Abstract
Purpose
Existing research hints that people living with and beyond cancer are at an increased risk of stroke. However, there is insufficient evidence to appropriately inform guidelines for specific stroke prevention or management for cancer patients. We conducted a systematic review and meta-analysis to describe and quantify stroke incidence in people living with and beyond cancer.
Methods
Medline, CINAHL, and EMBASE were searched for epidemiological studies comparing stroke incidence between cancer and non-cancer patients. Reviewers independently extracted data; random-effects meta-analyses and quality assessment were performed.
Results
Thirty-six studies were narratively synthesised. Meta-analysis was conducted using seven studies. Methodological quality was high for most studies. Study populations were heterogeneous, and the length of follow-up and risk factors varied. There was a variation in risk between different cancer types and according to stroke type: pancreatic (HR 2.85 (95% CI 2.43–3.36), ischaemic) (HR 2.28 (95% CI 1.43–3.63), haemorrhagic); lung (HR 2.33 (95% CI 1.63–3.35), ischaemic) (HR 2.14 (95% CI 1.45–3.15), haemorrhagic); and head and neck (HR 1.54 (95% CI 1.40–1.69), haemorrhagic) cancers were associated with significantly increased incidence of stroke. Risk is highest within the first 6 months of diagnosis. Narrative synthesis indicated that several studies also showed significantly increased incidence of stroke in individuals with colorectal cancer, breast cancer, ovarian cancer, nasopharyngeal cancer, leukaemia, and myeloma, and those who have received radiotherapy for head and neck cancers and platinum-based chemotherapy may also have higher stroke incidence.
Conclusions
Stroke incidence is significantly increased after diagnosis of certain cancers.
Implications for Cancer Survivors
Cardiovascular risk should be assessed during cancer survivorship care, with attention to modifying shared cancer/cardiovascular risk factors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Advances in cancer treatments have improved cancer survival in recent decades with approximately half of patients diagnosed with cancer in developed countries now expected to survive for at least 10 years [1]. The population of cancer survivors in the UK is projected to increase by approximately one million per decade from 2010 to 2040. Cancer disproportionately affects older people, almost a quarter of people aged 65 and over are cancer survivors [2]. The relationship between cancer and other major conditions thus becomes increasingly important.
Many studies have suggested that people with a history of some, but not all, cancers are at increased risk of cardiovascular disease [3]. Cancer is associated with a substantially increased 6-month risk of arterial thromboembolism, including ischaemic stroke [4,5,6,7]. Furthermore, cancer may increase the risk of early deterioration, disability, recurrent thromboembolism, and mortality after stroke [8,9,10]. Stroke risk has been shown to vary by age, gender, cancer type, histology, stage, and time after diagnosis [11] and to remain elevated for up to 10 years following cancer diagnosis [4, 12].
Any actual increased risk of stroke associated with cancer is likely to be multifactorial. Individuals with cancer may suffer strokes caused by mechanisms related to malignancy-associated prothrombotic states including changes in platelet function and increased production of neutrophil elastase traps (NETs); cardiotoxicity-associated with chemotherapeutic and radiotherapy treatments; shared risk factors; detection bias due to intensified surveillance; and underutilisation and frequent interruption of antithrombotic agents because of bleeding concerns and the potential for haemorrhagic stroke [4, 13].
Because evidence is lacking, there are currently no specific guidelines for stroke prevention, identification, or management in patients living with and beyond cancer. Currently, there is no tailored approach to preventing, managing, and treating patients with both cancer and stroke, a fact which could be worsening long-term outcomes for people with cancer. The lack of high-quality evidence to support optimal practice is likely to contribute to significant variations in clinical practice in secondary care. Optimal clinical practice in the prevention, diagnosis, and treatment of stroke in those living with and beyond cancer is crucial to improve survival and long-term outcomes.
There is a need to consolidate the evidence on the incidence of stroke in individuals living with and beyond cancer due to the potentially synergistic impact on stroke severity and disease outcomes. Our objective was to conduct a systematic review and meta-analysis of epidemiological studies comparing stroke incidence between individuals living with and beyond cancer and those without cancer (matched controls, controls from the general population, or using the general reference population of a region or country).
Methods
A systematic review was conducted to identify observational studies and randomised controlled trials (RCTs) of stroke incidence in patients living with and beyond cancer. The review was conducted according to the Cochrane Handbook and the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) statement [14]. A review protocol was registered and is available at https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=58953.
Search strategy
Keywords and Boolean operators were explored and combined on the advice of a senior medical librarian to search the electronic databases MEDLINE, CINAHL, and EMBASE. They were searched for quantitative studies published between 1946 and 2021 which explored the relationship between cancer and stroke risk. Database searches took place in 2017, 2018, 2020, and 2021. The last date of a search was 3rd February 2021. An example of the detailed search strategy is shown in Supplementary Fig. 1. Reference lists of reviews of stroke and cancer and all relevant full-text papers included in this review were searched for additional relevant titles.
Inclusion and exclusion criteria
This review considered all types of observational studies and RCTs in which ischaemic stroke, haemorrhagic stroke, or transient ischaemic stack (TIA) incidence was compared between individuals living with and beyond cancer and a control group of people never diagnosed with any cancer. Studies were eligible for inclusion if they were population-based cohort studies of adults who had received a diagnosis of cancer and had the onset of stroke or TIA as an observation endpoint. Excluded studies were other systematic reviews, case studies with less than 10 people, qualitative studies, letters, or editorials, not published in English, or focused on non-melanoma skin cancer. Excluded studies were documented with reasons for their exclusion. We initially included adult survivors of childhood cancers in the inclusion criteria but subsequently excluded these due to them being a different entity from adult-onset cancers and their heterogeneity.
Study selection
Study titles and abstracts were screened independently by three authors (MT, SD, AYO). Full texts were retrieved for all relevant abstracts and independently reviewed against the inclusion and exclusion criteria by at least two authors (MT, SD, AYO). Disagreements regarding study eligibility were resolved by discussion.
Data extraction
A data extraction form was created in Microsoft Word, and an Excel file was used to collate the extracted data. Data extracted included year of publication, cancer site, control group, age profile, primary and secondary outcomes, adjustment for covariates, handling of prior stroke, study size, and follow-up. The primary endpoint was occurrence of stroke, TIA, or cerebrovascular accident as defined by each individual study. Extraction was carried out by two reviewers (MT, RA). MT had read all the studies and compiled and reviewed all extraction forms for consistency.
Study quality assessment
Quality assessment was assessed independently by three authors (MT, RA, LW). The Newcastle–Ottawa Scale (NOS) was utilised for the quality assessment of the included studies [15]. NOS scale rates observational studies based on 3 parameters: selection of study population, comparability between the exposed and unexposed groups, and exposure/outcome assessment and follow-up. It assigns a maximum of 4 stars for selection and representativeness of patients, 2 stars for comparability between patient groups, and 3 stars for exposure/outcome assessment and follow-up. Studies with less than a total of 5 stars were considered low quality, while 5–6 stars reflected moderate quality, and more than 7 stars indicated high quality. Inter-rater reliability was assessed using Cohen’s kappa statistic, calculated on SPSS version 25 software.
Heterogeneity was assessed using visual inspection of forest plots, Cochran Q tests, and the I2 statistic as a measure for inconsistency due to chance.
Data synthesis and meta-analysis
We adopted a narrative approach to describing the number of studies, study settings, proportion of sex, mean or median age, and covariates adjusted for in each study. Our primary outcome was incidence of stroke in patients living with and beyond cancer.
For our quantitative assessment of stroke incidence in patients living with and beyond cancer, we selected the final adjusted statistical model from each article. Fully adjusted models considered a variety of confounding factors. Outcome data (hazard ratios) from included studies were entered into Review Manager version 5.3. Studies which reported hazard ratios (HR) were combined in a meta-analysis. If HRs were not provided, they were calculated manually from relevant information, e.g. estimate(beta), standard error, or confidence intervals.
Meta-analyses were performed on the log hazards of stroke incidence to provide the overall hazard ratio (HR) and confidence interval (CI) for individual cancer types (lung, pancreatic, stomach, ovarian, and head and neck) for ischaemic stroke or haemorrhagic stroke only depending on the number of studies and the data available. We chose to perform a random-effects (using the DerSimonian and Laird approach) meta-analysis of hazard ratios which account for both patient events and the time to events, and this effect estimate was measured in the largest proportion of included studies (n = 25, 70%). The control group was taken as the reference category. Statistical heterogeneity was assessed using the I2 statistics.
Results
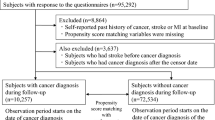
Database searches
A flow diagram of the study selection process is presented in Fig. 1. We carried out searches in 2017, 2018, and 2020 and updated the search on 3rd February 2021. A total of 5784 articles were identified from database searches. A total of 454 abstracts were screened, and 259 full-text articles were assessed, of which 36 satisfied the eligibility criteria and were included in the systematic review.
Definitions of stroke
Multiple definitions of stroke were used (Supplementary Table 1). The majority of these (n = 26) were based on ICD-9-CM and ICD-10 codes. Two studies were not clear on their definition of stroke (28, 33).
Characteristics of included studies
An overview of the characteristics of the studies included in the analysis is presented in Table 1.
Eleven of the studies were conducted in Taiwan using the Taiwan National Health Insurance Research Database [19,20,21, 23, 24, 29, 30, 32, 43, 47, 48] with the remaining studies being conducted in Northern European countries and North America. One study was conducted worldwide in 40 countries [34]. The process yielded a total of 2,226,660 cancer patients.
A variety of cancer types were studied: four prostate [36, 37, 39, 44], three cervical [19, 33, 43], three head and neck [23, 26, 27], three breast [12, 28, 45], two lung [21, 46], two gastric [30, 38], two ovarian [22, 29], two nasopharyngeal [24, 32], and one each of endometrial [40], oral [48], pancreatic [20], Hodgkin’s lymphoma [25], non-Hodgkin’s lymphoma [35], testicular [31], and thyroid [42]. Eight studies evaluated multiple cancer types [4, 6, 16,17,18, 34, 41, 47]. If not using the general country population as the control group, most studies matched cancer cases with non-cancer cases on age and sex as a minimum.
Studies adjusted for a variety of covariates, the most common being age, sex, and comorbidities. Smoking and cancer treatment received were not consistently adjusted for.
Prior stroke was excluded in 23 studies. Four studies adjusted for prior stroke in their analysis [16, 18, 34, 37]. Nine studies did not state or where not clear on whether they had accounted for prior stroke in analysis [4, 6, 26,27,28, 32, 33, 40, 44].
Most studies (n = 27) did not have any lag period from cancer diagnosis to stroke incidence, and there was a range of duration of follow-up time across the studies.
Stroke incidence
Narrative summary of studies
Across all 36 studies, stroke incidence was expressed using different statistical measures of association, including hazard ratios, incidence rate ratios, standardised incidence ratios, risk ratios, or odds ratios. Several studies reported a combination of association measures. The outcome of stroke incidence according to a categorisation of follow-up time or cancer treatment type was also reported [4, 24, 31, 36, 40, 45, 46].
Of the 28 studies looking at individual cancers and the incidence of stroke, 21 reported an increased incidence of stroke following cancer diagnosis compared to the control group. Seven studies reported a reduced incidence of stroke in individuals with cancer compared to controls (two studies of cervical cancer [19, 33], two of prostate cancer [36, 39], and one each of breast [28], gastric [38], and testicular cancers [31]).
Influence of cancer type on stroke incidence
Of eight studies looking at either all cancer types or a specific variety of different cancer types [4, 6, 16,17,18, 34, 41, 47], the incidence of stroke varied across different cancers. Adelborg et al. investigated haematological cancers and showed that the incidence of stroke was increased in those living with and beyond multiple myeloma, myeloproliferative neoplasms, Hodgkin lymphoma, and myelodysplastic syndrome when compared with the general population [16]. Armenian et al. showed that risk of stroke was increased in those living with and beyond ovarian cancer and lung cancer and was decreased among prostate cancer [17]. The risk of ischaemic stroke was increased for patients with lung, colon, bladder, rectal, or pancreatic cancer in Andersen et al., while haemorrhagic stroke risk was only significantly increased in patients with lung cancer [18].
Navi et al. looked at patients with a diagnosis of breast, colorectal, lung, pancreatic, or prostate cancer; cumulative incidence rates of stroke were higher in all cancer groups compared with matched controls. These were most pronounced for lung, pancreatic, and colorectal cancer patients [4]. Strongman et al. showed increased risk of stroke in eight out of 20 cancers compared to controls from the general population. These were oral, pancreas, lung, cervical, CNS, non-Hodgkin’s lymphoma, multiple myeloma, and leukaemia [41]. Wei et al. combined a range of cancers (colorectal, lung, urogenital, gastric, prostate, breast, brain, oesophageal, nasopharyngeal, ovarian, thyroid, hepatocellular carcinoma, leukaemia, and lymphoma) and showed that there was an increased risk of stroke within the year after cancer diagnosis [47]. Risk of ischaemic stroke was increased after cancer diagnosis in 20 of 34 cancers studied by Zoller et al. [6]. This risk was more than two times greater for small intestine, pancreas, lung, nervous system, endocrine glands, and leukaemia. The risk of haemorrhagic stroke was increased in 18 of the 34 cancers studied. This was greatest for small intestine, liver, kidney, nervous system, thyroid gland, endocrine glands, connective tissue, non-Hodgkin lymphoma, myeloma, and leukaemia. The only RCT included found no association between cancer cases and non-cancer cases and the incidence of stroke [34].
Influence of cancer treatment on stroke incidence
Twenty-one studies investigated cancer treatment and its association with incidence of stroke (Supplementary Table 2). Stroke risk was highest in patients receiving both radiotherapy and chemotherapy in head and neck cancer [23] compared with no treatment or singular treatment. Patients treated with neck irradiation together with mediastinal irradiation experienced a statistically significant increased risk for ischemic stroke compared with those treated with chemotherapy or infradiaphragmatic irradiation alone in a study of Hodgkin lymphoma survivors [25]. Non-Hodgkin lymphoma survivors treated with chemotherapy also had increased incidence of stroke compared to the general population [41]. Ischaemic stroke incidence rates were significantly higher in nasopharyngeal cancer patients after radiotherapy, radiotherapy/chemotherapy, and non-radio/chemotherapy than in the reference control population. Those receiving radiotherapy/chemotherapy had the highest incidence followed by those receiving radiotherapy only [24]. Incidence of stroke was increased in lung cancer survivors following singular treatment with radiotherapy or chemotherapy in addition to both chemotherapy and radiotherapy [41]. Cisplatin-based and carboplatin-based chemotherapy regimes for ovarian cancer were independent risk factors for ischaemic stroke, whereas non-platinum-based regimens were not [29]. Those within a palliative treatment regimen for prostate cancer had increased risk for ischaemic stroke [36], whereas stroke incidence was higher in those treated with endocrine therapy for prostate cancer [39, 44]. In one study for prostate cancer, only gonadotrophin-releasing hormone agonists resulted in an increased incidence of stroke [37]. In oral cancer patients, stroke incidence was highest in those treated with radiotherapy/chemotherapy/concurrent chemoradiotherapy compared to those treated with surgery alone [48]. Risk of stroke did not differ between breast cancer patients who were treated with surgery alone and those who received radiotherapy in combination with surgery. However, among patients who were treated with radiotherapy plus hormone therapy, an elevated risk of stroke was observed compared with the general population [28]. For patients with testicular cancer, risks for stroke were investigated in patients undergoing surveillance, radiotherapy, or bleomycin-etoposide-cisplatin (BEP) treatment. Only patients receiving BEP had an increased risk of cerebrovascular accident incidence in the year following treatment [31].
Influence of time since cancer diagnosis and stroke incidence
Follow-up time was categorised in seventeen studies in relation to the outcome of stroke incidence (Supplementary Table 3). For breast, colorectal, lung, pancreatic, and prostate cancer, stroke risk was greatest in the first month following cancer diagnosis, and that risk attenuated over time and was generally no longer present beyond 1 year in one study [4]. In other studies, this risk remained elevated for up to 10 years following cancer diagnosis [6, 12, 20, 41]. Zoller et al. showed that the standardised incidence ratios (SIR) for ischaemic stroke and haemorrhagic stroke increased during the first 6 months after diagnosis in 23 and 15 of 34 cancers, respectively [6]. It decreased thereafter but remained relatively constant after 6 months. A high incidence of both ischaemic and haemorrhagic stroke was observed within 6 months after diagnosis in a pancreatic cancer cohort; this declined with time and was no longer significant 24 months after the cancer diagnosis [20]. Risk of stroke for those with lung cancer was highest during the first 3 months for men and within 4 to 6 months for women and, then, decreasing over 1 year of follow-up for men and 2 years of follow-up for women [21]. Incidence rates for stroke in women with ovarian cancer were over two times higher than cancer-free women 3 months after cancer diagnosis and decreased but still elevated by 12 months [22].
People living with and beyond head and neck cancers had a consistently elevated stroke incidence over 8 years from cancer diagnosis [23, 26]. Hodgkin lymphoma patients experienced an approximately twofold increased SIR for stroke risk compared to the general population with no increasing or decreasing trends with longer follow-up time [25]. Non-Hodgkin lymphoma patients also had increased incidence of stroke which continued for over 10 years following diagnosis [6, 16, 41]. Increased stroke risk was seen in patients receiving BEP treatment for testicular cancer in the year following diagnosis; however, this risk decreased and was no longer significant after 1 year [31]. Nilsson et al. observed a 22% increase in the risk of stroke in the first year after breast cancer diagnosis. By 1 to 5 years, there was no significant increase, but then, an increase was observed again after 5 to 10 years of follow-up and after greater than 10 years of follow-up [12]. Soisson et al. followed patients from 1 year after endometrial cancer diagnosis, and there was no significantly increased risk for stroke between 1 to 10 years from cancer diagnosis [40]. In breast cancer patients, stroke incidence was increased, but this did not reach significance over three time periods (0 to 6 month, 6 to 12 month, or 12-month to total follow-up) from diagnosis [45]. In another study by van Herk-Sukel et al., there was a trend towards increased incidence in the 0 to 6 months following lung cancer diagnosis [46].
Influence of smoking and stroke incidence in individuals living with and beyond cancer
Smoking status and incidence of stroke in individuals living with and beyond cancer in comparison to the matched general population cohort were investigated in three studies [26, 35, 41] (Supplementary Table 4). Strongman et al. showed an increased incidence of stroke in survivors with non-Hodgkin lymphoma, lung, breast, or leukaemia who had ever smoked compared with the general population cohort [41]. No association was observed in survivors with colorectal, malignant melanoma, uterine, prostate, or bladder cancer [41]. Dorresteijn et al. observed an increased stroke risk in both non-smokers and smokers living with and beyond head and neck cancer in comparison with the general population [26]. Smoking status had no association with an increased incidence of stroke in those with non-Hodgkin lymphoma [35].
The association between cancers related to smoking and increased stroke risk was investigated in two studies [6, 18] (Supplementary Table 4). Andersen et al. grouped cancers into those strongly associated with smoking (lung, colon, bladder, rectum, pancreas, kidney, stomach, and head and neck) and those less strongly associated with smoking (non-Hodgkin lymphoma, breast, prostate, melanoma, CNS, ovary, and endometrial). They found that the risk of ischemic and haemorrhagic stroke was increased for all smoking-related cancers combined but not non-smoking-related cancers [18]. In another study, several non-smoking-related cancers were associated with an increased risk of haemorrhagic and ischaemic strokes [6]; these included small intestine, colon, rectum, breast, endometrium, ovary, other female genital, prostate, melanoma, nervous system, endocrine glands, connective tissue, non-Hodgkin lymphoma, and myeloma. This risk declined rapidly after 6 months but remained raised for 10 or more years [6].
Several other studies within the review looked at smoking and increased stroke risk but only within the cohort of cancer patients [25, 28, 38, 42] (Supplementary Table 4). Only one of these studies into thyroid cancer found an increased risk of stroke incidence in current smokers [42]; the others found no association.
Meta-analysis
Twenty-five of the included studies calculated hazard ratios for the incidence of stroke. The HR estimates for stroke incidence in all cancer types ranged from 0.25 to 7.43 (Table 2 and Fig. 2). Seven studies were included in the meta-analysis for individual cancer types (lung, pancreatic, stomach, ovarian, head and neck) (Fig. 3). Overall pooled HR of ischaemic stroke incidence was significant for lung cancer (HR 2.33, 95% CI 1.63–3.34) and pancreatic cancer (HR 2.85, 95% CI 2.43–3.34). For haemorrhagic stroke, the overall pooled HR remained significant for lung cancer (HR 2.14, 95% CI 1.45–3.15), pancreatic cancer (HR 2.28, 95% CI 1.43–3.63) and was also significant for head and neck cancer (HR 1.54 (95% CI 1.40–1.69). Pooled HR were not significant for either ischaemic stroke only for stomach cancer, head and neck cancer, and ovarian cancer (Fig. 3). Between-study variation was high for stomach cancer, lung cancer, head and neck cancer, and ovarian cancer when looking at ischaemic stroke.
In the remaining 11 studies, other measures of stroke incidence were used. Supplementary Table 5 shows the incidence rate ratio for stroke in four studies, where most cancer types within the studies showed an increased rate ratio. Six studies (Supplementary Table 6 ) calculated SIR, two of the studies reported SIRs of less than 1, whereas the remaining studies had SIRs of greater than 1. Two studies (Supplementary Table 7 ) reported odds ratios which were greater than 1; however, the 95% confidence interval included 1. Pooled ratios were not possible due to there being only one estimate per cancer type across all of the studies.
Quality assessment/risk of bias
Median quality score was 7 with a range of 5 to 9 (Table 3). There were five studies with a score of 5 or 6; however none of these formed part of the meta-analysis as they did not report hazard ratios. The low scores were mainly due to inadequacy of the follow-up period of the patient cohorts, lack of adjustment for additional factors in the comparability of the patient cohorts, and no demonstration that participants had not had a stroke prior to the start of the study. Only five out of the 36 studies were adjusted for smoking in the analysis which may be an important risk factor for stroke incidence.
A comparison of scorings was undertaken, and the kappa statistic was in strong agreement of 0.61.
Discussion
Principal findings
Meta-analysis of observational studies shows that individuals living with and beyond cancer had a higher incidence of stroke than demographically similar individuals who have not been diagnosed with cancer. The risk of ischaemic stroke is significantly higher in those with lung cancer (2 studies, HR 2.33, 95% CI 1.63–3.35), pancreatic cancer (2 studies, HR 2.85, 95% CI 2.43–3.36), and haemorrhagic stroke in those with lung cancer (2 studies, HR 2.14, 95% CI 1.45–3.15), pancreatic cancer (2 studies, HR 2.28, 95% CI 1.43–3.63), and head and neck cancer (2 studies, HR 1.54, 95% CI 1.40–1.69) compared to controls. No statistically significant increase in stroke incidence was observed in individuals with stomach cancer or ovarian cancer. In the narrative synthesis, several studies also showed significantly increased incidence of stroke in individuals with colorectal cancer, breast cancer, ovarian cancer, nasopharyngeal cancer, thyroid cancer, leukaemia, and myeloma [4, 6, 16, 18, 24, 25, 29, 32, 41, 42]. Narrative synthesis identified that the relationship between stroke incidence and cancer is not a simple one. Cancer type, time since diagnosis of cancer, the types of anti-cancer treatments received, and shared risk factors such as smoking can all influence the risk of stroke after cancer.
Comparison with existing literature
Earlier reviews have also noted increased incidence of stroke in cancer patients. A recent meta-analysis has shown that the overall relative risk for stroke in cancer patients was 1.66 (95% CI 1.35–2.04) [54]. This study included childhood cancers and pooled effects of association together, including SMR, and only identified 20 cohort studies as opposed to our 35 observational studies and one RCT. Previous reviews have also hinted that treatment type is important, with increased incidence of stroke noted in individuals receiving androgen deprivation therapy for prostate cancer, tamoxifen treatment for breast cancer, and radiotherapy in several different cancers [49,50,51,52]. The time between cancer diagnosis and incident stroke was discussed by Navi et al. in a narrative review of arterial thromboembolism and cancer [53]. The authors hypothesised that a “U”-shaped curve might exist, in which stroke risk is highest soon after diagnosis due to cancer-mediated hypercoagulability and then decreases as cancer is controlled by treatment, before increasing again in the long-term due to late effects of cancer treatment (particularly radiotherapy).
Potential mechanisms of increased stroke incidence after cancer
Several mechanisms, alone or together, may account for the increased risk of stroke in patients with cancer. Stroke risk has been shown to directly correlate with cancer stage, with stage 4 cancers demonstrating the highest risks [4, 6] including a more than tenfold increased risk in the first month after cancer diagnosis [5] indicating that both tumour burden (tumour emboli, vessel compression, or infiltration) and cancer-associated coagulopathy can underlie or enhance the occurrence of stroke in cancer patients. In our meta-analysis, lung and pancreatic cancer, which are known to be diagnosed at a later stage [55], showed significantly increased risk of stroke. Brain imaging studies have revealed that cancer patients with stroke often exhibit multiple arterial territorial involvements, suggesting an embolic origin, compared with the single infarct seen in those with conventional stroke risks [56].
Hypercoagulability associated with tumour proliferation may also contribute to the increased risk of stroke in cancer patients [25]. Follow-up times varied between the studies in this review; however, stroke risk among cancer survivors has been shown to be highest soon after diagnosis [12, 18] and declines over time [4, 6, 20, 21, 46]. This perhaps reflects a decreased tumour burden after treatment intervention, cessation of cytostatic agents (decreased chemotherapy-related complications), or death-related selective bias in the cancer group on the risk of stroke. Some studies showed that risk was consistent over time, and this may be related to the type of cancer; head and neck [23], Hodgkin lymphoma [25], and breast [45], or that risk declined and then increased again with breast cancer [12].
Increased stroke risk in cancer patients could also be a consequence of several cancer treatments. Studies have reported that platinum-based chemotherapy and angiogenesis inhibitors increase the risk of stroke [57,58,59]. This may occur because chemotherapy releases microparticles from cancer cells, which enhance thrombin generation [60]. In addition, radiotherapy can cause vasculopathy through accelerated atherosclerosis or other mechanisms, which can then precipitate stroke [61,62,63]. Several studies within this review looked at stroke incidence risk in relation to cancer treatment. Strongman’s analysis suggests cancer treatments, particularly chemotherapy, are likely to play a more prominent role than shared risk factors such as smoking or excess weight.
Patients with cervical cancer had decreased risk of stroke compared with the reference population [19]. It is suggested that supplementation of oestrogen after cancer treatment could explain this finding as hormone therapy has beneficial cardiovascular effects [64, 65]. A 45.5% of patients with cervical cancer took oestrogen supplementation compared with 15.5% in the control group. Several other studies, however, suggest increased cardiovascular morbidity following radiotherapy or chemoradiation in patients with cervical cancer [33, 43, 66]. Tsai et al. used the same database as Chang et al. to look at cervical cancer but in a group of patients who had radiotherapy treatment [43]. Patients who received radiation therapy as part of their cervical cancer treatment had a higher risk of ischaemic stroke compared with the general population. Radiotherapy in cervical cancer patients may induce systemic vascular damage that contributes to risk of stroke [67].
Hypertension and diabetes mellitus are predictors of ischemic stroke that remain significant into old age and have been shown to be risk factors in various cancer patients. Comorbidities in general may increase stroke risk much more for cancer patients than for controls. Cancer patients with diabetes, atrial fibrillation, or hypertension were at greater risk of stroke than those without [20, 29. 30, 40, 43]. In addition, cancer patients may be less likely to have primary and secondary stroke prevention.
Strengths and limitations
Our review comprehensively demonstrates that adult cancer patients are at increased risk of stroke. It provides up-to-date results of the effect of cancer on the higher risk of stroke incidence by synthesising a number of published studies (n = 36). The study yielded a large population of individuals from countries in Asia, Europe, and North America.
We have focussed on adult cancers which we believe is a strength as the cancer types that develop in children differ in underlying pathology, behaviour, and treatment outcome compared to the much more commonly occurring tumours of middle and old age. Unlike many adult cancers, childhood cancers are not strongly linked to lifestyle or environmental risk factors, and long-term side effects are more of a concern. Different treatment protocols are used, and certain cancer treatments in childhood have moderate-to-severe late effects that require treatment and affect quality of life.
We chose to perform meta-analysis only on HR which account for both patient events and the time to events. Odds ratios or relative risks that measure only the number of events and take no account of when they occur are appropriate only for measuring dichotomous outcomes. Using such measures in a meta-analysis of time-to-event outcomes can pose problems and results in an estimate that is unreliable and difficult to interpret. Bias can also arise if the time points have been subjectively chosen.
The major limitation of this review is the high heterogeneity between the included studies. The review has brought together research conducted in different countries using different methodological approaches and with different follow-up times. All the studies identified are from the developed world. There were a substantial number of studies carried out in Taiwan (n = 11) all using the same research database, although these all investigated different cancer types. There was a range of different cancer types in the review with most studies focusing on survivors of a single, organ-specific cancer. There were eight studies looking at multiple cancer types.
The risk of stroke in those living with and beyond cancer is likely to be multifactorial and this review is limited in being able to distinguish between stroke caused by mechanisms related to cancer versus spontaneous non-cancer-related complications. Studies within this review generally used a retrospective matched cohort design using research databases or hospital databases to determine their patient cohort. They are therefore constrained and dependent on the quality of the collected data. Potential confounding variables that may account for some of the observations have not been included in analysis or may not have been collected within the research or hospital databases which may have led to biased estimates. Cancer and stroke share some common pathophysiological pathways and share several risk factors, including age, smoking, and obesity. Most studies within this review matched on age, sex, and specific individual comorbidities; however, many studies have stated that the limitations of their work are the absence of behavioural factors and lifestyle variables. Only five of the 30 studies adjusted for smoking. Although one study within the review showed a higher risk of ischemic and haemorrhagic stroke for cancers strongly associated with smoking [18], another study found that several non-smoking-related cancers were also associated with an increased risk of both stroke sub-types [6]. This risk declined rapidly after 6 months but remained raised for 10 or more years [6]. Several other studies within the review looked at smoking and increased stroke risk only within the cohort of cancer patients and found no association [25, 28, 38]. Smoking as a risk factor is unlikely to fully explain the association between cancer and stroke.
This review cannot account for effects of different socioeconomic status, racial differences, and country-specific treatment differences. Most studies did not include details on cancer stage, cancer treatment, or adjust for this in the analysis. There was also a lack of comprehensive clinical information on surgical intervention, dosage and location of radiotherapy, treatment duration and regimen of chemotherapy, and laboratory data in most studies within the review. Further research should explore these factors in detail.
Implications and further research
This review presents strong evidence that patients with cancer are at increased risk of stroke. Stroke risk is particularly increased in individuals with leukaemia, myeloma, lung cancer, and pancreatic cancer. In addition to cancer type, cancer treatment is an important modifier of stroke risk; for example, those who have received platinum-based chemotherapy or who have received radiotherapy for head and neck cancer are at significantly increased risk of stroke. Further research is needed to explore mechanisms and provide specific guidance on how to minimise stroke risk in the growing population of cancer survivors. This includes studies on routinely collected data to explore behavioural and lifestyle factors, cancer stage, and treatment, prospective studies to identify biomarkers that can reliably predict first and recurrent stroke in cancer patients, translational studies to elucidate the mechanisms of these strokes, and clinical trials to identify the best strategies to prevent and acutely treat cerebrovascular events in the cancer population.
There is not yet sufficient evidence to provide a comprehensive patient-centred risk assessment tool for stroke that could be used in clinical settings with those living with and beyond cancer. Nonetheless, ensuring awareness of the link is important for both patients and clinicians, so that risk factors can be identified and modified. This review highlights the potential to use routinely collected healthcare data to develop and test new stroke risk calculators for individuals living with and beyond cancer. While there is not yet sufficient evidence to provide a comprehensive patient-centred risk assessment tool to use in clinical settings, clinicians should be aware that cancer can increase stroke risk and should use cancer care reviews as an opportunity to routinely discuss and address these modifiable risk factors for cardiovascular disease.
Primary prevention of cardiovascular diseases through the targeted management of modifiable risk factors such as hypertension, hypercholesterolaemia, diabetes, and lifestyle modification has been one of the major public health successes of the late twentieth century. However, current risk stratification tools such as QRISK and Framingham do not consider cancer or cancer treatment. More aggressive management of risk factors such as hypertension, obesity, and diabetes in cancer patients is needed. Patients with newly diagnosed malignancy should be routinely assessed and considered for antithrombotic and statin medicines for the primary prevention of cardiovascular disease. Given that patients with cancer are also prone to bleeding due to frequent coagulopathy and invasive procedures, carefully designed clinical trials are also needed to answer these questions.
This review highlights the need to use routinely collected healthcare data to develop and test new stroke risk calculators for individuals living with and beyond cancer and the need for clinical trials of primary prevention in individuals identified to be at high risk. Even with the limitations reported here, the development of comprehensive, evidence-based, national-level guidance on stroke in cancer survival care should be prioritised to optimise the care of this patient group.
Conclusions
In conclusion, there is evidence that stroke incidence is significantly increased in those living with and beyond certain cancers. There is substantial heterogeneity between studies, and further research is needed to explore the mechanisms. Cardiovascular risk should be assessed during cancer survivorship care, with attention to modifying shared cancer/cardiovascular risk factors.
Data availability
The data used and analysed during this study are available from the corresponding author.
Code availability
Not applicable.
References
Cancer Research UK. Cancer statistics for the UK. 2019. https://www.cancerresearchuk.org/health-professional/cancer-statistics-for-the-uk. Accessed 20 Aug 2020.
Maddams J, Utley M, Møller H. Projections of cancer prevalence in the United Kingdom, 2010–2040. Br J Cancer. 2012;107:1195–202.
Schoormans D, Vissers PAJ, van Herk-Sukel MPP, Denollet J, Pedersen SS, Dalton SO, et al. Incidence of cardiovascular disease up to 13 years after cancer diagnosis: a matched cohort study among 32757 cancer survivors. Cancer Med. 2018;7:4952–63.
Navi BB, Reiner AS, Kamel H, Iadecola C, Elkind MSV, Panageas KS, et al. Association between incident cancer and subsequent stroke. Ann Neurol. 2015;77:291–300.
Navi BB, Reiner AS, Kamel H. Risk of arterial thromboembolism in patients with cancer. J Am Coll Cardiol. 2017;70:92–938.
Zoller B, Ji J, Sundquist J, Sundquist K. Risk of haemorrhagic and ischaemic stroke in patients with cancer: a nationwide follow-up study from Sweden. Eur J Cancer. 2012;48:1875–83.
Zoller B, Ji J, Sundquist J, Sundquist K. Risk of coronary heart disease in patients with cancer: a nationwide follow-up study from Sweden. Eur J Cancer. 2012;48:121–8.
Kneihsl M, Enzinger C, Wünsch G, Khalil M, Culea V, Urbanic-Purkart T, et al. Poor short-term outcome in patients with ischaemic stroke and active cancer. J Neurol. 2016;263:150–6.
Kim J-M, Jung K-H, Park KH, Lee S-T, Chu K, Roh J-K. Clinical manifestation of cancer-related stroke: retrospective case-control study. J Neurooncol. 2013;111:295–301.
Cutting S, Wettengel M, Conners JJ, Ouyang B, Busl K. Three-month outcomes are poor in stroke patients with cancer despite acute stroke treatment. J Stroke Cerebrovasc Dis. 2017;26:809–15.
Zaorsky NG, Zhang Y, Tchelebi LT, Mackley HB, Chinchilli VM, Zacharia BE. Stroke among cancer patients. Nat Commun. 2019. https://doi.org/10.1038/s41467-019-13120-6.
Nilsson G, Holmberg L, Garmo H, Terent A, Blomqvist C. Increased incidence of stroke in women with breast cancer. Eur J Cancer. 2005;41:423–9.
Dearborn JL, Urrutia VC, Zeiler SR. Stroke and cancer – a complicated relationship. J Neurol Transl Neurosci. 2014;2:1039.
Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network metaanalyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162:777–84. https://doi.org/10.7326/M14-2385.
Institute OHR. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed date 13 Mar 2020.
Adelborg K, Corraini P, Darvalics B, Frederiksen H, Ording A, Horváth-Puhó E, et al. Risk of thromboembolic and bleeding outcomes following hematological cancers: a Danish population-based cohort study. J Thromb Haemost. 2019;17:1305–18.
Armenian SH, Xu L, Ky B, Sun C, Farol LET, Pal SK, et al. Cardiovascular disease among survivors of adult-onset cancer: a community-based retrospective cohort study. J Clin Oncol. 2016;34:1122–30.
Andersen KK, Olsen TS. Risk of ischemic and hemorrhagic strokes in occult and manifest cancers. Stroke. 2018;49:1585–92.
Chang W-C, Muo C-H, Chang S-N, Sung F-C, Chang Y-J, Kao C-H. A nationwide population-based retrospective cohort study: decreased risk of stroke in cervical cancer patients after receiving treatment. Arch Gynecol Obstet. 2013;288:867–71.
Chan P-C, Chang W-L, Hsu M-H, Yeh C-H, Muo C-H, Chang K-S, et al. Higher stroke incidence in the patients with pancreatic cancer. A nation-based cohort study in Taiwan. Medicine. 2018;97:11.
Chen P-C, Muo C-H, Lee Y-T, Yu Y-H, Sung F-C. Lung cancer and incidence of stroke. A population-based cohort study. Stroke. 2011;42:3034–9.
Chia VM, O’Malley CD, Danes MD, Lindquist KJ, Gleeson ML, Kelsh MA, et al. Prevalence and incidence of comorbidities in elderly women with ovarian cancer. Gynecol Oncol. 2013;129:346–52.
Chu C-N, Chen S-W, Bai L-Y, Mou C-H, Hsu CY, Sung F-C. Increase in stroke risk in patients with head and neck cancer: a retrospective cohort study. Br J of Cancer. 2011;105:1419–23.
Chu C-N, Chen P-C, Bai L-Y, Muo C-H, Sung F-C, Chen S-W. Young nasopharyngeal cancer patients with radiotherapy and chemotherapy are most prone to ischaemic risk of stroke: a national database, controlled cohort study. Clin Otolaryngol. 2013;38:39–47.
De Bruin ML, Dorresteijn LDA, van’t Veer MB, Krol ADG, van der Pal HJ, Kappelle AC, et al. Increased risk of stroke and transient ischaemic attack in 5-year survivors of Hodgkin lymphoma. J Natl Cancer Inst. 2009;101:928–37.
Dorresteijn LDA, Kappelle AC, Boogerd W, Klokman WJ, Balm AJM, Keus RB, et al. Increased risk of ischemic stroke after radiotherapy on the neck in patients younger than 60 years. J Clin Oncol. 2002;20:282–8.
Haynes JC, Machtay M, Weber RS, Weinstein GS, Chalian AA, Rosenthal DI. Relative risk of stroke in head and neck carcinoma patients treated with external cervical irradiation. Laryngoscope. 2002;122:1883–7.
Hooning MJ, Dorresteijn LDA, Aleman BMP, Kappelle AC, Klijn JGM, Boogerd W, et al. Decreased risk of stroke among 10-year survivors of breast cancer. J Clin Oncol. 2006;24:5388–94.
Kuan A-S, Teng C-J, Wu H-H, Su VY-F, Chen Y-T, Chien S-H, et al. Risk of ischemic stroke in patients with ovarian cancer: a nationwide population-based study. BMC Med. 2014;12:53.
Kuan A-S, Chen S-C, Yeh C-M, Hung M-H, Hung Y-P, Chen T-J, et al. Risk of ischemic stroke in patients with gastric cancer. A nationwide population-based cohort study. Medicine. 2015;94:e1336.
Lauritsen J, Hansen MK, Bandak M, Kreiberg MB, Skøtt JW, Wagner T, et al. Cardiovascular risk factors and disease after male germ cell cancer. J Clin Oncol. 2019;38:584–92.
Lee C-C, Su Y-C, Ho H-C, Hung S-K, Lee M-S, Chiou W-Y, et al. Increased risk of ischemic stroke in young nasopharyngeal carcinoma patients. Int J Radiation Oncology Biol Phys. 2011;81:e833–8.
Maduro JH, Den Dekker HA, Pras E, De Vries EG, Van der Zee AG, Klokman WJ, et al. Cardiovascular morbidity after radiotherapy or chemoradiation in patients with cervical cancer. Int J Radiation Oncology Biol Phys. 2010;78:1337–44.
Melloni C, Dunning A, Granger CB, Thomas L, Khouri MG, Garcia DA, et al. Efficacy and safety of apixaban versus warfarin in patients with atrial fibrillation and a history of cancer: insights from the ARISTOTLE Trials. Am J Med. 2017;130:1440–8.
Moser EC, Noordijk EM, van Leeuwen FE, le Cessie S, Baars JW, Thomas J, et al. Long-term risk of cardiovascular disease after treatment for aggressive non-Hodgkin lymphoma. Blood. 2006;107:2912–9.
Moutsten IR, Larsen SB, Dunn-Henriksen AK, Tjønneland A, Kjaer SK, Brasso K, et al. Risk of cardiovascular events in men treated for prostate cancer compared with prostate cancer-free men. Br J of Cancer. 2019;120:1067–74.
Robinson D, Garmo H, Lindahl B, Van Hemelrijck M, Adolfsson J, Bratt O, et al. Ischemic heart disease and stroke before and during endocrine treatment for prostate cancer in PCBaSe Sweden. Int J Cancer. 2012;130:478–87.
Shin DW, Suh B, Park Y, Lim H, Suh Y-S, Yun JM, et al. Risk of coronary heart disease and ischemic stroke incidence in gastric cancer survivors: a nationwide study in Korea. Ann Surg Oncol. 2018;25:3248–56.
Shin DW, Han K, Park HS, Lee S-P, Park SH, Park J. Risk of ischemic heart disease and stroke in prostate cancer survivors: a nationwide study in South Korea. Nat Sci Rep. 2020;10:10313. https://doi.org/10.1038/s41598-020-67029-y.
Soisoon S, Ganz PA, Gaffney D, Rowe K, Snyder J, Wan Y, et al. Long-term cardiovascular outcomes among endometrial cancer survivors in a large population-based cohort study. J Natl Cancer Inst. 2018;110:1342–51.
Strongman H, Gadd S, Matthews A, Mansfiled KE, Stanway S, Lyon AR, et al. Medium and long-term risks of specific cardiovascular diseases in survivors of 20 adult cancers: a population-based cohort study using multiple linked UK electronic health records databases. Lancet. 2019;394:1041–54.
Suh B, Shin DW, Park Y, Lim H, Yun JM, Song SO, et al. Increased cardiovascular risk in thyroid cancer patients taking levothyroxine: a nationwide cohort study in Korea. Eur J Endocrinol. 2019;180:11–20.
Tsai S-J, Hunang Y-S, Tung C-H, Lee C-C, Lee M-S, Chiou W-Y, et al. Increased risk of ischemic stroke in cervical cancer patients: a nationwide population-based study. Radiat Oncol. 2013;8:41.
Van Hemelrijck M, Garmo H, Holmberg L, Ingelsson E, Bratt O, Bill-Axelson A, et al. Absolute and relative risk of cardiovascular disease in men with prostate cancer: results from the population-based PCBaSe Sweden. J Clin Oncol. 2010;28:3448–56.
Van Herk-Sukel MPP, Shantakumar S, Kamphuisen PW, Penning-van Beest FJA, Herings RMC. Myocardial infarction, ischaemic stroke, and pulmonary embolism before and after breast cancer hospitalisation. Thromb Haemost. 2011;106:149–55.
Van Herk-Sukel MPP, Shantakumar S, Penning-van Beest FJA, Kamphuisen PW, Majoor CJ, Overbeek LIH, et al. Pulmonary embolism, myocardial infarction and ischemic stroke in lung cancer patients: results from a longituidinal study. Lung. 2013;191:501–9.
Wei Y-C, Chen K-F, Wu C-L, Lee T-W, Liu C-H, Shyu Y-C, et al. Stroke rate increases around the time of cancer diagnosis. Front Neurol. 2019;10:579.
Wu Y-T, Chen C-Y, Lai W-T, Kuo C-C, Hunag Y-B. Increasing risks of ischemic stroke in oral cancer patients treated with radiotherapy or chemotherapy: a nationwide cohort study. Int J Neurosci. 2015;125:808–16.
Meng F, Zhu S, Zhao J, Vados L, Wang L, Zhao Y, et al. Stroke related to androgen deprivation therapy for prostate cancer: a meta-analysis and systematic review. BMC Cancer. 2016;16:180.
Liu R, Zhou J, Xia S, Li T. Androgen deprivation therapy and the risk of stroke in patients with prostate cancer: an updated systematic review and meta-analysis. Urol Int. 2020;104:214–21.
Bushnell CD, Goldstein LB. Risk of ischemic stroke with tamoxifen treatment with breast cancer: a meta-analysis. Neurology. 2004;63:1230–3.
Huang R, Zhou Y, Hu S, Ren G, Cui F, Zhou P-K. Radiotherapy exposure in cancer patients and subsequent risk of stroke: a systematic review and meta-analysis. Front Neurol. 2019;10:233.
Navi BB, Iadecola C. Ischemic stroke in cancer patients: a review of an underappreciated pathology. Ann Neurol. 2018;83:873–83.
Zhang F, Wang K, Du P, Yang W, He Y, Li T, et al. Risk of stroke in cancer survivors: a meta-analysis of population-based cohort studies. Neurology. 2021;96:e513–26.
http://www.ncin.org.uk/publications/survival_by_stage. Accessed 8 Mar 2021.
Kim SG, Hong JM, Kim HY, Lee J, Chung P-W, Park K-Y, et al. Ischemic stroke in cancer patients with and without conventional mechanisms: a multicentre study in Korea. Stroke. 2010;41:798–801.
Li SH, Chen WH, Tang Y, Rau K-M, Chen Y-Y, Huang T-L, et al. Incidence of ischemic stroke post-chemotherapy: a retrospective review of 10,963 patients. Clin Neurol Neurosurg. 2006;108:150–6.
Zuo P-Y, Chen X-L, Liu Y-W, Xiao C-L, Liu C-Y. Increased risk of cerebrovascular events in patients with cancer treated with bevacizumab: a meta-analysis. PLoS ONE. 2014;9:e102484.
Ranpura V, Hapani S, Chuang J, Wu S. Risk of cardiac ischemia and arterial thromboembolic events with the angiogenesis inhibitor bevacizumab in cancer patients: a meta-analysis of randomized controlled trials. Acta Oncol. 2010;49:287–97.
Lysov Z, Dwivedi DJ, Gould TJ, Liaw PC. Procoagulant effects of lung cancer chemotherapy: impact on microparticles and cell-free DNA. Blood Coagul Fibrinolysis. 2017;28:72–82.
El-Fayech C, Haddy N, Allodji RS, Veres C, Diop F, Kahlouche A, et al. Cerebrovascular diseases in childhood cancer survivors: role of the radiation dose to Willis circle arteries. Int J Radiat Oncol Biol Phys. 2017;97:278–86.
Plummer C, Henderson RD, O’Sullivan JD, Read SJ. Ischemic stroke and transient ischemic attack after head and neck radiotherapy: a review. Stroke. 2011;42:2410–8.
Campen CJ, Kranick SM, Kasner SE, Kessler SK, Zimmerman RA, Lustig R, et al. Cranial irradiation increases risk of stroke in pediatric brain tumor survivors. Stroke. 2012;43:3035–40.
Rocca WA, Shuster LT, Brown RD. Could estrogen protect younger menopausal women from stroke? Expert Rev Neurother. 2012;12:363–5.
Petrovska S, Dejnaova B, Jurisic V. Estrogens: mechanisms of neuroprotective effects. J Physiol Biochem. 2012;68:455–60.
Jacobson G, Lammli J, Zamba G, Hua L, Goodheart MJ. Thromboembolic events in patients with cervical carcinoma: incidence and effect on survival. Gynecol Oncol. 2009;113:240–4.
Silverberg GD, Britt RH, Goffinet DR. Radiation-induced carotid artery disease. Cancer. 1978;41:130–7.
Author information
Authors and Affiliations
Contributions
Study concept and design, M. T., P. M., M-J. M., and R. A.; study selection, M. T., A. Y. O., and S.D.; data extraction, M. T. and R. A.; quality assessment, M. T., R. A., and L. W.; statistical analysis, M. T.; writing — original draft, M. T.; writing — reviewing and editing, M. T., P. M., M-J. M., R. A., and D.M. Approval of the final paper for submission, all authors.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All analyses were based on previously published studies; therefore, no ethical approval or patient consent is required.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Turner, M., Murchie, P., Derby, S. et al. Is stroke incidence increased in survivors of adult cancers? A systematic review and meta-analysis. J Cancer Surviv 16, 1414–1448 (2022). https://doi.org/10.1007/s11764-021-01122-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-021-01122-7