Abstract
Some cases of chronic rhinosinusitis (CRS) require surgical treatment and postoperative nasal packing, but bleeding and adhesion are common complications after nasal surgery. Biodegradable drug-loaded implants hold great therapeutic options for the treatment of CRS, but little data are available regarding the properties and effects of a novel drug-loaded haemostatic sponge (DLHS) in the nasal cavity and sinus. In this study, in vitro and in vivo experiments were used to test the physicochemical properties and investigate the biocompatibility and effectiveness of DLHS. The results showed that DLHSs present outstanding porosity and liquid absorption capacity, which might enhance their haemostatic ability, and they possess sustained-release ability for drugs. Further clinical trials confirmed their clinical efficacy and safety, and there was no evidence of adrenal cortical suppression. This study demonstrates the safety and efficacy of a novel biodegradable drug-loaded sponge with the possibility of being used in CRS patients, and it may reduce inflammation and minimize adhesions via controlled local drug delivery without measurable systemic exposure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic rhinosinusitis (CRS) is a long-term mucosal inflammatory disease. In China, the prevalence rate of CRS is up to 8%, affecting more than 100 million people and leading to a serious socioeconomic burden,1 and approximately 20% of patients with CRS require operative intervention.2 Endoscopic sinus surgery (ESS) may be the most useful intervention approach for treating CRS thus far.3 However, bleeding and adhesion are common complications after nasal surgery.4 Adhesion occurs in approximately 36% of patients, which might be an important factor for poor prognosis, because of impeding mucociliary clearance, and might result in persistent CRS symptoms after ESS. In terms of ESS, various haemostatic biomaterials need to be developed with the desire to reduce postoperative surgical complications and to improve patient outcomes. Some substantial research and development of nasosinusal implantation materials can deliver continuous, anti-inflammatory medications directly to the sinus mucosa after ESS, in the hope of haemostasis, adhesion prevention, and topical medication delivery to prevent disease recurrence and to reduce the need for systemic therapy.5
Because the nasosinusal mucosal inflammatory nature is characterized by type−2 cytokines, as well as the activation and recruitment of eosinophils and mast cells, high-quality evidence has proven that corticosteroids are effective and safe for treating patients with CRS. Corticosteroids have lower drug-induced risks and are widely considered to be treatment evidence 1a for CRS.6,7 Therefore, corticosteroids are often recommended as the mainstay of drug treatment by the current CRS guidelines, because they can inhibit the activation of eosinophils in the nasal mucosa and accelerate the recovery of nasal mucosa function because they act on the inflammatory nature of the disease.8 Meanwhile, sodium hyaluronate (SH) is involved in the regulation of vasomotor tone and gland secretion and it stimulates mucociliary clearance.9 Some studies have indicated that SH for nasal douching in addition to standard corticosteroids showed significantly fewer symptoms and better endoscopic appearance associated with CRS, and that this effect seems to be highlighted in patients with allergic CRS.10,11
Recent studies have shown that soaking packing materials Nasopore (Polyganics) with corticosteroids during surgery improves the endoscopic appearance of the sinus during the healing process of CRS after ESS.12 However, this treatment may result in uncontrolled and inconsistent drug release from the nasal packing material. For these reasons, choosing a novel nasal drug-loaded implant can deliver the drug to the mucosal contact site stably and for a long time which may assist in solving some of these problems.13 Carboxymethyl chitosan (CMCS) has attracted great attention in the field of haemostasis because of its wide range of sources, nontoxicity, hydrophilicity, and air permeability.14 Chitosan is a kind of natural polysaccharide produced by the deacetylation of chitin, and is composed of glucosamine and n-acetyl glucosamine. Chitosan possesses a wide variety of applications due to its functional properties, such as its antibacterial activity,15 potentiation of the coagulation cascade, and ability to improve the degree of patency for all ostia.16 In addition to these excellent properties, chitosan possesses potential applications in biomedical fields, including wound dressing, tissue engineering, and therapeutic drug delivery.17 Therefore, carboxymethylcellulose (CMC), CMCS, SH, and budesonide (BUD) have been used as the main materials to make a drug-loaded haemostatic sponge (DLHS) in the hope of diminishing bleeding after ESS. Meanwhile, the DLHS was formulated with BUD and SH for local sustained release of medication to the affected mucosa, which prevents adhesion, maintains ostial patency, reduces postoperative inflammation, and promotes mucosal healing.
Materials and Methods
Device Description
DLHS is a sterile, bioabsorbable, chitosan-based implant developed by our team. The structural properties of DLHS derive predominantly from CMCS and SH, which provide physical pressure on the mucosa as well as bioabsorbability, and can be used as a carrier in drug delivery. Each DLHS measures 4 cm × 2 cm × 1.5 cm, contains 1 mg BUD and 0.67 mg SH, and is designed to provide controlled local delivery of corticosteroids over 14 days.
Evaluation of the Liquid Absorption Capacity of the DLHS
First, all the DLHS were dried thoroughly in a vacuum dryer. To avoid influencing the experimental results, the testing process was completed at the same place and in the same time period to exclude the interference of environmental factors. The experimental liquid consisted of a solution of sodium chloride and calcium chloride containing 142 mmol sodium ions and 2.5 mmol calcium ions, which was equivalent to human serum or wound exudate. DLHS with a volume of 4 cm × 2 cm × 1.5 cm and a weight of 0.31 g were immersed in a culture dish containing the experimental liquid at a constant temperature of 37 °C. After 2 min, the DLHS was removed from the culture dish and hung for 30 s to drain the nonretentive liquid. Then, the sponge was immediately weighed to measure the wet weight.
The liquid absorption ratio (LAR) of the DLHS was defined using:
where Mb and Ma are the weights of fully saturated sponges with water and dry sponges, respectively.
Scanning Electron Microscopy (SEM)
The microstructure of the DLHS was observed by a scanning electron microscope (S-4800; Hitachi, Japan). All the samples were fully dried at 60 °C in a vacuum and treated with gold spraying before observation.
DLHS Sustained Release Drug Experiment
The DLHS (BUD loading 1.5 mg) was placed into a dialysis bag, and the molecular weight of the bag interception was 14,000. The bag was then placed in 200 mL release medium (pH 6.2 phosphate buffer/ethanol = 80/20) and was shaken at 30 rpm using a shaker incubator maintained at 37 °C. At predetermined intervals, 5 mL supernatant was taken, and UV absorbance readings were taken at 310 nm to determine the quantity of the drug released. All the measurements were performed in triplicate, and the data were plotted as the average of the drug released at specific time points.18
In Vitro Cytotoxicity Assay
Human nasal mucosal epithelial cells (Shanghai Yaji Biotechnology, China) that grew vigorously on the 3rd day of subculture were inoculated into 96-well plates at a density of 1 × 103 cells/well. After 24 h of conventional culture, the original medium and nonadherent cells were discarded. The cells were then randomly divided into an experimental group and a control group (n = 6), including 12 experimental groups. The experimental groups were treated with the extract of DLHS, the control group was treated with the extract of Nasopore (Polyganics), and the cultures were maintained under the same conditions. The cells in each group were cultured at different time points (24 h and 48 h), and 10 μL CCK-8 reagent was added to each well. After 4 h of culture under the same conditions, the absorbance was determined at 450 nm, and the morphology of the cells was observed using a microscope. Cell viability (CV) was determined as follows:
where AE represents the absorbance of the experimental groups and AN represents the absorbance of the negative control groups.
In Vivo Performance Assay
Experimental Animals
A total of 36 adult (12-month-old) male mice (weight, 300–400 g) were used in the current study. The mice were supplied by the Animal Laboratory Centre of Ningbo University (Ningbo, China), and maintained under controlled conditions: atmosphere, 20–25 °C, 12-h light/dark cycle and humidity of 40–60% and had free access to standard water and food (SYXK-2019-0005). All procedures were conducted in accordance with the “Guiding Principles in the Care and Use of Animals” (China).
The mice were randomized into three groups (n = 12/group): A, B, and C. The anaesthetic procedures, painless surgeries, and euthanasia procedures were approved by the ethics committee of Ningbo Municipal Hospital of TCM (Ningbo, China). The mice were treated according to the requirements of the local animal ethics commission.
Surgical Methods
The mice were anaesthetized via intramuscular injections (50 mg/kg ketamine + 5 mg/kg xylazine hydrochloride) and immobilized in a ventricumbent position with their faces shaved. A longitudinal 1.5-cm incision was formed along the nasal dorsum, and the skin and underlying tissue were scraped from the premaxilla. The periosteum was freed and retracted laterally, and a small hole with a diameter of approximately 1.5 mm × 1.5 mm was drilled. Ophthalmic forceps were used to insert a 1 mm × 1 mm × 2 mm experimental specimen into the drilled maxillary sinus. Group B was put into the Nasopore, group C was put into the DLHS, and group A was put into nothing. The incision was sutured to prevent infection. Two weeks after surgery, the mice were euthanized after drawing blood via the heart, and the sinus mucosa was harvested for histological analyses and laboratory inspection. IL-1β, IL-4, IL-5, IL-8, TNF-α, and cortisol concentrations were determined using an enzyme-linked immunosorbent assay (ELISA). At this time, the plasma sample was collected, and the entirety of the maxillary sinus mucosa from each side was harvested separately for BUD detection. BUD was extracted from the plasma samples via solid-phase extraction and from the maxillary sinus mucosa samples via liquid-phase extraction, and the concentrations of BUD in each sample were calculated by using reverse-phase high-performance liquid chromatography.
Statistical Analysis
All the data are presented as the mean ± standard deviation. Statistical analyses were performed using Student’s t test. P < 0.05 was considered statistically significant. Statistical analyses were performed using the SPSS® v.22.0 statistical software package.
Results and Discussion
DLHS should be primarily used to control haemorrhage but can also help to prevent adhesion formation, promote drainage of the sinus mucosa and wound healing and has superior clinical treatment effects. The ideal drug-loaded biomaterial should be efficacious in controlled sustained release drugs as well as biodegradable and biocompatible.19 Corticosteroids remain the standard in the treatment of CRS by reducing eosinophilic infiltrates and type−2 inflammation.20 CS is regarded as a promising tool for several biological and medical applications due to its inherent promotion of mucosal healing and potential hemostatic ability.21 Research shows that SH added to corticosteroids can reduce nasal mucosa inflammation with notable therapeutic benefits.9 Both CS and SH are naturally degradable polymer materials with good biocompatibility and are often used as carriers for the preparation of various slow-release systems.
Characterization of the DLHS
A strong liquid absorptive capacity is a necessary property of hemostatic sponges, which is conducive to accelerating blood coagulation.22 Considering the importance of improving the liquid absorption capacity to achieve rapid hemostasis, CMC, containing a large number of hydrophilic carboxymethyl functional groups, was introduced into the solution, which makes the DLHS have a super-liquid absorption capacity. The finding of the liquid absorptive capacity test (Fig. 1) shows that the LAR of DLHS was 258% of its own weight, which is attributed to its high porosity and strong hydrophilicity, indicating that it might have good hemostatic function. Meanwhile, the DLHS also exhibited a satisfactory resilience, as shown in Fig. 2, and should be able to exert a certain pressure on the sinus cavity.
Microscopy also makes it possible to explore the characteristic network structure of the implant.23 The microstructure and pore size distribution of DLHS significantly affect cell proliferation and function. The prepared DLHS had a uniform pore size distribution of approximately 200 μm, as shown in Fig. 3. The porous material was prepared by freeze-drying and high-speed stirring of the surfactant and polysaccharide, which not only gave it a uniform structure and high porosity but also enhanced its mechanical strength and was beneficial for accelerating hemostasis.14
In Vitro Drug Release Studies
Drug release studies of the BUD formulation were performed for 14 days. The results show that BUD was released sustainably in a time-dependent manner from the DLHS for 72 h before reaching equilibrium, followed by a sustained release of the drug BUD, as shown in Fig. 4. The DLHS was oscillated at suitable speeds using an oscillating incubator maintained at 37 °C to simulate the internal environment. The drug release curve in vitro can be determined by calculating the cumulative drug release percentage and time, which can more closely reflect the drug release of DLHS in vivo.
Biocompatibility and Biosafety Evaluation
The ideal drug-eluting biomaterial should be bioabsorbable, biocompatible, and efficacious in drug elution.19 To ensure the safety of the hybrid hemostatic sponges, both cytocompatibility assays and animal experiments were conducted. The CCK-8 assay was performed to evaluate the cytocompatibility of the DLHS. The cytotoxicity for all the tests was recorded at 24- and 48-h intervals, as shown in Fig. 5. According to the formula, the CV value of the negative control group should always be equal to 100%. The relative cell viability rate of epithelial cells reached 96.8% and 97%, and 89.8% and 87.5%, after the DLHS group and Nosapore group incubation within 24 and 48 h, respectively. These results demonstrated that DLHS could promote cell proliferation to some extent and exhibited good biocompatibility.
Animal experiments can provide drug release information in vivo, adverse reactions, the effects of combination drugs on nasal histology, and monitor inflammatory changes in the nasosinusal mucosa over a period of time.24 When the DLHSs were placed on intact mucosa, they had basically degraded by day 14 and could be easily cleaned with an aspirator, and no additional surgeries were required to remove them. HE staining (Fig. 6) showed that the nasal sinus mucosa epithelial tissue structure was regular and neatly arranged in the DLHS group, a few goblet cells were occasionally observed, and no obvious inflammatory cell infiltration was found in the submucosa. The epithelium of the control group and the nasopore group was swollen, with large nuclei and multiple lesions or dismemberment. Numerous inflammatory cell infiltrates, including neutrophils, eosinophils, and lymphocytes, were observed in the subepithelium and lamina propria, with submucosal gland hyperplasia, and there was a trend towards reduced mucosal inflammation when compared to the control and nasopore groups, with statistically significant differences. The DLHSs were confirmed by histologic analysis with minimal associated inflammatory reactions.
Surgical procedure (SP). A small hole with a diameter of approximately 1.5 mm × 1.5 mm was drilled in the nasal dorsum, while the sinus mucosa was completely preserved. Group B was put into the Nasopore, group C into the DLHS group, and group A into nothing. HE staining showed that the nasal sinus mucosa epithelial tissue structure was regular and neatly arranged in group C, and the epithelium of group A and group B were swollen, with large nuclei and multiple lesions or dismemberment. A the control group, B the Nasopore sponge group, C the DLHS group.
The inflammatory response in CRS is also associated with elevated levels of proinflammatory cytokines, and the levels of IL-1β, IL-6, IL-5, IL-8, and TNF-α were significantly elevated in the sinus mucosa of patients suffering from CRS.25 IL-5 regulates various inflammatory responses that promote the rapid clearance of pathogens, but it also contributes to the pathology in chronic inflammation and is a key mediator in type−2 eosinophilic inflammation.26,27 The chemokine IL-8 is a proinflammatory cytokine that is important in eosinophil chemotaxis, and a significant increase in IL-8 can be observed after allergen challenge.28 However, TNF-α plays a role in bacterial infections but is not involved in allergen-induced reactions.29 Oral corticosteroids can exert a beneficial effect in treating CRS by significantly reducing the levels of IL-6 and TNF-α.25 In this study, a series of serum and sinus mucosal inflammatory factors were detected, and the serum levels of IL-8, IL-5, and TNF-α and mucosal levels of IL-8, IL-5, TNF-α, and IL-4 were significantly downregulated in group C compared with groups A and B, as shown in Figs. 7 and 8.
The serum levels of IL-8, IL-5, and TNF-α were significantly downregulated in group C compared with groups A and B, and there were no significant changes in IL-1β, IL-4, or cortisol among the three groups. # P < 0.05, ## P < 0.01 versus group A, * P < 0.05, ** P < 0.01 versus group B. A Control group, B Nasopore sponge, C DLHS.
The mucosal levels of IL-8, IL-5, TNF-α, and IL-4 were significantly downregulated in group C compared with groups A and B, but the expression of mucosal cortisol was upregulated. No significant changes in IL-1β or cortisol were observed among the three groups. # P < 0.05, ## P < 0.01 versus group A, * P < 0.05, ** P < 0.01 versus group B. A Control group, B Nasopore sponge, C DLHS.
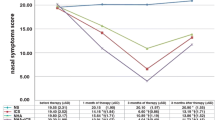
Drug delivery plasma BUD concentrations at time points 1, 3, 7, and 14 days are shown in Fig. 9. The BUD concentration in the maxillary sinus mucosa at day 14 was 7038.3 ± 1732.3 ng/g. In terms of the efficacy of drug delivery, the DLHS effectively delivered BUD locally to the sinus mucosal tissues but not in the serum. However, the mean cortisol concentrations at baseline and at the follow-up time points were within normal limits, which indicated no evidence of adrenal suppression. Meanwhile, DLHSs downregulated the levels of inflammatory factors in the serum and sinus mucosa and improved the inflammation of the nasal sinus mucosa.
Our experimental study showed that the property analysis regarding the sample composition results shows that the DLHS possesses good characteristics and favorable bioabsorbability and biocompatibility. Nevertheless, this study has several limitations. We could not speculate on the mechanisms of coagulation and whether to inhibit type−2 inflammatory responses. Clinical trials should be conducted to further validate the biological effects of the DLHS.
Conclusion
The excellent performance of the DLHSs with a low density, interconnected microchannel architecture, strong liquid absorption capacity, and sustained drug release has been shown. In vivo and in vitro experiments revealed anti-inflammatory effects, and no cytotoxicity or mucosal damage, which confirmed the biosafety and effectiveness of the DLHS. These results indicate that the DLHS possesses a high potential for achieving not only rapid hemostasis but also better anti-inflammatory properties, with reliable biosafety, biodegradability, and biocompatibility.
Data Availability
The data supporting the findings of this study are available within the article.
References
C. Bachert, N. Zhang, C. Cavaliere, W. Weiping, E. Gevaert, and O. Krysko, J. Allergy. Clin. Immunol 145, 725 (2020).
S. Fujieda, Y. Imoto, Y. Kato, T. Ninomiya, T. Tokunaga, T. Tsutsumiuchi, K. Yoshida, M. Kidoguchi, and T. Takabayashi, Allergol. Int 68, 403 (2019).
T.C. Wang, C.J. Tai, Y.A. Tsou, L.T. Tsai, Y.F. Li, and M.H. Tsai, Eur. Arch. Otorhinolaryngol 272, 1825 (2015).
R.S. Miller, D.L. Steward, T.A. Tami, M.J. Sillars, A.M. Seiden, M. Shete, and C. Paskowski, J. Welge. Otolaryngol. Head. Neck. Surg 128, 862 (2003).
C.J. Massey, J.D. Suh, B. Tessema, S.T. Gray, and A. Singh, Otolaryngol. Head. Neck. Surg 154, 606 (2016).
W.J. Fokkens, Rhinology 58, 1 (2020).
C.B. Small, P. Stryszak, M. Danzig, and A. Damiano, J. Allergy. Clin. Immunol 121, 928 (2008).
C. Wang, H. Lou, X. Wang, Y. Wang, E. Fan, Y. Li, H. Wang, C. Bachert, and L. Zhang, J. Allergy. Clin. Immunol 135, 922 (2015).
E. Cantone, and M. Iengo, Am. J. Rhinol. Allergy 30, 340 (2016).
M. Casale, A. Moffa, L. Sabatino, A. Pace, G. Oliveto, M. Vitali, P. Baptista, and F. Salvinelli, PLoS ONE 10, e0130637 (2015).
E. Savietto, G. Marioni, P. Maculan, A. Pettorelli, B. Scarpa, E. Simoni, L. Astolfi, R. Marchese-Ragona, and G. Ottaviano, Am. J. Otolaryngol. 41, 102502 (2020).
K.Q. Zhao, Y.Q. Yu, and H.MYu. Int, Forum. Allergy. Rhinol 8, 1233 (2018).
A. Parikh, U. Anand, M. Ugwu, T. Feridooni, E. Massoud, and R. Agu, Pharmaceutics 6, 249 (2014).
L. Wang, Y. Zhong, C. Qian, D. Yang, J. Nie, and G. Ma, Acta. Biomater 114, 193 (2020).
A. Muxika, A. Etxabide, J. Uranga, P. Guerrero, and K. de la Caba, Int. J. Biol. Macromol. 105, 1358 (2017).
F. Wang, Y. Pang, G. Chen, W. Wang, and Z. Chen, Carbohydr. Polym. 229, 115529 (2020).
Y. Zhang, T. Sun, and C. Jiang, Acta. Pharm. Sin. B 8, 34 (2018).
M. Fan, Q.F. Guo, J.C. Luo, F. Luo, P. Xie, X.H. Tang, and Z.Y. Qian, J. Biomater. Appl 28, 288 (2013).
V.S. Patel, E. Walgama, A. Psaltis, F. Lavigne, S.D. Pletcher, and P.H. Hwang, Am. J. Rhinol. Allergy 31, 382 (2017).
J. Shen, K. Welch, and R. Kern, Expert. Rev. Clin. Pharmacol 11, 1163 (2018).
F.Y. Song, Y. Kong, C.Y. Shao, Y. Cheng, J. Lu, Y.H. Tao, J. Du, and H.S. Wang, Acta. Biomater 136, 170 (2021).
R.N. Udangawa, P.E. Mikael, C. Mancinelli, C. Chapman, C.F. Willard, T.J. Simmons, and R.J. Linhardt, ACS. Appl. Mater. Interfaces 11, 15447 (2019).
Y. Wang, Y.T. Wei, Z.H. Zu, R.K. Ju, M.Y. Guo, X.M. Wang, Q.Y. Xu, and F.Z. Cui, Pharm. Res 28, 1406 (2011).
B.S. Bleier, D.P. Paulson, B.W. O’Malley, D. Li, J.N. Palmer, A.G. Chiu, and N.A. Cohen, Am. J. Rhinol. Allergy 23, 76 (2009).
C.M. Lennard, E.A. Mann, L.L. Sun, A.S. Chang, and W.E. Bolger, Am. J. Rhinol 14, 367 (2000).
M. Dougan, G. Dranoff, and S.K. Dougan, Immunity 50, 796 (2019).
K. Avdeeva, and W. Fokkens, Curr. Allergy. Asthma. Rep 18, 25 (2018).
A. KleinJan, M.D. Dijkstra, S.S. Boks, L.A. Severijnen, P.G. Mulder, and W.J. Fokkens, J. Allergy. Clin. Immunol 103, 441 (1999).
N. Van Bruaene, C. Perez-Novo, K. Van Crombruggen, N. De Ruyck, G. Holtappels, P. Van Cauwenberge, P. Gevaert, and C. Bachert, Clin. Exp. Allergy 42, 883 (2012).
Funding
This work was supported by the Zhejiang Provincial Health Science and Technology Foundation, China (Grant No. 2021PY069) and the University-level Fund of Zhejiang Chinese Medicine University (Grant No. 2021FSYYZY09).
Author information
Authors and Affiliations
Contributions
LW, JM, JX, WW, JW, JH, DW, XZ and MX built the experimental system, collected and analyzed the data. LW and JM wrote the manuscript and writing of the main body, formatting. MX supervised the main idea and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, L., Meng, J., Jia, X. et al. Properties and Effects of a Drug-Loaded Haemostatic Sponge. JOM 75, 5619–5627 (2023). https://doi.org/10.1007/s11837-023-05948-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11837-023-05948-7