Abstract
Objectives
To develop a risk score model for primary spontaneous pneumothorax surgery (prolonged air leak or ipsilateral recurrence). The model was internally validated for risk estimation.
Methods
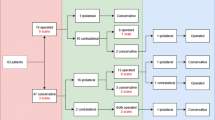
We analyzed 453 patients with primary spontaneous pneumothorax between 2014 and 2018. Patients were randomly assigned a 2:1 ratio to the development dataset (n = 302, study cohort) or the internal validation dataset (n = 151, validation cohort). The final outcomes of patients with primary spontaneous pneumothorax, the presence or absence of surgical indications, were tracked. Multivariable logistic regression models were prepared to estimate the probability of surgical indication and a scoring model was created. It was internally validated using the validation cohort. Calibration was ascertained using the Hosmer–Lemeshow method and Brier score.
Results
The surgery indication rate was 47.8% (n = 217) (prolonged air leak, n = 130; ipsilateral recurrence, n = 87). There were no demographic or radiological differences between the validation and the study cohorts. Logistic regression analysis showed that the presence of bullae or blebs (p < 0.001, odds ratio = 3.340, 95%CI = 1.753–6.363) and pneumothorax volume (p < 0.001, odds ratio = 1.033, 95%CI = 1.019–1.048) were independent risk factors for surgical indication. The scoring model significantly predicted surgical indications (area under the curve, AUC = 0.768, 95%CI = 0.714–0.821, p < 0.001). Our model showed acceptable discrimination with an AUC > 0.75 in the validation set (AUC = 0.777, 95%CI = 0.702–0.852, p < 0.001) and had an adequate calibration (Hosmer–Lemeshow test p = 0.249, Brier score = 0.25).
Conclusion
The internally validated primary spontaneous pneumothorax scoring model was a good predictor of the need for surgery in patients with primary spontaneous pneumothorax. Prospective external validation studies with larger patient cohorts are required.





Similar content being viewed by others
Data availability
The authors have full control of all primary data and that we agree to allow the journal to review their data if requested. The data underlying this article cannot be shared publicly due to the privacy of individuals that participated in the study. However, the data will be shared on reasonable request to the corresponding author.
Abbreviations
- AUC:
-
Area under the receiver operating characteristic curve
- CI:
-
Confidence interval
- DSS:
-
Dystrophic severity score
- Log odds:
-
Logarithm of the odds
- NPV:
-
Negative predictive value
- PPV:
-
Positive predictive value
- PSP:
-
Primary spontaneous pneumothorax
- PAL:
-
Prolonged air leak
- ROC:
-
Receiver operating curve
References
MacDuff A, Arnold A, Harvey J, BTS Pleural Disease Guideline Group. Management of spontaneous pneumothorax: British thoracic society pleural disease guideline 2010. Thorax. 2010;65(Suppl 2):ii18-31.
Tschopp JM, Bintcliffe O, Astoul P, Canalis E, Driesen P, Janssen J, et al. ERS task force statement: diagnosis and treatment of primary spontaneous pneumothorax. Eur Respir J. 2015;46(2):321–35.
Baumann MH, Strange C, Heffner JE, Light R, Kirby TJ, Klein J, et al. Management of spontaneous pneumothorax: an American college of chest physicians Delphi consensus statement. Chest. 2001;119(2):590–602.
Özdemir S, Çitak N. Determination of risk factors for recurrence in first episode pneumothorax. Indian J Surg. 2022. https://doi.org/10.1007/s12262-021-03274-3.
Tan J, Yang Y, Zhong J, Zuo C, Tang H, Zhao H, et al. Association between BMI and recurrence of primary spontaneous pneumothorax. World J Surg. 2017;41(5):1274–80.
Olesen WH, Katballe N, Sindby JE, Titlestad IL, Andersen PE, Lindahl-Jacobsen R, et al. Surgical treatment versus conventional chest tube drainage in primary spontaneous pneumothorax: a randomized controlled trial. Eur J Cardiothorac Surg. 2018;54(1):113–21.
Walker SP, Bibby AC, Halford P, Stadon L, White P, Maskell NA. Recurrence rates in primary spontaneous pneumothorax: a systematic review and meta-analysis. Eur Respir J. 2018;52(3):1800864.
Çıtak N, Özdemir S. Which pneumothorax volume/size measurement method can best predict surgical indication in primary spontaneous pneumothorax patients? A comparison of six different methods. Gen Thorac Cardiovasc Surg. 2022;70(10):871–9. https://doi.org/10.1007/s11748-022-01800-y.
Patel DA, Sharda R, Choksi YA, Slaughter JC, Higginbotham T, Garrett CG, et al. Model to select on-therapy vs off-therapy tests for patients with refractory esophageal or extraesophageal symptoms. Gastroenterology. 2018;155(6):1729–40.
McWilliams A, Tammemagi MC, Mayo JR, Roberts H, Liu G, Soghrati K, et al. Probability of cancer in pulmonary nodules detected on first screening CT. N Engl J Med. 2013;369(10):910–9.
Alessandrino G, Chevalier B, Lefèvre T, Sanguineti F, Garot P, Unterseeh T, et al. A clinical and angiographic scoring system to predict the probability of successful first-attempt percutaneous coronary intervention in patients with total chronic coronary occlusion. JACC Cardiovasc Interv. 2015;8(12):1540–8.
Gonzalez M, Karenovics W, Bédat B, Forster C, Sauvain MO, Triponez F, et al. Performance of prolonged air leak scoring systems in patients undergoing video-assisted thoracoscopic surgery segmentectomy. Eur J Cardiothorac Surg. 2022;1: ezac100. https://doi.org/10.1093/ejcts/ezac100.
Chen YY, Huang HK, Chang H, Lee SC, Huang TW. Postoperative predictors of ipsilateral and contralateral recurrence in patients with primary spontaneous pneumothorax. J Thorac Dis. 2016;8(11):3217–24.
Kircher LT Jr, Swartzel RL. Spontaneous pneumothorax and its treatment. J Am Med Assoc. 1954;155(1):24–9.
Casali C, Stefani A, Ligabue G, Natali P, Aramini B, Torricelli P, et al. Role of blebs and bullae detected by high-resolution computed tomography and recurrent spontaneous pneumothorax. Ann Thorac Surg. 2013;95(1):249–55.
Sayar A, Kök A, Citak N, Metin M, Büyükkale S, Gürses A. Size of pneumothorax can be a new indication for surgical treatment in primary spontaneous pneumothorax: a prospective study. Ann Thorac Cardiovasc Surg. 2014;20(3):192–7.
Ryu KM, Seo PW, Park S, Ryu JW. Complete atelectasis of the lung in patients with primary spontaneous pneumothorax. Ann Thorac Surg. 2009;87:875–9.
Daemen JHT, Lozekoot PWJ, Maessen JG, Gronenschild MHM, Bootsma GP, Hulsewé KWE, et al. Chest tube drainage versus video-assisted thoracoscopic surgery for a first episode of primary spontaneous pneumothorax: a systematic review and meta-analysis. Eur J Cardiothorac Surg. 2019;56(5):819–29.
Cui X, Heuvelmans MA, Han D, Zhao Y, Fan S, Zheng S, et al. Comparison of veterans affairs, Mayo, Brock classification models and radiologist diagnosis for classifying the malignancy of pulmonary nodules in Chinese clinical population. Transl Lung Cancer Res. 2019;8(5):605–13. https://doi.org/10.21037/tlcr.2019.09.17.
Zhang M, Zhuo N, Guo Z, Zhang X, Liang W, Zhao S, et al. Establishment of a mathematic model for predicting malignancy in solitary pulmonary nodules. J Thorac Dis. 2015;7(10):1833–41. https://doi.org/10.3978/j.issn.2072-1439.2015.10.56.
Erdoğu V, Çitak N, Yerlioğlu A, Aksoy Y, Emetli Y, Pekçolaklar A, et al. Is the Yedikule-solitary pulmonary nodule malignancy risk score sufficient to predict malignancy? An internal validation study. Interact Cardiovasc Thorac Surg. 2021;33(2):258–65.
Shahian DM, Edwards FH, Ferraris VA, Haan CK, Rich JB, Normand SL, et al. Quality measurement in adult cardiac surgery: part 1—conceptual framework and measure selection. Ann Thorac Surg. 2007;83(4 Suppl):S3-12.
Acknowledgements
We would like to thank Editage ® (www.editage.com) for English language editing.
Funding
The authors received no financial support for the research and/or authorship of this study.
Author information
Authors and Affiliations
Contributions
NÇ: formal analysis; investigation; software; writing—original draft; conceptualization; methodology; resources; validation; visualization; writing—review and editing; supervision; and project administration. SÖ: data curation; investigation; writing—original draft; resources; visualization; writing—review, and editing. SK: investigation, software, validation, and supervision.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Çıtak, N., Özdemir, S. & Köse, S. Could the probability of surgical indication be determined after first episode of primary spontaneous pneumothorax?. Gen Thorac Cardiovasc Surg 71, 472–479 (2023). https://doi.org/10.1007/s11748-023-01913-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-023-01913-y