Abstract
Objective
This study aims to examine whether cardiac surgery leads to symptom progression in the early postoperative period in patients with the peripheral arterial disease (PAD) and evaluate the difference between on-pump (OPCAB) and off-pump (ONCAB) coronary artery bypass graft surgery with regard to the symptom progression.
Methods
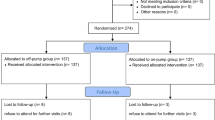
This retrospective study included one hundred consecutive adult patients with PAD at Fontaine stage 2b (pain-free walking distance less than 100 m) undergoing ONCAB and one hundred consecutive adult patients with PAD at Fontaine stage 2b (pain-free walking distance less than 100 m) undergoing OPCAB. Symptom progression was defined as the development of ischemic rest pain (Fontaine stage 3).
Results
In the first week after surgery, 12 patients in the OPCAB group and 53 patients in the ONCAB group had postoperative symptom progression (p < 0.001). Rest pain resolved in most of these patients on the 15th postoperative day. At the end of the second month, rest pain resolved in all patients. Logistic regression analysis revealed that cardiac surgery with CPB, ABI < 0.5, postoperative nadir hct levels ≤ 25%, and intraoperative tissue hypoxia were independently associated with postoperative symptom progression.
Conclusions
In summary, we found that cardiac surgery may lead to symptom progression in patients with severe claudication in the early postoperative period. Our results suggest that OPCAB may lead to lower rates of symptom progression compared to ONCAB.
Similar content being viewed by others
References
De Blasi RA, Tonelli E, Arcioni R, Mercieri M, Cigognetti L, Romano R, et al. In vivo effects on human skeletal muscle oxygen delivery and metabolism of cardiopulmonary bypass and perioperative hemodilution. Intensive Care Med. 2012;38(3):413–21.
Vincent JL, Sakr Y, De Backer D, Van der Linden P. Efficacy of allogeneic red blood cell transfusions. Best Pract Res Clin Anaesthesiol. 2007;21(2):209–19.
den Os MM, van den Brom CE, van Leeuwen ALI, Dekker NAM. Microcirculatory perfusion disturbances following cardiopulmonary bypass: a systematic review. Crit Care. 2020;24(1):218.
Shaefi S, Mittel A, Loberman D, Ramakrishna H. Off-pump versus on-pump coronary artery bypass grafting-a systematic review and analysis of clinical outcomes. J Cardiothorac Vasc Anesth. 2019;33(1):232–44.
Grenon SM, Vittinghoff E, Owens CD, Conte MS, Whooley M, Cohen BE. Peripheral artery disease and risk of cardiovascular events in patients with coronary artery disease: insights from the heart and soul study. Vasc Med. 2013;18(4):176–84.
Nakatsu T, Tamura N, Yanagi S, Kyo S, Koshiji T, Sakata R. Bilateral internal thoracic artery grafting for peripheral arterial disease patients. Gen Thorac Cardiovasc Surg. 2014;62(8):481–7.
Nielsen ND, Martin-Loeches I, Wentowski C. The effects of red blood cell transfusion on tissue oxygenation and the microcirculation in the intensive care unit: a systematic review. Transfus Med Rev. 2017;4:205–22.
Mandak J, Pojar M, Cibicek N, Lonsky V, Palicka V, Kakrdova D, et al. Impact of cardiopulmonary bypass on peripheral tissue metabolism and microvascular blood flow. Perfusion. 2008;23(6):339–46.
De Backer D, Creteur J, Dubois MJ, Sakr Y, Vincent JL. Microvascular alterations in patients with acute severe heart failure and cardiogenic shock. Am Heart J. 2004;147(1):91–9.
Dekker NAM, Veerhoek D, Koning NJ, van Leeuwen ALI, Elbers PWG, van den Brom CE, et al. Postoperative microcirculatory perfusion and endothelial glycocalyx shedding following cardiac surgery with cardiopulmonary bypass. Anaesthesia. 2019;74(5):609–18.
Mand’ák J, Zivný P, Lonský V, Palicka V, Kakrdová D, Marsíková M, et al. Changes in metabolism and blood flow in peripheral tissue (skeletal muscle) during cardiac surgery with cardiopulmonary bypass: the biochemical microdialysis study. Perfusion. 2004;19(1):53–63.
Tripodaki ES, Tasoulis A, Koliopoulou A, Vasileiadis I, Vastardis L, Giannis G, et al. Microcirculation and macrocirculation in cardiac surgical patients. Crit Care Res Pract. 2012;2012: 654381.
Butler E, Mahendran S, Nguyen J, Aneman A. Microvascular reactivity, assessed by near-infrared spectroscopy and a vascular occlusion test, is associated with patient outcomes following cardiac surgery: a prospective observational study. Eur J Anaesthesiol. 2018;35(5):356–64.
Kim TK, Cho YJ, Min JJ, Murkin JM, Bahk JH, Hong DM, et al. Microvascular reactivity and clinical outcomes in cardiac surgery. Crit Care. 2015;19(1):316.
Scolletta S, Franchi F, Damiani E, Cennamo A, Domizi R, Meola A, et al. Tissue oxygen saturation changes and postoperative complications in cardiac surgery: a prospective observational study. BMC Anesthesiol. 2019;19(1):229.
Maier S, Hasibeder WR, Hengl C, Pajk W, Schwarz B, Margreiter J, et al. Effects of phenylephrine on the sublingual microcirculation during cardiopulmonary bypass. Br J Anaesth. 2009;102(4):485–91.
Boerma EC, Kaiferová K, Konijn AJ, De Vries JW, Buter H, Ince C. Rectal microcirculatory alterations after elective on-pump cardiac surgery. Minerva Anestesiol. 2011;77(7):698–703.
Butler E, Chin M, Aneman A. Peripheral near-infrared spectroscopy: methodologic aspects and a systematic review in post-cardiac surgical patients. J Cardiothorac Vasc Anesth. 2016;S1053–0770(16):30299–303.
Vandenbulcke L, Lapage KG, Vanderstraeten KV, De Somer FM, De Hert SG, Moerman AT. Microvascular reactivity monitored with near-infrared spectroscopy is impaired after induction of anesthesia in cardiac surgery patients: an observational study. Eur J Anaesthesiol. 2017;34(10):688–94.
Atasever B, Boer C, Goedhart P, Biervliet J, Seyffert J, Speekenbrink R, et al. Distinct alterations in sublingual microcirculatory blood flow and hemoglobin oxygenation in on-pump and off-pump coronary artery bypass graft surgery. J Cardiothorac Vasc Anesth. 2011;25(5):784–90.
Lanzarone E, Gelmini F, Tessari M, Menon T, Suzuki H, Carini M, et al. Preservation of endothelium nitric oxide release by pulsatile flow cardiopulmonary bypass when compared with continuous flow. Artif Organs. 2009;33(11):926–34.
Dedichen HH, Hisdal J, Aadahl P, Nordhaug D, Olsen PO, Kirkeby-Garstad I. Elevated arterial lactate concentrations early after coronary artery bypass grafting are associated with increased anaerobic metabolism in skeletal muscle. J Cardiothorac Vasc Anesth. 2015;29(2):367–73.
Obi AT, Park YJ, Bove P, Cuff R, Kazmers A, Gurm HS, et al. The association of perioperative transfusion with 30-day morbidity and mortality in patients undergoing major vascular surgery. J Vasc Surg. 2015;61(4):1000-9.e1.
Al-Sarraf N, Al-Shammari F, Vislocky I, Malek L. Lower limb compartment syndrome following coronary artery bypass surgery: a rare entity. Gen Thorac Cardiovasc Surg. 2010;58(3):131–3.
Tsui AK, Dattani ND, Marsden PA, El-Beheiry MH, Grocott HP, Liu E, et al. Reassessing the risk of hemodilutional anemia: some new pieces to an old puzzle. Can J Anaesth. 2010;57(8):779–91.
Szabó Z, Andersson RG, Arnqvist HJ. Intraoperative muscle and fat metabolism in diabetic patients during coronary artery bypass grafting surgery: a parallel microdialysis and organ balance study. Br J Anaesth. 2009;103(2):166–72.
Flick M, Duranteau J, Scheeren TWL, Saugel B. Monitoring of the sublingual microcirculation during cardiac surgery: current knowledge and future directions. J Cardiothorac Vasc Anesth. 2020;34(10):2754–65.
Koning NJ, Vonk AB, Meesters MI, Oomens T, Verkaik M, Jansen EK, et al. Microcirculatory perfusion is preserved during off-pump but not on-pump cardiac surgery. J Cardiothorac Vasc Anesth. 2014;28:336–41.
Koning NJ, Simon LE, Asfar P, Baufreton C, Boer C. Systemic microvascular shunting through hyperdynamic capillaries after acute physiological disturbances following cardiopulmonary bypass. Am J Physiol Heart Circ Physiol. 2014;307(7):H967–75.
Atasever B, Boer C, Speekenbrink R, Seyffert J, Goedhart P, de Mol B, et al. Cardiac displacement during off-pump coronary artery bypass grafting surgery: effect on sublingual microcirculation and cerebral oxygenation. Interact Cardiovasc Thorac Surg. 2011;13(6):573–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
The authors declare that there is no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sevuk, U., Bahadir, M.V. Symptom progression following on-pump versus off-pump coronary artery bypass graft surgery in patients with peripheral arterial disease. Gen Thorac Cardiovasc Surg 71, 158–166 (2023). https://doi.org/10.1007/s11748-022-01855-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-022-01855-x