Abstract
Objectives
Video-assisted thoracic surgery (VATS) bullectomy is the mainstay treatment for primary spontaneous pneumothorax (PSP) but we encounter patients with pain due to chest tube. This study investigated the postoperative outcomes of shortened silicone drain as a chest tube after VATS bullectomy to reduce pain.
Methods
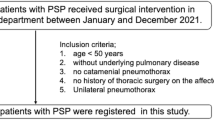
The current study included patients aged < 30 years who underwent VATS bullectomy for PSP. Patients with normal intrathoracic lengths of the silicone drain placed in a loop at the apex toward the diaphragm were categorized as Group L, whereas those with the silicone drain shortened to approximately 10 cm and placed toward the apex were classified as Group S. Postoperative pain evaluated using a numerical rating scale (NRS) and other perioperative outcomes were compared between the groups.
Results
Altogether, 43 patients were included, with 22 in Group L and 21 in Group S, respectively. The NRS before chest tube removal was significantly lower in Group S (mean, 2.1) than in Group L (4.4; p = 0.001). In Group L, 4 patients (p = 0.017) required early chest tube removal than expected due to severe pain whereas none in Group S required this intervention; additionally, more patients needed additional analgesics than in Group S (p = 0.003).
Conclusion
In VATS bullectomy for PSP, the pain intensity could be reduced by shortening the intrathoracic length of the silicone drain, compared to a longer intrathoracic length of the silicon drain. Our findings contribute to the establishment of optimal postoperative management of general thoracic surgery.


Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Bobbio A, Dechartres A, Bouam S, Damotte D, Rabbat A, Regnard JF, et al. Epidemiology of spontaneous pneumothorax: gender-related differences. Thorax. 2015;70:653–8.
Goto T, Kadota Y, Mori T, Yamashita S, Horio H, Nagayasu T, Iwasaki A. Video-assisted thoracic surgery for pneumothorax: republication of a systematic review and a proposal by the guideline committee of the Japanese association for chest surgery 2014. Gen Thorac Cardiovasc Surg. 2015;63:8–13.
Imperatori A, Rotolo N, Spagnoletti M, Festi L, Berizzi F, Di Natale D, et al. Risk factors for postoperative recurrence of spontaneous pneumothorax treated by video-assisted thoracoscopic surgery. Interact Cardiovasc Thorac Surg. 2015;20:647–52.
Hatz RA, Kaps MF, Meimarakis G, Loehe F, Müller C, Fürst H. Long-term results after video-assisted thoracoscopic surgery for first-time and recurrent spontaneous pneumothorax. Ann Thorac Surg. 2000;70:253–7.
Sedrakyan A, van der Meulen J, Lewsey J, Treasure T. Video assisted thoracic surgery for treatment of pneumothorax and lung resections: systematic review of randomised clinical trials. BMJ. 2004;329:1008.
Yamaguchi M, Yoshino I, Kameyama T, Osoegawa A, Tagawa T, Yohena T, Maehara Y. Use of small-bore silastic drains in general thoracic surgery. Ann Thorac Cardiovasc Surg. 2007;13:156–8.
Ishikura H, Kimura S. The use of flexible silastic drains after chest surgery: novel thoracic drainage. Ann Thorac Surg. 2006;81:331–3.
Tsuboshima K, Nagata M, Wakahara T, Matoba Y, Yamamoto M, Yamana H, Abe K, Oue H, et al. Propensity-score-matched comparison of postoperative pain between young and elderly patients who underwent video-assisted thoracoscopic surgery for spontaneous pneumothorax. Kyobu Geka. 2016; 69: 739–43 [written in Japanese].
Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res (Hoboken). 2011;63(Suppl 11):S240–52.
Yam MF, Loh YC, Tan CS, Khadijah Adam S, Abdul Manan N, Basir R. General pathways of pain sensation and the major neurotransmitters involved in pain regulation. Int J Mol Sci. 2018;19:2164.
Opitz I. Anatomy of the pleura. In: Locicero J, Colson YL, Feins RH, Rocco G, editors. Shield’s general thoracic surgery. 8th ed. Philadelphia: Wolters Kluwer; 2018. p. 706–11.
Minato T, Ishikura H, Kimura S. The experience of use silicon drain (blake drain) as a chest drainage and the later verification. Tokushima Red Cross Hosp Med J. 2010; 15: 144–7 [written in Japanese].
Kawaguchi Y, Hanaoka J, Hayashi K. Feasibility of early removal of chest tube in the operating room for spontaneous pneumothorax: a prospective randomized controlled study. Asian J Surg. 2021;44:339–44.
Igai H, Matsuura N, Numajiri K, Ohsawa F, Kamiyoshihara M. Feasibility of tubeless thoracoscopic bullectomy in primary spontaneous pneumothorax patients. Gen Thorac Cardiovasc Surg. 2023;71:138–44.
Acknowledgements
The authors would like to thank Enago (https://www.enago.jp/) for the English language review.
Funding
This work was supported by the Japan Society for the Promotion of Science, KAKENHI (grant number: JP20K17749).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kagimoto, A., Kamigaichi, A., Ishida, M. et al. Lessons from short chest drain management for primary spontaneous pneumothorax. Gen Thorac Cardiovasc Surg (2024). https://doi.org/10.1007/s11748-024-02039-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11748-024-02039-5