Abstract
Background
There is a higher prevalence of lifestyle-related diseases among Irish farmers than the general adult population. Lifestyle interventions that increase physical activity and improve dietary patterns have been associated with reduced chronic disease risk and improved quality of life among high-risk populations. The impact of lifestyle interventions among Irish farmers is unknown.
Aim
To assess the effectiveness of a community-based intervention on farmer health, cardiovascular fitness, lower limb strength endurance, and dietary intake.
Methods
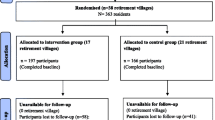
A 6-week physical activity and lifestyle education intervention involving two 60-min circuit-based exercise training sessions and one 60-min health education workshop per week was implemented. Pre- and post-measurements included total body weight, body fat percentage, lean muscle mass, resting blood pressure, fasting blood glucose, cholesterol, triglycerides, cardiovascular fitness, lower limb strength, perceived physical and mental health, and dietary intake.
Results
Thirty farmers completed the intervention giving an adherence rate of 75%. At baseline, mean BMI (32.7 ± 4.1 kg/m2), body fat percent (31.7 ± 6.7), waist circumference (110.2 ± 10.4 cm), systolic (128.7 ± 7.8 mmHg) and diastolic (86.2 ± 6.8 mmHg) blood pressure were higher than recommended levels. Significant improvements (p < 0.05) were found for total body weight, BMI, waist and hip circumferences, cardiovascular fitness, lower limb strength endurance, systolic blood pressure, total energy, total fat, total unsaturated fat, monounsaturated fat, saturated fat, trans fat, total carbohydrate, sodium, cholesterol and percentage energy intakes of total fat, saturated fat, protein, and physical and mental health scores.
Conclusions
Irish farmers remain at high risk of developing chronic diseases but respond positively to lifestyle intervention.

Similar content being viewed by others
References
World Health Organisation (2018). Noncommunicable diseases.
World Health Organisation (2018). Ireland. https://www.who.int/nmh/countries/irl_en.pdf
Smyth B, Evans DS, Kelly A et al (2012) The farming population in Ireland: mortality trends during the ‘Celtic Tiger’ years. Eur. J. Public Health 23(1):50–55. https://doi.org/10.1093/eurpub/cks017
van Doorn D, Richardson N, Osborne A (2017) Farmers have hearts: the prevalence of risk factors for cardiovascular disease among a subgroup of irish livestock farmers. J Agromedicine 22(3):264–274. https://doi.org/10.1080/1059924x.2017.1318728
Daghagh Yazd S, Wheeler SA, Zuo A (2019) Key risk factors affecting farmers’ mental health: a systematic review. Int J Environ Res. Public Health 16(23):4849. https://doi.org/10.3390/ijerph16234849
Furey EM, O’Hora D, McNamara J et al (2016) The roles of financial threat, social support, work stress, and mental distress in dairy farmers’ expectations of injury. Front. public health 4:126
Waggoner JK, Kullman GJ, Henneberger PK et al (2011) Mortality in the agricultural health study, 1993–2007. Am J Epidemiol 173(1):71–83. https://doi.org/10.1093/aje/kwq323
van Doorn D, Richardson N, Storey A et al (2018) Farming characteristics and self-reported health outcomes of Irish farmers. Occup Med 68(3):199–202. https://doi.org/10.1093/occmed/kqy020
Parks CG, Meyer A, Beane Freeman LE et al (2019) Farming tasks and the development of rheumatoid arthritis in the agricultural health study. Occup Environ Med 76(4):243–249. https://doi.org/10.1136/oemed-2018-105361
Walker-Bone K, Palmer KT (2002) Musculoskeletal disorders in farmers and farm workers. Occup Med 52(8):441–450. https://doi.org/10.1093/occmed/52.8.441
Torske MO, Hilt B, Glasscock D et al (2016) Anxiety and depression symptoms among farmers: the HUNT study. Norway. J Agromedicine 21(1):24–33. https://doi.org/10.1080/1059924X.2015.1106375
Fraser CE, Smith KB, Judd F et al (2005) Farming and mental health problems and mental illness. Int J Soc Psychiatry 51(4), 340-349. https://doi.org/10.1177/%2F0020764005060844
van Doorn D, Richardson N, Meredith D et al (2020) Farmers Have Hearts Cardiovascular Health Programme, Detailed Baseline Report. https://www.teagasc.ie/media/website/publications/2020/Farmers-Have-Hearts---Detailed-Baseline-Report.pdf
Central Statistics Office (2018) Statistical Yearbook of Ireland 2018, Farms and Farmers. https://www.cso.ie/en/releasesandpublications/ep/p-syi/psyi2018/agri/farmsandfarmers/
Central Statistics Office (2016) Farm Structure Survey 2016. https://www.cso.ie/en/releasesandpublications/ep/p-fss/farmstructuresurvey2016/da/foli/
Evans J, Frank B, Oliffe JL et al (2011) Health, Illness, Men and Masculinities (HIMM): a theoretical framework for understanding men and their health. J Mens Health 8(1):7–15. https://doi.org/10.1016/j.jomh.2010.09.227
Roy P, Tremblay G, Robertson S (2014) Help-seeking among male farmers: connecting masculinities and mental health. Sociol Rural 54(4):460–476. https://doi.org/10.1111/soru.12045
Eriksson MK, Hagberg L, Lindholm L et al (2010) Quality of life and cost-effectiveness of a 3-year trial of lifestyle intervention in primary health care. Arch Intern Med 170(16):1470–1479. https://doi.org/10.1001/archinternmed.2010.301
Fleming P, Godwin M (2008) Lifestyle interventions in primary care: systematic review of randomized controlled trials. Can Fam Physician 54(12):1706–1713
Saha S, Gerdtham UG, Johansson P (2010) Economic evaluation of lifestyle interventions for preventing diabetes and cardiovascular diseases. Int J Environ Res Public Health 7(8):3150–3195. https://doi.org/10.3390/ijerph7083150
McShane CJ, Quirk F, Swinbourne A (2016) Development and validation of a work stressor scale for Australian farming families. Aust J Rural Health 24(4):238–245. https://doi.org/10.1111/ajr.12261
Hagerty BM, Williams RA, Coyne JC et al (1996) Sense of belonging and indicators of social and psychological functioning. Arch of Psychiatr Nurs 10(4):235–244
Brumby S, Smith A (2009) Train the trainer’ model: implications for health professionals and farm family health in Australia. J Agromedicine 14(2):112–118. https://doi.org/10.1080/10599240902772563
Canadian Society for Exercise Physiology (2002). Physical Activity and Readiness Questionnaire - PAR-Q. http://www.westpointgrey.org/wp-content/uploads/2014/02/physical-activity-readiness-questionnaire.pdf
Kang JY, Cho SW, Lee JY et al (2010) The effects of a worksite on-line health education program on metabolic syndrome risk factors and nutrient intakes of male workers. J Nutr Health 43(1):57–68
Lua PL, Elena WPWD (2012) The impact of nutrition education interventions on the dietary habits of college students in developed nations: a brief review. Malays J Med Sci 19(1):4–14
Moore SG, Donnelly JK, Jones S et al (2018) Effect of educational interventions on understanding and use of nutrition labels: a systematic review. Nutrients 10(10):1432. https://doi.org/10.3390/nu10101432
Sahyoun NR, Pratt CA, Anderson A (2004) Evaluation of nutrition education interventions for older adults: a proposed framework. J Am Diet Assoc 104(1):58–69. https://doi.org/10.1016/j.jada.2003.10.013
Young DR, Haskell WL, Taylor CB et al (1996) Effect of community health education on physical activity knowledge, attitudes, and behavior: the Stanford Five-City Project. Am J Epidemiol 144(3):264–274. https://doi.org/10.1093/oxfordjournals.aje.a008921
Osborne A, Blake C, Fullen BM et al (2012) Prevalence of musculoskeletal disorders among farmers: a systematic review. Am J of Ind Med 55(2):143–158. https://doi.org/10.1002/ajim.21033
Osborne A, Finnegan G, Blake C et al (2013) An evaluation of low back pain among farmers in Ireland. Occup Med (Lond) 63(1):53–59. https://doi.org/10.1093/occmed/kqs173
Chodzko-Zajko WJ, Proctor DN, Fiatarone Singh MA et al (2009) American College of Sports Medicine position stand. Exercise and physical activity for older adults. Med Sci Sports Exerc 41(7), 1510–1530. https://doi.org/10.1249/MSS.0b013e3181a0c95c
Michie S, Abraham C, Whittington C et al (2009) Effective techniques in healthy eating and physical activity interventions: a meta-regression. Health Psychol 28:690–701. https://doi.org/10.1037/a0016136
Michie S, Ashford S, Sniehotta FF et al (2011) A refined taxonomy of behaviour change techniques to help people change their physical activity and healthy eating behaviours: the CALO-RE taxonomy. Psychol Health 26(11):1479–1498. https://doi.org/10.1080/08870446.2010.540664
Michie S, Richardson M, Johnston M et al (2013) The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med 46(1):81–95
Health Measures (2017) PROMIS Scoring Manual, PROMIS Global Health short form scoring information. https://www.healthmeasures.net/images/PROMIS/manuals/PROMIS_Global_Scoring_Manual.pdf
World Health Organisation (2011) Waist circumference and waist-hip ratio: report of a WHO expert consultation, Geneva, 8-11
World Health Organisation (no date) Body Mass Index – BMI. https://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi
Pickering D, Stevens S (2013) How to measure and record blood pressure. Community Eye Health 26(84):76–76
Ross R, Blair Steven N, Arena R et al (2016) Importance of assessing cardiorespiratory fitness in clinical practice: a case for fitness as a clinical vital sign: a scientific statement from the American Heart Association. Circulation 134(24):e653–e699. https://doi.org/10.1161/CIR.0000000000000461
Yamako G, Deng G, Totoribe K et al (2016) A novel protocol to test age-related decreases in sit-to-stand movement abilities in healthy subjects. J Orthop Sci 21(4):517–523. https://doi.org/10.1016/j.jos.2016.04.006
Mills A, Patel S (1994) Food Portion Sizes. Stationery Office
Goldberg GR, Black AE, Jebb SA et al (1991) Critical evaluation of energy intake data using fundamental principles of energy physiology: 1. Derivation of cut-off limits to identify under-recording. Eur J Clin Nutr 45(12), 569–581
Black AE (2000) Critical evaluation of energy intake using the Goldberg cut-off for energy intake:basal metabolic rate. A practical guide to its calculation, use and limitations. Int J Obes Relat Metab Disord 24(9),1119–1130. https://doi.org/10.1038/sj.ijo.0801376
Schofield WN (1985) Predicting basal metabolic rate, new standards and review of previous work. Hum Nutr Clin Nutr 39(Suppl 1):5–41
World Health Organisation (2003) Diet, Nutrition and the Prevention of Chronic Diseases. http://apps.who.int/iris/bitstream/10665/42665/1/WHO_TRS_916.pdf
Piepoli MF, Hoes AW, Agewall S et al (2016) 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts) Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Atherosclerosis 252:207–274. https://doi.org/10.1016/j.atherosclerosis.2016.05.037
Scientific Advisory Committee on Nutrition (2015) Carbohydrates and Health. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/445503/SACN_Carbohydrates_and_Health.pdf
World Research Cancer Fund (2018) Recommendations and public health and policy implications. https://www.wcrf.org/dietandcancer/cancer-prevention-recommendations
International Diabetes Federation (2006) The IDF consensus worldwide definition of the metabolic syndrome. https://www.idf.org/component/attachments/attachments.html?id=705&task=download
Pallant J (2013) SPSS survival manual: McGraw-Hill Education (UK)
Lohman TG (1982) Body composition methodology in sports medicine. Physician Sportsmed 10(12):46–58. https://doi.org/10.1080/00913847.1982.11947391
Department of Health (2019) Healthy Ireland Summary Report 2019 (ISBN 978-1-4468-8037-1). Dublin, Department of Health
Robertson S, Carroll P, Donohoe A et al (2018) “The environment was like they were in the pub but with no alcohol” – a process evaluation of engagement and sustainability in men on the move an Irish community based physical activity intervention. IJMSCH 1(1):e1–e14
Kelly L, Harrison M, Richardson N et al (2019) The impact of a gender-specific physical activity intervention on the fitness and fatness profile of men in Ireland. Eur J Public Health 29(6):1154–1160
Lin CH, Chiang SL, Tzeng WC et al (2014) Systematic review of impact of lifestyle-modification programs on metabolic risks and patient-reported outcomes in adults with metabolic syndrome. Worldviews Evid Based Nurs 11(6):361–368
Yamaoka K, Tango T (2012) Effects of lifestyle modification on metabolic syndrome: a systematic review and meta-analysis. BMC medicine 10(1):138
van Namen M, Prendergast L, Peiris C (2019) Supervised lifestyle intervention for people with metabolic syndrome improves outcomes and reduces individual risk factors of metabolic syndrome: a systematic review and meta-analysis. Metabolism 101:153988. https://doi.org/10.1016/j.metabol.2019.153988
Wei M, Kampert JB, Barlow CE et al (1999) Relationship between low cardiorespiratory fitness and mortality in normal-weight, overweight, and obese men. Jama 282(16):1547–1553. https://doi.org/10.1001/jama.282.16.1547
Enright PL (2003) The six-minute walk test. Respir Care 48(8):783–785
Chandler JM, Duncan PW, Kochersberger G et al (1998) Is lower extremity strength gain associated with improvement in physical performance and disability in frail, community-dwelling elders? Arch Phys Med Rehabil 79(1):24–30. https://doi.org/10.1016/s0003-9993(98)90202-7
Rosie J, Taylor D (2007) Sit-to-stand as home exercise for mobility-limited adults over 80 years of age—GrandStand System TM may keep you standing? Age and Ageing 36(5):555–562. https://doi.org/10.1093/ageing/afm093
Kutek SM, Turnbull D, Fairweather-Schmidt AK (2011) Rural men’s subjective well-being and the role of social support and sense of community: evidence for the potential benefit of enhancing informal networks. Aust J Rural Health 19(1):20–26
McLaren S, Challis C (2009) Resilience among men farmers: the protective roles of social support and sense of belonging in the depression-suicidal ideation relation. Death Studies 33(3):262–276
Alliance Irish Universities Nutrition (2011) National Adult Nutrition Survey Summary Report on Food and Nutrient intakes, Physical Measurements. Physical Activity Patterns and Food Choice Motives, Cork
Bannon S, Walton J, Flynn A (2011) The National Adult Nutrition Survey: dietary fibre intake of Irish adults. Proc Nutr Soc 70(OCE3):E113. https://doi.org/10.1017/S0029665111001534
Stephen AM, Champ MMJ, Cloran SJ et al (2017) Dietary fibre in Europe: current state of knowledge on definitions, sources, recommendations, intakes and relationships to health. Nutr Res Rev 30(2):149–190. https://doi.org/10.1017/S095442241700004X
Liu S, Willett WC, Manson JE et al (2003) Relation between changes in intakes of dietary fiber and grain products and changes in weight and development of obesity among middle-aged women. Am J Clin Nutr 78(5):920–927
Perry I, Browne G, Loughrey M et al (2010) Dietary salt intake and related risk factors in the Irish population. A report for Safefood Ireland (ISBN: 978-1-905767-14-4). Cork, Ireland
Coruzzi P, Parati G, Brambilla L et al (2005) Effects of salt sensitivity on neural cardiovascular regulation in essential hypertension. Hypertension 46(6):1321–1326. https://doi.org/10.1161/01.HYP.0000189183.50301.5c
van Doorn D, Richardson N, Osborne A et al (2019) The impact of a workplace cardiovascular health screening programme “Farmers Have Hearts” on health behaviour change among Irish farmers. Work 63(1):113–123. https://doi.org/10.3233/wor-192912
Margetts BM, Nelson M (1997) Design concepts in nutritional epidemiology. OUP Oxford
Macdiarmid J, Blundell J (1998) Assessing dietary intake: Who, what and why of under-reporting. Nutr Res Rev 11(2):231–53
Brumby S, Chandrasekara A, Kremer P et al (2013) The effect of physical activity on psychological distress, cortisol and obesity: results of the farming fit intervention program. BMC Public Health 13(1):1018. https://doi.org/10.1186/1471-2458-13-1018
Picorelli AMA, Pereira LSM, Pereira DS et al (2014) Adherence to exercise programs for older people is influenced by program characteristics and personal factors: a systematic review. J Physiother 60(3):151–156. https://doi.org/10.1016/j.jphys.2014.06.012
Cyril S, Smith BJ, Possamai-Inesedy A et al (2015) Exploring the role of community engagement in improving the health of disadvantaged populations: a systematic review. Glob Health Action 8:29842–29842. https://doi.org/10.3402/gha.v8.29842
Heyward VH, Wagner DR (2004) Applied body composition assessment: Human Kinetics
Ortega RM, Perez-Rodrigo C, Lopez-Sobaler AM (2015) Dietary assessment methods: dietary records. Nutr Hosp 31(3):38–45. https://doi.org/10.3305/nh.2015.31.sup3.8749
Wang L, Hui SSC (2015) Validity of four commercial bioelectrical impedance scales in measuring body fat among Chinese children and adolescents. BioMed Res Int 2015:614858–614858. https://doi.org/10.1155/2015/614858
Black AE (2000) The sensitivity and specificity of the Goldberg cut-off for EI:BMR for identifying diet reports of poor validity. Eur J Clin Nutr 54(5):395–404. https://doi.org/10.1038/sj.ejcn.1600971
Funding
Ruth Kavanagh received an employment-based postgraduate scholarship from the Irish Research Council in partnership with True Fitness and the Institute of Technology Sligo (Project ID: EBPPG/2019/118). Laura Keaver was the academic supervisor, Dr Diane Cooper was the employment-based mentor. True Fitness had no role in the analysis of results.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Ruth Kavanagh and Laura Keaver. The first draft of the manuscript was written by Ruth Kavanagh and Laura Keaver, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
Ethical approval was granted from the Research Ethics Committee at the Institute of Technology Sligo. Reference number 2020038.
Consent to participate
All participants provided informed written consent.
Consent for publication
All participants signed informed consent regarding publishing their data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kavanagh, R., Cooper, D., Bolton, J. et al. The impact of a 6-week community-based physical activity and health education intervention—a pilot study among Irish farmers. Ir J Med Sci 191, 433–445 (2022). https://doi.org/10.1007/s11845-021-02579-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-021-02579-2