Abstract
Introduction
Point prevalence surveys (PPS) are increasingly used to examining and compare hospital antibiotic consumption. The aim of this study was to identify the (1) point prevalence of antibiotic use in one regional hospital and (2) compare PPS data from similar regional/general hospitals.
Methods
Data were collected on all inpatients with an active antibiotic prescription and on all prescriptions issued in the emergency department over a 24-h period. Point prevalence data were obtained from three other regional/general hospitals.
Results
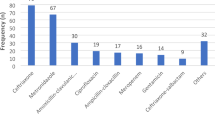
The frequency of antibiotic use was hospital A = 29%, B = 38%, C = 34% and D = 37%. Overall, the most commonly prescribed antibiotic was co-amoxiclav (30%), followed by macrolides (12%). However, new generation broad-spectrum antibiotics, such as piperacillin/tazobactam or ciprofloxacin, were also commonly used. Prescribing for common conditions such as respiratory infection or cellulites showed diverse antibiotic selection.
Conclusion
Point prevalence survey data using a standardised methodology could facilitate both local audit and national benchmarking to monitor antibiotic use.


Similar content being viewed by others
References
WHO (2001) Global strategy for containment of antimicrobial resistance. http://www.who.int/drugresistance. Accessed 11 Nov 2010
Goossens H (2005) European status of resistance in nosocomial infections. Chemotherapy 51(4):177–181
Livermore D (2004) Can better prescribing turn the tide of resistance? Nat Rev Microbiol 2(1):73–78
Mackenzie FM, Struelens MJ, Towner KJ, Gould IM (2005) Report of the Consensus Conference on Antibiotic Resistance; Prevention and Control (ARPAC). Clin Microbiol Infect 11(11):938–954
HSE-HPSC (2009) Health Protection Surveillance Centre Annual Report 2008. http://www.hpsc.ie. Accessed 11 Nov 2010
SARI (2001) Strategy for the control of antimicrobial resistance in Ireland. http://www.hpsc.ie. Accessed 22 Nov 2010
HSE-HPSC (2010) Hospital antimicrobial consumption report: sept Q1 Q2. http://www.hpsc.ie. Accessed 11 Nov 2010
Vlahovic-Palcevski V, Dumpis U, Mitt P et al (2007) Benchmarking antimicrobial drug use at university hospitals in five European countries. Clin Microbiol Infect 13(3):277–283
Bergman U, Popa C, Tomson Y et al (1998) Drug utilization 90%—a simple method for assessing the quality of drug prescribing. Eur J Clin Pharmacol 54(2):113–118
Kern WV, de WK, Steib-Bauert M, Fellhauer M, Plangger A, Probst W (2005) Antibiotic use in non-university regional acute care general hospitals in southwestern Germany, 2001–2002. Infection 33(5–6):333–339
Ansari F, Erntell M, Goossens H, Davey P (2009) The European surveillance of antimicrobial consumption (ESAC) point-prevalence survey of antibacterial use in 20 European hospitals in 2006. Clin Infect Dis 49(10):1496–1504
Kanerva M, Ollgren J, Lyytikainen O (2007) Antimicrobial use in Finnish acute care hospitals: data from national prevalence survey. J Antimicrob Chemother 60(2):440–444
McNulty CA, Francis NA (2009) Optimizing antibiotic prescribing in primary care settings in the UK: findings of a BSAC multi-disciplinary workshop. J Antimicrob Chemother 65(11):2278–2284
Arnold SR, Straus SE (2005) Interventions to improve antibiotic prescribing practices in ambulatory care. Cochrane Database Syst Rev (4). doi:10.1002/14651858.CD003539.pub2
Naughton C, Feely J, Bennett K (2009) A RCT evaluating the effectiveness and cost-effectiveness of academic detailing versus postal prescribing feedback in changing GP antibiotic prescribing. J Eval Clin Pract 15(5):807–812
Acknowledgments
We would like to thank all the nursing, pharmacy, medical staff and senior hospital management in each of the four hospitals for their ongoing support and help in this area.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Naughton, C., Hennessy, Y., Mannion, C. et al. A comparison of antibiotic point prevalence survey data from four Irish regional/general hospitals. Ir J Med Sci 180, 457–461 (2011). https://doi.org/10.1007/s11845-011-0677-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-011-0677-5