Abstract
Purpose
To assess associations between usual source of care (USC) type and health status, healthcare access, utilization, and expenses among adult cancer survivors.
Methods
This retrospective cross-sectional analysis using 2013–2018 Medical Expenditure Panel Survey included 2690 observations representing 31,953,477 adult cancer survivors who were currently experiencing cancer and reporting one of five USC types: solo practicing physician (SPP), a specific person in a non-hospital facility, a specific person in a hospital-based facility, a non-hospital facility, and a hospital-based facility. We used logistic regressions and generalized linear models to determine associations of USC type with health status, healthcare access, utilization, and expenses, adjusting for patient demographic and clinical characteristics.
Results
All non-SPP USC types were associated with reporting more difficulties contacting USC by telephone during business hours (p < 0.05). Compared to SPP, non-hospital facility was associated with more difficulty getting needed prescriptions (OR: 1.81, p = 0.036) and higher annual expenses ($5225, p = 0.028), and hospital-based facility was associated with longer travel time (OR: 1.61, p = 048), more ED visits (0.13, p = 0.049), higher expenses ($6028, p = 0.014), and worse self-reported health status (OR: 1.93, p = 0.001), although both were more likely to open on nights/weekends (p < 0.05). Cancer survivors with a specific person in a hospital-based facility (vs. SPP) as USC were > twofold as likely (p < 0.05) to report difficulty getting needed prescriptions and contacting USC afterhours.
Conclusions
Among adult cancer survivors who were currently experiencing cancer, having a non-SPP type of UCS was associated with reporting more difficulties accessing care, worse health, more ED visits, and higher total expenses.
Implications for Cancer Survivors
Transitioning to SPP type of USC may result in better healthcare outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Equity in healthcare delivery is considered a benchmark of quality of healthcare by the Institute for Healthcare Improvement [1]. Differences in accessing care, receiving treatment, and experiencing outcomes may randomly exist in any healthcare setting. However, when these differences occur systematically, they constitute healthcare disparities [1]. Age [2], race/ethnicity [3, 4], sex [5, 6], socioeconomic status [7], or geographic location [8], or a combination of these, are the major risk factors contributing to healthcare disparities. Average or weighted average of the care quality may mask poor quality of care received by subgroups of populations.
Studies assessing access to healthcare usually adjust for whether or not a person has a usual source of care (USC) [9,10,11]. Lack of a USC has been associated with healthcare disparities [10]; having a USC improves timely access to medical care [12] and improves health care quality, resulting in improved health [13]. However, very few studies have compared the different types of USC and how they affect access to healthcare, healthcare utilization, and costs differently. Several South Korean studies found that having a person as a USC, as opposed to a facility, has been associated with lower odds of hospitalizations and emergency department (ED) visits [13], and better quality of care [14]. In the US healthcare setting, having a doctor’s office where physicians practice either independently or as a part of a group as the USC has been associated with improved access to healthcare as compared to hospital outpatient clinic or other clinics or health centers [15]. Moreover, person-in-facility and facility, compared to solo practicing physician (SPP) type USC, have been associated with higher odds of having an ED visit among low-income individuals [16]. While these studies focus on the general population, little is known about the associations of different types of USC with healthcare access, cost, and outcomes among cancer survivors.
Cancer survivors have unique healthcare needs manifesting from various physical, functional, and psychosocial limitations [17], and often require care from a wide range of healthcare providers including doctors, nurses, and pharmacists to manage their special needs [18]. Coordination of cancer care provided to cancer survivors by different types of providers is crucial to deliver high-quality care. A primary care physician–type USC, who could either be SPP or a specific person in a non-hospital or hospital-based facility, may be better able to act as the link between a survivor’s cancer-related and non-cancer-related care [19]. Being most familiar with a patient’s medical history, a primary care physician may also help manage comorbid conditions and/or chronic pain, provide follow-up care, and assist in palliative care [19, 20]. However, the associations of USC location (a hospital-based facility, non-hospital facility, or personal office) with healthcare outcomes are yet to be studied among cancer survivors.
Given the disease agnostic nature and the limited number of studies evaluating associations of the USC type with healthcare access and utilization, this study aimed to assess the association between the USC type and healthcare access, utilization, self-reported health status, and total healthcare expenses among adult cancer survivors who were currently experiencing cancer and reported having a USC.
Methods
Data sources
We used the 2013–2018 Medical Expenditure Panel Survey (MEPS) data. The MEPS is collected and maintained by the Agency for Healthcare Research and Quality [21]. Non-institutionalized individuals who have responded to the National Health Interview Survey (NHIS) form the sampling frame of MEPS household component (HC) [22]. Details of the MEPS survey process can be found elsewhere [21]. MEPS uses an overlapping panel design where data about an individual is collected over a 2-year period and data collection for 2 separate panels proceeds simultaneously over 3 rounds within a calendar year (rounds 1–3 of the new panel and rounds 3–5 of the existing panel) [22]. The MEPS-HC collects information regarding insurance coverage, income, education, employment, total healthcare utilization, and total healthcare expenses.
Study design and cohort selection
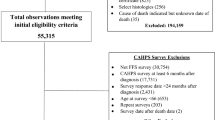
This retrospective cross-sectional study consisted of adult (aged ≥ 18 years) cancer survivors who were currently experiencing cancer and reported having a USC in a calendar year. Consistent with the National Cancer Institute’s definition of a cancer survivor [23], we defined a “cancer survivor” as someone who has ever been diagnosed with cancer. In MEPS, the full-year consolidated data file includes self-reported information on whether a person has ever been diagnosed with cancer. Additionally, the medical conditions file provides information on a person’s reported “current” medical conditions that are coded using the International Classification of Diseases 9th and 10th revision clinical modification codes (ICD-9-CM and ICD-10-CM codes). While a current medical condition was defined as a “condition reported as existing for a MEPS sample person at any time during the specific data year (i.e., those identified in the conditions enumeration (CE), medical events (ME), or disability days (DD) sections of the questionnaire)” for years 2013–2017 [24], this definition was revised in 2018 to include only medical conditions that can be linked to a medical event (i.e., in the ME section) [25]. To be consistent across all years, we considered a medical condition as current if it was associated with a medical event (inpatient stay, outpatient visit, office-based visit, ED visit, prescription medication, and home health visit) during the calendar year. For this study, we restricted our sample to individuals self-reported as ever been diagnosed with cancer using the full-year consolidated file and having reported cancer as a current condition using the medical conditions file. Following previous studies, we did not include individuals who reported only non-melanoma skin cancer or cancer of unknown type but no other cancers [26] (see Appendix Table 1 for the diagnosis codes used to identify cancer in the medical conditions file). In addition, we restricted the study to individuals who reported having a USC. In each calendar year, we excluded records for individuals who (1) were not in-scope in all survey rounds to avoid any bias due to differential follow-up times, (2) did not report a USC, (3) reported emergency room as USC, or (4) did not report location of USC. Figure 1 provides details on cohort selection.
Sample selection flowchart. A record indicates an individual’s information for a given calendar year. “n” refers to the number of observations. A medical condition was considered “current” if it was associated with a medical event (inpatient stay, outpatient visit, office-based visit, emergency department visit, prescription medication, and home health visit) during the calendar year
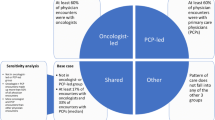
Type of usual source of care
Questions regarding USC are asked once in a calendar year as a part of Access to Care (AC) section of the MEPS-HC questionnaire and are fielded in the second round (round 4/2) [27]. In MEPS, a USC is defined as a particular doctor’s office, clinic, health center, or other place that the individual usually goes to if he/she is sick or needs advice about his/her health [28]. For persons reporting a USC, MEPS determines if the provider type is a (1) facility, (2) person, or (3) person-in-facility. Furthermore, MEPS asks the provider’s location: (1) an office, (2) hospital clinic/outpatient department, or (3) a hospital emergency room. Like previous studies [29], we excluded anyone who reported a hospital emergency room as their USC. Based on the remaining provider types and location combinations, the USC type was classified into 5 mutually exclusive groups: (1) solo practicing physician (SPP) (reference group); (2) a specific person in a non-hospital facility; (3) a specific person in a hospital clinic/outpatient department (hereafter referred to as a specific person in a hospital-based facility); (4) non-hospital facility; and (5) hospital clinic/outpatient department (hereafter referred to as a hospital-based facility).
Study outcomes
We studied the association of USC type with five types of outcomes: (a) access to USC provider; (b) delay/inability to get needed care; (c) self-reported health status; (d) healthcare utilization; and (e) total healthcare expenses. “Access to USC provider” included four measures: (1) difficulty contacting the USC provider during regular business hours over the telephone about a health problem; (2) difficulty contacting the USC provider after their regular hours in case of urgent medical needs; (3) USC open at nights/on weekends; and (4) traveling > 30 min to see USC provider. We defined the “Access to USC provider” measures as binary variables. For the first two measures with four levels, we dichotomized as follows: a person reporting “Somewhat difficult” or “Very difficult” was considered as “having difficulty” while a person reporting “Not too difficult” or “Not at all difficult” was considered “not having difficulty.” “Delay/inability to get needed care” measures included two binary measures (Yes/No) for delay/inability to get needed (1) medical care and (2) prescription medications. Self-reported health status is reported for the first (round 3/1) and last (round 5/3) rounds of each year. We used self-reported health status in the first round as a covariate to adjust for baseline health status and used the health status reported in the last round as an outcome variable. Health status as an outcome variable was defined as a binary variable: “Good” health if a person reported “excellent”/ “very good”/ “good” health; and “Not Good” health if reported “fair”/ “poor” health. Healthcare utilization was measured as the total annual number of (1) ED visits and (2) inpatient stays, since both may be an indication of poor healthcare quality. Total annual expenses were the “sum of direct payments for care provided during the year, including out-of-pocket payments and payments by private insurance, Medicaid, Medicare, and other sources.” [28]. The sum included expenses associated with office-based physician and non-physician visits, inpatient stays, hospital outpatient visits, ED visits, prescribed medicines, home health visits, medical equipment and services, and dental and vision services [28], and was inflation-adjusted to 2018 US dollars [30].
Covariates
For all analyses, we adjusted for the following covariates: socio-demographic variables (age, sex, race/ethnicity, family income as a percent of federal poverty level, education level, insurance), geographic region, baseline health status (self-reported health status in round 3/1), number of comorbid conditions, cancer site, calendar year, and being in remission. In MEPS, a set of medical conditions were considered priority conditions because of “their relatively high prevalence” and “generally accepted criteria for assessing appropriate clinical care.” [23]. Besides cancer, the “priority” conditions in MEPS include high blood pressure, heart disease, stroke, emphysema, chronic bronchitis, high cholesterol, diabetes, joint pain, arthritis, and asthma [23]. We counted the number of these non-cancer conditions and classified as (0, 1, or ≥ 2) following previous studies [31,32,33].
Remission status was not directly available in MEPS. To determine whether a survivor was being actively treated or in remission, we developed an algorithm as follows. We first examined the self-reported visit categories for outpatient and office-based visits from respective event files for all the persons in the study sample. If a visit was categorized as “Diagnosis or Treatment” or “Follow-up or Post-operative visit,” then we considered the event was for active treatment of cancer. Outpatient and office visits for all other reasons (“General checkup,” “Emergency (e.g., accident or injury),” “Psychotherapy/Mental Health Counselling,” “Immunizations or shots,” “Vision Exam,” “Pregnancy-related (including prenatal/delivery),” “Well Child Exam,” “Laser Eye Surgery,” and “Other”) were considered not for active cancer treatment. Since this variable is only available for outpatient or office-based visits, we used the following algorithm to identify active cancer treatment for other healthcare events. If a home health visit, inpatient stay, or an ED visit was reported to be related to cancer, we considered the visit to be for cancer treatment. If a prescription was for drugs in “antineoplastics,” “antineoplastic hormones,” or “topical antineoplastics” therapeutic classes, we considered that the prescription was for cancer treatment. All persons who did not have any medical event indicating they were being actively treated for cancer by our aforementioned definition were considered to be in remission in that year. Appendix Table 2 provides further description of the covariates.
Statistical analysis
We assessed associations of each of the outcomes with USC type adjusting for the covariates. Logistic regressions were used for six binary outcomes: (1) delay/inability to get needed medical care; (2) delay/inability to get needed prescription medications; (3) difficulty contacting the USC provider during regular business hours over the telephone about a health problem; (4) difficulty contacting the USC provider after their regular hours in case of urgent medical needs; (5) USC open at nights/on weekends; and (6) traveling > 30 min to see USC provider. Generalized linear models (GLMs) with a negative binomial distribution and a log link were used to analyze count outcomes: (1) total ED visits and (2) total inpatient stays since these outcomes had distributions that were over-dispersed and right skewed with heavy kurtosis. GLM with a gamma distribution and a log link was used to analyze total expenses since the expenses were right skewed with heavy kurtosis.
We used SAS v.9.4 and STATA v.16.1 to perform statistical analysis. STATA svy commands were used for all bivariate and multivariate analyses to adjust for complex survey design and obtain nationally representative estimates of the non-institutionalized population and standard errors were adjusted for survey clustering using Taylor series linearization [34]. Since the MEPS is de-identified public-use data, no IRB approval was needed.
Results
Study cohort and demographics
After applying inclusion and exclusion, the study sample included 2690 observations representing 31,953,477 cancer survivors over the study period. Table 1 compares the demographic and clinical characteristics of cancer survivors by USC type. In the unweighted sample, 24.4% had SPP, 20.1% had non-hospital facility, 16.1% had hospital-based facility, 27.9% had a specific person in a non-hospital facility, and 11.5% had a specific person in a hospital-based facility as their USC. The study sample had 68.3% non-Hispanic whites, 13.8% non-Hispanic blacks, 12.6% Hispanics, and 5.3% belonging to other races. About 60% of the cohort either had private insurance or were uninsured, aged ≥ 65 years, and had ≥ 2 comorbidities. Moreover, about 30% of the cohort reported fair or poor health in the first round (round 1/3), 67.9% having high income and 84.8% having a high school diploma or higher education. The study sample had a slightly higher proportion of females as compared to males. About one-fourth of the survivors were in remission. There was no difference in remission status by USC type.
Health status and access to healthcare
Table 2 provides adjusted odds ratios (ORs) and 95% confidence intervals (CIs) for associations of self-reported health and healthcare access outcomes with USC type. When compared to survivors with SPP-type USC, survivors with hospital-based facility–type USC reported higher odds (OR: 1.93, 95% CI: 1.32–2.83; p = 0.001) of having “Not good” health in round 5/3. Compared to SPP, survivors with all other types of USC had significantly higher odds of facing difficulty in contacting USC during regular business hours over the telephone about a health problem, with ORs ranging from 1.66 (95% CI: 1.09–2.54; p = 0.019) for a non-hospital facility to 2.08 (95% CI: 1.27–3.40; p = 0.004) for a specific person in a hospital-based facility–type USC. Moreover, people having a specific person in a hospital-based facility (compared to SPP) type USC also faced more difficulty contacting the USC during afterhours in case of urgent medical needs (OR: 2.07, 95% CI: 1.24–3.47; p = 0.006) and accessing needed prescription medications (OR: 2.28, 95% CI: 1.10–4.73; p = 0.028). People with non-hospital facility (compared to those with SPP) type USC reported higher odds of facing delay and/or inability in accessing needed prescription medications (OR: 1.81, 95% CI: 1.04–3.16; p = 0.036). On the other hand, survivors with non-hospital facility (OR: 3.81, 95% CI: 2.57–5.66; p < 0.001) and hospital-based facility (OR: 4.19, 95% CI: 2.72–6.44; p < 0.001) type USC reported higher odds of their USC being open at nights/weekends compared to survivors with SPP-type USC. Only survivors with hospital-based facility–type USC reported significantly higher odds (OR: 1.61, 95% CI: 1.00–2.58; p = 0.048) of travelling > 30 min to see USC provider. We did not find any significant differences by USC type in reporting delay/inability to get needed medical care.
Annual healthcare utilization and total expenses
Table 3 provides adjusted predicted means and differences in predicted means and 95% CIs for inpatient stays, ED visits, and total expenses. Survivors with hospital-based facility–type USC reported on average more ED visits annually (0.13 [95% CI: 0.00–0.26]; p = 0.049) and higher average annual total expenses ($6028 [95% CI: $1235–$10,822]; p = 0.014) as compared to survivors with SPP-type USC. Additionally, survivors with non-hospital facility–type USC also reported incurring higher average annual total expenses ($5225 [95% CI: $557–$9892]; p = 0.028) as compared to survivors with SPP-type USC. We did not find any significant association between USC type and the number of inpatient stays.
Discussion
In this nationally representative sample of adult cancer survivors with a non-ED USC type who were currently experiencing cancer, we found that different USC types when compared to SPP were associated with a greater likelihood of reporting difficulty in accessing care, “Not good” health, more ED visits, and higher total expenses.
Compared to SPP, survivors with all other USC types reported more difficulties contacting their USC providers over telephone during regular business hours. The ability to consult with providers regarding health problems through telecommunication technologies such as a telephone is a key aspect of telemedicine [35]. Telemedicine has been popular among cancer survivors who do not have easy access to a healthcare facility or must travel a long distance for medical appointment [36]. Besides being highly useful in delivering care to populations that have limited access to healthcare, telemedicine has been shown to be at par with in-person care [37]. Moreover, telemedicine also helps decrease healthcare costs [37]. Post-operative telemedicine provided to cancer survivors may also reduce ED visits [38]. Thus, difficulty in contacting USC about health problems by telephone during regular business hours would augment healthcare disparities among cancer survivors with non-SPP types of USC. On the other hand, having a non-hospital or a hospital-based facility–type USC may offer additional access during nights or weekends. We found that non-hospital facility and hospital-based facility types of USC were associated with significantly higher odds of being open during nights or weekends. Survivors with facility type of USC may have an option to see any provider available during nights or weekends, but continuity of care may be jeopardized.
Consistent with previous findings [13], hospital-based facility (compared to SPP) type USC was associated with a significantly higher mean number of ED visits. Acute healthcare utilization such as ED visits is often an indication of poor access to primary care, poor care coordination, and poor choices on the part of beneficiaries [39]. Given the high costs associated with ED visits, avoiding preventable ED visits would significantly help reduce total healthcare costs [40]. The high mean number of ED visits partially explains the significantly higher mean total healthcare expenses for hospital-based facility as compared to person-facility–type USC. Moreover, survivors with non-hospital facility compared to SPP-type USC also reported significantly higher mean total healthcare expenses. Healthcare services provided by USC providers located in a hospital facility (hospital-based facility/a specific person in a hospital-based facility) would include facility charges, in addition to charges for professional services, while USC providers in offices outside of hospital would only charge for professional services. Such additional charges would also increase the total healthcare expenses for cancer survivors who seek care through USC types having hospital-based locations.
Having a SPP-type USC indicates that the patient would most often interact with the same provider. Such interactions may eventually lead to developing strong patient-provider relationship [41]. Survivors who have an ongoing relationship with their provider are likely to develop trust in their provider and receive more personalized care, which may help in better adherence to provider’s advice and timely follow-up [42]. A high likelihood of seeing a different provider during health service encounters may lead to lack of care coordination, polypharmacy, higher chances of medical errors, poorly controlled symptoms, and higher medical costs [43]. While medical errors and poorly controlled symptoms may increase odds of a person reporting “Not Good” health, polypharmacy, lack of adherence to medical advice, and high healthcare costs may also explain higher odds of delay/inability to get needed prescription medications.
Our study findings show that different non-SPP types of USC were associated with worse healthcare access, poorer health outcome, and higher healthcare expenses. These findings highlight the importance of having a SPP-type USC among cancer survivors. With the ongoing national trend of physician practice mergers and acquisitions, access to SPPs may continue to decrease. A Physicians Advocacy Institute (PAI) report found a steep rise in the number of hospital-acquired physician practices over a period from mid-2012 through January 2018 [44]. The proportion of all the physicians in the USA who were employed by hospitals jumped from 25% in 2012 to 44% in early 2018, marking a 76% rise [44]. However, whether this consolidation improves patient care or lowers healthcare costs has been questioned. Consistent with our findings, research conducted by Avalere and released by PAI found that between 2012 and 2015, Medicare costs and financial responsibility of Medicare beneficiaries increased by $3.1 billion and $411 million, respectively, when using select cardiology, orthopedic, and gastroenterology services performed by hospital-employed physicians compared to if they were performed in independent physicians’ offices [45]. Moreover, routine services such as cardiac imaging, colonoscopy, and evaluation and management consistently cost higher when performed in hospital outpatient department as opposed to a physician’s office [45]. Larger studies are warranted to confirm our findings about poor healthcare outcomes among cancer survivors with non-SPP types of USC.
Several limitations of this study are worth noting. MEPS does not provide cancer-related clinical variables such as age at diagnosis, cancer stage, tumor grade, and other histological characteristics. Remission status was not directly available in MEPS. The variable for being in remission was derived from (1) self-reported reasons for office-based and outpatient visits; (2) inpatient, ED, or home health visits linked to cancer condition; or (3) antineoplastic prescriptions use, which may not accurately represent the clinical remission status. Moreover, we do not have detailed information regarding the type of treatment such as radiation or systemic chemotherapy use and therefore could not determine how patterns of cancer care differ by USC type. Despite adjusting our regression models for key socio-demographic characteristics, unmeasured variables such as health literacy, attitudes, and beliefs regarding healthcare resource utilization could potentially confound healthcare utilization. In MEPS, information about the USC is asked only in the second round (4/2), but a person may change USC type over the year.
In this nationally representative study of cancer survivors with a USC who was currently experiencing cancer, having any non-SPP (vs. SPP) type of USC was found to be associated with reporting more difficulties accessing care, worse health, more ED visits, and higher total expenses. Further research is warranted to replicate and extend findings of this study to better understand key factors contributing to these differences among cancer survivors.
References
Institute for Healthcare Improvement: Health Equity. (2020). Retrieved January 13, 2020, from http://www.ihi.org/Topics/Health-Equity/Pages/default.aspx
Williams MM. Invisible, unequal, and forgotten: health disparities in the elderly. Notre Dame Journal of Law Ethics Public Policy. 2007;21(2):441–78.
Farias AJ, Ochoa CY, Toledo G, Bang SI, Hamilton AS, Du XL. Racial/ethnic differences in patient experiences with health care in association with earlier stage at breast cancer diagnosis: findings from the SEER-CAHPS data. Cancer Causes Control. 2019. https://doi.org/10.1007/s10552-019-01254-3.
Weech-Maldonado R, Elliott MN, Adams JL, Haviland AM, Klein DJ, Hambarsoomian K, Gaillot, S. Do racial/ethnic disparities in quality and patient experience within Medicare plans generalize across measures and racial/ethnic groups? In Health Serv Res 2015;50:1829–1849). Blackwell Publishing Inc. https://doi.org/10.1111/1475-6773.12297
Kent JA, Patel V, Varela NA. Gender disparities in health care. Mt Sinai J Med: J Transl Pers Med. 2012;79(5):555–9. https://doi.org/10.1002/msj.21336.
MacCarthy S, Burkhart Q, Haviland AM, Dembosky JW, Wilson-Frederick S, Saliba D, Elliott MN. Exploring disparities in influenza immunization for older women. J Am Geriatr Soc. 2019;67(6):1268–72. https://doi.org/10.1111/jgs.15887.
Rogowski J, Freedman VA, Wickstrom SL, Adams J, Escarce JJ. Socioeconomic disparities in medical provider visits among Medicare managed care enrollees. Inquiry : J Med Care Organ, Prov Financ. 2008;45(1):112–29. https://doi.org/10.5034/inquiryjrnl_45.01.112.
Mollica MA, Weaver KE, McNeel TS, Kent EE. Examining urban and rural differences in perceived timeliness of care among cancer patients: a SEER-CAHPS study. Cancer. 2018;124(15):3257–65. https://doi.org/10.1002/cncr.31541.
Fastiggi MJ, Sim J-A, Huang I-C. Association of co-morbidities with financial hardship in survivors of adult cancer. Support Care Cancer : Off J Multinatl Assoc Support Care Cancer. 2021. https://doi.org/10.1007/S00520-021-06313-7.
Park S, Chen J, Ma GX, Ortega AN. Inequities in access to care and health care spending for Asian Americans with cancer. Med Care. 2021;59(6):528–36. https://doi.org/10.1097/MLR.0000000000001538.
Donley T, Tshiswaka DI, Blanc J, Seixas A, Okafor A, Mbizo J. Differences in breast and cervical cancer screening among U.S. women by nativity and family history. Am J Prev Med 2020;59(4): 578–587. https://doi.org/10.1016/J.AMEPRE.2020.05.018
Moss JL, Roy S, Shen C, Cooper JD, Lennon RP, Lengerich EJ, Ruffin MT. Geographic variation in overscreening for colorectal, cervical, and breast cancer among older adults. JAMA Netw Open. 2020;3(7):e2011645–e2011645. https://doi.org/10.1001/JAMANETWORKOPEN.2020.11645.
Kim KM, Jeon H, Lee JH. Having a physician rather than a place as a usual source of care would be better - from 2012 Korea health panel data. J Korean Med Sci. 2017;32(1):4–12. https://doi.org/10.3346/jkms.2017.32.1.4.
Sung NJ, Lee JH. Association between types of usual source of care and user perception of overall health care service quality in Korea. Korean J Fam Med. 2019;40(3):143–50. https://doi.org/10.4082/kjfm.17.0093.
Shi L, Nie X, Wang TFF. Type of usual source of care and access to care, 2013;36(3): 209–221
Liaw W, Jetty A, Petterson S, Bazemore A, Green L. Trends in the types of usual sources of care: a shift from people to places or nothing at all. Health Serv Res. 2018;53(4):2346–67. https://doi.org/10.1111/1475-6773.12753.
De Moor JS, Virgo KS, Li C, Chawla N, Han X, Blanch-Hartigan D, Yabroff KR. Access to cancer care and general medical care services among cancer survivors in the United States: an analysis of 2011 medical expenditure panel survey data. Public Health Rep. 2016;131(6):783–90. https://doi.org/10.1177/0033354916675852.
People in Health Care - National Cancer Institute. (n.d.). Retrieved December 4, 2020, from https://www.cancer.gov/about-cancer/managing-care/services/providers
Klabunde CN, Ambs A, Keating NL, He Y, Doucette WR, Tisnado D, Kahn KL. The role of primary care physicians in cancer care. J Gen Intern Med. 2009;24(9):1029–36. https://doi.org/10.1007/s11606-009-1058-x.
Chaput G, Broad K. (2018, August 1). General practitioners in oncology: their valuable role throughout the cancer care trajectory. Curr Oncol Multimed Inc.https://doi.org/10.3747/co.25.4222
Agency for Healthcare Research and Quality (AHRQ). (n.d.).Medical Expenditure Panel Survey Background. Retrieved May 11, 2020, from https://www.meps.ahrq.gov/mepsweb/about_meps/survey_back.jsp
Agency for healthcare research and quality. (n.d.).Medical Expenditure Panel Survey Content Summary of the Household Interview. Retrieved December 4, 2020, from https://www.meps.ahrq.gov/mepsweb/survey_comp/hc_data_collection.jsp
Definition of survivorship - NCI Dictionary of Cancer Terms - National Cancer Institute. (n.d.). Retrieved November 29, 2021, from https://www.cancer.gov/publications/dictionaries/cancer-terms/def/survivorship
Agency for Healthcare Research and Quality (AHRQ). (n.d.).Understanding and analyzing MEPS household component medical condition data. Retrieved April 7, 2022, from https://meps.ahrq.gov/survey_comp/MEPS_condition_data.shtml
IPUMS. (n.d.).IPUMS MEPS. Retrieved April 12, 2022, from https://meps.ipums.org/meps/userNotes_2018changes.shtml
CDC (Centers for Disease Control and Prevention). (2014). Medical Costs and Productivity Losses of Cancer Survivors — United States, 2008–2011.
Agency for Healthcare Research and Quality (AHRQ). (n.d.). Access to care: Medical Expenditure Panel Survey Topics. Retrieved April 8, 2022, from https://meps.ahrq.gov/mepsweb/data_stats/MEPS_topics.jsp?topicid=1Z-1
Agency for Healthcare Research and Quality. (2017). Medical Expenditure Panel Survey HC-201 2017 Full Year Consolidated Data File.
Simon AE, Rossen L, Schoendorf KC, Larson K, Olson LM. Location of usual source of care among children and adolescents in the US, 1997–2013. J Pediatr. 2015;167(6):1409. https://doi.org/10.1016/J.JPEDS.2015.09.026.
Calculator, U. S. I. (2020). Inflation Calculator | Find US Dollar’s Value from 1913–2020. Retrieved December 3, 2020, from https://www.usinflationcalculator.com/
Rai A, Han X, Zheng Z, Yabroff KR, Jemal A. Determinants and outcomes of satisfaction with healthcare provider communication among cancer survivors. JNCCN J Natl Compr Canc Netw. 2018;16(8):975–84.
Henry Olaisen R, Schluchter MD, Flocke SA, Smyth KA, Koroukian SM, Stange KC (n.d.). Assessing the longitudinal impact of physician-patient relationship on functional health, 18(5). https://doi.org/10.1370/afm.2554
Williams JS, Lu K, Akinboboye O, Olukotun O, Zhou Z, Nagavally S, Egede LE. Trends in obesity and medical expenditure among women with diabetes, 2008–2016: differences by race/ethnicity. Ethn Dis 2020;30(4): 621–628. https://doi.org/10.18865/ED.30.4.621
Agency for Healthcare Research and Quality. (2020). MEPS HC-209 2018 Full Year Consolidated Data File Codebook.
Health Resources and Services Administration (HRSA). (2021). What is telehealth? | Telehealth.HHS.gov. Retrieved July 27, 2021, from https://telehealth.hhs.gov/patients/understanding-telehealth/
American Cancer Society. (2020). Telemedicine and telehealth. Retrieved from https://www.cancer.org/treatment/finding-and-paying-for-treatment/choosing-your-treatment-team/telemedicine-telehealth.html#written_by
Sirintrapun SJ, Lopez AM. Telemedicine in cancer care. 2018. https://doi.org/10.1200/EDBK_200141,(38),540-545.doi:10.1200/EDBK_200141.
Knudsen KE, Willman C, Winn R. Optimizing the use of telemedicine in oncology care: postpandemic opportunities. Clin Cancer Res. 2021;27(4):933–6. https://doi.org/10.1158/1078-0432.CCR-20-3758.
Dowd B, Karmarker M, Swenson T, Parashuram S, Kane R, Coulam R, Jeffery MM. Emergency department utilization as a measure of physician performance. Am J Med Q: T Off J Am Coll Med Q. 2014;29(2):135–43. https://doi.org/10.1177/1062860613487196.
Weinick RM, Burns RM, Mehrotra A. How many emergency department visits could be managed at urgent care centers and retail clinics? Health affairs (Project Hope). 2010;29(9):1630. https://doi.org/10.1377/HLTHAFF.2009.0748.
Goold SD, Lipkin M. The doctor-patient relationship: challenges, opportunities, and strategies. J Gen Intern Med. 1999;14(1 SUPPL.):S26. https://doi.org/10.1046/j.1525-1497.1999.00267.x.
Chandra S, Mohammadnezhad M, Ward P. Trust and communication in a doctor-patient relationship: a literature review. J Health Commun. 2018;3(3):36. https://doi.org/10.4172/2472-1654.100146.
Gorin SS, Haggstrom D, Han PKJ, Fairfield KM, Krebs P, Clauser SB. Cancer care coordination: a systematic review and meta-analysis of over 30 years of empirical studies. Ann Behav Med. 2017;51(4):532–46. https://doi.org/10.1007/s12160-017-9876-2.
Physicians Advocacy Institute (PAI). (2019). Physician employment and practice acquisition trends: 2012–2018. Retrieved March 30, 2022, from http://www.physiciansadvocacyinstitute.org/PAI-Research/Physician-Employment-and-Practice-Acquisition-Trends-2012-2018
Physicians Advocacy Institute (PAI). (2019). Updated Physician Practice Acquisition Study: National and Regional Changes in Physician Employment 2012–2018.
Acknowledgements
The authors would like to acknowledge Ms. Sonali Joshi from the Fort Worth Independent School District (Texas) for her help with copyediting the manuscript.
Funding
CL is supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Number UL1 TR003107-02S2. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interests to declare. CL received research funding for an unrelated project sponsored by University of Utah/AstraZeneca.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pandit, A.A., Li, C. Types of usual sources of care and their association with healthcare outcomes among cancer survivors: a Medical Expenditure Panel Survey (MEPS) study. J Cancer Surviv 17, 748–758 (2023). https://doi.org/10.1007/s11764-022-01221-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-022-01221-z