Abstract
Objective
In the management of bilateral fetal hydrothorax where the fetus is non-hydropic and apparently otherwise normal, we wished to determine if pleural-amniotic shunt insertion was better than conservative management in terms of mortality.
Methods
A systematic review was conducted between 1992 and 2017. Data extracted was inspected for heterogeneity. Where there was comparative data available, the odds ratio (OR) and confidence interval (CI) were calculated.
Results
Seven studies were included in this systematic review. There was a paucity of comparative data where only 2 studies (28 cases) allowed for direct comparison. Within the limitations of the study, there was no difference between shunt insertion vs. conservative management in terms of stillbirth or miscarriage (OR = 1.00, 95% CI 0.12–8.34, heterogeneity I2 = 0%, p = 1.00).
Conclusion
There is insufficient data available to determine whether the outcome is improved by pleural-amniotic shunt insertion compared with conservative management in cases of bilateral fetal hydrothorax where the fetus is non-hydropic and otherwise normal.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In a pregnancy complicated by a fetus with primary bilateral hydrothorax with no other identifiable anomaly, the decision for pleural-amniotic shunt insertion or conservative management can be a therapeutic dilemma. Most clinicians faced with this clinical situation would consider shunt insertion in the presence of hydrops on the grounds that conservative management would likely result in fetal demise. If, however, the fetus was not hydropic, many clinicians would adopt a conservative approach while others would offer shunt insertion.
Given that pleural-amniotic shunt insertion is not without risk, with a procedure-related loss rate of about 1%, this question merits investigation. In this paper, we propose to study pregnancy where the fetus has primary bilateral hydrothorax with no other anomaly and is not hydropic. We wished to perform a systematic review of shunt insertion vs. conservative management in these cases.
Materials and methods
This systematic review was based on a protocol developed using widely recommended methods for the systematic review of observational studies [10, 12, 21, 23; Henderson et al. 2009]. The study was registered with the PROSPERO database (registration number CRD42017060485; www.crd.york.ac.uk/PROSPERO).
Search strategy
The search strategy involved searching the bibliographic databases MEDLINE and EMBASE, the Cochrane library and Web of Science between March 1992 and March 2017 inclusive, and followed the PRISMA guidelines [14]. The search terms used were “fetus, fetal, foetus, and foetal in combination with hydrothorax, chylothorax, pleural effusion, thoracoamniotic shunt, and shunting. A combination of MeSH and text words was used. All relevant abstracts were reviewed and where the abstract met the pre-defined selection criteria, the full article was retrieved and reviewed. No language restriction was applied. Experts in the area were consulted to ensure the review encompassed all relevant papers.
Study selection
Selection criteria were the following:
Population—Pregnancies with non-hydropic fetuses with primary bilateral fetal hydrothorax managed with thoracoamniotic shunting or conservative management.
Outcome—intrauterine demise (stillbirth or miscarriage), neonatal death.
Study design—Prospective and retrospective studies including case series involving more than 5 cases.
Quality assessment and data extraction
One reviewer (EC) extracted the data from all the papers meeting the selection criteria. This was checked by another reviewer (SO). The studies were assessed for quality using the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement criteria [23] and the following criteria were derived from the checklist [18]:
Data collection—Prospective data was considered ideal; retrospective collection was considered second best.
Description of population—A well-defined sample at a uniform early stage with clear documentation of gestation at diagnosis, gestation at intervention, and delivery was considered ideal.
Prognostic factors considered: Clear documentation of other anomalies was considered ideal.
Objective outcome—Clear documentation of intrauterine demise or neonatal death was considered ideal.
Outcome ascertainment—Greater than 90% follow-up of the original study population was considered ideal, less than 90% was considered second best.
Data synthesis
The extracted data were tabulated to allow qualitative inspection for clinical and methodological heterogeneity. The data were not weighted according to the quality of the paper. For comparison of dichotomous outcomes between groups, the odds ratio (OR) and standard errors were calculated for the association in each study. The heterogeneity of estimates was explored graphically using forest plots and formally tested using χ2 tests. A combined proportion was calculated using the random effects models on the log odds scale. Data from individual studies were pooled [6]. The analysis of odds ratios was conducted using Review Manger 5 [1].
Results
Identification of the literature
The electronic search of bibliographical databases yielded 335 citations, of which 15 were considered potentially relevant [3,4,5, 7,8,9, 11, 13, 15,16,17, 19, 20, 22, 24]. Examination of the full manuscripts revealed that 8 did not meet the selection criteria. Thus, a total of 7 primary studies [4, 7, 9, 11, 16, 20, 22] were selected for review (Fig. 1; Table 1). All studies were retrospective observational studies.
Study characteristics and quality
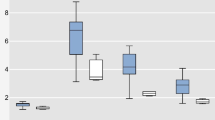
The quality assessment of included studies is demonstrated in Figs. 2 and 3. The gestational age at diagnosis was reported in 43% of studies. Gestation at shunt insertion was reported in 72% of studies.
Survival rates following shunt insertion vs. conservative management
Only 2 of the 7 selected studies had direct comparative data of conservative management vs. pleural-amniotic shunting (Fig. 4).
There was a paucity of comparative data where only 2 studies (28 cases) allowed for direct comparison. Within the limitations of the study, there was no difference between shunt insertion vs. conservative management in terms of stillbirth or miscarriage (OR = 1.00, 95% CI 0.12–8.34, heterogeneity I2 = 0%, p = 1.00).
Discussion
This systematic review did not provide sufficient evidence for or against pleural-amniotic shunting in cases of bilateral hydrothorax where the fetus is non-hydropic and apparently otherwise normal. The number of cases was too small to reach a meaningful conclusion.
The strength of this review is that it employed an exhaustive research strategy. This way, we were able to collate evidence for a condition that is imprecisely assessed in individual studies. In addition, the quality of these studies was assessed.
A major weakness of this systematic review is that all the papers evaluated were retrospective in nature and the overall number of cases was very small.
A further weakness of this review is that subtle reasons whereby decision-making may change are not accounted for. For example, a clinician may see a woman with a non-hydropic fetus with bilateral hydrothorax at 20 weeks. He may decide to adopt a conservative approach as the fetus is in a difficult position for shunt insertion. By 24 weeks, the clinical picture may be the same but the fetus could be in a better position for shunt insertion. The clinician may well decide to opt for shunt insertion. Our systematic review would have classified such a case as an intervention. In reality, a period of conservative management followed by shunt insertion took place.
In the original conception of this systematic review, we hoped to study outcome at different gestations, i.e., 20 to 24 weeks, 24 to 28 weeks, 28 to 32 weeks, and 32 to 34 weeks. We were particularly keen to study the outcome at the later gestations, where iatrogenic premature delivery (with its attendant risk of morbidity and mortality) is a possibility. Due to the paucity of our data, we were not able to provide useful information at different gestations.
Conclusion
In cases of bilateral fetal hydrothorax, where the fetus is non-hydropic and otherwise structurally normal, the correct management strategy in terms of pleural-amniotic shunting or conservative management remains unknown.
A multicenter randomized controlled trial is the best way to answer this question but may prove to be an impossible undertaking. Another solution would be for several large units to standardize reporting at the outset and pool their respective results in a large observational study.
Summary
In a pregnancy complicated by a fetus with primary hydrothorax and no other identifiable anomaly, we wished to determine whether pleural-amniotic shunt insertion was better than conservative management in terms of mortality. To do this, we conducted a systematic review between 1992 and 2017 and identified seven studies from which we could extract data. There was a paucity of comparative data with only two studies allowing for direct comparison. Within the limitations of the review, there was no difference between shunt insertion vs. conservative management.
References
(2008) Review Manager (RevMan) 5th edn. The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen
(2009) NHS Centre for Reviews and Dissemination CRD’s guidance for undertaking reviews in health care. In: York UO (ed). York
Bernaschek G, Deutinger J, Hansmann M, Bald R, Holzgreve W, Bollmann R (1994) Feto-amniotic shunting--report of the experience of four European centres. Prenat Diagn 14:821–833
Bianchi S, Lista G, Castoldi F, Rustico M (2010) Congenital primary hydrothorax: effect of thoracoamniotic shunting on neonatal clinical outcome. J Matern Fetal Neonatal Med 23:1225–1229
Blaicher W, Hausler M, Gembruch U, Bollmann R, Terinde R, Rempen A, Deutinger J, Bernaschek G (2005) Feto-amniotic shunting -- experience of six centres. Ultraschall Med 26:134–141
Deeks JJ, Altman DG, Bradburn MJ (2001) Statistical methods for examining heterogeneity and combining results from several studies in meta-analysis. BMJ Books, London
Derderian SC, Trivedi S, Farrell J, Keller RL, Rand L, Goldstein R, Feldstein VA, Hirose S, Mackenzie TC (2014) Outcomes of fetal intervention for primary hydrothorax. J Pediatr Surg 49:900–903 discussion 903-4
Deurloo KL, Devlieger R, Lopriore E, Klumper FJ, Oepkes D (2007) Isolated fetal hydrothorax with hydrops: a systematic review of prenatal treatment options. Prenat Diagn 27:893–899
Estoff JA, Parad RB, Frigoletto FD Jr, Benacerraf BR (1992) The natural history of isolated fetal hydrothorax. Ultrasound Obstet Gynecol 2:162–165
Henderson LK, Craig JC, Willis NS, Tovey D, Webster AC (2010) How to write a Cochrane systematic review. Nephrology (Carlton) 15:617–624
Jeong BD, Won HS, Lee MY, Shim JY, Lee PR, Kim A (2015) Perinatal outcomes of fetal pleural effusion following thoracoamniotic shunting. Prenat Diagn 35:1365–1370
Khan K, Riet GT, Glanville J, Sowden A, Kleijnen J (2000) Undertaking systematic reviews of research on effectiveness. CRD’s guidance for carrying out or commissioning reviews, 2nd edn. NHS Centre for Reviews and Dissemination, University of York, York
Mallmann MR, Geipel A, Bludau M, Matil K, Gottschalk I, Hoopmann M, Muller A, Bachour H, Heydweiller A, Gembruch U, Berg C (2014) Bronchopulmonary sequestration with massive pleural effusion: pleuroamniotic shunting vs intrafetal vascular laser ablation. Ultrasound Obstet Gynecol 44:441–446
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 62:1006–1012
O’brien B, Kesby G, Ogle R, Rieger I, Hyett JA (2015) Treatment of primary fetal hydrothorax with OK-432 (Picibanil): outcome in 14 fetuses and a review of the literature. Fetal Diagn Ther 37:259–266
Pellegrinelli JM, Kohler A, Kohler M, Weingertner AS, Favre R (2012) Prenatal management and thoracoamniotic shunting in primary fetal pleural effusions: a single centre experience. Prenat Diagn 32:467–471
Petersen S, Kaur R, Thomas JT, Cincotta R, Gardener G (2013) The outcome of isolated primary fetal hydrothorax: a 10-year review from a tertiary center. Fetal Diagn Ther 34:69–76
Rennie D (2003) Improving reports of studies of diagnostic tests: the STARD initiative. JAMA 289:89–90
Rustico MA, Lanna M, Coviello D, Smoleniec J, Nicolini U (2007) Fetal pleural effusion. Prenat Diagn 27:793–799
Smith RP, Illanes S, Denbow ML, Soothill PW (2005) Outcome of fetal pleural effusions treated by thoracoamniotic shunting. Ultrasound Obstet Gynecol 26:63–66
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 283:2008–2012
Takahashi Y, Kawabata I, Sumie M, Nakata M, Ishii K, Murakoshi T, Katsuragi S, Ikeda T, Saito M, Kawamoto H, Hayashi S, Sago H (2012) Thoracoamniotic shunting for fetal pleural effusions using a double-basket shunt. Prenat Diagn 32:1282–1287
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP (2007) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med 4:e296
Yinon Y, Kelly E, Ryan G (2008) Fetal pleural effusions. Best Pract Res Clin Obstet Gynaecol 22:77–96
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Summary
In a pregnancy complicated by a fetus with primary hydrothorax and no other identifiable anomaly, we wished to determine whether pleural-amniotic shunt insertion was better than conservative management in terms of mortality. To do this, we conducted a systematic review between 1992 and 2017 and identified seven studies from which we could extract data. There was a paucity of comparative data with only two studies allowing for direct comparison. Within the limitations of the review, there was no difference between shunt insertion and conservative management.
Impact statement
What is already known on this subject?
In a fetus with bilateral hydrothorax, which is hydropic, clinicians will often insert a thoracoamniotic shunt, as conservative management will often result in fetal demise. However, in the absence of hydrops, it is not clear whether shunt insertion or conservative management is preferable.
What do the results of this study add?
In fetuses with bilateral hydrothorax but no hydrops, our study indicates that there is insufficient evidence to determine if shunt insertion is better than conservative management.
What are the implications of these findings for clinical practice and/or further research?
The lack of evidence demonstrated by our systematic review highlights the need for fetal anomaly registries with standardized definitions, outcome measures, and follow-up.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Carson, E., Devaseelan, P. & Ong, S. Systematic review of pleural-amniotic shunt insertion vs. conservative management in isolated bilateral fetal hydrothorax without hydrops. Ir J Med Sci 189, 595–601 (2020). https://doi.org/10.1007/s11845-019-02094-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-019-02094-5