Abstract
Purpose
Physical activity has been shown to improve survival and quality of life of cancer patients. Due to differences in patient populations, healthcare settings, and types of intervention, cost-effectiveness analyses of physical activity interventions in cancer survivors are difficult to compare. Available evidence from breast cancer survivor research has shown inconsistent results, and transfer of results to other types of cancer is not straightforward. This paper systematically reviewed current evidence on the cost-effectiveness of physical activity interventions in cancer survivors independent of cancer type compared to usual care or another experimental intervention.
Methods
The literature search was conducted in seven databases and enhanced by a search for gray literature. Eligible studies were restricted to developed countries and assessed using the CHEERS, CHEC, and PHILIPS checklists. The study protocol was pre-published in PROSPERO.
Results
Seven studies, five cost-utility, and two combined cost-utility/cost-effectiveness analyses fully met the inclusion criteria. They covered eight different types of cancer and various interventions. The cost-effectiveness analyses were of moderate to high methodological quality. A high probability of cost-effectiveness was reported in two analyses. One intervention appeared to be not cost-effective, and one to be cost-effective only from an organizational perspective. Three other analyses reported a cost-effectiveness better than US$ 101,195 (€ 80,000) per QALY gained.
Conclusions
Physical activity interventions in cancer survivors of developed countries were cost-effective in some but not all clinical trials reviewed.
Implications for Cancer Survivors
Cost-effectiveness of physical activity interventions appear to depend upon the intensity of the activity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cancer is one of the leading causes of death worldwide. The incidence of cancer was 18.1 million cases in 2018 and is increasing [1]. In western healthcare systems, 5-year survival rates range from 5% for liver or lung cancers to 90% for breast cancer [2] and are still improving over time. Therefore, cancer often becomes a chronic condition, which remains a challenge for daily life.
Survivors have to contend with secondary effects, such as physical, psychological, or social impairments, either caused by the disease itself or by treatment [3]. An overall reduction in quality of life is common for several cancer types because of symptoms such as fatigue, pain, or functional disability [4,5,6], which in turn affect employment, family life, and recreation. The symptoms often persist for many years, leading to chronicity and multi-morbidity. Most survivors do not achieve previous levels of function and report prolonged fatigue, cognitive limitations, depression, anxiety, sleep problems, pain, or sexual dysfunction for up to ten years after diagnosis [7].
Lifestyle interventions directed at physical activity, diet, weight control, and cessation of smoking are thought to be effective in alleviating these detrimental effects and improving quality of life [8,9,10,11]. Physical activity interventions have a positive effect on the quality of life of cancer survivors [12] and are frequently promoted and well-established in rehabilitation programs to combat the secondary effects of cancer. It is well documented that physical activity reduces the risks of cancer recurrence, all-cause mortality, and secondary chronic diseases [13, 14].
Healthcare systems operate under constrained budget conditions and must consider the increasing demand for rehabilitation programs for cancer survivors critically. The goals of optimizing quality of life and preventing secondary chronic diseases must be combined with a focus on patient-specific care needs, within the constraints of the healthcare budget. Therefore, an understanding of financial spending and cost-effectiveness in cancer care is essential. Depending on cancer type, disease stage, and age, net costs to all payers in the USA were expected to range between US$ 20,000 and US$ 100,000 in the first year after diagnosis and to be lower in the extended survivorship phase, before increasing in end-of-life treatment [15]. Costs are driven by medical costs such as new cancer treatments and hospitalization and indirect costs such as absenteeism, job loss or disability pensions [15,16,17]. Out-of-pocket expenses for medical care could range from 7 to 11% of medical costs [18,19,20,21]. The individual financial strain affects the patient and their family substantially [22] and correlates to poor treatment adherence [23], worsening of symptoms [24], poor quality of life [25], and shorter survival [26].
Interventions, such as those directed at physical activity, must be evaluated carefully regarding their impact on private and/or healthcare system budget allocation and value for money. There is some evidence of cost-effectiveness in physical activity promotion in population-based programs [27]. In cancer rehabilitation, results remain unclear. A systematic review of cost-effectiveness studies of physical activity programs in a multidimensional setting including all types of cancer showed little available evidence [28]. In programs for breast cancer survivors, results remained unclear because of differences in patient populations and healthcare settings [29]. A tendency in the literature to focus on breast cancer limits the transferability of results to other cancer types [28]. The present study systematically reviewed the existing literature on the cost-effectiveness of physical activity interventions in cancer survivors independent of cancer type compared to usual care or another experimental intervention.
Methods
The systematic review on the cost-effectiveness of physical activity interventions in cancer survivors focused on quality-adjusted life years (QALYs), costs, and incremental cost-effectiveness as outcome data. The predefined study protocol was registered in the international prospective register of systematic reviews (PROSPERO; CRD42019130284).
Selection criteria
Publications included in this review had to be written in English and had to be clinical trial-based or decision-analytical model-based cost-effectiveness or cost-utility studies conducted in developed countries, as defined in the UN World Economic Situation and Prospects 2018 [30] (USA, Canada, Japan, Australia, New Zealand, and the states of Europe), to allow for sufficient comparability, limiting transferability to developing and/or emerging countries. The studies included were considered without time restrictions. Studies conducted in other countries or not meeting eligible study designs were excluded.
The eligible populations were cancer survivors over 18 years of age with histologically confirmed cancer diagnosis of any type, expected survival period of at least 1 year, and participating in either a physical activity intervention or referred to a comparator strategy which could either be usual care or another experimental intervention. Studies including patients not meeting the criteria of a cancer survivor [31] were excluded. Physical activity interventions not following the definition of Casperson [32] that focused predominantly on physiologic effects, such as cardiovascular and/or endurance and/or strength-training, were not considered in the study.
Search strategy
PubMed/MEDLINE via Ovid, CINAHL, Cochrane Library, EMBASE, Centre for Review and Dissemination (CRD), EconLit, and Epistemonikos were searched electronically using predefined key words and medical subject headings (MeSH). Validated search strings of the InterTASC Information Specialists’ Sub-Group guidelines (ISSG) [33] were used for costs, focusing on optimization of sensitivity and specificity (95.0% and specificity of 95.6% [34] for MEDLINE and sensitivity of 98.4% and a specificity of 97.1% [35] for EMBASE). Advanced searches for gray literature were performed using website search functionality in Google Scholar and the BioRxiv preprint server. Finally, bibliography mining and cited reference searches using reference lists was undertaken [36]. Table 1 provides an overview of the search strategy used, which was adapted for the other sources.
Screening process
Citations of all search results were downloaded into a literature-management package (EndNote X7.8; Thomson and Reuters, Philadelphia, PA) and imported to the free web-based application Rayyan QCRI [37]. Title and abstract were screened by two authors independently. The same approach was used for full-text screening. Discrepancies were solved by discussion or third-party arbitration.
Data extraction and quality assessment
The data extraction form was developed prior to conduct of the review, based on Centre for Reviews and Dissemination (CRD)-recommendations [38, 39], the Cochrane Handbook guidance [40], and ISPOR recommendations [41]. The form was tested prior to the review by two authors independently and was adjusted through discussion. Extracted study characteristics included author, year of publication, country of study performance, study design, population, type of intervention, and comparator. To cover economic evaluation, data on study perspective, analytical approach, time horizon, direct and indirect costs, effectiveness, and cost-effectiveness were added. Data extraction was performed by one reviewer and verified by a second.
Quality assessments
Quality of reporting and quality of methodology were determined using different checklists for cost-effectiveness analyses and were assessed by one reviewer and verified by a second. The Consolidated Health Economic Evaluation Reporting Scale (CHEERS) [42] was used to gather information on the quality of reporting. For the quality assessment of primary clinical trial-based cost-effectiveness analyses, the extended Consensus Health Economics Criteria (CHEC) checklist [43] was used, while for decision-analytic model-based analyses the guidelines for good practice in decision-analytic modeling (Philips) [44] were used. Both checklists (CHEC [43] and Philips [44]) were employed to assess studies using a combined trial-based and decision-analytic model-based approach. As recommended by the GRADE guidelines [45] and to ensure the confidence in effect estimates, the Cochrane Rob2 tool [46] was used to assess the risk of bias in the underlying clinical trials, where appropriate.
Synthesis
Results were summarized in tables and graphically represented in cost-effectiveness planes. Subgroups of studies were formed based on type of intervention, starting point of intervention during medical treatment process, intensity and type of cancer. Specifically, interventions were subdivided into the categories of direct (face-to-face), indirect, or combined support groups. Intensity was subdivided into low intensity (up to 12 Borg [47]/65% of one repetition max. [48, 49]), moderate intensity (13–15 Borg [47]/66–79% of one repetition max. [48, 49]) or high intensity (16–20 Borg [47]/80–100% of one repetition max. [48, 49]) groups. Intervention starting point was either during or post medical treatment (radiotherapy and/or chemotherapy).
Cost data extracted from the studies were inflated to 2017 US Dollars using purchasing power parity (PPP) conversion factors [50]. In studies not reporting price year data, it was assumed that the price year was 1 year prior to study publication. Reporting was undertaken following PRISMA guidance [51].
Results
The literature search was conducted in May 2019. A total of 3290 articles were identified. The gray literature search yielded one additional record, which has been published in the meantime [52]. Deduplication resulted in 2.078 remaining articles, of which 2061 were excluded in the title and abstract screening. The full text of the remaining 17 articles was analyzed, resulting in the exclusion of a further eight articles. No more articles were identified from bibliography mining and cited reference search (Fig. 1). Seven publications were finally included in the review: May et al. [53], Gordon et al. [54], van Waart et al. [55], Kampshoff et al. [56], Mewes et al. [57], Haines et al. [58], and Ha et al. [52] met all inclusion criteria. Broderick et al. [59] reported an incomplete cost-effectiveness analysis due to the unavailability of survival information, and Gordon et al. [60] presented a cost-consequences analysis. Both papers were included in the discussion.
Study characteristics and participants
Five cost-utility analyses [52, 53, 56,57,58] and two combined cost-utility/cost-effectiveness analyses [54, 55] were published between 2010 and 2019 in the Netherlands, Australia, USA, and Ireland. Study characteristics are presented in Table 2 (see extended online Table 2 for more detail). A trial-based approach was chosen by five research groups [53,54,55,56, 58]. Mewes et al. [57] combined a trial-based and model-based approach, and Ha et al. [52] carried out a model-based analysis. The various clinical studies underlain the cost-effectiveness evaluations included a total of 3494 patients, ranging from 89 [58] to 1635 [52] participants per study. Four studies reported a breast cancer [54, 55, 57, 58], one study a lung cancer [52] and two studies a mixed cancer population [53, 56]. The mean age of the study populations was between 48.2 [57] and 78.9 [52] years and covered a wide range of baseline physical fitness level.
Intervention characteristics
Interventions were launched either during the cancer treatment or after completion of the primary therapy, ranging from as early as 6 to 10 weeks after cancer diagnosis [53] to a start after completed chemotherapy [56, 57]. Intervention intensity and duration ranged from low to moderate [55] to high intensity [56] and from twelve [56, 57] to 125 weeks [52]. In the control groups, cancer survivors received either usual care [54, 55], usual care with instructions to maintain habitual levels of activity [53], waiting list control [56, 57], or active sham intervention with relaxation program or weekly health education [52, 58]. Interventions focused on cardiovascular [57] or combined cardiovascular and strength [52,53,54,55,56, 58] training respecting the needs of the patient.
Activities in single sessions varied in duration and frequency. Participants were physically active between 30 [55] to 60 min [53, 58] per session, from two [54, 57], to five [55] times a week, in a range from low to moderate [58] to high [55,56,57,58] intensity. Adherence to the training varied between 48 [55] and 88% [54].
Quality assessments
Quality assessment of cost-effectiveness studies
Quality of reporting was moderate to high [52,53,54,55,56,57,58], and was affected by missing or incomplete cost data [54, 55], insufficient information about discount rates [54, 55, 58], and unclear adjustment of unit cost estimates to a base year [54, 56, 58] (Table 3).
Moderate to high quality of methodology was found overall for the studies by May et al. [53], Gordon et al. [54], van Waart et al. [55], Kampshoff et al. [56], Mewes et al. [57], and Haines et al. [58] (Table 3). Weaknesses identified were that some important and relevant costs for alternatives were not identified [54, 57], that not all data were reported, and that not all costs were valued appropriately [58]. Ha et al.’s [52] model-based cost-effectiveness analysis and the Mewes et al. [57] paper, as a combination of trial-based and model-based analysis, were considered to be of high methodological quality.
Quality assessment of RCTs underlying the cost-effectiveness studies
The RCTs of Kampshoff et al. [61] and Pahor et al. [62] were considered to have low risk of bias due to implementation of a sham intervention (Fig. 2). Some concerns in the studies by Travier et al. [63] and Hayes et al. [64] were lack of assessor blinding. High risk of bias in the studies by van Waart et al. [65], Duijts et al. [66], and Haines et al. [58] was based on lack of information on concealment of the allocation sequence and high losses to follow-up.
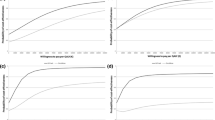
Cost-effectiveness
Cost-effectiveness results are summarized in Table 4 (see extended online Table 4 for more detail) and on the cost-effectiveness plane in Fig. 3. High-intensity training in the study of Kampshoff et al. [56], physical activity interventions in colon [53] and lung [52] cancer patients, were reported to be cost-effective. For breast cancer, inconsistent results were shown. Mewes et al. [57] showed cost-effectiveness up to a ceiling ratio of US$ 36,229/QALY gained. Gordon et al. [54], van Waart et al. [55], and Haines et al. [58] and their colleagues demonstrated a likelihood of being cost-effective under 45%. Personal-supported programs delivered by physiotherapists or exercise physiologists [52, 53, 55, 56] were more likely to be cost-effective than self-management programs [54, 57, 58].
Breast cancer
An Australian study reported a moderate- to high-intensity 32-week physical activity intervention with an ICER of US$ 81,648/QALY from the service provider perspective and US$ 70,483/QALY from the private perspective, respectively. With a threshold of US$ 34,615/QALY, the probability of cost-effectiveness was 44.4% and 46.3% [54] in the probabilistic sensitivity analysis. Sensitivity analysis indicated that ICERs were sensitive to EQ-5D-3L weights when varied within their 95% confidence intervals [54]. Another study from the Netherlands conducted 17-week physical activity programs of both low intensity and of moderate- to high-intensity and observed an ICER of US$ 88,611/QALY and the moderate to high-intensity training an ICER of US$ 34,047/QALY. With a threshold of US$ 101,195/QALY, the probability of cost-effectiveness ranged from 55% for low intensity to 79% for moderate to high-intensity training [55]. In a sensitivity analysis including solely compliant participants, probability of cost-effectiveness seemed to be better [55]. The study by Mewes et al. [57], a 12-week individualized physical activity training, showed an ICER of US$ 39,124/QALY for the physical exercise strategy. The exercise intervention had the highest probability of being cost-effective up to a willingness-to-pay of US$ 32,888/QALY. Beyond this value, the second intervention assessed (cognitive behavioral therapy) had a higher probability of being cost-effective. Results were robust, showing lower cost-effectiveness with shorter treatment duration [57] in a sensitivity analysis. Haines et al. undertook a moderate to high-intensity 18-week DVD-delivered physical activity intervention without reporting any QALY values transparently [58].
Breast and colon cancer
A Dutch 18-week low to moderate physical activity intervention for breast and colon cancer showed an ICER of US$ 599.083/QALY. In breast cancer, the probability of being cost-effective was 2 to 6% with a willingness-to-pay threshold of US$ 101,195/QALY [53]. Sensitivity analyses with different willingness to pay thresholds showed higher costs for a small additional effect on QALY. Therefore, the physical activity intervention was shown to be cost-effective for colon, but not breast cancer patients [53].
Lung cancer
A US study assessing a moderate to high-intensity training over 125 weeks in lung cancer survivors showed an incremental cost-effectiveness ratio of US$ 79,504/QALY and led to a probability of being cost-effective of 71% with a willingness to pay threshold of US$ 100,000/QALY and of 94% with US$ 150,000/QALY [52]. With costs of US$ 116,686, the moderate- to high-intensity training [52] reported the highest program expenditures seen in this review, for a long-term intervention. In this study, the model was most sensitive to the costs of the exercise program, probability of increasing exercise, and health utility benefit related to exercise [52]. The intervention was cost-effective from an organizational perspective, including costs for targeted therapy but not immunotherapy. No cost-effectiveness was seen from a societal perspective, including participant opportunity costs related to time spent in exercise [52].
Mixed cancer population
A Dutch trial, comparing high- and low-to-moderate-intensity training of 12 weeks, indicated a significant effect of high-intensity physical activity on role and social functioning. Cardiorespiratory fitness showed a short- and long-term increase in the low-to-moderate- and high-intensity groups [56]. An ICER of US$ 128.163/QALY was indicated for the high-intensity-training compared to the low to moderate-intensity training [56]. With a willingness-to-pay of US$ 25,299/QALY, the probability of cost-effectiveness was 91% and 95% with a willingness-to-pay of US$ 65,777/QALY [56]. Sensitivity analyses for payment of all scheduled exercise sessions and disease recurrence were robust [56]. High-intensity training was cost-effective and reduced healthcare costs [56].
Discussion
This systematic review assessed the cost-effectiveness of physical activity interventions in cancer survivors, including any type of cancer. Seven cost-utility and/or cost-effectiveness studies [52,53,54,55,56,57,58] were included and systematically analyzed. These studies evaluated eleven different types of interventions, in four settings and at three different levels of intensity. Studies were of moderate to high methodological and reporting quality and the risk of bias of underlying clinical trials ranged from low to high. Whereas results for breast cancer were unclear [53,54,55, 57, 58], physical activity interventions for lung cancer patients were reported to be cost-effective, with 71% probability at a willingness-to-pay threshold of US$100,000/QALY rising to 94% at a US$150,000/QALY willingness-to-pay [52]. For colon cancer, results were reported to be dominant [53] and for a high-intensity training, a probability of cost-effectiveness of 91% at a willingness-to-pay threshold of US$ 25,299/QALY was reported [56]. Studies indicating cost-effectiveness of physical activity interventions were of high quality of reporting and methodology [52, 53, 55, 56] with low to high risk of bias [58, 61, 62, 65, 66].
Our results are in line with previous reviews. Mewes et al. reported ICER’s below the prevailing willingness-to-pay threshold in multidimensional rehabilitation programs applied to various types of cancer [28]. In 2012, they found four economic evaluations published between 2005 and 2011 with significant benefits of the intervention over the control group in terms of QALYs, energy, fear of regression, mood, and pain. However, comparability between the studies found was low due to different types of interventions. Khan et al. focused their review on breast cancer survivors and documented contrasting conclusions due to heterogeneity in the interventions delivered [29]. Guillon and colleagues discussed unclear results of three cost-effectiveness analyses of physiotherapy-led exercise programs for breast and head and neck cancer patients [67, 68].
The identified findings for colon cancer [53, 56] are underlined by documented effects of physical activity interventions on quality of life in colon and colorectal cancer survivors [59, 60, 69, 70], but further reliable data on cost-effectiveness are missing. The same applies to lung cancer. With a probability of being cost-effective of 94% with a willingness-to-pay threshold of US$150,000 per QALY [52], the intervention studied by Ha and colleagues in lung cancer was cost-effective [52]. This is in line with the effectivity of physical activity interventions in lung cancer but with no further information on cost-effectiveness [71].
Van Dongen et al. included patients with hematologic malignancy treated with stem cell transplantation and trained them in a supervised 18-week high-intensity interval and resistance training [72]. They found the intervention to be not cost-effective due to lack of clinical effectiveness [72]. One reason could have been suboptimal compliance or the timing of the intervention, due to the length of time to recovery in stem cell transplantation [72], which is a problem in comparability between different types of cancer.
Effects of physical activity interventions are driven by intensity, duration/adherence, delivery mode, and starting point of intervention during rehabilitation. This has implications for cost-effectiveness. We found high-intensity interventions, such as described by van Waart et al. [55] and Kampshoff et al. [56], may be more cost-effective relative to usual care than light to moderate physical activity programs, due to a potential reduction in healthcare use [56]. This is in line with studies on effectiveness which compared a low-volume and high-intensity to low-to-moderate-intensity training or usual care. They included different types of cancer and described an effect on quality of life (d = 1.11; 95% CI 0.50, 1.72), cardiorespiratory fitness (d = 0.97; 95% CI 0.36, 1.56), lower body strength (P < 0.01; d = − 0.83; 95% CI − 1.40, − 0.22) and waist circumference (P = 0.01; d = − 0.48; 95% CI − 1.10, 0.10) [73]. The result is underlined by another study, which delivered a well-tolerated, high-intensity intervention over 20 weeks in lung cancer patients, showing significant effects on peak oxygen uptake (3.4 mL/kg/min between-group difference, 95% CI 3.3 to 6.7; p < 0.001), total muscle strength (leg press increased by 27.4 ± 26.2 kg (p = 0.001)), functional fitness and quality of life (after intervention, the QoL scale was 51.8 ± 5.5 in the exercise group and 43.3 ± 11.3 in the control group (p = 0.006)) compared to usual care [74].
Two thirds of cancer survivors do not meet physical activity recommendations in the USA [75], in particular women of low education and with comorbid conditions [76]. Program duration and adherence to intervention could play important roles in the cost-effectiveness of physical activity interventions such that long-term support might result in better adherence to training and less hospitalizations [75]. However, in our review, intervention duration, varying from 12 to 125 weeks, did not correlate with cost-effectiveness. Adherence to physical activity interventions, which ranged from 48% for home-based activities [55] to 83% for supervised classes [53], was also not correlated with cost-effectiveness.
Delivery modes of physical activity programs vary widely, from personal support to distance-based interventions. In our analysis, the interventions that were cost-effective [52, 53, 55, 56] were personal support programs delivered by a home-based additional training or recommendation. However, the starting point of the physical activity intervention did not seem to affect cost-effectiveness. Patients diagnosed with cancer often report difficulties in the adoption and maintenance of exercise. Concerns about safety, desire for professional guidance, physical limitations, fatigue, or lack of time were reported [77,78,79]. This indicates that personal support could be beneficial. A systematic review of 27 distance-based physical activity interventions in cancer survivors found no effect on reported physical activity [80]. Goode et al. reported an effect of non-face-to-face lifestyle interventions in three quarters of the 27 studies, with a preference for telephone-based activities [81]. Novel technologies, with the possibility of delivering physical activity interventions to meet patients’ needs with an optimal allocation of resources, should be investigated. Furthermore, cost-effectiveness of program duration, frequency and intensity needs to be observed in-depth to allocate resources in an optimal manner. Last but not least, information about maintenance of long-term adherence is needed.
The strength of this study is that it uses a robust methodological procedure, based on clear eligibility criteria and standardized, validated assessment instruments. Two independent reviewers and a professional librarian were involved in the definition of the search process and analysis undertaken. Thorough analyses of different aspects of interventions were performed and the implications for cost-effectiveness assessed. There are some limitations to point out. Due to the heterogeneity of the identified studies researchers were unable to summarize the results quantitatively. The population in the trials underlying most of the cost-effectiveness analyses were not representative of all patients with the respective cancer types, with those included in the trials probably at an advanced stage of cancer, at an older age, more likely to be female and more active [82,83,84]. Due to inclusion of studies only from developed countries, transferability to developing and/or emerging countries is not possible. Further physical activity arrangements outside the study protocols were not assessed or reported. With respect to the reporting of cost-effectiveness, relevant information was not necessarily available from all studies, particularly for direct costs, indirect costs, and productivity losses. The economic burden of early retirement, productivity loss, and disability pensions is substantial [85].
Conclusion
We systematically reviewed cost-effectiveness analyses of physical activity interventions in cancer survivors over all types of cancer. High-intensity training interventions appeared to have a potential for being cost-effective and two studies found that interventions for colon, respectively, lung cancer were cost-effective. Further results are inconclusive because of the heterogeneity of interventions and cost data available. More research is needed to make results more robust. A greater focus on cost-effectiveness studies considering different intervention characteristics, such as, frequency, intensity, duration, and intervention delivery modalities, could deliver more in-depth results. Furthermore, future work will need to cover software-assisted tools and wearables.
Data availability
Systematic review—all data is publically available
References
Wiseman M. The Second World Cancer Research Fund/American Institute for Cancer Research Expert Report. Food, nutrition, physical activity, and the prevention of cancer: a global perspective: utrition Society and BAPEN Medical Symposium on ‘Nutrition support in cancer therapy. Proc Nutr Soc. 2008;67:253–6.
Allemani C, Matsuda T, Di Carlo V, Harewood R, Matz M, Nikšić M, et al. Global surveillance of trends in cancer survival 2000–14 (CONCORD-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet. 2018;391:1023–75.
de Boer AG, Taskila TK, Tamminga SJ, Feuerstein M, Frings-Dresen MH, Verbeek JH. Interventions to enhance return-to-work for cancer patients. Cochrane Database Syst Rev [Internet] 2015 [cited 2018 Oct 9];Available from: https://www.readcube.com/articles/10.1002/14651858.CD007569.pub3
Adam S, Koch-Gallenkamp L, Bertram H, Eberle A, Holleczek B, Pritzkuleit R, et al. Health-related quality of life in long-term survivors with localised prostate cancer by therapy-Results from a population-based study. Eur J Cancer Care (Engl). 2019;28:e13076.
Cramer JD, Johnson JT, Nilsen ML. Pain in head and neck cancer survivors: prevalence, predictors, and quality-of-life impact. Otolaryngol Head Neck Surg. 2018;159:853–8.
Crossnohere NL, Richardson DR, Reinhart C, O’Donoghue B, Love SM, Smith BD, et al. Side effects from acute myeloid leukemia treatment: results from a national survey. Curr Med Res Opin. 2019;35:1–6.
Harrington CB, Hansen JA, Moskowitz M, Todd BL, Feuerstein M. It’s not over when it’s over: long-term symptoms in cancer survivors—a systematic review. Int J Psychiatry Med. 2010;40:163–81.
Fuller JT, Hartland MC, Maloney LT, Davison K. Therapeutic effects of aerobic and resistance exercises for cancer survivors: a systematic review of meta-analyses of clinical trials. Br J Sports Med. 2018;52:1311.
Eyl RE, Xie K, Koch-Gallenkamp L, Brenner H, Arndt V. Quality of life and physical activity in long-term (≥5 years post-diagnosis) colorectal cancer survivors - systematic review. Health Qual Life Outcomes. 2018;16:112.
Grimmett C, Corbett T, Brunet J, Shepherd J, Pinto BM, May CR, et al. Systematic review and meta-analysis of maintenance of physical activity behaviour change in cancer survivors. Int J Behav Nutr Phys Act. 2019;16:37.
Rock CL, Doyle C, Demark-Wahnefried W, Meyerhardt J, Courneya KS, Schwartz AL, et al. Nutrition and physical activity guidelines for cancer survivors. CA Cancer J Clin. 2012;62:242–74.
Burke S, Wurz A, Bradshaw A, Saunders S, West MA, Brunet J. Physical activity and quality of life in cancer survivors: a meta-synthesis of qualitative research. Cancers (Basel) [Internet] 2017 [cited 2019 Nov 24];9. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5447963/
Speck RM, Courneya KS, Mâsse LC, Duval S, Schmitz KH. An update of controlled physical activity trials in cancer survivors: a systematic review and meta-analysis. J Cancer Surviv. 2010;4:87–100.
Spei M-E, Samoli E, Bravi F, La Vecchia C, Bamia C, Benetou V. Physical activity in breast cancer survivors: a systematic review and meta-analysis on overall and breast cancer survival. Breast. 2019;44:144–52.
Pisu M, Henrikson NB, Banegas MP, Yabroff KR. Costs of cancer along the care continuum: what we can expect based on recent literature. Cancer. 2018;124:4181–91.
Paltrinieri S, Fugazzaro S, Bertozzi L, Bassi MC, Pellegrini M, Vicentini M, et al. Return to work in European Cancer survivors: a systematic review. Support Care Cancer. 2018;26:2983–94.
Stapelfeldt CM, Klaver KM, Rosbjerg RS, Dalton SO, Bültmann U, Labriola M, et al. A systematic review of interventions to retain chronically ill occupationally active employees in work: can findings be transferred to cancer survivors? Acta Oncol. 2019;58:548–65.
Guy GP, Ekwueme DU, Yabroff KR, Dowling EC, Li C, Rodriguez JL, et al. Economic burden of cancer survivorship among adults in the United States. JCO. 2013;31:3749–57.
Davidoff AJ, Erten M, Shaffer T, Shoemaker JS, Zuckerman IH, Pandya N, et al. Out-of-pocket health care expenditure burden for Medicare beneficiaries with cancer. Cancer. 2013;119:1257–65.
Ekwueme DU, Yabroff KR, Guy GP, Banegas MP, de Moor JS, Li C, et al. Medical costs and productivity losses of cancer survivors--United States, 2008-2011. MMWR Morb Mortal Wkly Rep. 2014;63:505–10.
Zheng Z, Yabroff KR, Guy GP, Han X, Li C, Banegas MP, et al. Annual medical expenditure and productivity loss among colorectal, female breast, and prostate cancer survivors in the United States. J Natl Cancer Inst. 2016;108:djv382.
Shippee TP, Wilkinson LR, Ferraro KF. Accumulated financial strain and women’s health over three decades. J Gerontol B Psychol Sci Soc Sci. 2012;67:585–94.
Bestvina CM, Zullig LL, Yousuf ZS. The implications of out-of-pocket cost of cancer treatment in the USA: a critical appraisal of the literature. Future Oncol. 2014;10:2189–99.
Fenn KM, Evans SB, McCorkle R, DiGiovanna MP, Pusztai L, Sanft T, et al. Impact of financial burden of cancer on survivors’ quality of life. JOP. 2014;10:332–8.
Lathan CS, Cronin A, Tucker-Seeley R, Zafar SY, Ayanian JZ, Schrag D. Association of financial strain with symptom burden and quality of life for patients with lung or colorectal cancer. JCO. 2016;34:1732–40.
Ramsey SD, Bansal A, Fedorenko CR, Blough DK, Overstreet KA, Shankaran V, et al. Financial insolvency as a risk factor for early mortality among patients with cancer. J Clin Oncol. 2016;34:980–6.
Abu-Omar K, Rütten A, Burlacu I, Schätzlein V, Messing S, Suhrcke M. The cost-effectiveness of physical activity interventions: a systematic review of reviews. Prev Med Rep. 2017;8:72–8.
Mewes JC, Steuten LMG, IJzerman MJ, van Harten WH. Effectiveness of multidimensional cancer survivor rehabilitation and cost-effectiveness of cancer rehabilitation in general: a systematic review. Oncologist. 2012. https://doi.org/10.1634/theoncologist.2012-0151.
Khan KA, Mazuquin B, Canaway A, Petrou S, Bruce J. Systematic review of economic evaluations of exercise and physiotherapy for patients treated for breast cancer. Breast Cancer Res Treat. 2019;176:37–52.
United Nations. World economic situation and prospects. New York: United Narions Publication, 2018.
The NCCS definition of a “cancer survivor” [Internet]. NCCS - National Coalition for Cancer Survivorship 2014 [cited 2019 Nov 24];Available from: https://www.canceradvocacy.org/news/defining-cancer-survivorship/
Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep. 1985;100:126–31.
Glanville J, Bayliss S, Booth A, Dundar Y, Fernandes H, Fleeman ND, et al. So many filters, so little time: the development of a search filter appraisal checklist. J Med Libr Assoc. 2008;96:356–61.
Wilczynski NL, Haynes RB, Lavis JN, Ramkissoonsingh R, Arnold-Oatley AE. Optimal search strategies for detecting health services research studies in MEDLINE. CMAJ. 2004;171:1179–85.
the Hedges Team, McKinlay RJ, Wilczynski NL, Haynes RB. Optimal search strategies for detecting cost and economic studies in EMBASE. BMC Health Serv Res[Internet] 2006 [cited 2018 Oct 22];6. Available from: http://bmchealthservres.biomedcentral.com/articles/10.1186/1472-6963-6-67
P R, N W. Literature searching for clinical and cost-effectiveness studies used in health technology assessment reports carried out for the National Institute for Clinical Excellence appraisal system. Health Technology Assessment [Internet] 2003 [cited 2019 Dec 9];7. Available from: https://www.journalslibrary.nihr.ac.uk/hta/hta7340#/abstract
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev [Internet] 2016 [cited 2019 Oct 9];5. Available from: https://www.readcube.com/articles/10.1186/s13643-016-0384-4
Polinder S, Toet H, Panneman M, van Beeck E. Methodological approaches for cost–effectiveness and cost–utility analysis of injury prevention measures. Copenhagen: World Health Organisation, 2011.
Tacconelli E. Systematic reviews: CRD’s guidance for undertaking reviews in health care. Lancet Infect Dis. 2010;10:226.
Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions. Chichester (UK): John Wiley & Sons, 2011.
Cost-effectiveness analysis alongside clinical trials II [Internet]. ISPOR | International Society For Pharmacoeconomics and Outcomes Research [cited 2019 Oct 9];Available from: https://www.ispor.org/heor-resources/good-practices-for-outcomes-research/article/cost-effectiveness-analysis-alongside-clinical-trials-ii
Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D, et al. Consolidated Health Economic Evaluation Reporting Standards (CHEERS) statement. BMJ. 2013;346:f1049.
Evers S, Goossens M, de Vet H, van Tulder M, Ament A. Criteria list for assessment of methodological quality of economic evaluations: consensus on health economic criteria. Int J Technol Assess Health Care. 2005;21:240–5.
Philips Z, Ginnelly L, Sculpher M, Claxton K, Golder S, Riemsma R, et al. Review of guidelines for good practice in decision-analytic modelling in health technology assessment. Health Technol Assess. 2004;8:iii–iv, ix–xi, 1–158.
Brunetti M, Shemilt I, Pregno S, Vale L, Oxman AD, Lord J, et al. GRADE guidelines: 10. Considering resource use and rating the quality of economic evidence. J Clin Epidemiol. 2013;66:140–50.
Sterne JA, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. Bmj. 2019;366:l4898.
Borg G, Ljunggren G, Ceci R. The increase of perceived exertion, aches and pain in the legs, heart rate and blood lactate during exercise on a bicycle ergometer. Eur J Appl Physiol. 1985;54:343–9.
Morishita S, Yamauchi S, Fujisawa C, Domen K. Rating of perceived exertion for quantification of the intensity of resistance exercise. Int J Phys Med Rehabil 2013;1:192.
Day ML, McGuigan MR, Brice G, Foster C. Monitoring exercise intensity during resistance training using the session RPE scale. J Strength Cond Res. 2004;18:353–8.
Conversion rates - Purchasing power parities (PPP) - OECD Data [Internet]. the OECD [cited 2019 Nov 11];Available from: http://data.oecd.org/conversion/purchasing-power-parities-ppp.htm
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. PLoS Med [Internet] 2009 [cited 2019 Dec 11];6. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2707599/
Ha DM, Kerr J, Ries AL, Fuster MM, Lippman SM, Murphy JD. A model-based cost-effectiveness analysis of an exercise program for lung cancer survivors following curative-intent treatment. Am J Phys Med Rehabil. 2020;99:233–40.
May AM, Bosch MJC, Velthuis MJ, van der Wall E, Bisschop CNS, Los M, et al. Cost-effectiveness analysis of an 18-week exercise programme for patients with breast and colon cancer undergoing adjuvant chemotherapy: the randomised PACT study. BMJ Open. 2017;7:e012187.
Gordon LG, DiSipio T, Battistutta D, Yates P, Bashford J, Pyke C, et al. Cost-effectiveness of a pragmatic exercise intervention for women with breast cancer: results from a randomized controlled trial. Psycho-Oncology. 2017;26:649–55.
van Waart H, van Dongen JM, van Harten WH, Stuiver MM, Huijsmans R, Hellendoorn-van Vreeswijk JAJH, et al. Cost-utility and cost-effectiveness of physical exercise during adjuvant chemotherapy. Eur J Health Econ. 2018;19:893–904.
Kampshoff CS, van Dongen JM, van Mechelen W, Schep G, Vreugdenhil A, Twisk JWR, et al. Long-term effectiveness and cost-effectiveness of high versus low-to-moderate intensity resistance and endurance exercise interventions among cancer survivors. J Cancer Surviv. 2018;12:417–29.
Mewes JC, Steuten LMG, Duijts SFA, Oldenburg HSA, van Beurden M, Stuiver MM, et al. Cost-effectiveness of cognitive behavioral therapy and physical exercise for alleviating treatment-induced menopausal symptoms in breast cancer patients. J Cancer Surviv. 2015;9:126–35.
Haines TP, Sinnamon P, Wetzig NG, Lehman M, Walpole E, Pratt T, et al. Multimodal exercise improves quality of life of women being treated for breast cancer, but at what cost? Randomized trial with economic evaluation. Breast Cancer Res Treat. 2010;124:163–75.
Broderick JM, Guinan E, O’ Donnell DM, Hussey J, Tyrrell E, Normand C. Calculating the costs of an 8-week, physiotherapy-led exercise intervention in deconditioned cancer survivors in the early survivorship period (the PEACH trial). Physiotherapy. 2014;100:182–4.
Gordon LG, Patrao T, Kularatna S, Hawkes AL. A telephone-delivered multiple health behaviour change intervention for colorectal cancer survivors: making the case for cost-effective healthcare. Eur J Cancer Care (Engl). 2015;24:854–61.
Kampshoff CS, Chinapaw MJM, Brug J, Twisk JWR, Schep G, Nijziel MR, et al. Randomized controlled trial of the effects of high intensity and low-to-moderate intensity exercise on physical fitness and fatigue in cancer survivors: results of the Resistance and Endurance exercise After ChemoTherapy (REACT) study. BMC Med. 2015;13:275.
Pahor M, Guralnik JM, Ambrosius WT, Blair S, Bonds DE, Church TS, et al. Effect of structured physical activity on prevention of major mobility disability in older adults: the LIFE study randomized clinical trial. JAMA. 2014;311:2387–96.
Travier N, Velthuis MJ, Steins Bisschop CN, van den Buijs B, Monninkhof EM, Backx F, et al. Effects of an 18-week exercise programme started early during breast cancer treatment: a randomised controlled trial. BMC Med. 2015;13:121.
Hayes SC, Rye S, Disipio T, Yates P, Bashford J, Pyke C, et al. Exercise for health: a randomized, controlled trial evaluating the impact of a pragmatic, translational exercise intervention on the quality of life, function and treatment-related side effects following breast cancer. Breast Cancer Res Treat. 2013;137:175–86.
van Waart H, Stuiver MM, van Harten WH, Geleijn E, Kieffer JM, Buffart LM, et al. Effect of low-intensity physical activity and moderate- to high-intensity physical exercise during adjuvant chemotherapy on physical fitness, fatigue, and chemotherapy completion rates: results of the PACES randomized clinical trial. J Clin Oncol. 2015;33:1918–27.
Duijts SFA, van Beurden M, Oldenburg HSA, Hunter MS, Kieffer JM, Stuiver MM, et al. Efficacy of cognitive behavioral therapy and physical exercise in alleviating treatment-induced menopausal symptoms in patients with breast cancer: results of a randomized, controlled, multicenter trial. J Clin Oncol. 2012;30:4124–33.
Guillon M, Rochaix L, Dupont J-CK. Cost-effectiveness of interventions based on physical activity in the treatment of chronic conditions: a systematic literature review. Int J Technol Assess Health Care. 2018;34:481–97.
Roine E, Roine RP, Räsänen P, Vuori I, Sintonen H, Saarto T. Cost-effectiveness of interventions based on physical exercise in the treatment of various diseases: a systematic literature review. Int J Technol Assess Health Care. 2009;25:427–54.
Eyl RE, Xie K, Koch-Gallenkamp L, Brenner H, Arndt V. Quality of life and physical activity in long-term (≥ 5 years post-diagnosis) colorectal cancer survivors - systematic review. Health Qual Life Outcomes [Internet] 2018 [cited 2019 Nov 23];16. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5984808/
Wolin KY, Yan Y, Colditz GA, Lee I-M. Physical activity and colon cancer prevention: a meta-analysis. Br J Cancer. 2009;100:611–6.
Coups EJ, Park BJ, Feinstein MB, Steingart RM, Egleston BL, Wilson DJ, et al. Physical activity among lung cancer survivors: changes across the cancer trajectory and associations with quality of Life. Cancer Epidemiol Biomark Prev. 2009;18:664–72.
van Dongen JM, Persoon S, Jongeneel G, Bosmans JE, Kersten MJ, Brug J, et al. Long-term effectiveness and cost-effectiveness of an 18-week supervised exercise program in patients treated with autologous stem cell transplantation: results from the EXIST study. J Cancer Surviv. 2019;13:558–69.
Toohey K, Pumpa K, McKune A, Cooke J, DuBose KD, Yip D, et al. Does low volume high-intensity interval training elicit superior benefits to continuous low to moderate-intensity training in cancer survivors? World J Clin Oncol. 2018;9:1–12.
Edvardsen E, Skjønsberg OH, Holme I, Nordsletten L, Borchsenius F, Anderssen SA. High-intensity training following lung cancer surgery: a randomised controlled trial. Thorax. 2015;70:244–50.
Yan AF, Wang Y, Ng AV. Physical activity and annual medical outlay in U.S. colorectal, breast and prostate cancer survivors. Prev Med Rep. 2018;9:118–23.
Troeschel AN, Leach CR, Shuval K, Stein KD, Patel AV. Physical activity in cancer survivors during “re-entry” following cancer treatment. Prev Chronic Dis [Internet] 2018 [cited 2019 Nov 23];15. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5985854/
Sander AP, Wilson J, Izzo N, Mountford SA, Hayes KW. Factors that affect decisions about physical activity and exercise in survivors of breast cancer: a qualitative study. Phys Ther. 2012;92:525–36.
Clifford BK, Mizrahi D, Sandler CX, Barry BK, Simar D, Wakefield CE, et al. Barriers and facilitators of exercise experienced by cancer survivors: a mixed methods systematic review. Support Care Cancer. 2018;26:685–700.
Whitehead S, Lavelle K. Older breast cancer survivors’ views and preferences for physical activity. Qual Health Res. 2009;19:894–906.
Groen WG, van Harten WH, Vallance JK. Systematic review and meta-analysis of distance-based physical activity interventions for cancer survivors (2013–2018): We still haven’t found what we’re looking for. Cancer Treat Rev. 2018;69:188–203.
Goode AD, Lawler SP, Brakenridge CL, Reeves MM, Eakin EG. Telephone, print, and Web-based interventions for physical activity, diet, and weight control among cancer survivors: a systematic review. J Cancer Surviv. 2015;9:660–82.
Age Disparities Among patients in cancer clinical trials and patients with cancer in the general population - The ASCO Post [Internet]. [cited 2019 Nov 24];Available from: https://www.ascopost.com/News/60346
Geifman N, Butte AJ. Do Cancer clinical trial populations truly represent cancer patients? a comparison of open clinical trials to the Cancer Genome Atlas. Pac Symp Biocomput. 2016;21:309–20.
Kalata P, Martus P, Zettl H, Rödel C, Hohenberger W, Raab R, et al. Differences between clinical trial participants and patients in a population-based registry: the German Rectal Cancer Study vs. the Rostock Cancer Registry. Dis Colon Rectum. 2009;52:425–37.
Yabroff KR, Lund J, Kepka D, Mariotto A. Economic burden of cancer in the US: estimates, projections, and future research. Cancer Epidemiol Biomark Prev. 2011;20:2006–14.
Acknowledgements
Renato Mattli, Zurich University of Applied Sciences, Department of Health Economics, Gertrudstrasse 15, 8401 Winterthur, Switzerland; Sabine Klein, University of Zurich, Medical Library, Gloriastrasse 16, 8006 Zurich, Switzerland; Karen Linwood, University of Applied Science, Proofreader, Technikumstrasse 71, 8401 Winterthur
Funding
Open Access funding provided by Universität Zürich. This study was supported by the Swiss Cancer League (Krebsliga Schweiz).
Author information
Authors and Affiliations
Contributions
Conception and design: S. Rohrmann, M. Schwenkglenks, B. Gubler-Gut
Collection and assembly of data: B. E. Gubler-Gut, J. Pöhlmann
Data analysis and interpretation: B. E. Gubler-Gut, J. Pöhlmann
Author of manuscript: B. E. Gubler-Gut
Final approval of manuscript: All authors
Accountability for all aspects of the work: All authors
All authors contributed to the initiation, conceptualization and design of this systematic review. MS and SR led all phases of the systematic review; BEGG screened papers for inclusion and extracted all the data, synthesized the findings and drafted the manuscript. BEGG designed and ran the literature searches. BEGG and JP conducted data extraction. All authors revised the manuscript and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Systematic review—not applicable
Consent for publication
Approved by all authors
Competing interests
Dr. Aline Flatz is employed by Krebsliga Schweiz.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Matthias Schwenkglenks and Sabine Rohrmann shared last authorship.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gubler-Gut, B.E., Pöhlmann, J., Flatz, A. et al. Cost-effectiveness of physical activity interventions in cancer survivors of developed countries: a systematic review. J Cancer Surviv 15, 961–975 (2021). https://doi.org/10.1007/s11764-021-01002-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-021-01002-0