Abstract
Objectives
We determined whether patients requiring surgery could be identified using pneumothorax volume/size in the first episode of primary spontaneous pneumothorax (PSP) and confirmed which of six different measurement methods of pneumothorax volume/size best predicted surgical indication (prolonged air leak, PAL, or ipsilateral recurrence).
Methods
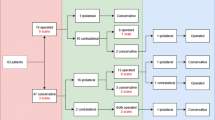
Between 2013 and 2017, 282 patients with PSP were analysed. The volume of the pneumothorax (%) was calculated using volumetric methods (Collins, Rhea, Kircher, Light), while its size (large or small) was determined using the British Thoracic Society (BTS) and American College of Chest Physicians (ACCP) guidelines for the first PSP episode. The optimal cut-off points of pneumothorax volume in patients requiring surgery were based on the most sensitive and specific scores, calculated using receiver operating characteristic analysis.
Results
Surgery was indicated in 162 patients (57.4%) because of PAL (n = 92) or ipsilateral recurrence (n = 70). Kircher’s method had a better area under the curve (AUC) value than the others (AUC = 0.731, 95% confidence interval [CI] 0.676–0.782). Comparing the calculated cut-off points for each volumetric method and the known thresholds from the BTS/ACCP, the best predictor for surgical indications (for both PAL and ipsilateral recurrence) was Kircher’s method (odds ratio = 5.636, 95% CI 3.338–9.516, p < 0.001). The four volumetric methods were significantly correlated with pneumothorax volume (rho ≥ 0.8, p < 0.001, for all comparisons).
Conclusions
Pneumothorax volume/size calculated in the first PSP episode may help predict surgical candidates, with Kircher's method being the best predictor. There was a correlation between all the volumetric methods of the pneumothorax volume.


Similar content being viewed by others

Abbreviations
- AUC:
-
Area under the curve
- CI:
-
Confidence interval
- CT:
-
Computed tomography
- OR:
-
Odds ratio
- PAL:
-
Prolonged air leak
- PSP:
-
Primary spontaneous pneumothorax
- ROC:
-
Receiver operating characteristic
References
Tsai TM, Lin MW, Li YJ, et al. The size of spontaneous pneumothorax is a predictor of unsuccessful catheter drainage. Sci Rep. 2017;7(1):181.
MacDuff A, Arnold A, Harvey J, BTS Pleural Disease Guideline Group. Management of spontaneous pneumothorax: British Thoracic Society Pleural Disease guideline 2010. Thorax. 2010;65(Suppl 2):ii18–31.
Tschopp JM, Bintcliffe O, Astoul P, et al. ERS task force statement: diagnosis and treatment of primary spontaneous pneumothorax. Eur Respir J. 2015;46(02):321–35.
Baumann MH, Strange C, Heffner JE, AACP Pneumothorax Consensus Group, et al. Management of spontaneous pneumothorax: an American College of Chest Physicians Delphi consensus statement. Chest. 2001;119(02):590–602.
Chambers A, Scarci M. In patients with first-episode primary spontaneous pneumothorax is video-assisted thoracoscopic surgery superior to tube thoracostomy alone in terms of time to resolution of pneumothorax and incidence of recurrence? Interact Cardiovasc Thorac Surg. 2009;9(6):1003–8.
Bintcliffe OJ, Hallifax RJ, Edey A, et al. Spontaneous pneumothorax: time to rethink management? Lancet Respir Med. 2015;3:578–88.
Sayar A, Kök A, Citak N, et al. Size of pneumothorax can be a new indication for surgical treatment in primary spontaneous pneumothorax: a prospective study. Ann Thorac Cardiovasc Surg. 2014;20:192–7.
Ryu KM, Seo PW, Park S, Ryu JW. Complete atelectasis of the lung in patients with primary spontaneous pneumothorax. Ann Thorac Surg. 2009;87:875–9.
Chee CB, Abisheganaden J, Yeo JK, Lee P, Huan PY, Poh SC, Wang YT. Persistent air-leak in spontaneous pneumothorax–clinical course and outcome. Respir Med. 1998;92(5):757–61.
Collins CD, Lopez A, Mathie A, Wood V, Jackson JE, Roddie ME. Quantification of pneumothorax size on chest radiographs using interpleural distances: regression analysis based on volume measurements from helical CT. AJR Am J Roentgenol. 1995;165(5):1127–30.
Rhea JT, DeLuca SA, Greene RE. Determining the size of pneumothorax in the upright patient. Radiology. 1982;144(4):733–6.
Light RW. Management of spontaneous pneumothorax. Am Rev Respir Dis. 1993;148(1):245–8.
Noppen M, Alexander P, Driesen P, Slabbynck H, Verstraeten A. Manual aspiration versus chest tube drainage in first episodes of primary spontaneous pneumothorax: a multicenter, prospective, randomized pilot study. Am J Respir Crit Care Med. 2002;165(9):1240–4.
Kelly AM, Weldon D, Tsang AY, Graham CA. Comparison between two methods for estimating pneumothorax size from chest X-rays. Respir Med. 2006;100(8):1356–9.
Kelly AM, Druda D. Comparison of size classification of primary spontaneous pneumothorax by three international guidelines: a case for international consensus? Respir Med. 2008;102(12):1830–2.
Kircher LT Jr, Swartzel RL. Spontaneous pneumothorax and its treatment. J Am Med Assoc. 1954;155(1):24–9.
Olesen WH, Lindahl-Jacobsen R, Katballe N, et al. Recurrent primary spontaneous pneumothorax is common following chest tube and conservative treatment. World J Surg. 2016;40(9):2163–70.
Casali C, Stefani A, Ligabue G, et al. Role of blebs and bullae detected by high-resolution computed tomography and recurrent spontaneous pneumothorax. Ann Thorac Surg. 2013;95(1):249–55.
Lang-Lazdunski L. Invited commentary. Ann Thorac Surg. 2010;90(1):188–9.
Mitani A, Hakamata Y, Hosoi M, et al. The incidence and risk factors of asymptomatic primary spontaneous pneumothorax detected during health check-ups. BMC Pulm Med. 2017;17(1):177.
Baumann MH. Non-spontaneous pneumothorax. In: Light RW, Lee YCG, editors. Textbook of pleural diseases. London: Arnold; 2003. p. 464–74.
Noppen M, Alexander P, Driesen P, Slabbynck H, Verstraete A, Vlaamse Werkgroep voor Medische Thoracoscopie en Interventionele Bronchoscopie. Quantification of the size of primary spontaneous pneumothorax: accuracy of the Light index. Respiration. 2001;68(4):396–9.
Hoi K, Turchin B, Kelly AM. How accurate is the Light index for estimating pneumothorax size? Australas Radiol. 2007;51(2):196–8.
Funding
The authors received no specific funding for this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None declared.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Çıtak, N., Özdemir, S. Which pneumothorax volume/size measurement method can best predict surgical indication in primary spontaneous pneumothorax patients? A comparison of six different methods. Gen Thorac Cardiovasc Surg 70, 871–879 (2022). https://doi.org/10.1007/s11748-022-01800-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-022-01800-y