Abstract
Purpose
Gynecologic cancer survivors often hesitate to raise sexual health concerns with their clinicians. We pilot tested Starting the Conversation (STC), a theory-guided intervention aimed at facilitating survivors’ clinical communication about sexual health.
Methods
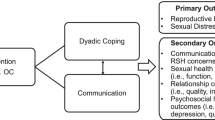
Survivors (N = 32) were randomized 2:1 to STC (23-min video and accompanying workbook grounded in social cognitive theory that provides information and skills training for communicating with providers about sexual concerns, and resource guide) or control (resource guide only). Feasibility was assessed through enrollment, retention, and intervention completion rates (benchmarks: 60%, 80%, 70%); acceptability was assessed through post-intervention program evaluations (benchmark: 75%). Preliminary effects were assessed for sexual health communication (self-reported after next clinic encounter), self-efficacy for clinical communication about sexual health (post-intervention and 2-month follow-up), and sexual activity and anxiety/depressive symptoms (2-month follow-up).
Results
All feasibility/acceptability benchmarks were surpassed; 76% enrolled, 97% retained, ≥ 95% used intervention materials, and 100% endorsed STC as acceptable. Positive STC effects were seen for increases in self-efficacy (Cohen’s d’s = 0.45 at post-intervention; 0.55 at follow-up). In STC, 35% and 45% of women raised or asked about sexual health concerns during the post-intervention clinic visit, respectively, versus 0 and 27% in the control arm. Other measures showed little change.
Conclusions
Data support the STC intervention as feasible and acceptable, with promising effects for gynecologic cancer survivors’ communication about sexual health concerns. Because sexual health communication is relevant across the treatment trajectory, we included both on-treatment and post-treatment survivors. While this may be a limitation, it could also enhance sample generalizability. A larger trial is needed to determine efficacy.
Implications for Cancer Survivors
Communication about sexual health is important yet lacking for cancer survivors. Patient-focused interventions may help address concerns and improve survivors’ health outcomes.

Similar content being viewed by others
Data availability
Reasonable requests for datasets generated during and/or analyzed during the current study will be considered by the corresponding author.
Notes
Age data was missing from one clinician.
We intended to assess preliminary effects on women’s sexual function using the Female Sexual Function Index (FSFI) [37]. However, preliminary analysis revealed a sizeable number of participants (N = 17; 53%) whose responses on the FSFI indicated they were not sexually active. Because the FSFI has been shown to be problematic in sexually inactive women [38], the responses were to be excluded from analyses. With such a large proportion of participants’ data to be excluded, the interpretation of findings would be highly problematic and thus, it was deemed inappropriate to conduct analyses with the FSFI.
References
Carter J, Stabile C, Gunn A, Sonoda Y. The physical consequences of gynecologic cancer surgery and their impact on sexual, emotional, and quality of life issues. J Sex Med. 2013;10(Suppl 1):21–34.
Hopkins TG, Stavraka C, Gabra H, Fallowfield L, Hood C, Blagden S. Sexual activity and functioning in ovarian cancer survivors: an internet-based evaluation. Climacteric. 2015;18:94–8.
Abbott-Anderson K, Kwekkeboom KL. A systematic review of sexual concerns reported by gynecological cancer survivors. Gynecol Oncol. 2012;124:477–89.
Lara LA, de Andrade JM, Consolo FD, Romão AP. Women’s poorer satisfaction with their sex lives following gynecologic cancer treatment. Clin J Oncol Nurs. 2012;16:273–7.
Levin AO, Carpenter KM, Fowler JM, Brothers BM, Andersen BL, Maxwell GL. Sexual morbidity associated with poorer psychological adjustment among gynecological cancer survivors. Int J Gynecol Cancer. 2010;20:461–70.
Flay LD, Matthews JH. The effects of radiotherapy and surgery on the sexual function of women treated for cervical cancer. Int J Radiat Oncol Biol Phys. 1995;31:399–404.
Jensen PT, Froeding LP. Pelvic radiotherapy and sexual function in women. Transl Androl Urol. 2015;4:186–205.
Lin H, Fu H-C, Wu C-H, Tsai Y-J, Chou Y-J, Shih C-M, et al. Evaluation of sexual dysfunction in gynecologic cancer survivors using DSM-5 diagnostic criteria. BMC Womens Health. 2022;22:1.
Gilbert E, Ussher JM, Perz J. Sexuality after gynaecological cancer: a review of the material, intrapsychic, and discursive aspects of treatment on women’s sexual-wellbeing. Maturitas. 2011;70:42–57.
Harris MG. Sexuality and menopause: unique issues in gynecologic cancer. Semin Oncol Nurs. 2019;35:211–6.
Lammerink EA, de Bock GH, Pras E, Reyners AK, Mourits MJ. Sexual functioning of cervical cancer survivors: a review with a female perspective. Maturitas. 2012;72:296–304.
Sekse RJT, Hufthammer KO, Vika ME. Sexual activity and functioning in women treated for gynaecological cancers. J Clin Nurs. 2017;26:400–10.
Lindau ST, Gavrilova N, Anderson D. Sexual morbidity in very long term survivors of vaginal and cervical cancer: a comparison to national norms. Gynecol Oncol. 2007;106:413–8.
Carter J, Lacchetti C, Andersen BL, Barton DL, Bolte S, Damast S, et al. Interventions to address sexual problems in people with cancer: American Society of Clinical Oncology Clinical Practice Guideline Adaptation of Cancer Care Ontario Guideline. J Clin Oncol. 2017;36:492–511.
Denlinger CS, Sanft T, Baker KS, Broderick G, Demark-Wahnefried W, Friedman DL, et al. Survivorship, Version 2.2018, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2018;16:1216–47.
Chapman CH, Heath G, Fairchild P, Berger MB, Wittmann D, Uppal S, et al. Gynecologic radiation oncology patients report unmet needs regarding sexual health communication with providers. J Cancer Res Clin Oncol. 2019;145:495–502.
Flynn KE, Reese JB, Jeffery DD, Abernethy AP, Lin L, Shelby RA, et al. Patient experiences with communication about sex during and after treatment for cancer. Psychooncology. 2012;21:594–601.
Stafford L, Russell H, Knoetze E, Wilson V, Little R. Sexual functioning after ovarian cancer: are women receiving the information and support they need? Support Care Cancer. 2022;30:4583–6.
Vermeer WM, Bakker RM, Kenter GG, de Kroon CD, Stiggelbout AM, ter Kuile MM. Sexual issues among cervical cancer survivors: how can we help women seek help? Psychooncology. 2015;25:458–64.
Stabile C, Goldfarb S, Baser RE, Goldfrank DJ, Abu-Rustum NR, Barakat RR, et al. Sexual health needs and educational intervention preferences for women with cancer. Breast Cancer Res Treat. 2017;165:77–84.
Hay CM, Donovan HS, Hartnett EG, Carter J, Roberge MC, Campbell GB, et al. Sexual health as part of gynecologic cancer care: what do patients want? Int J Gynecol Cancer. 2018;28:1737–42.
McCallum M, Lefebvre M, Jolicoeur L, Maheu C, Lebel S. Sexual health and gynecological cancer: conceptualizing patient needs and overcoming barriers to seeking and accessing services. J Psychosom Obstet Gynecol. 2012;33:135–42.
Bandura A. Social foundations of thought and action: a social cognitive theory. Englewood Cliffs: Prentice Hall, Inc.; 1986.
Reese JB, Sorice KA, Pollard W, Handorf E, Beach MC, Daly MB et al. Efficacy of a multimedia intervention in facilitating breast cancer patients’ clinical communication about sexual health: results of a randomized controlled trial. Psychooncology. 2020;30.
Dai Y, Cook OY, Yeganeh L, Huang C, Ding J, Johnson CE. Patient-reported barriers and facilitators to seeking and accessing support in gynecologic and breast cancer survivors with sexual problems: a systematic review of qualitative and quantitative studies. J Sex Med. 2020;17:1326–58.
Beaver K, Booth K. Information needs and decision-making preferences: comparing findings for gynaecological, breast and colorectal cancer. Eur J Oncol Nurs. 2007;11:409–16.
Aerts L, Enzlin P, Verhaeghe J, Vergote I, Amant F. Sexual and psychological functioning in women after pelvic surgery for gynaecological cancer. Eur J Gynaecol Oncol. 2009;30:652–6.
Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982;5:649–55.
Reese JB, Beach MC, Smith KC, Bantug ET, Casale KE, Porter LS, et al. Effective patient-provider communication about sexual concerns in breast cancer: a qualitative study. Support Care Cancer. 2017;25:3199–207.
Brandes K, Linn AJ, Butow PN, Weert JCM. The characteristics and effectiveness of Question Prompt List interventions in oncology: a systematic review of the literature. Psychooncology. 2015;24:245–52.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap) – a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–81.
Bandura A. Guide for constructing self-efficacy scales. In: Pajares F, Urdan T, editors. Self-Efficacy Beliefs of Adolescents. Greenwich: IAP-Information Age Publishing Inc.; 2006. p. 307–38.
Reese JB, Lepore SJ, Daly MB, Handorf E, Sorice KA, Porter LS, et al. A brief intervention to enhance breast cancer clinicians’ communication about sexual health: feasibility, acceptability, and preliminary outcomes. Psychooncology. 2019;28:872–9.
Reese JB, Sorice KA, Pollard W, Zimmaro LA, Beach MC, Handorf E, et al. Understanding sexual help-seeking for women with breast cancer: what distinguishes women who seek help from those who do not? J Sex Med. 2020;17:1729–39.
Reese JB, Sorice K, Lepore SJ, Daly MB, Tulsky JA, Beach MC. Patient-clinician communication about sexual health in breast cancer: a mixed-methods analysis of clinic dialogue. Patient Educ Couns. 2019;102:436–42.
Weinfurt KP, Lin L, Bruner DW, Cyranowski JM, Dombeck CB, Hahn EA, et al. Development and initial validation of the PROMIS® sexual function and satisfaction measures version 2.0. J Sex Med. 2015;12:1961–74.
Ljungman L, Ahlgren J, Petersson L-M, Flynn KE, Weinfurt K, Gorman JR, et al. Sexual dysfunction and reproductive concerns in young women with breast cancer: type, prevalence, and predictors of problems. Psychooncology. 2018;27:2770–7.
Zigmond A, Snaith R. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–70.
Reese JB, Zimmaro LA, Bober SL, Sorice K, Handorf E, Wittenberg E et al. Mobile technology-based (mLearning) intervention to enhance breast cancer clinicians’ communication about sexual health: a pilot trial. J Natl Compr Canc Netw. 2021. https://doi.org/10.6004/jnccn.2021.7032.
Eldridge SM, Lancaster GA, Campbell MJ, Thabane L, Hopewell S, Coleman CL, et al. Defining feasibility and pilot studies in preparation for randomised controlled trials: development of a conceptual framework. PLoS One. 2016;11:e0150205.
Eldridge SM, Chan CL, Campbell MJ, Bond CM, Hopewell S, Thabane L, et al. CONSORT 2010 statement: extension to randomised pilot and feasibility trials. BMJ. 2016;355:i5239.
Reese JB, Smith KC, Handorf E, Sorice K, Bober SL, Bantug ET, et al. A randomized pilot trial of a couple-based telephone intervention addressing sexual concerns for breast cancer survivors. J Psychosoc Oncol. 2019;37:242–63.
Del Re AC. compute.es: compute effect sizes. R package version 0.2–2. 2013.
Bornstein M. Effect sizes for continuous data. In: Cooper H, Hedges LV, Valentine JC, editors. The handbook of research synthesis and meta analysis. New York: Russel Sage Foundation; 2009. p. 279–93.
Cohen J. A power primer. Psychol Bull. 1992;112:155–9.
Schover LR, Strollo S, Stein K, Fallon E, Smith T. Effectiveness trial of an online self-help intervention for sexual problems after cancer. J Sex Marital Ther. 2020;46:576–88. https://doi.org/10.6004/jnccn.2021.7032.
Scanlon M, Blaes A, Geller M, Majhail NS, Lindgren B, Haddad T. Patient satisfaction with physician discussions of treatment impact on fertility, menopause and sexual health among pre-menopausal women with cancer. J Cancer. 2012;3:217–25.
Flynn KE, Lin L, Cyranowski JM, Reeve BB, Reese JB, Jeffery DD, et al. Development of the NIH PROMIS® sexual function and satisfaction measures in patients with cancer. J Sex Med. 2013;10:43–52.
Funding
This study was supported by P30CA006927 from the National Cancer Institute of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
JBR, SLB, EH, CSC, and AE-J contributed to the study conception and design. Data collection was performed by KAS, DM, and SM. Data preparation/analysis were performed by JBR, KAS, and EH. The first draft was written by JBR and all authors reviewed and contributed to the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the Fox Chase Institutional Review Board (IRB Protocol #21–1066). Informed consent was obtained from all participants.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Reese, J.B., Bober, S.L., Sorice, K.A. et al. Starting the Conversation: randomized pilot trial of an intervention to promote effective clinical communication about sexual health for gynecologic cancer survivors. J Cancer Surviv 18, 800–809 (2024). https://doi.org/10.1007/s11764-022-01327-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-022-01327-4