Abstract
Purpose
Despite extensive research on cancer and work-related outcomes, evidence from longitudinal cohort studies is limited, especially in young women with breast cancer (BC). We aimed to investigate employment trajectories in young BC survivors and to identify potential factors associated with changes in work activity.
Methods
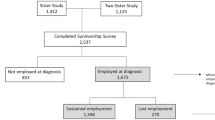
The HOHO European prospective multicenter cohort study enrolled 300 young women (≤ 40 years) with newly diagnosed BC. Women completed surveys at baseline and every 6 months for 3 years, then yearly for up to 10 years to assess, among other variables, employment status, sociodemographic, medical, and treatment data. Symptoms were assessed by the Breast Cancer Prevention Trial symptom scales and single items from the Cancer Rehabilitation Evaluation System. Univariable and multivariable multinomial logistic regression analyses identified factors associated with changes in employment status.
Results
Among the 245 women included in this analysis, 85% were employed at the last individual post-baseline assessment (1 to 10 years). At 5 years, women had a 29.4% probability (95% CI: 23.6–35.5) of experiencing any reduction and a 14.9% probability (95% CI: 10.6–19.9) of experiencing any increase in work activities. Being enrolled in Switzerland (vs. Italy) and reporting more trouble in performing daily activities were significantly associated with work reduction.
Conclusion
Our results suggest that most young BC survivors remain employed in the long-term.
Implications for Cancer Survivors
Regular evaluation of symptoms which may interfere with daily life and identification of financial discomfort is critical in providing timely and individually tailored interventions and in limiting unwanted reductions in work activities.


Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Allemani C, et al. Global surveillance of trends in cancer survival 2000–14 (CONCORD-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet. 2018;391(10125):1023–75.
Sun Y, Shigaki CL, Armer JM. Return to work among breast cancer survivors: a literature review. Support Care Cancer. 2017;25(3):709–18.
van Maarschalkerweerd PEA, et al. Changes in employment status, barriers to, and facilitators of (return to) work in breast cancer survivors 5–10 years after diagnosis. Disabil Rehabil. 2020;42(21):3052–8.
Paalman CH, et al. Employment and social benefits up to 10 years after breast cancer diagnosis: a population-based study. Br J Cancer. 2016;114(1):81–7.
Wang L, et al. Predictors of unemployment after breast cancer surgery: a systematic review and meta-analysis of observational studies. J Clin Oncol. 2018;36(18):1868–79.
Vayr F, et al. Work adjustments and employment among breast cancer survivors: a French prospective study. Support Care Cancer. 2020;28(1):185–92.
Park, J. and S. Mamdouh, Returning to work after breast cancer: a critical review. International J Disabil Manag, 2013(8, e1): p. 1–10.
Islam T, et al. Factors associated with return to work of breast cancer survivors: a systematic review. BMC Public Health. 2014;14(Suppl 3):S8.
Schmidt ME, et al. Return to work after breast cancer: the role of treatment-related side effects and potential impact on quality of life. Eur J Cancer Care (Engl). 2019;28(4):e13051.
Dumas A, et al. Impact of breast cancer treatment on employment: results of a multicenter prospective cohort study (CANTO). J Clin Oncol. 2020;38(7):734–43.
Carlsen K, et al. Self-reported work ability in long-term breast cancer survivors. A population-based questionnaire study in Denmark. Acta Oncol. 2013;52(2):423–9.
Gregorowitsch ML, et al. Self-reported work ability in breast cancer survivors; a prospective cohort study in the Netherlands. Breast. 2019;48:45–53.
Zomkowski K, et al. Physical symptoms and working performance in female breast cancer survivors: a systematic review. Disabil Rehabil. 2018;40(13):1485–93.
Feuerstein M, et al. Work in cancer survivors: a model for practice and research. J Cancer Surviv. 2010;4(4):415–37.
Monteiro I, et al. Changes in employment status up to 5 years after breast cancer diagnosis: a prospective cohort study. Breast. 2019;48:38–44.
Chan RJ, et al. A longitudinal analysis of phenotypic and symptom characteristics associated with inter-individual variability in employment interference in patients with breast cancer. Support Care Cancer. 2020;28(10):4677–86.
Tan CJ et al. Investigating how cancer-related symptoms influence work outcomes among cancer survivors: a systematic review. J Cancer Surviv, 2021.
Tiedtke C, et al. Experiences and concerns about 'returning to work’ for women breast cancer survivors: a literature review. Psychooncology. 2010;19(7):677–83.
Colombino ICF, et al. Factors associated with return to work in breast cancer survivors treated at the Public Cancer Hospital in Brazil. Support Care Cancer. 2020;28(9):4445–58.
Nascimento PF et al. Women’s occupational performance and quality of life during breast cancer treatment. BMJ Support Palliat Care, 2019.
Boelhouwer IG, Vermeer W, van Vuuren T. The associations between late effects of cancer treatment, work ability and job resources: a systematic review. Int Arch Occup Environ Health. 2021;94(2):147–89.
Lee MK, et al. Three-year prospective cohort study of factors associated with return to work after breast cancer diagnosis. J Occup Rehabil. 2017;27(4):547–58.
Gallicchio L et al. Evidence gaps in cancer survivorship care: a report from the 2019 National Cancer Institute Cancer Survivorship Workshop. J Natl Cancer Inst, 2021.
DeSantis CE, et al. Breast cancer statistics, 2019. CA Cancer J Clin. 2019;69(6):438–51.
ECIS - European Cancer Information System - incidence and mortality. 2020; Available from: https://ecis.jrc.ec.europa.eu/explorer.php?0-01-All2-All4-1,23-06-0,855-2008,20087-7CEstByCountryX0_8-3X0_19-AE27X0_20-NoCEstBySexByCountryX1_8-3X1_19-AE27X1_-1-1CEstByIndiByCountryX2_8-3X2_19-AE27X2_20-NoCEstRelativeX3_8-3X3_9-AE27X3_19-AE27CEstByCountryTableX4_19-AE27.
Paluch-Shimon S, et al. ESO-ESMO 4th International Consensus Guidelines for Breast Cancer in Young Women (BCY4). Ann Oncol. 2020;31(6):674–96.
Rosenberg SM, et al. Employment trends in young women following a breast cancer diagnosis. Breast Cancer Res Treat. 2019;177(1):207–14.
Ruggeri M, et al. Fertility concerns, preservation strategies and quality of life in young women with breast cancer: baseline results from an ongoing prospective cohort study in selected European Centers. Breast. 2019;47:85–92.
The Office for National Statistics UK. SOC2010 volume 3: the National Statistics Socio-economic classification (NS-SEC rebased on SOC2010). 2010 London, UK.
Sonnega A, et al. Cohort profile: the health and retirement study (HRS). Int J Epidemiol. 2014;43(2):576–85.
Gierisch JM, et al. Longitudinal predictors of nonadherence to maintenance of mammography. Cancer Epidemiol Biomarkers Prev. 2010;19(4):1103–11.
Stanton AL, Bernaards CA, Ganz PA. The BCPT symptom scales: a measure of physical symptoms for women diagnosed with or at risk for breast cancer. J Natl Cancer Inst. 2005;97(6):448–56.
Terhorst L, et al. Evaluation of the psychometric properties of the BCPT Symptom Checklist with a sample of breast cancer patients before and after adjuvant therapy. Psychooncology. 2011;20(9):961–8.
Ganz PA, et al. The CARES: a generic measure of health-related quality of life for patients with cancer. Qual Life Res. 1992;1(1):19–29.
Schag CA, Heinrich RL. Cancer Rehabilitation Evaluation System (CARES) manual. Santa Monica, CA: CARES Consultants; 1988.
Schag CA, Ganz PA, Heinrich RL. CAncer Rehabilitation Evaluation System–short form (CARES-SF). A cancer specific rehabilitation and quality of life instrument. Cancer. 1991;68(6):1406–13.
Kalbfleisch JD, Prentice RL. The statistical analysis of failure time data. Hoboken, NJ: Wiley & Sons Ltd; 1980.
Chan RJ et al. Future research in cancer survivorship. J Cancer Surviv, 2021.
de Boer AG, et al. Long-term work retention after treatment for cancer: a systematic review and meta-analysis. J Cancer Surviv. 2020;14(2):135–50.
Naughton MJ, et al. Prevalence and correlates of job and insurance problems among young breast cancer survivors within 18 months of diagnosis. BMC Cancer. 2020;20(1):432.
Hiltrop K et al. Involuntariness of job changes is related to less satisfaction with occupational development in long-term breast cancer survivors. J Cancer Surviv, 2021.
Swiss Federal Statistical Office. [cited 2022 May 04]; Available from: https://www.bfs.admin.ch/bfs/de/home/statistiken/wirtschaftliche-soziale-situation-bevoelkerung/gleichstellung-frau-mann/erwerbstaetigkeit.assetdetail.21804586.html
Istat. Tasso di occupazione. Available from: http://dati.istat.it/Index.aspx?DataSetCode=DCCV_TAXDISOCCU1.
Ragioneria Generale dello Stato. [cited 2022 May 12]; Available from: https://www.rgs.mef.gov.it/VERSIONE-I/attivita_istituzionali/formazione_e_gestione_del_bilancio/rendiconto/bilancio_di_genere.
Istat: Istituto Nationale di Statistica. [cited 2022 May 14]; Available from: https://www.istat.it/donne-uomini/bloc-2b.html?lang=it.
Bijker R, et al. Functional impairments and work-related outcomes in breast cancer survivors: a systematic review. J Occup Rehabil. 2018;28(3):429–51.
Tevaarwerk A, et al. Survivorship, Version 1.2021. J Natl Compr Canc Netw. 2021;19(6):676–85.
de Boer AG, et al. Interventions to enhance return-to-work for cancer patients. Cochrane Database Syst Rev. 2015;9:CD007569.
Acknowledgements
The IBCSG 43-09 HOHO European protocol was developed and conducted by the Frontier Science & Technology Research Foundation, Southern Europe (FSE) and the International Breast Cancer Study Group (IBCSG) with the financial support of the Fondazione Leonardo, Lugano Switzerland, Pink Ribbon Switzerland and private donations. We thank the patients, physicians, nurses, and trial coordinators who participated in the HOHO study.
Funding
This work was supported by the Frontier Science & Technology Research Foundation, Southern Europe (FSE), Chiasso, Switzerland and the International Breast Cancer Study Group (IBCSG), Bern, Switzerland.
Author information
Authors and Affiliations
Contributions
Karin Ribi PhD: manuscript writing — original draft; manuscript review, editing, and approval. Eleonora Pagan PhD: statistical analysis, manuscript writing — original draft; manuscript review, editing, and approval. Isabella Sala MSc: statistical analysis, manuscript writing — original draft; manuscript review, editing, and approval. Monica Ruggeri: conceptualization and study design; data management; manuscript writing — original draft; manuscript review, editing, and approval. Nadia Bianco MD: data acquisition; manuscript review, editing, and approval. Eraldo Oreste Bucci MD: data acquisition; manuscript review, editing, and approval. Rossella Graffeo MD: data acquisition; manuscript review, editing, and approval. Markus Borner MD: data acquisition; manuscript review, editing, and approval. Monica Giordano MD: data acquisition; manuscript review, editing, and approval. Lorenzo Gianni MD: data acquisition; manuscript review, editing, and approval. Manuela Rabaglio MD: data acquisition; manuscript review, editing, and approval. Andrea Freschi MD: data acquisition; manuscript review, editing, and approval. Elisabetta Cretella MD: data acquisition; manuscript review, editing, and approval. Elena Seles MD: data acquisition; manuscript review, editing, and approval. Alberto Farolfi MD: data acquisition; manuscript review, editing, and approval. Edda Simoncini MD: data acquisition; manuscript review, editing, and approval. Mariangela Ciccarese MD: data acquisition; manuscript review, editing, and approval. Daniel Rauch MD: data acquisition; manuscript review, editing, and approval. Adolfo Favaretto MD: data acquisition; manuscript review, editing, and approval. Agnes Glaus PhD, MSc: data acquisition; manuscript review, editing, and approval. Rossana Berardi MD: data acquisition; manuscript review, editing, and approval. Alessandra Franzetti-Pellanda MD: data acquisition; manuscript review, editing, and approval. Vincenzo Bagnardi PhD: conceptualization and study design, statistical analysis, manuscript writing — original draft; manuscript review, editing, and approval. Shari Gelber PhD, MSc: conceptualization and study design; statistical analysis; manuscript review, editing, and approval. Ann H. Partridge MD, MPH: conceptualization and study design; manuscript review, editing, and approval. Aron Goldhirsch MD: conceptualization and study design. Olivia Pagani MD: conceptualization and study design; data acquisition; manuscript writing — original draft; manuscript review, editing, and approval.
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
The manuscript does not contain any individual person’s data in any form, and consent for publication was therefore not obtained from the patients included in this study.
Competing interests
Karin Ribi reports no conflicts related to this study, Eleonora Pagan reports no conflicts related to this study, Isabella Sala reports no conflicts related to this study, Monica Ruggeri reports no conflicts related to this study, Nadia Bianco reports no conflicts related to this study, Eraldo Oreste Bucci receives consulting or advisory fees from Astra Zeneca and travels/accommodations from Astellas, BMS, Lilly, Merck Serono, Roche, Takeda, Rossella Graffeo reports no conflicts related to this study, Markus Borner reports no conflicts related to this study, Monica Giordano reports no conflicts related to this study, Lorenzo Gianni receives consulting or advisory fees from Astra Zeneca and travels/accommodations from Novartis, Manuela Rabaglio reports no conflicts related to this study, Andrea Freschi reports no conflicts related to this study, Elisabetta Cretella reports no conflicts related to this study, Elena Seles reports no conflicts related to this study, Alberto Farolfi receives honoraria from Janssen Oncology, GSK-Tesaro, Astrazeneca, Clovis, Edda Simoncini reports no conflicts related to this study, Mariangela Ciccarese reports no conflicts related to this study, Daniel Rauch (pending), Adolfo Favaretto reports no conflicts related to this study, Agnes Glaus reports no conflicts related to this study, Rossana Berardi receives donations to her institution and/or fees for advisory board participations from AZ, BI, Novartis, MSD, Otsuka, Lilly, Roche, Amgen, GSK, EISAI (none related to this study), Alessandra Franzetti-Pellanda reports no conflicts related to this study, Vincenzo Bagnardi reports no conflicts related to this study, Shari Gelber reports no conflicts related to this study, Ann H. Partridge (pending), and Olivia Pagani reports no conflicts related to this study.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Aron Goldhirsch deceased.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ribi, K., Pagan, E., Sala, I. et al. Employment trajectories of young women with breast cancer: an ongoing prospective cohort study in Italy and Switzerland. J Cancer Surviv 17, 1847–1858 (2023). https://doi.org/10.1007/s11764-022-01222-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-022-01222-y