Abstract
Objectives
Lobes occasionally displace after lobectomy, referred to as “lobar shifting”. However, the benefits, especially in postoperative pulmonary function, remain controversial. This study aimed to measure the effect of lobar shifting on postoperative pulmonary function especially in the right upper lobe.
Methods
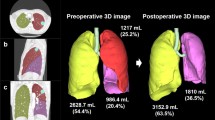
This retrospective study includes 273 right upper lobectomy patients (lobectomy group) and 24 right upper segmentectomy patients (segmentectomy group) from 2012 to 2021. The lobectomy group was further subdivided based on their Synapse Vincent® image: with their postoperative middle lobe bronchus shifted toward the head (shift group: 176 cases) and without (non-shift group: 97 cases). Several factors were examined to determine the cause of lobar shifting. The rate of measured actual postoperative forced expiratory volume in 1 s (FEV1.0) to predicted postoperative FEV1.0 was analyzed and compared among the three groups.
Results
Factors that correlated with lobar shifting included age (p < 0.001), a relatively small middle lobe volume (p = 0.03), no adhesions (p < 0.001), and good upper/middle and middle/lower lobulation (p = 0.04, p = 0.02). The rate of measured actual postoperative FEV1.0 to predicted postoperative FEV1 for the shift, non-shift, and segmentectomy groups were 112.5%, 107.9%, and 103.1% (shift vs non-shift: p = 0.04, shift vs segmentectomy: p = 0.02, non-shift vs segmentectomy: p = 0.19).
Conclusions
Lobar shifting after right upper lobectomy is influenced by morphological factors and may have a beneficial impact on postoperative pulmonary function.





Similar content being viewed by others

Data availability
No data was used for the research described in the article.
References
Saji H, Okada M, Tsuiboi M, Nakajima R, Suzuki K, Aokage K, et al. Segmentectomy versus lobectomy in small-sized peripheral non-small cell lung cancer (JCOG0802/WJOG4607L): a multicentre, open-label, phase 3, randomised, controlled, non-inferiority trial. Lancet. 2022;399:1607–17.
Choo-Won K, Alla G, Vineet RJ, Avraham M, Linda BH. Postlobectomy chest radiographic changes: a quantitative analysis. Can Assoc Radiol J. 2011;62:280–7.
Usuda K, Sagawa M, Aikawa H, Tanaka M, Machida Y, Ueno M, et al. Do Japanese thoracic surgeons think that dissection of the pulmonary ligament is necessary after an upper lobectomy? Surg Today. 2010;40:1097–9.
Nonaka M, Kadokura M, Michihata T, Inoue K, Takaba T. How different surgical methods of performing right upper lobectomy contribute to postoperative bronchial branching deformity: an experimental study. Surg Today. 1999;29:610–3.
Matsuoka H, Nakamura H, Nishio W, Sakamoto T, Harada H, Tsubota N. Division of the pulmonary ligament after upper lobectomy is less effective for the obliteration of dead space than leaving it intact. Surg Today. 2004;34:498–500.
Saji H, Inoue T, Kato Y, Shimada Y, Hagiwara M, Kudo Y, et al. Virtual segmentectomy based on high-quality three-dimensional lung modelling from computed tomography images. Interact Cardiovasc Thorac Surg. 2013;17:227–32.
Chan EG, Landreneau JR, Schuchert MJ, Odell DD, Gu S, Pu J, et al. Preoperative (3-dimensional) computed tomography lung reconstruction before anatomic segmentectomy or lobectomy for stage I non–small cell lung cancer. J Thorac Cardiovasc Surg. 2015;150:523–8.
Tane S, Nishikubo M, Kitazume M, Fujibayashi Y, Kimura K, Kitamura Y, et al. Cluster analysis of emphysema for predicting pulmonary complications after thoracoscopic lobectomy. Eur J Cardiothorac Surg. 2021;60:608–13.
Seok Y, Cho S, Lee JY, Yang HC, Kin K, Jheon S. The effect of postoperative change in bronchial angle on postoperative pulmonary function after upper lobectomy in lung cancer patients. Interact Cardiovasc Thorac Surg. 2014;18:183–9.
Ueda K, Tanaka T, Hayashi M, Tanaka N, Li TS, Hamano K. Clinical ramifications of bronchial kink after upper lobectomy. Ann Thorac Surg. 2012;93:259–65.
Nakazawa S, Shimizu K, Kawatani N, Obayashi K, Ohtaki Y, Nagashima T, et al. Right upper lobe segmentectomy guided by simplified anatomic models. JTCVS Techn. 2020;4:288–97.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None declared.
Date and number of IRB approval
G-304. December, 27, 2022.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kuroda, S., Miura, K., Shimizu, N. et al. The effect of lobar shifting following right upper lobectomy on postoperative pulmonary function. Gen Thorac Cardiovasc Surg (2024). https://doi.org/10.1007/s11748-024-02019-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11748-024-02019-9