Abstract
Background
The prospective surveillance model (PSM) is an evidence-based rehabilitation care delivery model that facilitates functional screening and intervention for individuals undergoing cancer treatment. While PSM is empirically validated and feasible in practice, implementation into cancer care delivery has languished. The purpose of this manuscript is to characterize the barriers and facilitators to implementing PSM in a breast cancer center and to share policy and process outcomes that have sustained the model in practice.
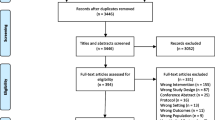
Methods
The PSM implementation was undertaken as a quality improvement initiative of our cancer center. We retrospectively assessed barriers to implementation and define those according to the Consolidated Framework for Implementation Research (CFIR). Implementation strategies are defined based on the Expert Recommendations for Implementation Change (ERIC) taxonomy. Breast center policy changes and stakeholder-reported process improvement outcomes at the clinic and system level are described.
Results
PSM implementation facilitation was driven primarily by adapting the model to align with the cancer center workflow, engaging interdisciplinary stakeholders as program champions, enhancing knowledge and awareness among cancer care providers, and changing infrastructure to support the model. System and clinic-level policy and process changes included the development of clinical pathways, EHR order sets and automated referrals, new staffing models, and adapted clinical workflows.
Conclusion
Our report provides insight on implementing the PSM at a single institution in a cancer care delivery setting. Successful implementation strategies addressed individual, clinic, and system-level barriers and facilitated process and policy changes that have enabled PSM sustainment. Improving integration of rehabilitation services into oncology care has significant implications for survivorship care by enhancing proactive management of functional morbidity.
Implications for Cancer Survivors
Improving integration of rehabilitation services into oncology care has significant implications for survivorship care by enhancing proactive management of functional morbidity.
Similar content being viewed by others
References
Cheville AL, McLaughlin SA, Haddad TC, Lyons KD, Newman R, Ruddy KJ. Integrated rehabilitation for breast cancer survivors. Am J Phys Med Rehabil. 2019;98(2):154–64. https://doi.org/10.1097/PHM.0000000000001017.
Runowicz CD, Leach CR, Henry NL, et al. American Cancer Society/American Society of Clinical Oncology breast cancer survivorship care guideline. Cancer J Clin. 2016;66(1):43–73. https://doi.org/10.3322/caac.21319.
Springer BA, Levy E, McGarvey C, et al. Pre-operative assessment enables early diagnosis and recovery of shoulder function in patients with breast cancer. Breast Cancer Res Treat. 2010;120(1):135–47. https://doi.org/10.1007/s10549-009-0710-9.
Stout Gergich NL, Pfalzer LA, McGarvey C, Springer B, Gerber LH, Soballe P. Preoperative assessment enables the early diagnosis and successful treatment of lymphedema. Cancer. 2008;112(12):2809–19. https://doi.org/10.1002/cncr.23494.
Levy EW, Pfalzer LA, Danoff J, et al. Predictors of functional shoulder recovery at 1 and 12 months after breast cancer surgery. Breast Cancer Res Treat. 2012;134(1):315–24. https://doi.org/10.1007/s10549-012-2061-1.
Santa Mina D, Brahmbhatt P, Lopez C, et al. The case for prehabilitation prior to breast cancer treatment. PM R. 2017;9(9S2):S305-R316. https://doi.org/10.1016/j.pmrj.2017.08.402.
Lai L, Binkley J, Jones V, et al. Implementing the prospective surveillance model (PSM) of rehabilitation for breast cancer patients with 1-year postoperative follow-up, a prospective, observational study. Ann Surg Oncol. 2016;23(10):3379–84. https://doi.org/10.1245/s10434-016-5315-z.
Rafn BS, Hung S, Hoens AM, et al. Prospective surveillance and targeted physiotherapy for arm morbidity after breast cancer surgery: a pilot randomized controlled trial. Clin Rehabil. 2018;32(6):811–26. https://doi.org/10.1177/0269215518757292.
Koelmeyer LA, Borotkanics RJ, Alcorso J, et al. Early surveillance is associated with less incidence and severity of breast cancer-related lymphedema compared with a traditional referral model of care. Cancer. 2019;125(6):854–62. https://doi.org/10.1002/cncr.31873.
Stout NL, Binkley JM, Schmitz KH, et al. A prospective surveillance model for rehabilitation for women with breast cancer. Cancer. 2012;118(8 Suppl):2191–200. https://doi.org/10.1002/cncr.27476.
Barnes CA, Stout NL, Varghese TK Jr, et al. Clinically integrated physical therapist practice in cancer care: a new comprehensive approach. Phys Ther. 2020;100(3):543–53. https://doi.org/10.1093/ptj/pzz169.
Stout NL, Brunelle C, Scheiman N, Thawer H. Surveillance protocols for survivors at risk for lymphedema. Curr Breast Cancer Rep 2021;13(1):19–27. https://doi.org/10.1007/s12609-020-00402-y.
Yang EJ, Ahn S, Kim E-K, et al. Use of a prospective surveillance model to prevent breast cancer treatment-related lymphedema: a single-center experience. Breast Cancer Res Treat. 2016;160(2):269–76.
Leach HJ, Covington KR, Pergolotti M, et al. Translating research to practice using a team-based approach to cancer rehabilitation: a physical therapy and exercise-based cancer rehabilitation program reduces fatigue and improves aerobic capacity. Rehabil Oncol 2018;36(4):206–213.
Alfano CM, Kent EE, Padgett LS, Grimes M, de Moor JS. Making cancer rehabilitation services work for cancer patients: recommendations for research and practice to improve employment outcomes. PM R. 2017;9(9S2):S398–406. https://doi.org/10.1016/j.pmrj.2017.06.019.
Brown CH, Curran G, Palinkas LA, et al. An overview of research and evaluation designs for dissemination and implementation. Annu Rev Public Health. 2017;38:1–22.
Mitchell SA, Chambers DA. Leveraging implementation science to improve cancer care delivery and patient outcomes. J Oncol Pract. 2017;13(8):523.
Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4:50. https://doi.org/10.1186/1748-5908-4-50.
Proctor EK, Powell BJ, McMillen JC. Implementation strategies: recommendations for specifying and reporting. Implement Sci. 2013;8:139. https://doi.org/10.1186/1748-5908-8-139.
Ahmed S. Integrating DMAIC approach of Lean Six Sigma and theory of constraints toward quality improvement in healthcare. Rev Environ Health. 2019;34(4):427–34.
Waltz TJ, Powell BJ, Matthieu MM, et al. Use of concept mapping to characterize relationships among implementation strategies and assess their feasibility and importance: results from the Expert Recommendations for Implementing Change (ERIC) study. Implement Sci. 2015;10(1):109.
Swisher AK, Mia Erickson P, Cht A. Frequency and severity of self-reported upper extremity impairments, activity limitations, and participation restrictions following breast cancer treatment. Rehabil Oncol. 2010;28(1):3.
Hayes SC, Johansson K, Stout NL, et al. Upper-body morbidity after breast cancer: incidence and evidence for evaluation, prevention, and management within a prospective surveillance model of care. Cancer. 2012;118(8 Suppl):2237–49. https://doi.org/10.1002/cncr.27467.
Schmitz KH, Speck RM, Rye SA, DiSipio T, Hayes SC. Prevalence of breast cancer treatment sequelae over 6 years of follow-up: the Pulling Through Study. Cancer. 2012;118(8 Suppl):2217–25. https://doi.org/10.1002/cncr.27474.
Stout NL, Santa Mina D, Lyons KD, Robb K, Silver JK. A systematic review of rehabilitation and exercise recommendations in oncology guidelines. CA Cancer J Clin. 2021;71(2):149–175. https://doi.org/10.3322/caac.21639.
American College of Surgeons Commission on Cancer. Cancer program standards 2020: optimal resources for cancer care. 2020. Accessed May 1, 2022. https://www.facs.org/-/media/files/quality-programs/cancer/coc/optimal_resources_for_cancer_care_2020_standards.ashx.
American College of Surgeons, National Accreditation Program for Breast Centers. Standards manual 2018. National Accreditation Program for Breast Centers. Accessed May 1, 2022. https://www.facs.org/quality-programs/cancer-programs/national-accreditation-program-for-breast-centers/standards-and-resources/.
Alfano CM, Cheville AL, Mustian K. Developing high-quality cancer rehabilitation programs: a timely need. Am Soc Clin Oncol Educ Book. 2016;35:241–9. https://doi.org/10.1200/EDBK_156164.
Stout NL, Silver JK, Raj VS, et al. Toward a national initiative in cancer rehabilitation: recommendations from a subject matter expert group. Arch Phys Med Rehabil. 2016;97(11):2006–15. https://doi.org/10.1016/j.apmr.2016.05.002.
National Academies of Sciences, Engineering, and Medicine. Long-term survivorship care after cancer treatment: Proceedings of a workshop. National Academies Press, 2018. Accessed May 2022. https://nap.nationalacademies.org/catalog/25043/long-term-survivorship-care-after-cancer-treatment-proceedings-of-a
Schmitz KH, Stout NL, Andrews K, Binkley JM, Smith RA. Prospective evaluation of physical rehabilitation needs in breast cancer survivors: a call to action. Cancer. 2012;118(8 Suppl):2187–90. https://doi.org/10.1002/cncr.27471.
Neo J, Fettes L, Gao W, Higginson IJ, Maddocks M. Disability in activities of daily living among adults with cancer: a systematic review and meta-analysis. Cancer Treat Rev. 2017;61:94–106. https://doi.org/10.1016/j.ctrv.2017.10.006.
Cheville AL, Beck LA, Petersen TL, Marks RS, Gamble GL. The detection and treatment of cancer-related functional problems in an outpatient setting. Support Care Cancer. 2009;17(1):61–7. https://doi.org/10.1007/s00520-008-0461-x.
Pergolotti M, Deal AM, Lavery J, Reeve BB, Muss HB. The prevalence of potentially modifiable functional deficits and the subsequent use of occupational and physical therapy by older adults with cancer. Journal of geriatric oncology. 2015;6(3):194–201.
McNeely ML, Binkley JM, Pusic AL, Campbell KL, Gabram S, Soballe PW. A prospective model of care for breast cancer rehabilitation: postoperative and postreconstructive issues. Cancer. 2012;118(8 Suppl):2226–36. https://doi.org/10.1002/cncr.27468.
Greenlee H, DuPont-Reyes MJ, Balneaves LG, et al. Clinical practice guidelines on the evidence-based use of integrative therapies during and after breast cancer treatment. CA: Cancer J Clin. 2017;67(3):194–232. https://doi.org/10.3322/caac.21397.
Senkus E, Kyriakides S, Ohno S, et al. Primary breast cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2015;26(suppl 5):v8-30. https://doi.org/10.1093/annonc/mdv298.
Goetz MP, Gradishar WJ, Anderson BO, et al. Breast cancer, version 3.2018: featured updates to the NCCN guidelines. J Natl Compr Cancer Netw. 2019;17(2):118–26.
Stubblefield MD. Radiation fibrosis syndrome: neuromuscular and musculoskeletal complications in cancer survivors. PM R. 2011;3(11):1041–54. https://doi.org/10.1016/j.pmrj.2011.08.535.
Moullin JC, Dickson KS, Stadnick NA, Rabin B, Aarons GA. Systematic review of the Exploration, Preparation, Implementation, Sustainment (EPIS) framework. Implement Sci. 2019;14(1):1. https://doi.org/10.1186/s13012-018-0842-6.
Shelton RC, Cooper BR, Stirman SW. The sustainability of evidence-based interventions and practices in public health and health care. Annu Rev Public Health. 2018;39(1):55–76. https://doi.org/10.1146/annurev-publhealth-040617-014731.
Baumann AA, Cabassa LJ, Stirman SW. Adaptation in dissemination and implementation science. Dissemination Implement Res Health: Translating Sci Pract. 2017;2:286–300.
Li S-A, Jeffs L, Barwick M, Stevens B. Organizational contextual features that influence the implementation of evidence-based practices across healthcare settings: a systematic integrative review. Syst Rev. 2018;7(1):72. https://doi.org/10.1186/s13643-018-0734-5.
Miech EJ, Rattray NA, Flanagan ME, Damschroder L, Schmid AA, Damush TM. Inside help: an integrative review of champions in healthcare-related implementation. SAGE Open Med. 2018;6:2050312118773261.
Bowen SJ, Graham ID. From knowledge translation to engaged scholarship: promoting research relevance and utilization. Arch Phys Med Rehabil. 2013;94(1):S3–8.
Powell BJ, Waltz TJ, Chinman MJ, et al. A refined compilation of implementation strategies: results from the Expert Recommendations for Implementing Change (ERIC) project. Implement Sci. 2015;10(1):21.
Meyers DC, Durlak JA, Wandersman A. The quality implementation framework: a synthesis of critical steps in the implementation process. Am J Community Psychol. 2012;50(3):462–80.
Fernandez ME, Ten Hoor GA, Van Lieshout S, et al. Implementation mapping: using intervention mapping to develop implementation strategies. Front Public Health. 2019;7:158.
Nilsen P, Bernhardsson S. Context matters in implementation science: a scoping review of determinant frameworks that describe contextual determinants for implementation outcomes. BMC Health Serv Res. 2019;19(1):1–21.
Author information
Authors and Affiliations
Contributions
Concept and design: AS, NS, RU. Acquisition, analysis, or interpretation of data: NS, RU, AS, MB, HHJ. Drafting of the manuscript: NS, AS, RU. Critical revision of the manuscript: NS, RU, AS, MB, HHJ. Statistical analysis: N/A. Obtained funding: N/A. Administrative, technical, or material support: NS, RU, AS, MB, HHJ. Supervision: N/A.
Corresponding author
Ethics declarations
Conflict of interest
NS: consultant/speakers bureau: MedBridge Inc., Survivorship Solutions LLC. RU: none. HHJ: none. MB: none. AS: none.
Data availability
This narrative review did not collect a data set for this report.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Stout, N.L., Utzman, R., Jenkins, H.H. et al. Implementing and sustaining a breast cancer prospective surveillance rehabilitation program: an institutional perspective. J Cancer Surviv 17, 509–517 (2023). https://doi.org/10.1007/s11764-022-01304-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-022-01304-x