Abstract
Background
The aim of this study was to evaluate hematological parameters in children with COVID-19 and determine the effects of inflammatory biomarkers on the assessment of hospitalization.
Methods
This retrospective single-center study was performed on 633 children with COVID-19 between March 2020 and January 2021. The study population was separated into two groups: inpatients (n = 83) and outpatients (n = 550). Univariate and multivariate logistic regression was applied to identify risk factors for hospitalization.
Results
Lymphopenia (n = 228, 36%) was found mainly to be a hematological abnormality in all cases. Compared with outpatients, inpatients had significantly higher white blood cell (WBC) (p = 0.005), lymphocyte (p < 0.001), and platelet counts (p = 0.036), and significantly higher red cell distribution width (p = 0.001), C-reactive protein (CRP) (p = 0.003), procalcitonin (p = 0.001), d-dimer (p < 0.001), and lymphocyte to monocyte ratio values (p = 0.004). On the other hand, they had significantly lower values of hemoglobin (p < 0.001), neutrophil to lymphocyte ratio (p = 0.024), platelet lymphocyte ratio (p = 0.001), derivated neutrophil to lymphocyte ratio (p = 0.037), and mean platelet volume to lymphocyte ratio (p < 0.001). ROC analysis showed that WBC, CRP, and procalcitonin cutoff values were the best discriminated between inpatients and outpatients. The results for the areas under the curve of WBC, CRP, and procalcitonin used to assess patients’ hospitalization were 0.595 (95% CI 0.519–0.670, p = 0.005), 0.599 (95% CI 0.527–0.672, p = 0.003), and 0.599 (95% CI 0.525–0.673, p = 0.004), respectively.
Conclusion
We suggest that high WBC and procalcitonin levels can be used as independent predictors of hospitalization in children with COVID-19.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
An outbreak of coronavirus disease 2019 (COVID-19) is spreading rapidly around the world and affects all age groups. Epidemiological studies have confirmed a lower prevalence of COVID-19 in children. Furthermore, it has been observed that children tend to have a milder clinical course or asymptomatic carriers and rarely develop critical illness compared with adults [1].
Children with COVID-19 can be asymptomatic (up to 45%) or present with fever, dry cough, shortness of breath, fatigue, and gastrointestinal symptoms, such as diarrhea, nausea, vomiting, and abdominal pain. The majority of children with mild or moderate COVID-19 will not progress to severe illness, and treatment remains largely supportive, including prevention and management of complications. Infants with underlying medical conditions (neurometabolic conditions, obesity, asthma, immunosuppression, congenital heart disease, etc.) might be at increased risk for severe disease [2]. Except for severe pediatric cases, children with non-severe COVID-19 disease, especially febrile infants, can require hospitalization for supportive treatment and close monitoring.
SARS-CoV-2 virus can affect several organ systems and exhibits clinical diversity with a wide range of manifestations, including in the hematological system. Lymphopenia and hypercoagulability have been frequently reported in adults with COVID-19 and seen to indicate poor outcomes [3].
Inflammatory parameters are expected to increase at different levels in the acute phase of COVID-19. Uncontrolled systemic inflammation can cause organ damage. C‐reactive protein (CRP), ferritin, d‐dimer, lower platelet count, and increased levels of several inflammatory cytokines have been associated with severity of COVID-19 disease [4, 5]. In a few studies, biomarkers of inflammation derived from the peripheral blood, such as neutrophil to lymphocyte ratio (NLR), neutrophil to monocyte ratio (NMR), lymphocyte to monocyte ratio (LMR), platelet to lymphocyte ratio (PLR), and lymphocyte to CRP ratio (L/CRP) were evaluated as prognostic factors of severity of COVID-19 disease in adults [6]. A limited number of pediatrics COVID-19 studies have rarely reported hematological involvement, possibly due to the immature immune systems of the patients or to lesser severity of the disease.
In this study, the primary outcomes were to assess the characteristics of hematological and inflammatory parameters in children with COVID-19. Secondary outcomes were to determine if these parameters may serve as a predictor of hospitalization.
Methods
This retrospective single-center study was conducted at the Department of Pediatric Infectious Disease in the Selcuk University Faculty of Medicine, Konya, Turkey, after approval by our hospital’s ethics committee (approval number 2021/83). During March 2020–January 2021, 633 children with SARS-CoV-2 infection, which was confirmed with real-time polymerase chain reaction (RT-PCR), were included in the study. The patients were separated into two groups on the basis of hospitalization. The outpatient group included 550 cases who were asymptomatic or had mild COVID clinical course. The inpatient group included 83 cases who presented with gastroenteritis, persistent fever, or inability to feed. We did not perform statistical analysis comparing the parameters between moderate, severe, or critically ill patients due to inadequate case numbers. Therefore, patients with lung involvement (bronchitis or pneumonia), bacterial coinfections, an underlying disease, or Down syndrome were excluded from the study.
The data on demographic characteristics and results of the laboratory tests were obtained from patient records. Hematological parameters and inflammatory biomarkers on admission were compared between the two groups. The complete blood count (CBC), including white blood cells (WBC), hemoglobin (Hb), platelets (PLT), lymphocytes (LYM), neutrophils (NEU), monocytes (MO), mean corpuscular volume (MCV), red cell distribution width (RDW), mean platelet volume (MPV), platelet distribution width (PDW), ferritin, and procalcitonin (PCT) were analyzed by a Beckman Coulter DXI 800 automated autoanalyzer (Beckman, CA, USA). d-dimers were determined using a Beckman Coulter 5800 automated autoanalyzer (Beckman, CA, USA). Hematological parameters were assessed according to age-specific intervals [7]. Thrombocytopenia was defined as platelet count < 150 K/µL. MPV, which is one of the platelet indices (MPV (fL) = plateletcrit/platelet count), was calculated obligatorily by Beckman Coulter automated autoanalyzer (reference range 6.5–11 fL).
Serological biomarkers were derived from a combination of two or more of the above indicators, including NLR, NMR, LMR, PLR, L/CRP, derivate neutrophil lymphocyte ratio (d-NLR), mean platelet volume to lymphocyte ratios (MPVLR), and systemic inflammatory index (SII) listed in Table 1. d-NLR was calculated by neutrophil count divided by the result of WBC count minus neutrophil count. The systemic inflammatory index (SII) was calculated as thrombocyte count × neutrophil count/lymphocyte count.
Statistical analysis
Categorical variables were presented as numbers and percentages. Shapiro–Wilk test and Kolmogorov–Smirnov test were applied to check the distribution of parameters. All parameters were presented as median with interquartile range (IQR) as they did not normally distribute. Continuous variables were analyzed by the Mann–Whitney U test. The chi-square test was used to compare categorical variables between groups. Associations between parameters were assessed using Spearman’s rank correlation test. Univariate and multivariate logistic regressions were applied to identify risk factors for hospitalization. All variables from the univariate analysis with p < 0.05 were subjected to forward stepwise multivariate logistic regression. The receiver-operating characteristic (ROC) curves were performed to estimate the predictive values of factors affecting the hospitalization of children with COVID-19. Statistical analysis was performed using a computer software package (SPSS for Windows, version 21.0).
Results
Demographic and laboratory characteristics of children with COVID-19
The 633 patients included in the study whose laboratory results were available comprised 310 (49%) males and 323 (51%) females, with a median age of 12.3 years. Of the 83 (13.1%) patients who were hospitalized, 550 (86.9%) patients were monitored with self-isolation in their home. The median ages of inpatients and outpatients were 8.1 years (IQR; 13.4) and 12.5 years (IQR; 9.5), respectively (p = 0.044). There was no significant difference in the gender ratio of the two groups.
When all the patients were taken into consideration, lymphopenia (36%), leukopenia (19.2%), thrombocytosis (8.8%), neutropenia (7.6%), neutrophilia (2.6%), thrombocytopenia (2.4%), leukocytosis (1.8%), and lymphocytosis (0.3%) were observed on admission. Lymphopenia was found mainly to be a hematological abnormality. When evaluated as subgroups, lymphopenia was the most common abnormal finding in both groups, while leukocytosis, neutrophilia, and thrombocytosis were found to be significantly higher in the inpatient group (Table 2).
Differential counts for WBC, lymphocyte, and platelets in subgroups suggested significant statistical differences with p < 0.05 for each test category. However, differential counts of neutrophil, eosinophil (EO), and monocyte between the two groups were not significant (p > 0.05). Inpatients had statistically significant lower median hemoglobin (p < 0.001) and higher RDW values (p = 0.001) when compared to outpatients (Table 1).
Comparison of hematological parameters and inflammatory markers in outpatients and inpatients
We determined the correlation between the hematological markers and hospitalization using Spearman’s rank correlation coefficient. The differences in the ratios of peripheral blood cell inflammatory markers, such as NLR, NMR, LMR, PLR, d-NLR, L/CRP, MPVLR, and SII, in the two groups were assessed. The comparison of the baseline laboratory characteristics between the two groups is shown in Table 1.
d-dimer was checked in 470 patients, and it was higher than > 500 ng/mL in 17.9% of them, and the median level of d-dimer was significantly higher in hospitalized patients (p < 0.001).
Higher than normal CRP (> 8 mg/L) and PCT (> 0.5 µg/L) were seen in 131 (20.7%) and 15 (2.4%) of the children on admission, respectively. The median levels of CRP and PCT were significantly higher in inpatients than in outpatients (p = 0.003, p = 0.001).
Inpatients had significantly lower NLR, PLR, d-NLR, and MPVL ratios than outpatients (p = 0.024, p = 0.001, p = 0.037, p < 0.001), respectively.
In all children with COVID-19, a significant positive correlation was detected between PCT level and WBC, NEU, MO, PLT, RDW, CRP, ferritin, d-dimer, NLR, d-NLR, and S-II, whereas a significant negative correlation was detected between PCT level and EO, MPV, PDW, hemoglobin, LMR, and L/CRP ratio. While PCT level was positively correlated with WBC, NEU, MO, PLT, RDW, CRP, ferritin, and d-dimer in hospitalized patients, it was negatively correlated with hemoglobin and L/CRP ratio. In outpatient patients, PCT level was positively correlated with WBC, NEU, MO, CRP, ferritin, d-dimer, d-NLR, and S-II, while negatively correlated with EO, MPV, PDW, hemoglobin, LMR, and L/CRP ratio (Table 3). The median count of WBC, LYM, PLT, RDW, d-dimer, and LMR was significantly higher in inpatients at the time of admission (p < 0.05).
Analysis of ROC curves by laboratory findings
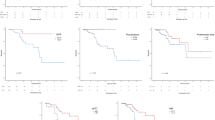
ROC analysis was performed on the laboratory findings of the blood samples collected at the first admission of the patients. All the results were used to evaluate the ability of various hematological and inflammatory parameters to assess hospitalization of children with COVID-19. As shown in Fig. 1, WBC, CRP, and PCT showed a reasonable ability to distinguish inpatients from outpatients. The areas under the curve (AUC) of WBC were 0.595 (95% CI 0.519–0.670, p = 0.005), and the associated criterion value in ROC was 5.250 K/µL with sensitivity and specificity of 71.1% and 31.4%, respectively. The AUC of CRP was 0.599 (95% CI 0.527–0.672, p = 0.003), with sensitivity and specificity of 73.5% and 40.3%, respectively. The AUC of PCT was 0.599 (95% CI 0.525–0.673, p = 0.004), with sensitivity and specificity of 50.0% and 62.2%, respectively.
Logistic regression of factors affecting hospitalization in children with COVID-19
First, univariate logistic regression analysis for the association of each variable with hospitalization was performed. Early age, leukocytosis, neutrophilia, NEU count, LYM count, MO count, platelet count, hemoglobin, RDW, CRP, ferritin, PLR, MPVLR, thrombocytosis, increased CRP, PCT, and d-dimer levels were statistically significant indicators for predicting hospitalization. Next, multivariate logistic regression analysis was used to determine which explanatory variables independently predict the outcome. All the variables in the univariate analysis were included in the model. The forward stepwise method was used for parameter selection. Leukocytosis (OR 6422; 95% CI 1.516–27.203; p = 0.012) and increased PCT (OR 21.221; 95% CI 6.095–73.889; p < 0.001) were the best independent predictors of hospitalization in children with COVID-19 on multivariate logistic regression analysis (Table 4).
Discussion
Karbuz et al. evaluated 1156 children with COVID-19 in Turkey; the median age of patients was 10.75 years. Of the total number of patients, 50.3% were male, and more than 80% of all patients had asymptomatic or mild disease. The most common symptoms include fever, cough, fatigue, dyspnea, diarrhea, and stomachache [8]. The demographic and clinical features of our COVID-19 cases were very similar to those previously reported. Although 13.1% of children were hospitalized in our study, none of them had a severe clinic.
COVID-19 is a systemic infection with a significant impact on the hematopoietic system and hemostasis. The most common hematological findings were reported as lymphopenia, leukocytosis, neutrophilia, and hypercoagulability related to the severity of COVID-19. Although peripheral blood alterations for assessing the severity of COVID-19 disease have been commonly documented in adults, in children, this was not so evident [9]. Recent systemic reviews indicated that the majority of children with COVID-19 had a normal WBC count, while the most common hematological abnormality was leukopenia. Lymphopenia was reported to be rarer in children than in adults. While lymphocytes play a major role in the inflammatory response, neutrophils are important in the innate immune response. Although most viruses cause lymphocytosis in infected persons, SARS-CoV-2 can directly infect lymphocytes via the ACE2 receptor and trigger lymphocytic apoptosis [3, 10, 11]. We observed lymphopenia in 228 (36%) children regardless of hospitalization. A less mature immune system, less expression of ACE2 receptors, and faster virus clearance may explain the infrequent occurrence of lymphopenia and the better COVID-19 prognosis in children [12, 13]. Also, age may have an impact on CBC in children with COVID-19. Lymphocytosis was more common in infants and neonates, similar to other viral infections [3]. In our study, we observed that inpatient age groups were younger than outpatients. The high frequency of hospitalization in the younger age group can be associated with nutritional intolerance and resistant fever, rather than clinical severity. The common COVID-19 abnormal hematological indexes on admission included lymphopenia, leukopenia, thrombocytosis, neutropenia, and neutrophilia, with indexes of 36%, 19.2%, 8.8%, 7.6%, and 2.6%, respectively. Unlike adult cases, neutropenia is observed in pediatric patients with SARS-CoV-2 infection. In the study of Yarali et al., lymphopenia, neutropenia, and neutrophilia were noted in 30%, 23.3%, and 13.3% of children, respectively [14]. Ozenen et al. reported that a total of 55 (21.9%) children with COVID-19 required hospitalization. The 14.3% of confirmed COVID‐19 children had neutropenia, 25.9% patient’s lymphopenia, and 4.4% thrombocytopenia [15].
Leukocytosis, neutrophilia, lymphopenia, and thrombocytopenia have been reported to be associated with a worse prognosis of COVID-19 in adults [16]. In our study, inpatients had higher WBC, lymphocyte, and platelet counts than outpatients.
There are a few studies in the literature about peripheral blood-related parameters such as NLR, NMR, LMR, PLR, d-NLR, MPVLR, L/CRP, and SII, which are inflammatory indices for predicting the severity of various infectious and inflammatory diseases in adults [17, 18]. NLR, PLR, and LMR are effective inflammatory mediators utilized in predicting mortality among adult patients [19, 20]. Many recent studies reported that NLR, NMR, LMR, PLR, and d-NLR of severe patients were significantly higher than non-severe patients [21,22,23]. MPV is a marker for the rate of platelet production and activation in the bone marrow. An adult study showed that MPV and MPVRL were more elevated in severe COVID-19 patients than in the mild group [24]. In our study, LMR was significantly elevated in hospitalized patients; however, the NLR, PLR, d-NLR, and MPVLR were significantly decreased. The difference in the results from those of the adults can be related to the higher values of lymphocyte counts in our hospitalized patients and to the patients having a better clinical course than the adults.
L/CRP is a newly developed inflammatory score that reflects systemic inflammation status. Recently, a meta-analysis by Rangel demonstrated that the L/CRP was significantly decreased in the severity of COVID-19 cases [25]. Adults’ studies indicated that low Hb concentration and platelet counts and increased levels of d-dimer were significantly correlated with mortality in patients with COVID-19 [26]. In our study, there was no statistically significant difference in the L/CRP level between inpatients and outpatients. Although Hb concentration was lower, platelet counts and levels of d-dimer were higher in inpatients than outpatients. Because COVID-19 infection causes an inflammatory response, cytokines suppress erythropoietin production during inflammation and cause anemia. While thrombocytopenia is frequently defined in severe clinics in adults, thrombocytosis may be explained by bone marrow stimulation without peripheral destruction in our hospitalized patients.
A recently proposed prognostic score is the SII, which relies on thrombocytes, neutrophils, and lymphocytes. This score is an index defining the instability in the inflammatory response. Fois et al. indicated that patients with higher SII values had a significantly worse outcome in COVID-19 adults [27]. There was no statistically significant difference in the SII ratio between our patient groups.
PDW reflects the variation in the size of platelets. Cytokine release and inflammation lead to higher platelet production and increased PDW. RDW conveys the degree of anisocytosis, which is a hugely inflammation-dependent process. Cytokine release and inflammation lead to higher platelet production, and increased PDW and RDW are associated with increased mortality in adults [28]. In our study, inpatients had statistically higher RDW while there was no significant difference of PDW levels between inpatients and outpatients. This condition may be associated with a milder inflammatory response of children to the SARS-CoV-2 virus than adults.
Cytokine response triggered by SARS-CoV-2 may result in rising acute phase reactants and a wide range of changes in hematological parameters. CRP is an acute-phase protein synthesized by hepatocytes that were observed to increase in COVID-19 patients in response to pro-inflammatory cytokines, especially interleukin (IL)-6 [27]. PCT is a precursor of the hormone calcitonin and is released into the blood circulation during bacterial infections or due to cytokine stimulation. Interleukin-1, tumor necrosis factor (TNF)-α, and IL-6 activate the concentrations of PCT [29]. In COVID-19 disease, an increase in CRP and PCT is expected to be related to the severity of the disease. In our study, higher than normal CRP (> 8 mg/L), PCT (> 0.5 µg/L) were seen in 20.7% and 2.4% of patients on admission, respectively. CRP and PCT levels were statistically higher in inpatients than outpatients. PCT level was positively correlated with WBC, NEU, MO, PLT, RDW, CRP, ferritin, and d-dimer in hospitalized patients.
In our study, the risk of hospitalization was determined to be 6.4-fold greater in children with higher WBC and 21-fold greater in children with higher PCT. We showed that the most powerful predictor of hospitalization due to COVID‐19 was the cutoff value of WBC (5.2 K/µL), CRP (2.29 mg/L), PCT (0.055 µg/L), respectively.
However, there seems to be a significant difference between inpatients and outpatients in terms of some tests; most of these tests seem to be within normal limits. In addition, with laboratory tests, the patient’s clinical condition should be also considered in the hospitalization decision of children with COVID-19.
Antibiotic treatment was started in patients with high CRP and PCT levels, but none of them had growth in their cultures. The results showed that, unlike other viral infections, the elevation of CRP and PCT may increase due to the activation of cytokines in COVID-19, apart from bacterial co-infection. The study has some limitations. First, it is a retrospective study and covers mild and asymptomatic cases. The laboratory values of the patients at the time of admission were retrospectively collected and not performed daily. These laboratory findings can change over the course of the disease, and patients were admitted at different times for their complaints. We also recognize that correlating severity of disease with hematological parameters is important, but this was not done in this study as the number of moderate or critical cases was small. Further studies are needed to evaluate laboratory analysis to predict hospitalization and correlate the clinical condition of COVID-19 in children.
In our study, the major hematological findings were lymphopenia, leukopenia, thrombocytosis, and neutropenia similar to other viral infections, which is possibly related to the milder clinical course of COVID-19 in children. We suggest that high WBC and PCT levels can be used as independent predictors of hospitalization in children with COVID-19. There is a need for further multicenter studies on inexpensive, easily accessible, and reliable diagnostic methods that can be used to determine the prognosis in children with COVID-19, regardless of their clinical status at the time of presentation.
Data availability
The authors confirm that the data supporting the findings of this study are available within the article [and/or] its supplementary materials.
Code availability
All source codes are available within the article [and/or] its supplementary materials.
References
Ladhani SN, Amin-Chowdhury Z, Davies HG et al (2020) COVID-19 in children: analysis of the first pandemic peak in England. Arch Dis Child. https://doi.org/10.1136/archdischild-2020-320042
Coronavirus Disease 2019 (COVID-19) Treatment Guidelines (2021). National Institutes of Health (US). https://www.covid19treatmentguidelines.nih.gov. Accessed 21 April 2021
Kosmeri C, Koumpis E, Tsabouri S et al (2020) Hematological manifestations of SARS-CoV-2 in children. Pediatr Blood Cancer 67(12):e28745
Kermali M, Khalsa RK, Pillai K et al (2020) The role of biomarkers in diagnosis of COVID-19—a systematic review. Life Sci. https://doi.org/10.1016/j.lfs.2020.117788
Pourbagheri-Sigaroodi A, Bashash D, Fateh F, Abolghasemi H (2020) Laboratory findings in COVID-19 diagnosis and prognosis. Clin Chim Acta 510:475–482
Xue G, Gan X, Wu Z et al (2020) Novel serological biomarkers for inflammation in predicting disease severity in patients with COVID-19. Int Immunopharmacol. https://doi.org/10.1016/j.intimp.2020.107065
Walkovich KL, Newburger PE (2016). Leukopenia In: Kliegman RM, Stanton BF, St Geme JW, III, Schor NF, Behrman RE, eds. Nelson Textbook of Pediatrics. 20th ed International Edition: Elsevier, pp 1047–1055
Karbuz A, Akkoc G, Bedir Demirdag T et al (2021) Epidemiological, clinical, and laboratory features of children with COVID-19 in Turkey. Front Pediatr. https://doi.org/10.3389/fped.2021.631547
Lippi G, Plebani M (2020) Laboratory abnormalities in patients with COVID-2019 infection. Clin Chem Lab Med 58:1131–1134
Zhu Y, Cao X, Tao G et al (2013) The lymph index: a potential hematological parameter for viral infection. Int J Infect Dis. https://doi.org/10.1016/j.ijid.2012.12.002
Terpos E, Ntanasis-Stathopoulos I, Elalamy I et al (2020) Hematological findings and complications of COVID-19. Am J Hematol 95:834–847
Castagnoli R, Votto M, Licari A et al (2020) Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in children and adolescents: a systematic review. JAMA Pediatr 174:882–889
Xu H, Liu E, Xie J et al (2020) A follow-up study of children infected with SARS-CoV-2 from western China. Ann Transl Med 8:623–623. https://doi.org/10.21037/atm-20-3192
Yarali N, Akcabelen YM, Unal Y, Parlakay AN (2021) Hematological parameters and peripheral blood morphologic abnormalities in children with COVID-19. Pediatr Blood Cancer 68:e28596
Guner Ozenen G, Sahbudak Bal Z, Umit Z et al (2021) Demographic, clinical, and laboratory features of COVID-19 in children: the role of mean platelet volume in predicting hospitalization and severity. J Med Virol 93:3227–3237. https://doi.org/10.1002/jmv.26902
Yan X, Li F, Wang X et al (2020) Neutrophil to lymphocyte ratio as prognostic and predictive factor in patients with coronavirus disease 2019: a retrospective cross-sectional study. J Med Virol 92:2573–2581. https://doi.org/10.1002/jmv.2606
Asghar MS, Khan NA, Haider Kazmi SJ et al (2020) Hematological parameters predicting severity and mortality in COVID-19 patients of Pakistan: a retrospective comparative analysis. J Community Hosp Intern Med Perspect 10:514–520. https://doi.org/10.1080/20009666.2020.1816276
Djordjevic D, Rondovic G, Surbatovic M et al (2018) Neutrophil-to-lymphocyte ratio, monocyte-to-lymphocyte ratio, platelet-to-lymphocyte ratio, and mean platelet volume-to-platelet count ratio as biomarkers in critically Ill and ınjured patients: which ratio to choose to predict outcome and nature of bacteremia? Mediat Inflamm. https://doi.org/10.1155/2018/3758068
Lee JS, Kim NY, Na SH et al (2018) Reference values of neutrophil-lymphocyte ratio, lymphocyte-monocyte ratio, platelet-lymphocyte ratio, and mean platelet volume in healthy adults in South Korea. Medicine (United States). https://doi.org/10.1097/MD.0000000000011138
Gong S, Gao X, Xu F et al (2018) Association of lymphocyte to monocyte ratio with severity of coronary artery disease. Medicine (United States). https://doi.org/10.1097/MD.0000000000012813
Yang AP, Liu JP, Tao WQ, Li HM (2020) The diagnostic and predictive role of NLR, d-NLR and PLR in COVID-19 patients. Int Immunopharmacol. https://doi.org/10.1016/j.intimp.2020.106504
Kalabin A, Mani VRK, Valdivieso SC, Donaldson B (2021) Role of neutrophil-to-lymphocyte, lymphocyte-to-monocyte and platelet-to-lymphocyte ratios as predictors of disease severity in COVID-19 patients. Infez Med 29:46–53
Rizo-Téllez SA, Méndez-García LA, Flores-Rebollo C et al (2020) The neutrophil-to-monocyte ratio and lymphocyte-to-neutrophil ratio at admission predict in-hospital mortality in mexican patients with severe SARS-CoV-2 infection (COVID-19). Microorganisms 8:1–17. https://doi.org/10.3390/microorganisms8101560
Wang H, Xing Y, Yao X et al (2020) Retrospective study of clinical features of COVID-19 in inpatients and their association with disease severity. Med Sci Monit. https://doi.org/10.12659/MSM.927674
Lagunas-Rangel FA (2020) Neutrophil-to-lymphocyte ratio and lymphocyte-to-C-reactive protein ratio in patients with severe coronavirus disease 2019 (COVID-19): a meta-analysis. J Med Virol 92:1733–1734
Mousavi SA, Rad S, Rostami T et al (2020) Hematologic predictors of mortality in hospitalized patients with COVID-19: a comparative study. Hematol (United Kingdom) 25:383–388. https://doi.org/10.1080/16078454.2020.1833435
Fois AG, Paliogiannis P, Scano V et al (2020) The systemic inflammation index on admission predicts in-hospital mortality in COVID-19 patients. Molecules. https://doi.org/10.3390/molecules25235725
Bommenahalli Gowda S, Gosavi S, Ananda Rao A et al (2021) Prognosis of COVID-19: red cell distribution width, platelet distribution width, and C-reactive protein. Cureus. https://doi.org/10.7759/cureus.13078
Lippi G, Plebani M (2020) Procalcitonin in patients with severe coronavirus disease 2019 (COVID-19): a meta-analysis. Clin Chim Acta 505:190–191
Author information
Authors and Affiliations
Contributions
GA: substantial contributions to conception and design, acquisition of data, analysis, and interpretation of data; and drafting the article and revising it critically for important intellectual content. AS: substantial contributions to conception and design, acquisition of data, analysis, and interpretation of data; and drafting the article. ME: substantial contributions to conception and design, acquisition of data, analysis, and interpretation of data; and revising it critically for important intellectual content. SKTO: substantial contributions to conception and design, acquisition of data, analysis, and interpretation of data; and revising it critically for important intellectual content. HV: substantial contributions to conception and design, acquisition of data, analysis, and interpretation of data; and revising it critically for important intellectual content. We further confirm that any aspect of the work covered in this manuscript that has involved either experimental animals or human patients has been conducted with the ethical approval of all relevant bodies and that such approvals are acknowledged within the manuscript.
Corresponding author
Ethics declarations
Ethical approval
The study protocols were approved by the Selcuk University Faculty of Medicine ethics committee (approval number 2021/83).
Consent to participate
We confirm that the manuscript has been read and approved by all named authors and that there are no other persons who satisfied the criteria for authorship but are not listed. We further confirm that the order of authors listed in the manuscript has been approved by all of us.
Consent for publication
All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work. The manuscript is not under publication or consideration for publication elsewhere.
Conflict of interest
Each author declared that there are no conflicts of interest in connection with this paper and no financial support, and the material described is not under publication or consideration for publication, elsewhere.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Alkan, G., Sert, A., Emiroglu, M. et al. Evaluation of hematological parameters and inflammatory markers in children with COVID-19. Ir J Med Sci 191, 1725–1733 (2022). https://doi.org/10.1007/s11845-021-02762-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-021-02762-5