Abstract
Background
The rate of induction of labour varies across Health Service Executive hospital regions in Ireland averaging at 23.3 per 100 deliveries in 2005–2009. The increasing rate of elective induction of labour in Ireland calls for more studies looking into associated maternal and/or neonatal outcomes.
Study aim
The aim of this study is to show that an elective induction policy with management by a sole consultant obstetrician can decrease caesarean section rates as well as positively impact maternal and neonatal complications.
Methods
We conducted a retrospective review of women attending a named obstetrician over a 1-year period. In total, 22 variables were collected, including basic patient demographics, mode of onset of labour, method of induction, mode of delivery, length of labour and neonatal outcomes.
Results
In total, 583 patients were identified in the study period. One hundred twenty-six (21.6%) patients presented with a spontaneous onset of labour, and 405 (69.4%) of patients had an induction of labour. Relative risk of having an emergency caesarean section, if labour is induced, is 1.42 (95% CI 0.64 to 3.14), and no statistical significance was demonstrated (p = 0.38). There was a statistically significant difference in operative vaginal delivery versus standard vaginal delivery relative risk between women ≥ 35-year-old and < 35-year-old groups, 0.47 (95% CI 0.39–0.57), p < 0.0001.
Conclusion
Elective induction of labour is not associated with an increased risk of caesarean section or operative vaginal delivery in patients less than 35 years of age. This shows that elective induction is an appropriate intervention in selected scenarios without affecting mode of delivery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Induction of labour (IOL) is the initiation of labour by artificial means prior to its spontaneous onset at a viable gestational age, with the aim of achieving a vaginal delivery in a pregnant woman with intact membranes [1]. This can be achieved by membrane sweeping, administration of oral/vaginal prostaglandins, mechanical methods and infusion of intravenous oxytocin. In 2004 and 2005, one in five deliveries in the UK had undergone an IOL [2]. When labour was induced using pharmacological methods (whether surgical induction was also attempted), less than two thirds of women gave birth without further intervention, with 15% having instrumental births and 22% having an emergency caesarean section (CS) [2]. The most common indications for IOL are to prevent prolonged pregnancy (more than 42 weeks), preterm or term pre-labour rupture of membranes, foetal growth restriction, maternal medical disorders and maternal request [3]. The choice of method of IOL depends on the indication, maternal condition, gestation, parity and wishes, as well resources and facilities available [1,2,3]. Many studies have been conducted comparing delivery outcomes following IOL with each method of IOL; however, no one method was proven to be superior to the other [4,5,6,7,8,9]. IOL has a large impact on the health of women, on their babies and on the workload of maternity units; thus, the indications, method and timing of IOL need to be carefully considered in each case to minimise adverse patient and service focussed outcomes.
In the Republic of Ireland, rates of IOL vary across Health Service Executive regions, with Dublin Northeast being lowest and West region being the highest, at 23.3 and 31.3 per 100 deliveries in 2005–2009 respectively [10]. The incidence of prostaglandin use for IOL was highest in the Southern region at 8.9 per 100 deliveries, while the use of oxytocin as a method for IOL was highest in Dublin Mid Leinster region, 6.8 per 100 deliveries, and Artificial Rupture of Membranes (ARM) being highest in the Western region at 8.9 per 100 deliveries.
Our institution had 4690 total live births in 2015 and 4473 in 2016. The overall IOL rate increased by almost 2% from 2015 to 2016, 33.33% (n = 1563) and 35.03% (n = 1567) respectively. In 2015 and 2016 respectively, the rate of CS remained the same (34.75% (n = 1630) and 34.76% (n = 1555)), with the rate of spontaneous vaginal delivery (SVD) decreasing slightly, from 49.28% (n = 2311) to 47.06% (n = 2105). With regard to operative vaginal delivery (OVD) in 2015 and 2016, the rate of forceps delivery increased from 1.3% (n = 61) to 2.46% (n = 110) while the rate of vacuum delivery remained unchanged, 14.63% (n = 686) and 14.87% (n = 665) [11].
The outcomes of indicated IOL for maternal or foetal reasons and elective IOL vary from study to study. Guerra et al. demonstrated that mean CS rate in elective induction was lower, 11.7%, compared to CS rate of all inductions (29.5%). However, when compared to spontaneous onset of labour (SOL), CS rate was higher in the elective IOL group, 8.6% versus 11.6% respectively [12]. Bailit et al. showed that elective induction had a lower rate of CS compared to induction for maternal or foetal reasons, at 8 and 24% respectively. Moreover, it has been demonstrated that elective induction at 39 weeks is associated with lower CS rate compared to SOL [13]. Both studies report no significantly increased risk of neonatal complications, such as neonatal intensive care unit (NICU) admission and length of stay, sepsis and neonatal ventilator use. Similarly, maternal morbidity, such as risk of perineal laceration or postpartum haemorrhage, lengthened hospital stay, and greater needs for blood transfusion are increased following IOL [10,11,12,13]. Stock et al. demonstrated that elective induction before 40 weeks’ gestation compared with expectant management is not associated with increased rates of emergency CS or operative vaginal delivery (OVD) at 37–39 weeks and a reduction in both rates at 40–41 weeks. Moreover, the odds of maternal complications at 39 weeks gestation such as postpartum haemorrhage (95% CI, 0.90 0.83–0.98; p = 0.002) and anal sphincter injury (95% CI 0.43–0.89; p < 0.001) were lower in the elective IOL group at 38–40 weeks’ gestation compared to expectant management. However, the odds of neonatal admission to NICU were increased in the elective induction group at 39 weeks compared to those in the expectant management, 1.17 (95% confidence interval, 1.07–1.26; p value < 0.001) [14].
A Cochrane review concluded that there were significantly fewer CS compared with expectant management in 21 trials of 8749 women (RR 0.89, 95% CI 0.81 to 0.97) [15]. Furthermore, two systematic reviews reviewed 31 and 157 papers respectively found that an elective induction policy was associated with a reduction in the risk of CS compared with expectant management (OR 0.83, 95% CI 0.76–0.92 [16]) and that CS rate was 12% lower in IOL groups versus expectant management [17]. A further meta-analysis of five randomised controlled trials in 2015 showed no statistically significant difference in CS and OVD rates between IOL and expectant management groups [18].
The aim of this study is to show that an elective induction policy with management by a sole consultant obstetrician can decrease CS rates and maternal and neonatal complications.
Methods
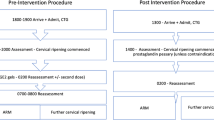
We conducted a retrospective observational study of all women attending a named consultant obstetrician for shared antenatal care with their general practitioner, who delivered over a 2.5-year period. All women had planned to deliver in a tertiary-level referral hospital, with more than 4000 deliveries per year.
Basic patient identifiers were retrieved from a database held by the named consultant obstetrician. Subsequently, authors interrogated an institutional audit tool utilised by the delivery suite to record deliveries and associated data in this institution. These paper forms were hand-searched and relevant variables extracted to a password-protected database, with sole access to the data collectors. All women delivered by the named consultant obstetrician following attendance at his clinic antenatally were included. Women excluded were those delivered by another obstetrician while the named obstetrician was unable to attend the delivery or those who did not have clearly documented onset of labour and mode of delivery. Initially, all women delivered were included for analysis. Following this, we interrogated women who had an IOL and compared outcomes to other patients who had a SOL. Those who had an elective CS were excluded from statistical analysis. In total, 22 variables were collected. After the initial data analysis, these were sub-classified into two groups: women ≥ 35-year-old and < 35-year-old groups. We then used various statistical analysis methods to compare the outcomes between the study groups. Moreover, we compared our results with background data retrieved from our institution.
The study was exempt from ethical approval, due to its’ observational nature, and no identifiable factors were recorded.
Results
In total, 583 women were identified to have delivered during the study period. There were 126 (21.6%) patients who had a SOL, 405 (69.4%) who had an IOL and 52 (8.9%) who had an elective CS. Patient demographics are demonstrated in Table 1.
One hundred twenty-six (23.7%) women presented with an SOL, of those 61.9% (n = 78) had spontaneous vaginal delivery (SVD) and 32.5% (n = 41) had operative vaginal delivery (OVD). The emergency CS rate in this group was 5.5% (n = 7). Four hundred five women (76.3%) had an IOL. 59.5% (n = 241) had SVD, and 32.5% (n = 132) had operative vaginal delivery. Relative risk of OVD in those being induced is 1.03 (95% CI 0.77 to 1.36); however, no statistical significance was demonstrated (p = 0.85). The overall CS rate in this group was 7.9% (n = 32). Relative risk of having an emergency CS, if labour is induced, is 1.42 (95% CI 0.64 to 3.14); no statistical significance was demonstrated (p = 0.38).
Following this, we further sub-categorised the groups by the maternal age where age was available. In total, 321 (55.9%) women were ≥ 35 years old, and 253 (44.1%) in the < 35-year-old group. The average maternal age was 37.5 years in ≥ 35-year-old group and 31.8 years in < 35-year-old group. Table 2 demonstrates the onset of labour and mode of delivery of these groups. 25.5% of the ≥ 35-year-old group (n = 82) and 16.6% (n = 42) of the < 35-year-old group had an SOL. 10.2% (n = 33) of those in the ≥ 35-year-old group having a CS, compared to 8.3% (n = 21) in the < 35-year-old group. Those of ≥ 35-year-old group were more likely to have a SOL versus an IOL (p = 0.01); however, the relative risk of VD versus CS in this group was not statistically significant, 0.75 (95% CI 0.45–1.25; p = 0.27). There was a statistically significant difference in OVD versus SVD relative risk between ≥ 35-year-old group and < 35-year-old group, 0.48 (95% CI 0.39–0.57), p < 0.01.
Furthermore, we compared our results with background hospital data. In 2015–2016, cumulative rate of spontaneous vaginal delivery was 48.19% (n = 4416); 1.87% (n = 171) for forceps delivery; 14.74% (n = 1351) for vacuum delivery; and 34.76% (n = 3185) for caesarean section. Absolute risk reduction of caesarean section after IOL compared to overall rate of caesarean sections in the unit is 26.86% (95% CI − 0.2983 to − 0.2389). Absolute risk reduction of vaginal delivery after IOL is 11.31% (95% CI 0.06 to 0.16). Absolute risk increase of operative vaginal delivery is 15.89% (95% CI 0.11 to 0.21) after induction of labour.
Discussion
Induction of labour is a common obstetric intervention in modern obstetric practice with rates varying between regions.
Our study shows that in the presence of sole and consistent management, IOL does not negatively impact on the mode of delivery or outcomes of women who have undergone an IOL. There was a similar rate of SVD, as well as CS, and no statistically significant difference between single instrument OVD. However, those who had a SOL were more likely to have a combined instrumental delivery. It is known that a combined operative vaginal delivery is associated with higher maternal and neonatal morbidity, and therefore, it can be extrapolated that patients who had an IOL had a lower risk of significant morbidity secondary to this, postulated perhaps to an increased use of oxytocin in the IOL group.
When we look at the higher risk sub-group—those of ≥ 35-year-old group—we demonstrated that there are no associated increased risk of CS if an IOL is carried out prior to term, in the absence of obstetric indications.
While our study adds some interesting literature to the topic of elective induction of labour, there are several limitations. This is mostly due to inadequate data collection at the time of delivery, limiting our analysis. Some delivery information was missing or illegible and thus was excluded from analysis. Secondly, as our study is retrospective, it is subjected to a selection bias; however, a prospective study could also be affected by the Hawthorne effect and has skewed results. Our study was underpowered to demonstrate some statistically significant results. This is due to the retrospective nature of our study, and the sample size was limited to the time frame of the study. We could have potentially lowered type 1 error or power of the study in order to obtain statistically significant results; however, authors decided on using commonly acceptable 5% type 1 error rate for our calculations. However, the clinical findings are still significant and applicable to clinical practice.
Conclusion
Our study corroborates previous findings that there is no significant difference in CS rates between inductions of labour at term compared with expectant management [7, 8]. Results presented in this study provide an effective starting point for a randomised trial into this topic and hopefully aim to dispel the myth that induction of labour is a negative predictive factor for caesarean section.
References
World Health Organization (2011) WHO recommendations for induction of labour 2011, Geneva
NICE Clinical Guideline 70, (2008). National Institute for Health and Clinical Excellence. Induction of Labour: http://wwwniceorguk/CG070fullguideline Accessed 2 February 2016
Mozurkewich E, Chilimigras J, Koepke E, Keeton K, King VJ (2009) Indications for induction of labour: a best evidence review. Br J Obstet Gynaecol 116(5):626–636
Alfirevic Z, Kelly AJ, Dowswell T. (2009) Intravenous oxytocin alone for cervical ripening and induction of labour. Cochrane Database of Systematic Reviews. Issue 4. Art. no.: cD003246; DOI: https://doi.org/10.1002/14651858.cD003246.pub2
Hofmeyr GJ, Gülmezoglu AM, Pileggi C. (2003). Vaginal misoprostol for cervical ripening and induction of labour. Cochrane Database of Systematic Reviews, Issue 1. Art. No.: cD000941; DOI: https://doi.org/10.1002/14651858.cD000941
Alfirevic Z, Weeks A. (2006). Oral misoprostol for induction of labour. Cochrane Database of Systematic Reviews. Issue 2. Art. no.: cD001338. DOI: https://doi.org/10.1002/14651858.cD001338.pub2
Kelly AJ et al. (2009). Vaginal prostaglandin (PGE2 and PGF2α) for induction of labour at term. Cochrane Database of Systematic Reviews. Issue 4. Art. no.: cD003101; DOI: https://doi.org/10.1002/14651858.cD003101.pub2
Boulvain M et al. (2001). Mechanical methods for induction of labour. Cochrane Database of Systematic Reviews. Issue 4. Art. no.: cD001233; DOI: https://doi.org/10.1002/14651858.cD001233
Boulvain M, Stan CM, Irion O. (2005). Membrane sweeping for induction of labour. Cochrane Database of Systematic Reviews. Issue 1. Art. no.: cD000451. DOI: https://doi.org/10.1002/14651858.cD000451.pub2
Lutomski JE, Morrison JJ, Lydon-Rochelle MT (2012) Regional variation in obstetrical intervention for hospital birth in the Republic of Ireland, 2005–2009. BMC Pregnancy and Childbirth 12:123. https://doi.org/10.1186/1471-2393-12-123
University Maternity Hospital Limerick, Clinical report 2015-2016
Guerra GV, Cecatti JG, Souza JP, Faúndes A, Morais SS, Gülmezoglu AM, Passini R Jr, Parpinellia MA, Carroll G (2011) Elective induction versus spontaneous labour in Latin America. Bull World Health Organ. 89:657–665. https://doi.org/10.2471/BLT.08.061226
Bailit JL, Gregory KD, Reddy UM, Gonzalez-Quintero VH, Hibbard JU, Ramirez MM, Ware Branch D, Burkman R, Haberman S, Hatjis CG, Hoffman MK, Kominiarek M, Landy HJ, Learman LA, Troendle J, Veldhuisen PV, Wilkins I, Sun L, Zhang J (2010) Maternal and neonatal outcomes by labour onset type and gestational age. Am J Obstet Gynecol 202(3):245.e1–245.e12. https://doi.org/10.1016/j.ajog.2010.01.051
Stock SJ, Ferguson E, Duffy A, Ford I, Chalmers E, Norman JE (2012) Outcomes of elective induction of labour compared with expectant management: population based study. BMJ 344:e2838. https://doi.org/10.1136/bmj.e2838
Gülmezoglu AM, Crowther CA, Middleton P, Heatley E (2012) Induction of labour for improving birth outcomes for women at or beyond term. Cochrane Database Syst Rev 6:CD004945. https://doi.org/10.1002/14651858.CD004945.pub3
Wood S, Cooper S, Ross S (2014) Does induction of labour increase the risk of caesarean section? A systematic review and meta-analysis of trials in women with intact membranes. BJOG 121(6):674–685; discussion 685. https://doi.org/10.1111/1471-0528.12328
Mishanina E, Rogozinska E, Thatthi T, Uddin-Khan R, Khan KS, Meads C (2014 Jun 10) Use of labour induction and risk of cesarean delivery: a systematic review and meta-analysis. CMAJ 186(9):665–673. https://doi.org/10.1503/cmaj.130925
Saccone G, Berghella V (2015 Nov) Induction of labor at full term in uncomplicated singleton gestations: a systematic review and metaanalysis of randomized controlled trials. Am J Obstet Gynecol 213(5):629–636. https://doi.org/10.1016/j.ajog.2015.04.004
Author information
Authors and Affiliations
Contributions
Dmitry A. Loktionov: the acquisition, analysis, and interpretation of data for the work; contributions to the design of the work; drafting the work; guarantor
Claire M. McCarthy: final approval of the version to be published; contributions to the design of the work; interpretation of data for the work; revising it critically for important intellectual content; guarantor
Mark C. Skehan: contributions to the conception of the work; final approval of the version to be published
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Statement of human rights
For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Loktionov, D., McCarthy, C.M. & Skehan, M.C. Does an elective induction policy negatively impact on vaginal delivery rates? A 30-month review of an elective induction policy. Ir J Med Sci 188, 563–567 (2019). https://doi.org/10.1007/s11845-018-1883-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-018-1883-1