on pain and depression in patients with cancer: a randomized trial. JAMA 304:163–171
Williams DA, Kuper D, Segar M et al (2010) Internet-enhanced management of fibromyalgia: a randomized controlled trial. Pain 151:694–702
Pronovost A, Peng P, Kern R (2009) Telemedicine in the management of chronic pain: a cost analysis study. Can J Anesth 56:590–596
Irish Medical Council (2020) Telemedicine phone and video consultations a guide for patients. https://www.medicalcouncil.ie/public-information/telemedicine-phone-and-video-consultations-guide-for-patients/. Accessed 9 Sept 2021
Irish Medical Council (2019) Guide to professional conduct and ethics for registered medical practitioners (Amended) 8th Edition. https://www.medicalcouncil.ie/news-and-publications/reports/guide-to-professional-conduct-and-ethics-for-registered-medical-practitioners-amended-.pdf. Accessed 9 Sept 2021
Breivik H, Collett B, Ventafridda V et al (2006) Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain 10(4):287–333. https://doi.org/10.1016/j.ejpain.2005.06.009. Epub 2005 Aug 10. PMID: 16095934
Raftery MN, Sarma K, Murphy AW et al (2011) Chronic pain in the Republic of Ireland—community prevalence, psychosocial profile and predictors of pain-related disability: results from the Prevalence, Impact and Cost of Chronic Pain (PRIME) study, part 1. Pain 152(5):1096–1103. https://doi.org/10.1016/j.pain.2011.01.019. Epub 2011 Mar 29. PMID: 21450402
HSE (2021) Outpatient Services. https://www.hse.ie/eng/about/who/acute-hospitals-division/patient-care/outpatient-services/. Accessed 18 Sept 2021
Author information
Authors and Affiliations
Contributions
This is an original article submission. All authors contributed to the study conception and design. Material preparation and data collection were performed by Andrew Purcell, Deirdre O’Shea, and Camillus Power. Data and analysis were performed by Andrew Purcell and Deirdre O’Shea. The first draft of the manuscript was written by Andrew Purcell, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
Ethical approval was not required for this project as it represents an audit of data regarding clinical activity that was already being carried out by the department.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Purcell, A., O’Shea, D. & Power, C. Advanced clinical prioritisation in an Irish, tertiary, chronic pain management service: an audit of outcomes. Ir J Med Sci 192, 817–821 (2023). https://doi.org/10.1007/s11845-022-03022-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-022-03022-w