Abstract
Background
Lung cancer patients undergoing surgery are at increased risk for Venous thromboembolism (VTE). We monitored changes in perioperative coagulation status through Thrombo-elastography (TEG), and monitored the anticoagulant effect of low molecular weight heparin through TEG for the first time.
Methods
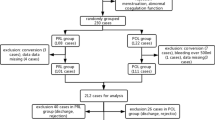
From July 2019 to January 2020, 207 patients receiving curative surgery were retrospectively screened. and 23 patients were excluded because they did not meet the inclusion criteria. Blood samples were required at three time points (prior to, the first and third day after surgery). Some patients were administrated nadroparin calcium daily from the first day after surgery. Repeated measures ANOVA and Chi-square test were used to analyze the coagulation states variation. To balance the confounders, propensity score matching (PSM) was used to determine the differences of coagulation states between patients with or without Low-molecular-weight heparin (LMWH) prophylaxis.
Results
In 184 patients, TEG parameters displayed significant procoagulant changes after lung surgery but conventional coagulation tests exhibited paradoxical trends. There were 6.5% (12/184) of patients identified as hypercoagulability before surgery. According to TEG results, the proportion of patients with hypercoagulability rose from 21.7% to 25% postoperatively, but more were classified into platelet or mixed hypercoagulability at third day compared with that at first day (3.8% vs 14.1%, P < 0.001). By PSM analysis, there were no significant differences in the proportion of hypercoagulable patients postoperatively between chemoprophylactic and nonprophylactic group.
Conclusions
TEG was eligible to distinguish changing states of hypercoagulability postoperatively and indicate the role of platelet in blood hypercoagulability. Administration of postoperative LMWH prophylaxis showed little mitigation on hypercoagulable states.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Venous thromboembolism (VTE), which consists of deep vein thrombosis (DVT) and pulmonary embolism (PE), presents as a major life-threatening complication that contributes to increasing morbidity and mortality [1]. Patients undergoing oncological surgery were considered to be at high risk of postoperative VTE [2]. Malignant patients often experienced considerable thromboembolic disorders and procoagulant changes following surgical operation [3], which is believed to facilitate the formation of venous thrombi [4]. Therefore, surveillance of coagulation state during perioperative phrases are necessary for overall acknowledgement of patient’s hemostatic change and dynamics in thrombotic risk, which is beneficial for improving healthcare of this complication.
Thromboglothiography (TEG) was originally invented by Hartert and is described as a sensitive blood coagulation test that analyzes the kinetics of clot formation, from the initial fibrin thread to fibrinolysis. TEG is used to assess the overall coagulation kinetics and strength of whole blood and has been successfully used clinically to detect hypercoagulable states [5,6,7]. It takes the coagulation factors, fibrinogen and platelet into account in the process of natural coagulation in vitro. This test minimizes the impact of shortage in dynamic interaction of various procoagulant factors (platelets especially) in clot formation, which is the inherent defect in conventional coagulation tests that introduce only plasma-based specimen. As a viscoelastic method, TEG results unscramble the real-time functional state of patients’ coagulation and fibrinolysis system, and has been used in assessing hypercoagulability or impaired coagulability in many circumstances like pregnancy, sepsis, severe injury [8]. Additionally, there is a potential application of TEG in assessing hypercoagulation following surgery [9].
Low-molecular-weight heparin (LMWH) is recommended as standard chemoprophylaxis for patients undergoing cancer surgery, but the utilization of proper prophylactic strategy was underperformed, including insufficient administrative dose and lack of extended chemoprophylaxis in China, which was considered to be due to inappropriate recognition of high-risk patients and scruple about bleeding risk caused by anticoagulation [10]. Even LMWH was recognized to reduce the risk of postoperative VTE, it was found that patients receiving LMWH thromboprophylaxis still develop VTE [11]. A randomized study, that compared the prophylactic effect of high- and low-dose LMWH in patients undergoing lung surgery, showed that even a high dose administration did not provide adequate prophylactic effect [12]. On the other hand, a new meta-analysis indicated that in patients with lung cancer, the reduction of VTE risk rendered by LMWH was accompanied by an increasement in bleeding risk at the meantime [13]. Therefore, monitoring the effectiveness of postoperative prophylactic LMWH is necessary for individualized chemoprophylaxis appropriate for patients with different VTE risk stratification to optimize the outcomes. Currently, there were no formal recommendations of monitoring solutions. Anti-Xa activity and prothrombin fragment F1 + 2 have been used in monitoring the dosage of LMWH [14], but these assays are not routinely tested in clinical practice and displayed inconsistent reliability. TEG, as a rapid and cost-efficient test, has been implemented in cardiovascular surgery and proved to facilitate improved individual anticoagulation management [15, 16]. Previous study showed that enoxaparin sodium exhibited a dose-dependent inhibition of clot formation on TEG tracing [17]. Thus, we assumed that the potency of TEG in monitoring the effects of LMWH on blood coagulation for lung cancer surgery could be highlighted.
In this study, we aimed to figure out how the coagulation profile changes after curative surgery in lung cancer patients by means of TEG, and to investigate the influence of postoperative LMWH administration on coagulation status for thrombophylactic purpose.
Materials and methods
Population and material
In this study, patients with primary lung cancer hospitalized for surgery were retrospectively studied from July 2019 to January 2020. The exclusion criteria listed as (1) any anticoagulation or anti-platelet therapy within 30 days before surgery; (2) malignancy history or neoadjuvant chemotherapy/radiotherapy before surgery; (3) VTE event prior to surgery; (4) lack of necessary data. All eligible patients received radical surgery under general anesthesia. Venous ultrasound of lower limbs was performed postoperatively in order to detect DVT, and patients suspected of PE with clinical symptoms were arranged to computer tomography pulmonary angiography (CTPA). Patients given postoperative VTE chemoprophylaxis received subcutaneous nadroparin calcium (10,250 WHO Unit/mL) every night from the first day postoperative until discharge and the dose was calculated according to weight, ranging from 0.3 mL to 0.6 mL in our practice. All patients were given gradient compress stocking during operation and early days after surgery until they were allowed to off-bed activity.
Blood tests at three time points were needed (baseline prior to surgery, the first and third day postoperatively) for all included patients. The clinical data (age, gender, body mass index, smoking history, chronical disease including hypertension, coronary heart disease, diabetes mellitus, chronical pulmonary disease, surgical information, histological type, anticoagulation information, VTE event) and blood tests results were obtained from electronical medical database. The pathological stage of lung cancer was determined according to 8th edition IASLC classification of TNM staging [18]. All patients were followed until discharge. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2000). Patient consents were waived because of the retrospective nature. This research has been approved by hospital ethical commitment board (KY2023-111-02).
Laboratory measurement
Blood samples were collected via venipuncture in forearm and were delivered to automated analysis in the laboratory within 1 h after sampling. For patients receiving LMWH, the blood sample was obtained after subcutaneous injection of nadroparin calcium. TEG assay was performed on citrated sample by the TEG® 5000 Thromboelastograph® Hemostasis Analyzer System activated by kaolin and 20 μL of calcium chloride. We collected TEG parameters including reaction time (R, the time from the onset of test to the first detectable formation of clot), kinetics (K, the time from the clotting to the formation at certain strength level of 20 mm in amplitude), α angle (the angle between the baseline and the imaginary tangent line to the curve), maximum amplitude (MA, maximal amplitude of the TEG curve), and other conventional coagulation tests including international normalized ratio (INR), fibrinogen, platelet, D-dimer concentration.
The hypercoagulative state was categorized into three types according to the manufacturer: (1) enzymatic hypercoagulability, R < 5 min or α angle > 72° or K < 1 min, and MA ≤ 70 mm; (2) platelet hypercoagulability, R ≥ 5 min, α angle ≤ 72°, K ≥ 1 min, and MA > 70 mm; (3) mixed hypercoagulability, R < 5 min or α angle > 72° or K < 1 min, and MA > 70 mm.
Statistical methods
The data were expressed as mean ± standard derivation, median with interquartile range, or ratio according to their statistical distribution. Repeated measures one-way ANOVA to detect the variation of laboratory measurements perioperatively, and if sphericity was not assumed, the results were then modified by Greenhouse–geisser method. Spearman’ s correlation was applied to test correlation between TEG and conventional coagulation parameters. Chi-square test and Fisher’s exact test were performed accordingly to compare the different proportion of three types of hypercoagulability at three time points and to determine the relationship between hypercoagulative state and anticoagulation therapy. For the purpose to balance the distribution of patient characteristic (age, sex, pathological staging, postoperative hospital stay) and surgical procedure (surgical approach, surgical time), we used propensity score matching (PSM) with a caliper less than 0.02 to select patients from those without postoperative LMWH prophylaxis to match those receiving prophylaxis. The propensity score was calculated from logistic regression model incorporating potential confounders. As a reminder, patients with therapeutic administration of LMWH after established VTE were beforehand excluded. Two-tailed P-value < 0.05 of each test was considered statistically significant throughout the study. All data were statistically processed using IBM SPSS statistics version 26.0 (Armonk, NY: IBM Corp).
Results
Population characteristics
From July 2019 to January 2020, a total of 207 patients were screened. Twenty-three patients did not meet our inclusion criteria and were excluded: (1) Seven patients received anticoagulant or antiplatelet therapy within 30 days before surgery; (2) Three patients had a history of malignancy or neoadjuvant chemotherapy/radiotherapy before surgery; (3) Five patients had venous thromboembolism before surgery; (4) 8 patients lacked necessary data. After exclusion, 184 eligible patients were finally enrolled for analysis (Table 1). The average age of patients when admitted into hospital was 58.7 ± 9.7, and 39.7% of the population was male. Most patients were taken to video-assisted thoracoscopic surgery (VATS) and the other 18 (9.8%) patients undergone thoracotomy. Lobectomy and sublobar resection were considered as most common surgical procedure and only 3 (1.6%) patients received pneumonectomy. In terms of pathological type, adenocarcinoma (87.0%) accounted for the major type of lung cancer, and 10 (9.8%) patients were diagnosed as squamous cell carcinoma. Until discharge, 11 patients (6.0%) were found VTE, and all these VTE events were DVT.
Variation of perioperative laboratory results
In whole population, the ANOVA analysis illustrated significant changes compared to preoperative baseline for all parameters (Fig. 1). In terms of TEG variables, the decrease of R and K as well as the increase of MA and α angle indicated a tendency toward hypercoagulable state after surgery, while the conventional coagulation tests showed paradoxical trends, in which the hypo-coagulation was indicated by the INR dropping and hypercoagulation by fibrinogen and D-dimer elevating.
Correlations of measures of coagulation
Analysis revealed some significant correlation between TEG and conventional measures of hemostasis (Table 2). The fibrinogen and platelet were significantly correlated with MA (r = 0.44–0.51, P < 0.05), and other correlations were deemed as trivial and insignificant.
Changes of perioperative coagulation status
The baseline status of coagulation of whole population before surgery was virtually within normal range indicated by TEG (Fig. 2). Only 12 (6.5%) were classified as hypercoagulability, 11 of whom were enzymatic hypercoagulability. At the first day after surgery, the proportion of patients with hypercoagulable states significantly increased compared to baseline (21.7% vs 6.5%, P < 0.001), but most of them (33/40) were still classified into enzymatic hypercoagulability according to TEG references. At the third day, patients with hypercoagulable states took up 25% of the whole population and 14.1% were platelet or mixed hypercoagulability where platelet played an essential role.
Differences in coagulation status between chemoprophylaxis and no-chemoprophylaxis group
The PSM analysis selected 37 pairs of patients (Table 3) with balanced baseline clinical characteristics (Supplement 1). After PSM, 1 of 37 patients (2.7%) who received LWMH developed VTE, whereas 2 of 37 patients (5.4%) who did not receive LWMH developed VTE. There was no statistically significant difference between the two groups (Fig. 3).The coagulation state was identical before surgery between two groups. At the first day after surgery, 24.3% patients (n = 9) receiving LWMH prophylaxis were identified as hypercoagulability, which was significantly higher compared to that before surgery, and the number is 10 at the third day postoperatively. In patients without prophylaxis, 6 patients were found hypercoagulability at first day and the number doubled at third day. But the difference in the proportion of hypercoagulable patients between two groups reached no statistical significance at both time points postoperatively (P = 0.386; P = 0.611, respectively).
Discussion
This study revealed a hypercoagulative trend among patients after lung cancer resection and demonstrated that there were significantly diverse states of hypercoagulability following surgery by means of TEG measurement, in which the proportion of platelet-dominated hypercoagulability prevailed gradually after surgery. PSM analysis indicated that administration of LMWH prophylaxis was not associated with significant mitigation in patient procoagulant state after surgery.
Conventional coagulation tests have been used for surveillance for decades but manifesting suboptimal ability in revealing coagulation function for surgery patients [9, 19]. In this study, all incorporated TEG parameters mutually verified that there was a procoagulant tendency after lung cancer surgery, but conventional coagulation tests exhibited paradoxical changes. Mao and colleagues performed TEG and conventional coagulation tests on patients with DVT and healthy controls, and they discovered that a hypercoagulable tendency was found by TEG not by conventional coagulation tests like APTT, PT or platelet [20]. In our study, INR, which is the calculation generated from the PT, also showed undesired ability to indicate postoperative hypercoagulative status. Consistently, another research also proved that PT and APTT were underpowered in revealing significant hypercoagulable state [21]. INR tests are performed in platelet-free blood sample, which means it is ineligible to vindicate the role of cell surface in the coagulation course. INR is in alignment with fibrin generation, reflecting the number and function of particular coagulation factors (prothrombin, FV, FVII and FX), therefore, the dropping of INR in early days of post-operation may associate with the consumption of coagulation factors during surgery. However, it is not necessary to show the hypocoagulative state given that INR represent incomplete measurement of clot formation [5].
Contrary, TEG can unfold more information about the phases of clot formation based on whole blood, including activation of coagulation cascade, thrombin generation, platelet activation and aggregation [18]. TEG was able to identify hypercoagulability in colorectal and prostate cancer [9, 22]. As for lung cancer, Davies et al. found that some parameters in rotational thromboelastometry (ROTEM) that is similar to TEG test were significantly different in lung cancer patients compared to health controls [23]. Nevertheless, these researches defined hypercoagulation by using few parameters and had not assessed the dynamic changes of these parameters, which underutilized of TEG in assessing overall aspects of blood coagulation status. In our study, individual coagulation state and the defined hypercoagulability were set down by incorporating a wide panel of TEG parameters according to their normal range, which provided full-scale assessment of coagulation conditions and was more applicable in clinical practice.
It is very necessary to emphasize that the VTE risk differs significantly among individuals, also, the risk profile can be dynamically changed within the same patient over time. The surveillance the changes of coagulation state of patients undergoing surgery can shed insight into surgery-induced coagulation system fluctuation, promoting the understanding of the true course of thrombosis complication [24]. Surgical operation introduces traumatic stress but removes the tumor load, which represents a shortened impact on patient hematologic system instead of a prolonged effect that is more common in multi-period chemotherapy, so the risk of VTE seems to predominantly occur within the initial postoperative time [25]. Notably, the bleeding risk at the early period after surgery can be simultaneously higher, which may baffle the healthcare management in balancing the VTE risk and bleeding risk, so elaborate surveillances of coagulation state during the limited time widow of hypercoagulability should be prioritized.
According to the classification of TEG reference, the hypercoagulable state was divided into three different types, including enzymatic, platelet and mixed hypercoagulability. At the early days after surgery, the proportion of patients with platelet or mixed hypercoagulability raised significantly from 3.8% to 14.1%, and both hypercoagulable states meant that MA was higher than upper limit. At the same time, MA was significantly elevated compared to baseline. MA reflects the strength of clot that depends on platelet concentration and function as well as platelet-fibrinogen cross-link in the clot formation. As shown in this study, platelet displayed a decent correlation with MA. Platelet concentration exhibited a trend that was downside at the first day and rebounded at the third day postoperatively, which corresponded to the alteration of distribution in hypercoagulability. Apart from quantifying concentration to justify the role of platelet in the coagulation process, the contribution of platelet to procoagulant state can be more validated by their hyperactivation in the hemostasis process [26]. Study utilizing ROTEM suggested that testing array incorporating platelet contribution are more recommendable to detect hypercoagulation [27]. Similarly, a higher MA in TEG tracing is associated with enhanced platelets adherence and aggregation that lead to intensive strength of clot formation. These results suggested that in the early period, activated platelet played an important role in postoperative hypercoagulative state among lung cancer patients.
Although the pathophysiologic theory underlying the prothrombotic state for cancer patients remains unsolved, several mechanisms concerning platelets activation have been proposed and there are growing recognition of platelet contribution to cancer associated venous thrombosis [28]. Cancer cell can initiate the coagulation cascade by upgrading the secretion of tissue factor (TF), which leads to thrombin generation and platelets activation [29]. Cancer cell can also directly stimulate platelets by releasing platelet activation receptor or providing binding site for platelet aggregation [30]. In lung cancer patients receiving chemotherapy, platelets had enhanced phosphatidylserine exposure and elevated secretion of platelet-derived microparticle compared to health controls, which suggested that platelets obtained increased procoagulant activity after chemotherapy [31]. Surgery also represents as an important driver to increase prothrombotic risk. Surgical patients typically experienced blood stasis, endothelial damage and inflammation perioperatively. These predisposed clinical conditions were responsible for thrombin generation, release of vascular cell-derived microparticles and upregulation of platelet adherence molecules, all of which induced platelets activation [32]. As found in our study, a substantial proportion of patients were haunted by platelet-relevant hypercoagulability at the early period after lung cancer surgery. It is noticed that curative resections have removed tumor, therefore, provoked platelets should be blamed on the surgical intervene that introduces direct impact on blood system, which exactly reflects the early alteration of hypercoagulation patterns.
Most international guidelines recommended the use of prophylaxis dose of LMWH in patients undergoing cancer surgery to prevent postoperative VTE [33,34,35]. Prevention strategy involving LMWH was illustrated to reduce the occurrence of VTE among ambulatory patients with lung cancer [36]. However, a randomized trial discovered significantly differences of individual sensitivity of heparin and suggested that a fixed dosage of heparin administration might not provide sufficient anticoagulation for thromboprophylaxis postoperatively [16]. Even receiving LMWH thromboprophylaxis, some patients still develop VTE [11]. In a recent meta-analysis, it showed that for surgical patients, the benefit of VTE chemoprophylaxis was found only among specific group of patients [37]. In our PSM analysis, the small gaps of hypercoagulable state between patients with and without prophylactic administration of LMWH also indicated its incompetence to alleviate prothrombotic stress. Surgery has extended influence on coagulation function and integrity of vascular endothelial cell. Normally, injury to vascular wall during surgery exposes collagen and then triggers platelet activation to reconstruct vascular integrity, but meanwhile, subsequent secretion of platelet factor 4 from activated platelets has a strong binding ability to heparin, which could repress the heparin dependent anticoagulation with antithrombin III [38]. Even LMWH primary inhibits coagulation factor Xa, it still has extended effects on other coagulation factors in the coagulation cascade, which can affect subsequent platelet activation. But in our study, TEG results suggested that activated platelet still dampened the thromboprophylaxis efficacy of LMWH. Further explanation about the mechanism that activated platelet interrupted the anticoagulation effect of LMWH should be addressed. But before that, it was proclaimed that the platelet activation in clot formation need to be aggressively guided by TEG during prophylactic treatment [39].
In the LMWH group, the number of hypercoagulable patients increased from 9 to 10 following surgery (Table 3), but there were higher proportion of platelet-associated hypercoagulation in hypercoagulable patients at the third day (8/10) compared to that at first day (2/9) after surgery, in the meantime, the proportion of enzymatic hypercoagulation dropped. Even the sample size was small, it was conjectured that even enzymatic hypercoagulation still existed in some patients after anticoagulation, it was useful in reducing hazard of the enzymatic hypercoagulation in clot formation on TEG. Normally, the dubious anticoagulation effectiveness that reflected the insufficiency of prophylaxis can be indicative of higher dose of LMWH [12]. However, the emerging of elevated proportion of platelet hypercoagulation may indicate a lack of thromboprophylaxis by solely adopting anti-thrombogenesis strategy, whereupon the hypercoagulative state sustains [40]. Currently, anti-platelet agents were mostly utilized in preventing artery embolization, venous thromboprophylaxis by means of anti-platelet strategy like aspirin was currently applied only for orthopaedic surgery. As for cancer patients, the use of LMWH represents the current standard prevention for VTE, whereas aspirin remained controversial and lacked for robust evidence for clinical application to reduce thrombotic risk [41]. Even some new anti-platelet agent targeting different platelet ligands was found to effectively inhibit platelet activity without significantly increasing hemorrhage tendency [42, 43], the bleeding risk was still the essential factor that impeded further utilization of anti-platelet in VTE prevention. Overall, viewing the dynamic pattern of hypercoagulable status after lung cancer surgery, we thought that current anticoagulation protocol by mere LMWH was seemingly insufficient, and the combination of anti-platelet therapy may be of additional value for reducing the prothrombotic stress among surgical patients.
Current study has certain limitations that hindered some conclusive interpretations. First, we were unable to investigate the relationship between hypercoagulability and LMWH administration by a randomized method, but we applied PMS to narrow the impact of confounders between groups as possible. Mechanical and pharmacological prophylaxis were most important strategies in VTE prevention. In this study, all patients received standard perioperative mechanical prevention by compress stocking and early mobilization, therefore, there was a reasonable perspective that the changes of coagulation status reflected the real effectiveness of chemoprophylactic LMWH. Second, the number of patients was relatively small, and they were primarily among those with early-stage non-small cell lung cancer diagnosed as adenocarcinoma, which may introduce some biases. Finally, the lack of prolonged monitoring of TEG is another limitation, and yet current results still uncovered significant variation of hypercoagulability based on limited period of monitoring.
Conclusions
This study tested that TEG results disclosed significantly different hypercoagulative states at different time points in the early period postoperatively, in which the role of platelets cannot be neglected. Also, TEG results found no distinguishably alleviated hypercoagulability in patient with postoperative prophylactic LMWH, which indicated insufficient thromboprophylaxis and warranted extra efforts in determine more efficient VTE prevention strategy. Even more studies based on prospective protocol among larger cohorts are needed, our results were promising to indicate that TEG is an effective tool to stratify various prothrombotic risk at different time points. By incorporating full panel of parameters, TEG can be conductive to monitoring of anticoagulation efficacy when developing proper thromboprophylaxis strategy in further investigations.
Data availability
The data sets used and analyzed in this study are available from the corresponding author on reasonable request.
References
Trinh V, Karakiewicz P, Sammon J, Sun M, Sukumar S, Gervais M, et al. Venous thromboembolism after major cancer surgery: temporal trends and patterns of care. JAMA Surg. 2014;149:43–9. https://doi.org/10.1001/jamasurg.2013.3172.
Silverstein M, Heit J, Mohr D, Petterson T, O’Fallon W, Melton L. Trends in the incidence of deep vein thrombosis and pulmonary embolism: a 25-year population-based study. Arch Intern Med. 1998;158:585–93. https://doi.org/10.1001/archinte.158.6.585.
Osborne N, Wakefield T, Henke P. Venous thromboembolism in cancer patients undergoing major surgery. Ann Surg Oncol. 2008;15:3567–78. https://doi.org/10.1245/s10434-008-0151-4.
Abdol Razak N, Jones G, Bhandari M, Berndt M, Metharom P. Cancer-associated thrombosis: an overview of mechanisms, risk factors, and treatment. Cancers (Basel). 2018. https://doi.org/10.3390/cancers10100380.
Akay OM, Ustuner Z, Canturk Z, Mutlu FS, Gulbas Z. Laboratory investigation of hypercoagulability in cancer patients using rotation thrombelastography. Med Oncol. 2009;26(3):358–64. https://doi.org/10.1007/s12032-008-9129-0.
McCrath DJ, Cerboni E, Frumento RJ, Hirsh AL, Bennett-Guerrero E. Thromboelastography maximum amplitude predicts postoperative thrombotic complications including myocardial infarction. Anesth Analg. 2005;100(6):1576–83. https://doi.org/10.1213/01.ANE.0000155290.86795.12.
Bischof D, Dalbert S, Zollinger A, Ganter MT, Hofer CK. Thrombelastography in the surgical patient [published correction appears in Minerva Anestesiol. 2010;76(5):383. Gantner MT [corrected to Ganter MT]. Minerva Anestesiol. 2010;76(2):131–137.
Walsh M, Moore E, Moore H, Thomas S, Lune S, Zimmer D, et al. Use of viscoelastography in malignancy-associated coagulopathy and thrombosis: a review. Semin Thromb Hemost. 2019;45:354–72. https://doi.org/10.1055/s-0039-1688497.
Toukh M, Siemens D, Black A, Robb S, Leveridge M, Graham C, et al. Thromboelastography identifies hypercoagulablilty and predicts thromboembolic complications in patients with prostate cancer. Thromb Res. 2014;133:88–95. https://doi.org/10.1016/j.thromres.2013.10.007.
Zhai Z, Kan Q, Li W, Qin X, Qu J, Shi Y, et al. VTE risk profiles and prophylaxis in medical and surgical inpatients: the identification of Chinese hospitalized patients’ risk profile for venous thromboembolism (DissolVE-2)-a cross-sectional study. Chest. 2019;155:114–22. https://doi.org/10.1016/j.chest.2018.09.020.
Simonneau G, Sors H, Charbonnier B, Page Y, Laaban JP, Azarian R et al. A comparison of low-molecular-weight heparin with unfractionated heparin for acute pulmonary embolism. The THESEE Study Group. Tinzaparine ou Heparine Standard: Evaluations dans l’Embolie Pulmonaire. N Engl J Med 1997;337: 663–69. https://doi.org/10.1056/NEJM199709043371002
Attaran S, Somov P, Awad WI. Randomised high- and low-dose heparin prophylaxis in patients undergoing thoracotomy for benign and malignant disease: effect on thrombo-elastography. Eur J Cardiothorac Surg. 2010;37:1384–90. https://doi.org/10.1016/j.ejcts.2009.12.027.
Yu Y, Lv Q, Zhang B, Lan F, Dai Y. Adjuvant therapy with heparin in patients with lung cancer without indication for anticoagulants: a systematic review of the literature with meta-analysis. J Cancer Res Ther. 2016;12:37–42. https://doi.org/10.4103/0973-1482.191627.
Croles FN, Lukens MV, Mulder R, de Maat MPM, Mulder AB, Meijer K. Monitoring of heparins in antithrombin-deficient patients. Thromb Res. 2019;175:8–12. https://doi.org/10.1016/j.thromres.2019.01.007.
Vonk AB, Veerhoek D, van den Brom CE, van Barneveld LJ, Boer C. Individualized heparin and protamine management improves rotational thromboelastometric parameters and postoperative hemostasis in valve surgery. J Cardiothorac Vasc Anesth. 2014;28:235–41. https://doi.org/10.1053/j.jvca.2013.09.007.
Veerhoek D, Groepenhoff F, van der Sluijs M, de Wever JWB, Blankensteijn JD, Vonk ABA, et al. Individual differences in heparin sensitivity and their effect on heparin anticoagulation during arterial vascular surgery. Eur J Vasc Endovasc Surg. 2017;54:534–41. https://doi.org/10.1016/j.ejvs.2017.07.006.
Zmuda K, Neofotistos D, Ts’ao CH. Effects of unfractionated heparin, low-molecular-weight heparin, and heparinoid on thromboelastographic assay of blood coagulation. Am J Clin Pathol. 2000;113:725–31. https://doi.org/10.1309/Q4AE-BMCW-CQ7J-NUVT.
Detterbeck FC, Boffa DJ, Kim AW, Tanoue LT. The eighth edition lung cancer stage classification. Chest. 2017;151(1):193–203. https://doi.org/10.1016/j.chest.2016.10.010
Park M, Martini W, Dubick M, Salinas J, Butenas S, Kheirabadi B et al. Thromboelastography as a better indicator of hypercoagulable state after injury than prothrombin time or activated partial thromboplastin time. J Trauma 2009;67:266–75; discussion 275–266. https://doi.org/10.1097/TA.0b013e3181ae6f1c
Mao C, Xiong Y, Fan C. Comparison between thromboelastography and conventional coagulation assays in patients with deep vein thrombosis. Clin Chim Acta. 2021;520:208–13. https://doi.org/10.1016/j.cca.2021.06.019.
Park MS, Martini WZ, Dubick MA, Salinas J, Butenas S, Kheirabadi BS et al. Thromboelastography as a better indicator of hypercoagulable state after injury than prothrombin time or activated partial thromboplastin time. J Trauma 2009; 67: 266–275; discussion 275–266. https://doi.org/10.1097/TA.0b013e3181ae6f1c
Ustuner Z, Akay OM, Keskin M, Kus E, Bal C, Gulbas Z. Evaluating coagulation disorders in the use of bevacizumab for metastatic colorectal cancer by thrombelastography. Med Oncol. 2012;29:3125–8. https://doi.org/10.1007/s12032-012-0274-0.
Davies NA, Harrison NK, Sabra A, Lawrence MJ, Noble S, Davidson SJ, et al. Application of ROTEM to assess hypercoagulability in patients with lung cancer. Thromb Res. 2015;135:1075–80. https://doi.org/10.1016/j.thromres.2015.03.021.
Christensen T, Vad H, Pedersen S, Licht P, Nybo M, Hornbech K, et al. Video-assisted Thoracoscopic surgery (VATS) lobectomy for lung cancer does not induce a procoagulant state. Thromb J. 2017;15:29. https://doi.org/10.1186/s12959-017-0152-2.
Christensen TD, Vad H, Pedersen S, Hvas AM, Wotton R, Naidu B, et al. Venous thromboembolism in patients undergoing operations for lung cancer: a systematic review. Ann Thorac Surg. 2014;97:394–400. https://doi.org/10.1016/j.athoracsur.2013.10.074.
Van Der Meijden P, Van Schilfgaarde M, Van Oerle R, Renné T, ten Cate H, Spronk H. Platelet- and erythrocyte-derived microparticles trigger thrombin generation via factor XIIa. J Thromb Haemost. 2012;10:1355–62. https://doi.org/10.1111/j.1538-7836.2012.04758.x.
Hincker A, Feit J, Sladen R, Wagener G. Rotational thromboelastometry predicts thromboembolic complications after major non-cardiac surgery. Crit Care. 2014;18:549. https://doi.org/10.1186/s13054-014-0549-2.
Abdol Razak NB, Jones G, Bhandari M, Berndt MC, Metharom P. Cancer-associated thrombosis: an overview of mechanisms, risk factors, and treatment. Cancers (Basel) 2018; 10. https://doi.org/10.3390/cancers10100380
Hisada Y, Mackman N. Cancer-associated pathways and biomarkers of venous thrombosis. Blood. 2017;130:1499–506. https://doi.org/10.1182/blood-2017-03-743211.
Suzuki-Inoue K. Platelets and cancer-associated thrombosis: focusing on the platelet activation receptor CLEC-2 and podoplanin. Blood. 2019;134:1912–8. https://doi.org/10.1182/blood.2019001388.
Ma R, Bi Y, Kou J, Zhou J, Shi J. Enhanced procoagulant activity of platelets after chemotherapy in non-small cell lung cancer. Cancer Biol Ther. 2017;18:627–34. https://doi.org/10.1080/15384047.2017.1345387.
Riondino S, Ferroni P, Zanzotto FM, Roselli M, Guadagni F. Predicting VTE in cancer patients: candidate biomarkers and risk assessment models. Cancers (Basel). 2019. https://doi.org/10.3390/cancers11010095.
Farge D, Frere C, Connors JM, Ay C, Khorana AA, Munoz A, et al. 2019 international clinical practice guidelines for the treatment and prophylaxis of venous thromboembolism in patients with cancer. Lancet Oncol. 2019;20:e566–81. https://doi.org/10.1016/S1470-2045(19)30336-5.
Lyman GH, Bohlke K, Khorana AA, Kuderer NM, Lee AY, Arcelus JI, et al. Venous thromboembolism prophylaxis and treatment in patients with cancer: American Society of clinical oncology clinical practice Guideline Update 2014. J Clin Oncol. 2015;33:654–6. https://doi.org/10.1200/JCO.2014.59.7351.
Mandala M, Falanga A, Roila F, Group EGW. Management of venous thromboembolism (VTE) in cancer patients: ESMO Clinical Practice Guidelines. Ann Oncol 2011;22 Suppl 6:vi85–92. https://doi.org/10.1093/annonc/mdr392.
Fuentes HE, Oramas DM, Paz LH, Casanegra AI, Mansfield AS, Tafur AJ. Meta-analysis on anticoagulation and prevention of thrombosis and mortality among patients with lung cancer. Thromb Res. 2017;154:28–34. https://doi.org/10.1016/j.thromres.2017.03.024.
Pannucci CJ, Swistun L, MacDonald JK, Henke PK, Brooke BS. Individualized venous thromboembolism risk stratification using the 2005 Caprini score to identify the benefits and harms of chemoprophylaxis in surgical patients: a meta-analysis. Ann Surg. 2017;265:1094–103. https://doi.org/10.1097/SLA.0000000000002126.
Levy J, Sniecinski R, Welsby I, Levi M. Antithrombin: anti-inflammatory properties and clinical applications. Thromb Haemost. 2016;115:712–28. https://doi.org/10.1160/th15-08-0687.
Laubscher GJ, Lourens PJ, Venter C, Kell DB, Pretorius E. TEG((R)), microclot and platelet mapping for guiding early management of severe COVID-19 coagulopathy. J Clin Med. 2021. https://doi.org/10.3390/jcm10225381.
Gonzalez E, Kashuk J, Moore E, Silliman C. Differentiation of enzymatic from platelet hypercoagulability using the novel thrombelastography parameter delta (delta). J Surg Res. 2010;163:96–101. https://doi.org/10.1016/j.jss.2010.03.058.
Elwood PC, Pickering JE, Morgan G, Galante J, Weightman AL, Morris D, et al. Systematic review update of observational studies further supports aspirin role in cancer treatment: time to share evidence and decision-making with patients? PLoS One. 2018;13: e0203957. https://doi.org/10.1371/journal.pone.0203957.
Suzuki-Inoue K. Roles of the CLEC-2-podoplanin interaction in tumor progression. Platelets 2018: https://doi.org/10.1080/09537104.2018.1478401
Shirai T, Inoue O, Tamura S, Tsukiji N, Sasaki T, Endo H, et al. C-type lectin-like receptor 2 promotes hematogenous tumor metastasis and prothrombotic state in tumor-bearing mice. J Thromb Haemost. 2017;15:513–25. https://doi.org/10.1111/jth.13604.
Funding
This research received no funding.
Author information
Authors and Affiliations
Contributions
X-x Y, Y-sC and Lh-K collected and analyzed the patient data and were the major contributors in writing this manuscript. X-x Y, Y-sC and Lh-K participated in data collection and collation. B-W contributed to designing and critically revising the article. B-W contributed to the article review. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
All authors report no conflict of interest.
Institutional review board statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the ethics committee of Beijing Tiantan Hospital Affiliated with Capital Medical University.
Informed consent statement
The review board waived the need for patient consent, as this was a retrospective study, and all data had been deidentified.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yang, X., Cai, Y., Ke, L. et al. Hypercoagulable state and effect of low-molecular-weight heparin prophylaxis on coagulation after lung cancer resection: results from thrombo-elastography. Gen Thorac Cardiovasc Surg (2024). https://doi.org/10.1007/s11748-024-02062-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11748-024-02062-6