Abstract
Purpose
Pediatric healthcare systems must support childhood cancer survivors to optimize their transition to adult care. This study aimed to assess the state of healthcare transition services provided by Children’s Oncology Group (COG) institutions.
Methods
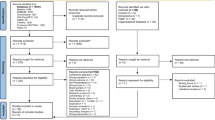
A 190-question online survey was distributed to 209 COG institutions to assess survivor services, including transition practices, barriers, and implementation of services aligned with the six core elements of Health Care Transition 2.0 from the US Center for Health Care Transition Improvement.
Results
Representatives from 137 COG sites reported on institutional transition practices. Two-thirds (66.4%) of site discharge survivors to another institution for cancer-related follow-up care in adulthood. Transfer to primary care (33.6%) was a commonly reported model of care for young adult-aged survivors. Site transfer at ≤ 18 years (8.0%), ≤ 21 years (13.1%), ≤ 25 years (7.3%), ≥ 26 years (12.4%), or when survivors are "ready" (25.5%). Few institutions reported offering services aligned with the structured transition process from the six core elements (Median = 1, Mean = 1.56, SD = 1.54, range: 0–5). The most prevalent barriers to transitioning survivors to adult care were perceived lack of late-effects knowledge among clinicians (39.6%) and perceived lack of survivor desire to transfer care (31.9%).
Conclusions
Most COG institutions transfer adult-aged survivors of childhood cancer elsewhere for survivor care, yet few programs report delivering recognized standards for quality healthcare transition programming to support survivors.
Implications for Cancer Survivors
Development of best practices for survivor transition is needed to help promote increased early detection and treatment of late effects among adult survivors of childhood cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Approximately 85% of children and adolescents diagnosed with cancer will become long-term survivors [1], leading to a growing survivor population with unique healthcare needs. Studies have shown that 60–90% of adult-aged survivors of childhood cancer have ≥ 1 chronic condition, with 25–80% having severe or life-threatening conditions [2, 3]. The National Academy of Medicine and Children’s Oncology Group (COG) recommends that survivors participate in continuous, risk-based survivor care across the lifespan to monitor for late effects of their previous cancer treatments [4, 5]. Facilitating healthcare transition and eventual transfer of risk-based survivor care from pediatric to adult settings is critical to the long-term health of childhood cancer survivors, since their morbidity and mortality risks increase significantly over time and do not reach a plateau [2, 3, 6].
Healthcare transition has been conceptualized as a process leading to an event: the process necessitates gradual, planned movement toward an adult-centered model for healthcare (i.e., transition), while the event occurs when the patient transfers from a pediatric to an adult healthcare team (i.e., transfer) [7, 8]. Historical healthcare transition practices in pediatric oncology have been insufficient, given that fewer than half of adult-aged survivors of childhood cancer remain actively engaged in survivor care [9,10,11]. Research on patient- and provider-reported barriers to healthcare transition for pediatric cancer survivors has become more abundant [10, 12,13,14,15,16,17,18,19], yet data characterizing available transition support services for survivors remain inadequate [12, 16]. In a systematic review of global transition practices, Otth et al. (2020) identified only three studies describing detailed transition processes for adult survivors of childhood cancer in the USA or Canada. Future efforts to improve access and engagement in risk-based care among adult-aged survivors of childhood cancer must be informed by the gaps and barriers to healthcare transition services offered by pediatric oncology institutions.
To improve organizational healthcare transition practices, the US Center for Health Care Transition (Got Transition®; https://www.gottransition.org/) developed and disseminated six core elements of Health Care Transition [20, 21]. These six core elements offer a framework for clinicians and institutions to provide a structured transition process with patients and their caregivers, beginning early in adolescence and continuing into young adulthood. The six core elements include guidance on transition and care policy development and dissemination (Core Element 1), establishing criteria and processes for tracking and monitoring transition-aged youth (Core Element 2), conducting regular transition readiness assessments (Core Element 3), the steps involved in transition planning (Core Element 4) and transfer of care (Core Element 5), and confirming transfer completion (Core Element 6). The six core elements of Health Care Transition have been endorsed by the American Academy of Pediatrics (AAP), American Academy of Family Physicians (AAFP), and the American College of Physicians (ACP) [20] and incorporated into consensus statements on managing the transition to adult-centered healthcare for youth with a wide variety of special healthcare needs [22,23,24,25]. For youth with healthcare needs, these types of structured healthcare transition practices have been shown to result in improvements in adherence to care and adult ambulatory visits, satisfaction with care, and quality of life, while also reducing barriers to care and decreasing the time between last pediatric and first adult visits [26, 27]. Improvements in these health outcomes are critically needed among adult survivors of childhood cancer [9,10,11]; thus, the six core elements are relevant to pediatric survivor care delivery.
The goals of this study were to (1) describe the state of healthcare transition services provided by COG institutions, (2) evaluate pediatric oncology service alignment with the six core elements of Health Care Transition, and (3) reassess perceived barriers to transferring survivors to adult long-term follow-up care previously studied in a 2007 COG survey [13].
Methods
We conducted a cross-sectional survey to assess survivorship services offered by COG institutions [28], including healthcare transition supports. An online survey was made available from October 26, 2017 to February 23, 2018, on SurveyMonkey. Emory University’s Institutional Review Board (IRB) determined the study to be exempt from IRB review.
Sample and procedures
Potential respondents were COG Principal Investigators (PIs) or the institutional contact in the COG Late Effects Directory of Services at existing member institutions (n = 209). COG leadership sent an introductory email and survey instructions to one individual per institution. Following the introductory email, Emory University researchers emailed a link to complete the online survey. Two additional email notifications were sent at 2-week intervals. Any non-responding institutions were then approached personally by members of the COG Outcomes and Survivorship, Adolescent and Young Adult, and Nursing committees and invited to participate.
Measures
The current analysis is derived from a subset of a 190-item online survey assessing cancer survivorship practices, services, and care delivery at COG institutions [28]. In follow-up to a 2007 survey of COG survivorship practices [13], respondents were asked to report institutional characteristics, including institution type, size, upper age limits for newly diagnosed patients, institutional policies on age at transfer, and models of care for adult survivors of childhood cancer.
If respondents reported their institution transferred patients out for long-term follow-up care in adulthood (e.g., their institution transferred patients at a certain age or transferred survivors "when they are ready"), they were asked to complete nine items related to healthcare transition programming. These items included identifying (1) the top two most difficult barriers to transitioning survivors to adult care providers for cancer-related care, (2) care team members involved in introducing and coordinating transition, (3) when in the cancer trajectory sites typically introduce the concept of transition, and (4) if sites had implemented transition programming (6 items) aligned with the six core elements of Health Care Transition 2.0 from the US Center for Health Care Transition Improvement [14]. If respondents reported their patients are “seen indefinitely and not transferred elsewhere,” they were not asked any further questions about institutional healthcare transition supports. All respondents were allowed to omit responses to individual questions at their discretion.
Data analysis
Frequencies were used to summarize institutional characteristics, healthcare transition practices, and barriers to transition. Institutions were dichotomized based on whether or not they transferred patients out for long-term follow-up care in adulthood. Institutions reporting their patients are “seen indefinitely and not transferred elsewhere” on the institutional policies on age at transfer question were categorized as not transferring patients. Institutions transferring patients at a certain age (i.e., age 18, 21, 25, 26, or older) or transferring “when they are ready” without age-based limitations were categorized as transferring patients.
Associations between institutional characteristics (e.g., type and size) and transfer of young adult patients were determined using chi-square tests. The total number of US Center for Health Care Transition Improvement Core Elements offered at each COG institution was summed, and descriptive statistics were used to characterize healthcare transition services. One-way ANOVAs and Tukey’s HSD post hoc tests were performed to compare differences between institutions on the number of healthcare transition services provided. Kruskal-Wallis tests were also performed to confirm parametric results due to the distribution of the number of healthcare transition services provided. Non-parametric post hoc tests were adjusted by the Bonferroni correction for multiple tests. All analyses were conducted using SPSS Statistics, Version 27.0 (IBM Corp, Armonk, NY), with p-values < 0.05 considered statistically significant.
Results
Representatives from 153 of the 209 invited COG institutions responded to the parent survey (73.2% response rate). Of these, 137 institutions (89.5%) completed survey items about their healthcare transition practices and were included in these analyses. Institution characteristics are outlined in Table 1.
Transfer of survivors and models of care
Two-thirds of institutions (91/137) transfer survivors out of their pediatric programs to receive adult-focused cancer survivorship care (Table 1). These transfers often occur following age-based institutional policies at COG sites beginning at ≤ 18 years (8.0%), ≤ 21 years (13.1%), ≤ 25 years (7.3%), or ≥ 26 years (12.4%). In comparison, 25.5% of institutions do not have age limitations related to transition and transfer survivors “when they are ready.” There was a significant relationship between institution type and requirements to transfer young adult patients for survivor care, with freestanding children’s hospitals being more likely to transfer (81.4%), compared to other institution types (59.6%; p = .012, Cramer’s V = 0.21). The percentage of institutions requiring transfer of care did not differ by program size (p = .084).
Continuation of care at the pediatric center/treating institution (33.6%) and transfer to primary care (33.6%) were equally common models of long-term follow-up care for young adult survivors of childhood cancer (Table 1). Some sites (13.9%) reported transferring to adult oncology or adult cancer survivor programs, while few (5.1%) reported typically transferring patients to specialty clinics for young adult-aged survivors of childhood cancer.
Introduction of healthcare transition and barriers to transitioning survivors
Among the ninety-one institutions transferring survivors for adult long-term follow-up care (Table 2), the concept of transition is often introduced to patients during pediatric survivorship care (89.0%) and less frequently at earlier points during the cancer trajectory (e.g., diagnosis, during treatment, and end of treatment). The multidisciplinary staff typically involved in introducing survivors to the concept of transition most frequently include survivorship care providers. The top three barriers to transitioning survivors to adult care reported by institutions included (1) perceived “lack of late-effects knowledge among clinicians survivors are transferred to” (39.6%), (2) perceived “lack of survivor desire to leave comfort of treating institution or oncologist” (31.9%), and (3) perceived “lack of survivor access to primary care provider for reasons other than insurance such as geography” (26.4%).
Alignment with the six core elements of health care transition
In regard to the US Center for Health Care Transition Improvement six core elements, only a minority of institutions reported having an established process to match and communicate with survivors’ adult providers (44.4%), incorporating transition readiness assessment into clinical practice (33.3%), having a patient navigator or care coordinator to facilitate transition (28.6%), having a written transition policy (24.2%), utilizing a transition readiness assessment tool (17.6%), and systematically obtaining feedback from young adults about the transition process (8.8%; Table 2). On average, institutions reported offering only one service aligned with any of the six core elements (Median = 1, M = 1.56, SD = 1.54), and no institution offered all six services (range: 0–5; Fig. 1).
Associations with the six core elements of Health Care Transition
There were differences in the number of healthcare transition services offered based on institution type (p = .002, η2 = .16). Children’s centers within adult hospitals offered fewer healthcare transition services (M = 0.82, SD = 1.25) than freestanding children’s hospitals (M = 1.94, SD = 1.55; p = .016), or children’s hospitals in close proximity to adult institutions (M = 2.19, SD = 1.63; p = .008). There was also a difference in the number of transition services offered based on institution size (p = .019, η2 = .13). The smallest programs (≤ 30 new oncology diagnoses per year) offered fewer transition services (M = 0.54, SD = 0.88) than midsize programs with 61–90 new oncology diagnoses per year (M = 2.11, SD = 1.88; p = .034) or large programs with > 150 new oncology diagnoses per year (M = 2.04, SD = 1.57; p = .032). Non-parametric tests yielded qualitatively equivalent findings for differences in the number of healthcare transition services offered based on institution type and size.
Discussion
The National Academy of Medicine and COG recommend continued survivor care throughout adulthood because morbidity and mortality risks increase over time for long-term survivors of childhood cancer [2,3,4,5,6]. Our results show that most COG institutions eventually transfer survivors of childhood cancer to another institution for cancer-related follow-up care during adulthood. Successful healthcare transition of adult-aged survivors of childhood cancer is critical for continued risk-based screening and early detection of late effects in adulthood [3], yet our study found that very few survivorship programs deliver comprehensive transition programming. In this first national survey of delivery of the six core elements of Health Care Transition 2.0 in pediatric oncology, no COG institutions reported offering healthcare transition services in complete alignment with recommendations from the US Center for Health Care Transition Improvement [21]. As in earlier studies of pediatric cancer survivorship programs [12, 13], our survey confirmed that institutions continue to vary in the age at which they transfer care and the type of healthcare model used to deliver survivor care to adult-aged survivors. Taken together, these results suggest there is no standard of care for transitional survivorship care across COG institutions and the development of best practices is needed to guide transition program development for childhood cancer survivors.
Within our sample of COG institutions that transferred adult-aged survivors, the most common model of survivorship care for young adult survivors of childhood cancer was transfer to primary care providers (PCPs). Previous studies have found that 73% of PCPs lack knowledge or training in survivorship care [29], and only 25–37% report being comfortable caring for survivors of childhood cancer [30]. Respondents to the current and 2007 survey [13] of COG survivorship practices endorsed “lack of late-effects knowledge among clinician survivors are transferred to ”as the most frequent barrier to transitioning survivors to adult care.” These findings are consistent with barriers related to the lack of adult providers with survivor expertise/knowledge frequently reported by pediatric oncologists [14] and survivorship providers [12]. Correspondingly, young adult survivors of childhood cancer have reported they perceive that their PCPs lack sufficient cancer knowledge and encounter difficulty finding good/regular PCPs [31]. In efforts to bridge these gaps, recent recommendations from the American Academy of Pediatrics (AAP) encourage PCPs to incorporate the COG Long-Term Follow-Up Guidelines [4] into their practice to deliver evidence-based surveillance to survivors [32]. These guidelines also recommend PCPs collaborate with oncology subspecialists to educate survivors and ensure successful transfer to adult-oriented survivor care. Future research is critically needed to evaluate the adoption and implementation of these recommendations for primary care-pediatric oncology partnerships and the subsequent impact of these recommendations on survivors’ healthcare transition outcomes.
Our results indicate that the responsibilities of introducing healthcare transition and preparing patients for transfer fall almost exclusively on survivorship programs, which are often under-resourced in terms of funding and dedicated time for program development [13, 28]. These barriers likely contribute to the concerning lack of systematic transition programming offered at COG institutions observed in this study. Kenney et al. [14] found that most pediatric oncologists identified the need for specific transition programs for survivors (77.4%, 264/347) and would support the allocation of departmental resources to support these types of programs (86.8%, 296/347). Without access to institutional programming to support transition preparation and transfer to adult care, it is not surprising that most survivors of childhood cancer discontinue risk-based care during their young adult years [9,10,11]. These findings underscore the need for investment in improved organizational programming at the health system level to better coordinate survivors’ healthcare transition and improve access to and engagement in lifelong risk-based survivor care.
Pediatric oncology and survivor programs should consider implementing health system supports to prepare survivors for healthcare transition and, if applicable, eventual transfer to adult-centered care. The US Center for Health Care Transition Improvement offers guides to assist clinicians and health systems in assessing their healthcare transition activities and implementing the six core elements of Health Care Transition [33] [https://www.gottransition.org/six-core-elements/]. These guides offer frameworks for supporting the transition to adult-centered care with or without a change in survivor care provider; thus, they are applicable regardless of whether or not institutions transfer survivors out for long-term follow-up care in adulthood. Our results suggest COG programs are most in need of developing written transition policies (Core Element 1 — Transition and Care Policy/Guide), adopting transition readiness tools (Core Element 3 — Transition Readiness), and establishing mechanisms to obtain feedback from young adult survivors about their transition process (Core Element 6 — Transfer Completion). Considerations for developing transition policies and eliciting elicit feedback from survivors on their experience with the transition process can be found on the Got Transition® website, along with sample policies and example feedback surveys [33]. Systematic reviews of health transition assessment tools [34, 35] have identified several measures that can be used to evaluate transition readiness, including the Transition Readiness Assessment Questionnaire (TRAQ) [36, 37], TRxANSITION Index [38], Self-management and Transition to Adulthood with Rx = treatment (STARx) [39], Readiness for Transition Questionnaire (RTQ) [40,41,42], Transition Q [43], and the California Healthy and Ready to Work Transition Assessment Tool (HRTW) [44, 45]. Specific to cancer survivorship, transition assessment tools have been developed or adapted for adolescent and young adult survivors of childhood cancer, including the Transition Readiness Inventory (TRI), Transition-Q [46], and Readiness for Transition Questionnaire (RTQ-Survivor) [47].
Our results build upon the knowledge garnered from previous surveys of COG members [14] and member institutions [12]. The strengths of this survey include [1] improvement in response rate, compared to previous studies, resulting in a large sample of COG institutions reporting on their healthcare transition practices and [2] novel data on service alignment with the six core elements of Health Care Transition within COG survivorship programs. There were also limitations to the work that are important to address in future research. Due to our electronic recruitment methods, we cannot be certain if the uncompleted surveys (26.8%) ever reached a potential respondent (e.g., out-of-date contact information listed in COG directory, email blocked by firewall or delivered to spam) or if potential respondents were not interested in sharing their program information. Most respondents completed the survey items sufficiently to characterize their healthcare transition practices and were included in these analyses, but some discontinued the survey early (n = 16) before transition questions were asked. Thus, these findings reflect the state of healthcare transition programming at the majority of, but not all, COG institutions. Additionally, neither information is unavailable to compare institutional characteristics of non-responding COG institutions to responding institutions, nor did this survey collect information from sites about the sociodemographics of the patient populations they serve (e.g., race/ethnicity, rural/urban, and insurance status), which may influence healthcare access and quality.
Future studies seeking to survey COG institutions may offer incentives to reimburse clinicians for their time responding to the survey, embed very brief surveys into the recruitment email, or streamline survey items in external data capture platforms using skip patterns to reduce respondent burden. For projects where surveying all COG institutions is not feasible, researchers may consider using purposeful sampling of institutions based on program characteristics (i.e., size, location and type of institution) to enhance generalizability. Researchers may also seek to include questions assessing the demographics of the populations served by institutions to identify potential social determinants of health impacting healthcare transition program delivery. Lastly, as these data were collected from institutions prior to the COVID-19 pandemic, future work may seek to understand if and how pandemic-related changes in survivorship care delivery [48] impacted healthcare transition services.
Conclusion
Although most COG institutions transfer adult-aged survivors of childhood cancer elsewhere for survivor care, very few programs deliver comprehensive programming to aid in successful healthcare transition. Successful healthcare transition can help promote increased early detection and treatment of late effects, leading to reduced morbidity and mortality among adult survivors of childhood cancer. To better serve survivors, novel research into best practices for survivor transition is needed, including transition readiness tools and mechanisms to obtain survivor feedback about the transition process. Developing successful strategies to support the implementation of healthcare transition programming in pediatric oncology and collaborations with primary care practices will be integral to advancing lifelong health after childhood cancer.
References
SEER. Cancer Statistics Review, 1975-2017 [Internet]: National Cancer Institute. Available from: https://seer.cancer.gov/csr/1975_2017/
Oeffinger KC, Mertens AC, Sklar CA, Kawashima T, Hudson MM, Meadows AT, Friedman DL, Marina N, Hobbie W, Kadan-Lottick NS, Schwartz CL, Leisenring W, Robison LL. Chronic health conditions in adult survivors of childhood cancer. N Engl J Med. 2006;355(15):1572–82. https://doi.org/10.1056/NEJMsa060185.
Hudson MM, Ness KK, Gurney JG, Mulrooney DA, Chemaitilly W, Krull KR, Green DM, Armstrong GT, Nottage KA, Jones KE, Sklar CA, Srivastava DK, Robison LL. Clinical ascertainment of health outcomes among adults treated for childhood cancer. JAMA. 2013;309(22):2371–81. https://doi.org/10.1001/jama.2013.6296.
Children’s Oncology Group. Long-term follow-up guidelines for survivors of childhood, adolescent and young adult cancers. Version 5.0. Monrovia, CA; 2018. Available online: http://www.survivorshipguidelines.org/.
Council IoMatNR. In: Hewitt M, Greenfield S, Stovall E, editors. From cancer patient to cancer survivor: lost in transition. Washington, DC: National Academies Press; 2006.
Mertens AC, Liu Q, Neglia JP, Wasilewski K, Leisenring W, Armstrong GT, Robison LL, Yasui Y. Cause-specific late mortality among 5-year survivors of childhood cancer: the Childhood Cancer Survivor study. J Natl Cancer Inst. 2008;100(19):1368–79. https://doi.org/10.1093/jnci/djn310.
Schwartz L, Tuchman L, Hobbie W, Ginsberg J. A social-ecological model of readiness for transition to adult-oriented care for adolescents and young adults with chronic health conditions. Child Care Health Dev. 2011;37(6):883–95. https://doi.org/10.1111/j.1365-2214.2011.01282.x.
Freyer DR. Transition of care for young adult survivors of childhood and adolescent cancer: rationale and approaches. J Clin Oncol. 2010;28(32):4810–8. https://doi.org/10.1200/JCO.2009.23.4278.
Oeffinger KC, Mertens AC, Hudson MM, Gurney JG, Casillas J, Chen H, Whitton J, Yeazel M, Yasui Y, Robison LL. Health care of young adult survivors of childhood cancer: a report from the Childhood Cancer Survivor study. Ann Fam Med. 2004;2(1):61–70. https://doi.org/10.1370/afm.26.
Ford JS, Tonorezos ES, Mertens AC, Hudson MM, Casillas J, Foster BM, Moskowitz CS, Smith SM, Chou JF, Buchanan G, Robison LL, Oeffinger KC. Barriers and facilitators of risk-based health care for adult survivors of childhood cancer: a report from the Childhood Cancer Survivor study. Cancer. 2020;126(3):619–27. https://doi.org/10.1002/cncr.32568.
Nathan PC, Greenberg ML, Ness KK, Hudson MM, Mertens AC, Mahoney MC, Gurney JG, Donaldson SS, Leisenring WM, Robison LL, Oeffinger KC. Medical care in long-term survivors of childhood cancer: a report from the Childhood Cancer Survivor study. J Clin Oncol. 2008;26(27):4401–9. https://doi.org/10.1200/JCO.2008.16.9607.
Sadak KT, Szalda D, Lindgren BR, Kinahan KE, Eshelman-Kent D, Schwartz LA, Henderson T, Freyer DR. Transitional care practices, services, and delivery in childhood cancer survivor programs: a survey study of U.S. survivorship providers. Pediatr Blood Cancer. 2019;66(8):e27793. https://doi.org/10.1002/pbc.27793.
Eshelman-Kent D, Kinahan K, Hobbie W, Landier W, Teal S, Friedman D, Nagarajan R, Freyer D. Cancer survivorship practices, services, and delivery: a report from the Children’s Oncology Group (COG) nursing discipline, adolescent/young adult, and late effects committees. J Cancer Surviv. 2011;5(4):345–57. https://doi.org/10.1007/s11764-011-0192-8.
Kenney LB, Melvin P, Fishman LN, O'Sullivan-Oliveira J, Sawicki GS, Ziniel S, Diller L, Fernandes SM. Transition and transfer of childhood cancer survivors to adult care: a national survey of pediatric oncologists. Pediatr Blood Cancer. 2017;64(2):346–52. https://doi.org/10.1002/pbc.26156.
TO H, Friedman DL, Meadows AT. Childhood cancer survivors: transition to adult-focused risk-based care. Pediatrics. 2010;126(1):129–36. https://doi.org/10.1542/peds.2009-2802.
Otth M, Denzler S, Koenig C, Koehler H, Scheinemann K. Transition from pediatric to adult follow-up care in childhood cancer survivors-a systematic review. J Cancer Surviv. 2021;15(1):151–62. https://doi.org/10.1007/s11764-020-00920-9.
Rosenberg-Yunger ZR, Klassen AF, Amin L, Granek L, D'Agostino NM, Boydell KM, Greenberg M, Barr RD, Nathan PC. Barriers and facilitators of transition from pediatric to adult long-term follow-up care in childhood cancer survivors. J Adolesc Young Adult Oncol. 2013;2(3):104–11. https://doi.org/10.1089/jayao.2013.0003.
Casillas J, Kahn KL, Doose M, Landier W, Bhatia S, Hernandez J, Zeltzer LK. Transitioning childhood cancer survivors to adult-centered healthcare: insights from parents, adolescent, and young adult survivors. Psycho-Oncology. 2010;19(9):982–90.
Nandakumar BS, Fardell JE, Wakefield CE, Signorelli C, McLoone JK, Skeen J, Maguire AM, Cohn RJ. Attitudes and experiences of childhood cancer survivors transitioning from pediatric care to adult care. Support Care Cancer. 2018;26(8):2743–50. https://doi.org/10.1007/s00520-018-4077-5.
White PH, Cooley WC. Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics. 2018;142(5). https://doi.org/10.1542/peds.2018-2587.
Cooley WC, Sagerman PJ. Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics. 2011;128(1):182–200. https://doi.org/10.1542/peds.2011-0969.
John AS, Jackson JL, Moons P, Uzark K, Mackie AS, Timmins S, Lopez KN, Kovacs AH, Gurvitz M. Advances in managing transition to adulthood for adolescents with congenital heart disease: a practical approach to transition program design: a scientific statement from the American Heart Association. J Am Heart Assoc. 2022;11(7):e025278. https://doi.org/10.1161/jaha.122.025278.
Medicine SfAHa. Transition to adulthood for youth with chronic conditions and special health care needs. J Adolesc Health. 2020;66(5):631–4. https://doi.org/10.1016/j.jadohealth.2020.02.006.
Bryant R, Porter JS, Sobota A. Association of Pediatric Hematology/Oncology N, American Society of Pediatri Hematology O. APHON/ASPHO policy statement for the transition of patients with sickle cell disease from pediatric to adult health care. J Pediatr Oncol Nurs. 2015;32(6):355–9. https://doi.org/10.1177/1043454215591954.
Rocque BG, Weprin BE, Blount JP, Hopson BD, Drake JM, Hamilton MG, Williams MA, White PH, Orrico KO, Martin JE. Health care transition in pediatric neurosurgery: a consensus statement from the American Society of Pediatric Neurosurgeons. J Neurosurg Pediatr. 2020;25:555–63. https://doi.org/10.3171/2019.12.Peds19524.
Gabriel P, McManus M, Rogers K, White P. Outcome evidence for structured pediatric to adult health care transition interventions: a systematic review. J Pediatr. 2017;188:263–9.e15. https://doi.org/10.1016/j.jpeds.2017.05.066.
Schmidt A, Ilango SM, McManus MA, Rogers KK, White PH. Outcomes of pediatric to adult health care transition interventions: an updated systematic review. J Pediatr Nurs. 2020;51:92–107. https://doi.org/10.1016/j.pedn.2020.01.002.
Effinger KE, Haardörfer R, Marchak JG, Escoffery C, Landier W, Kommajosula A, Hendershot E, Sadak KT, Eshelman-Kent D, Kinahan K, Freyer DR, Chow EJ, Mertens AC. Current pediatric cancer survivorship practices: a report from the Children’s Oncology Group. J Cancer Surviv. 2022:1–10. https://doi.org/10.1007/s11764-021-01157-w.
Iyer NS, Mitchell HR, Zheng DJ, Ross WL, Kadan-Lottick NS. Experiences with the survivorship care plan in primary care providers of childhood cancer survivors: a mixed methods approach. Support Care Cancer. 2017;25(5):1547–55. https://doi.org/10.1007/s00520-016-3544-0.
Suh E, Daugherty CK, Wroblewski K, Lee H, Kigin ML, Rasinski KA, Ford JS, Tonorezos ES, Nathan PC, Oeffinger KC, TO H. General internists’ preferences and knowledge about the care of adult survivors of childhood cancer: a cross-sectional survey. Ann Intern Med. 2014;160(1):11–7. https://doi.org/10.7326/m13-1941.
Signorelli C, Wakefield CE, Fardell JE, Foreman T, Johnston KA, Emery J, Thornton-Benko E, Girgis A, Lie HC, Cohn RJ. The role of primary care physicians in childhood cancer survivorship care: multiperspective interviews. Oncologist. 2018. https://doi.org/10.1634/theoncologist.2018-0103.
Hudson MM, Bhatia S, Casillas J, Landier W. Long-term follow-up care for childhood, adolescent, and young adult cancer survivors. Pediatrics. 2021;148(3). https://doi.org/10.1542/peds.2021-053127.
White P, Schmidt A, Ilango S, Shorr J, Beck D, McManus M. Six core elements of Health Care Transition™ 3.0: an implementation guide. Washington, DC: Got Transition, The National Alliance to Advance Adolescent Health; 2020.
Schwartz LA, Daniel LC, Brumley LD, Barakat LP, Wesley KM, Tuchman LK. Measures of readiness to transition to adult health care for youth with chronic physical health conditions: a systematic review and recommendations for measurement testing and development. J Pediatr Psychol. 2014. https://doi.org/10.1093/jpepsy/jsu028.
South K, George M, Smaldone A. Gaps in transition readiness measurement: a comparison of instruments to a conceptual model. J Transit Med. 2022;4(1):20220002. https://doi.org/10.1515/jtm-2022-0002.
Sawicki GS, Lukens-Bull K, Yin X, Demars N, Huang I. Measuring the transition readiness of youth with special healthcare needs: validation of the TRAQ--Transition Readiness Assessment Questionnaire. J Pediatr Psychol. 2009. Epub December 29, 2009. https://doi.org/10.1093/jpepsy/jsp128.
Wood DL, Sawicki GS, Miller MD, Smotherman C, Lukens-Bull K, Livingood WC, Ferris M, Kraemer DF. The Transition Readiness Assessment Questionnaire (TRAQ): its factor structure, reliability, and validity. Acad Pediatr. 2014;14(4):415–22. https://doi.org/10.1016/j.acap.2014.03.008.
Ferris ME, Harward DH, Bickford K, Layton JB, Ferris MT, Hogan SL, Gipson DS, McCoy LP, Hooper SR. A clinical tool to measure the components of health-care transition from pediatric care to adult care: the UNC TR(x)ANSITION scale. Ren Fail. 2012;34(6):744–53. https://doi.org/10.3109/0886022x.2012.678171.
Ferris M, Cohen S, Haberman C, Javalkar K, Massengill S, Mahan JD, Kim S, Bickford K, Cantu G, Medeiros M, Phillips A, Ferris MT, Hooper SR. Self-management and transition readiness assessment: development, reliability, and factor structure of the STARx Questionnaire. J Pediatr Nurs. 2015;30(5):691–9. https://doi.org/10.1016/j.pedn.2015.05.009.
Marchak JG, Reed-Knight B, Amaral S, Mee L, Blount RL. Providers’ assessment of transition readiness among adolescent and young adult kidney transplant recipients. Pediatr Transplant. 2015;19(8):849–57. https://doi.org/10.1111/petr.12615.
Gilleland J, Amaral S, Mee L, Blount R. Getting ready to leave: transition readiness in adolescent kidney transplant recipients. J Pediatr Psychol. 2012;37(1):85–96. https://doi.org/10.1093/jpepsy/jsr049.
Haarbauer-Krupa J, Alexander NM, Mee L, Johnson A, Wise J, Gupta NA, Schechter MS, Wasilewski-Masker K, Marchak JG. Readiness for transition and healthcare satisfaction in adolescents with complex medical conditions. Child Care Health Dev. 2019. https://doi.org/10.1111/cch.12656.
Klassen AF, Grant C, Barr R, Brill H, Kraus de Camargo O, Ronen GM, Samaan MC, Mondal T, Cano SJ, Schlatman A, Tsangaris E, Athale U, Wickert N, Gorter JW. Development and validation of a generic scale for use in transition programmes to measure self-management skills in adolescents with chronic health conditions: the TRANSITION-Q. Child Care Health Dev. 2015;41(4):547–58. https://doi.org/10.1111/cch.12207.
Betz CL. California healthy and ready to work transition health care guide: developmental guidelines for teaching health care self-care skills to children. Issues Compr Pediatr Nurs. 2000;23(4):203–44. https://doi.org/10.1080/014608600300029867.
Betz CL, Redcay G, Tan S. Self-reported health care self-care needs of transition-age youth: a pilot study. Issues Compr Pediatr Nurs. 2003;26(3):159–81. https://doi.org/10.1080/01460860390223880.
Klassen AF, Rosenberg-Yunger ZR, D'Agostino NM, Cano SJ, Barr R, Syed I, Granek L, Greenberg ML, Dix D, Nathan PC. The development of scales to measure childhood cancer survivors’ readiness for transition to long-term follow-up care as adults. Health Expect. 2015;18(6):1941–55. https://doi.org/10.1111/hex.12241.
Lee JL, Gutierrez-Colina A, Williamson Lewis R, Wasilewski-Masker K, Meacham LR, Mertens AC, Gilleland MJ. Knowledge of late effects risks and healthcare responsibility in adolescents and young adults treated for childhood cancer. J Pediatr Psychol. 2019;44(5):557–66. https://doi.org/10.1093/jpepsy/jsy102.
van den Oever SR, SMF P, Skinner R, Glaser A, Mulder RL, Armenian S, Bardi E, Berger C, Ehrhardt MJ, Gilleland Marchak J, Haeusler GM, Hartogh JD, Hjorth L, Kepak T, Kriviene I, Langer T, Maeda M, Márquez-Vega C, Michel G, et al. Childhood cancer survivorship care during the COVID-19 pandemic: an international report of practice implications and provider concerns. J Cancer Surviv. 2022;16(6):1390–400. https://doi.org/10.1007/s11764-021-01120-9.
Funding
Research reported in this publication was supported by the Children’s Oncology Group Outcomes and Survivorship, Adolescent and Young Adult, and Nursing Committees, the National Cancer Institute under Award Numbers R01CA218389, U10CA180886, and UG1CA189955, and the Intervention Development, Dissemination, and Implementation Developing shared resource of Winship Cancer Institute of Emory University and NIH/NCI under award number P30CA138292.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflict of interest
The author declares that there are no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Marchak, J.G., Sadak, K.T., Effinger, K.E. et al. Transition practices for survivors of childhood cancer: a report from the Children’s Oncology Group. J Cancer Surviv 17, 342–350 (2023). https://doi.org/10.1007/s11764-023-01351-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-023-01351-y