Abstract
Introduction
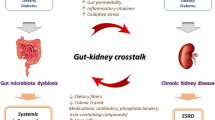
The colon has an important role in managing nitrogenous waste products, electrolytes, and mineral balance during kidney diseases. However, colonic microbiota produces uremic toxins, such as indoxyl sulfate and p-cresyl sulfate, in chronic kidney disease (CKD) patients, which due to their proinflammatory properties contribute to CKD progression. Conversely, in acute renal injury patients, intestinal microbiota could reduce inflammation by secreting short-chain fatty acids and inducing a renal protective immune response. However, since the intestines are the most frequently affected organ in advanced sepsis, colonic microbiota can also represent a negative factor for kidney health in this scenario.
Conclusion
In the present review, the main characteristics of kidney-gut crosstalk are described.




Similar content being viewed by others
References
Muso CG (2020) Biosemiotic medicine: from an effect-based medicine to a process-based medicine. Arch Argent Pediatr 118(5):e449–e453
Poesen R, Meijers B, Evenepoel P (2013) The colon: an overlooked site for therapeutics in dialysis patients. Semin Dial 26(3):323–332
Ranganathan N, Ranganathan P, Friedman EA et al (2010) Pilot study of probiotic dietary supplementation for promoting healthy kidney function in patients with chronic kidney disease. Adv Ther 27(9):634–647. https://doi.org/10.1007/s12325-010-0059-9
Musso CG (2004) Potassium metabolism in patients with chronic kidney disease. Part II: patients on dialysis (stage 5). Int Urol Nephrol 36(3):469–472
Vaziri ND (2016) Effect of synbiotic therapy on gut-derived uremic toxins and the intestinal microbiome in patients with CKD. Clin J Am Soc Nephrol 11(2):199–201
Mafra D, Lobo JC, Barros AF et al (2014) Role of altered intestinal microbiota in systemic inflammation and cardiovascular disease in chronic kidney disease. Future Microbiol 9(3):399–410
Gong J, Noel S, Pluznick J, Hamad A et al (2019) Gut microbiota-kidney cross-talk in acute kidney injury. Semin Nephrol 39(1):107–116
Evenepoel P, Meijers BKI, Bammens BRM, Verbeke K (2009) Uremic toxins originating from colonic microbial metabolism. Kidney Int Suppl 114:S12–S19
Crespo-Salgado J, Vehaskari VM, Stewart T et al (2016) Intestinal microbiota in pediatric patients with end stage renal disease: a Midwest Pediatric Nephrology Consortium study. Microbiome. 4(1):50
de Andrade L, Ishikawa-Ramos C, Cuppari L (2017) The cross-talk between the kidney and the gut: implications for chronic kidney disease. Nutrire 42(27):2–14. https://doi.org/10.1186/s41110-017-0054-x
Kanbay M, Onal E, Afsar B et al (2018) The crosstalk of gut microbiota and chronic kidney disease: role of inflammation, proteinuria, hypertension, and diabetes mellitus. Int Urol Nephrol 50:1453–1466. https://doi.org/10.1007/s11255-018-1873-2
Pahl MV, Vaziri ND (2015) The chronic kidney disease-colonic axis. Semin Dial 28:459–463
Ritz E (2011) Intestinal-renal syndrome: mirage or reality? Blood Purif 31:70–76
Sirich TL (2015) Dietary protein and fiber in end stage renal disease. Semin Dial 28(1):75–80. https://doi.org/10.1111/sdi.12315
Meyer TW, Hostetter TH (2012) Uremic solutes from colon microbes. Kidney Int 81(10):949–954
Soulage CO, Koppe L, Fouque D (2013) Protein-bound uremic toxins. New targets to prevent insulin resistance and dysmetabolism in patients with chronic kidney disease. J Ren Nutr 23:464–466
Neirynck N, Glorieux G, Schepers E et al (2013) Review of protein-bound toxins, possibility for blood purification therapy. Blood Purif 35:45–50
Niwa T (2011) Role of indoxyl sulfate in the progression of chronic kidney disease and cardiovascular disease: experimental and clinical effects of oral sorbent AST-120. Ther Apher Dial 15:120–124
Niwa T (2013) Targeting protein-bound uremic toxins in chronic kidney disease. Expert Opin Ther Targets 17(11):1287–1301
Aronov PA, Luo FJ, Plummer NS et al (2011) Colonic contribution to uremic solutes. J Am Soc Nephrol 22:1769–1776
Leong S, Sirich T (2016) Indoxyl sulfate-review of toxicity and therapeutic strategies. Toxins (Basel) 8(12):E35
Risso MA, Sallustio S, Sueiro V et al (2019) The Importance of tubular function in chronic kidney disease. Int J Nephrol Renov Dis 12:257–262. https://doi.org/10.2147/IJNRD.S216673
Enomoto A, Takeda M, Tojo A et al (2002) Role of organic anion transporters in the tubular transport of indoxyl sulfate and the induction of its nephrotoxicity. J Am Soc Nephrol 13(7):1711–1720
Zhang J, Ankawi G, Sun J et al (2018) Gut-kidney crosstalk in septic acute kidney injury. Crit Care 22(1):117. https://doi.org/10.1186/s13054-018-2040-y
Meyer TW, Hostetter TH (2007) Uremia. N Engl J Med 357(13):1316–1325
Patel K, Luo F, Plummer N et al (2012) The production of p-cresol sulfate and indoxyl sulfate in vegetarians versus omnivores. Clin J Am Soc Nephrol 7:982–988. https://doi.org/10.2215/CJN.12491211
Sirich TL, Plummer NS, Gardner CD et al (2014) Effect of increasing dietary fiber on plasma levels of colon-derived solutes in hemodialysis patients. Clin J Am Soc Nephrol 9(9):1603–1610
Vaziri ND, Liu SM, Lau WL et al (2014) High amylose resistant starch diet ameliorates oxidative stress, inflammation, and progression of chronic kidney disease. PLoS One 9(12):e114881
Marzocco S, Dal Piaz F, Di Micco L et al (2013) Very low protein diet reduces indoxyl sulfate levels in chronic kidney disease. Blood Purif 35:196–201
Rossi M, Johnson D, Morrison M et al (2016) Synbiotics easing renal failure by improving gut microbiology (SYNERGY): a randomized trial. Clin J Am Soc Nephrol 11:223–231. https://doi.org/10.2215/CJN.05240515
Meijers B, De Preter V, Verbeke K et al (2010) p-Cresyl sulfate serum concentrations in haemodialysis patients are reduced by the prebiotic oligofructose-enriched inulin. Nephrol Dial Transplant 25:219–224. https://doi.org/10.1093/ndt/gfp414
Shoji T, Wada A, Inoue K et al (2007) Prospective randomized study evaluating the efficacy of the spherical adsorptive carbon AST-120 in chronic kidney disease patients with moderate decrease in renal function. Nephron Clin Pract 105:c99–c107. https://doi.org/10.1159/000097985
Madero M, Cano KB, Campos I et al (2019) Removal of protein bound uremic toxins during hemodialysis using a binding competitor. Clin J Am Soc Nephrol 14(3):394–402. https://doi.org/10.2215/CJN.05240418
Cornelis T, Eloot S, Vanholder R et al (2015) Protein-bound uraemic toxins, dicarbonyl stress and advanced glycation end products in conventional and extended haemodialysis and haemodiafiltration. Nephrol Dial Transplant 30(8):1395–1402. https://doi.org/10.1093/ndt/gfv038
Camacho O, Rosales M, Shafi T et al (2016) Effect of a sustained difference in hemodialytic clearance on the plasma levels of p-cresol sulfate and indoxyl sulfate. Nephrol Dial Transplant 31:1335–1341. https://doi.org/10.1093/ndt/gfw100
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Human and animal rights and informed consent
This paper is a review article, so it was not a research involving human participants and/or animals nor had a need of an informed consent.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.