Abstract
Objective
This study aimed to analyze whether comorbidities impact postoperative complication rate or survival after anatomical lung resection for non-small cell lung cancer (NSCLC).
Methods
A retrospective analysis of 1219 patients who underwent NSCLC resection between 2000 and 2015 was performed. Analyzed comorbidities included chronic obstructive lung disease (COPD), hypertension, coronary artery disease (CAD), peripheral artery disease, myocardial infarction history, diabetes mellitus, renal insufficiency and other malignancies.
Results
Most patients (78.9%) had comorbidities, most commonly hypertension (34.1%) followed by COPD (26.4%) and other malignancies (19%). The overall complication rate was 38.6% (26.4% pulmonary; 14.8% cardiac; and 3.0% gastrointestinal). Hypertension (odds ratio (OR) = 1.492, p = 0.031) was associated with more cardiac complications. Heavy smoking (OR = 1.008, p = 0.003) and low body mass index (BMI) (OR = 0.932, p < 0.001) affected the pulmonary complication rate significantly. None of the included comorbidities affected the overall complication rate or the survival negatively. However, the patient characteristics of advanced age (p < 0.001), low BMI (p = 0.008), and low FEV1 (p = 0.008) affected the overall complication rate as well as survival (each p < 0.001).
Conclusion
Advanced age, low BMI, and low FEV1 were predictive of greater complication risk and shorter long-term survival in patients who underwent NSCLC resection. Cardiac complications were associated with hypertension and CAD, whereas pulmonary complications were associated with a high pack year count.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lung cancer is a major public health issue worldwide, constituting the second most common cancer in both men and women and being responsible for more cancer-related deaths per year in Switzerland than any other cancer diagnosis [1]. Unfortunately, in more than half of cases, diagnoses of non-small cell lung cancer (NSCLC) are made at an advanced stage and patients with NSCLC tend to have higher comorbidity burdens than patients with other types of malignant tumors, such as breast cancer, prostate cancer, colon cancer, and head and neck cancers [2].
Comorbidity of NSCLC with other tobacco-associated illnesses, including chronic obstructive pulmonary disease (COPD), cardiovascular diseases, and head and neck cancers, can complicate treatment and affect posttreatment survival. Surgical resection remains a critical potentially curative treatment of lung cancer, but having a good outcome is dependent upon the selection of suitable patients for anatomical lung resection of NSCLC.
Population aging has been associated with an increase in the median age of patients being diagnosed with lung cancer, with the age band of patients that are most frequently diagnosed with lung cancer being 60–69 years, followed closely by people that are 70–79 years old [3]. This increase in geriatric patients referred for surgical resection of lung cancer has brought greater attention to how comorbidities should be considered in NSCLC treatment planning [4]. The aim of the present study was thus to analyze whether and how preoperative comorbidities may impact the occurrence of postoperative complications or survival after anatomical lung resection in patients diagnosed with NSCLC.
Methods
Patients
This retrospective study examines the cases of patients with a diagnosis of NSCLC who underwent anatomical lung resections between January 2000 and December 2015 at the University Hospital Zurich. Initially, 1′312 such patients were included. Patients with low-frequency characteristics were excluded to facilitate statistical analyses. Specifically, patients under 40 years of age (N = 30), patients with a postoperatively determined disease staging of zero (N = 12), patients with GOLD stage IV COPD (N = 3), and a patient who received only radiotherapy as a preoperative treatment (N = 1) were excluded. An additional 47 patients who were lost to follow-up were excluded from the final analysis. After these exclusions, we included a total of 1219 patients. The cantonal ethics committee of Zurich approved this study (2016-00799).
Comorbidities
The following comorbidities were included in this study: COPD, diabetes mellitus, renal insufficiency, another malignancy; and cardiovascular comorbidities including coronary artery disease (CAD), hypertension, previous myocardial infarction, and peripheral artery disease. Hypertension was defined as a repeated measurement of a blood pressure over 140/90 mmHg. CAD was diagnosed with exercise ECG, myocardial scintigraphy, echocardiography, or coronary angiography. The diagnostic criteria for peripheral artery disease were a high ankle-brachial index, a history of claudication, ischemic rest pain and/or an abnormally low extremity pulse, nonhealing lower extremity wound or gangrene apparent upon physical examination. Post-myocardial infarction status was determined based on chart review and patient history. COPD was defined by a post bronchodilator Tiffenau-Pinelli Index of < 0.7 and divided into four categories according to the GOLD Classification [5]. Diabetes mellitus was included as a comorbidity if diagnosed according to the 1999 World Health Organization guidelines [6]. Any cancer outside the lungs was considered another malignancy. Renal insufficiency was defined as a glomerular filtration rate < 60 ml/min/1.73 m2.
Complications and survival
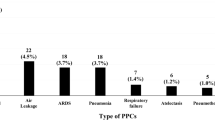
Postoperative complications were divided into four major groups: cardiac; pulmonary; gastrointestinal; and other (e.g., local and systemic postoperative infections). We included the most common and most severe complications after lung resection (Table 1).
Pneumonia was defined as bacterial pneumonia diagnosed on chest X-Ray. Atelectasis equally was a radiographic diagnosis. Prolonged air leakage was defined as an air leak that persisted beyond the seventh postoperative day. The diagnosis of ARDS was made in accordance with the Berlin definition of ARDS [7]. Regarding cardiac arrhythmias, both atrial and ventricular arrhythmias were included in this study. Postoperative hypertension was defined as a blood pressure over 140/90 mmHg requiring antihypertensive medication. Sepsis was defined as a life-threatening organ dysfunction caused by a dysregulated response to infection [8]. Postoperative Complications were included within 30 days after surgery.
Operative mortality or 30-day mortality was defined as ‘any death regardless of cause occurring within 30 days after surgery in or out of the hospital, and after 30 days during the same hospitalization subsequent to the operation’ [9]. Furthermore, if a patient had any further surgery during their hospitalization, operative mortality is assigned to the first operation of the given hospitalization.
Follow-up was completed in January of 2019 or upon death.
Statistical analysis
Statistical analyses were performed in SPSS for Windows version 26.0 (IBM, Armok, NY, USA) and R version 3.6.1 (R Foundation for Statistical Computing, Vienna, Austria). Continuous data are presented as means and standard deviations; categorical data are presented as frequencies and percentages. To identify possible predictive factors, binominal and multivariate logistic regressions were performed to ascertain the effects of patient characteristics and comorbidities on the occurrence of complications. A Cox proportional hazards model was applied to find possible associations of patient characteristics or comorbidities with overall survival. Odds ratios (ORs) and hazard ratios (HRs) are reported as appropriate. In all cases, p < 0.05 was considered significant.
Results
Patient population, tumor characteristics, and surgery
The demographic characteristics of the patients, their tumor characteristics, and their surgical interventions are summarized for the patient sample as a whole in Table 2, together with comparisons between patients with complications and patients without complications for each variable. With respect to patient characteristics, a majority of the patients were men, most were in their sixties, and a majority had a healthy body mass index (BMI), though about one in twenty was underweight. The mean FEV1 of all subjects was within normal range, and there was a wide range of smoking history in terms of pack years. Notably, tumor histology revealed that resected lung tumors were most frequently adenocarcinomas, followed by squamous cell carcinomas, carcinoids, other tumor types, and large cell carcinomas, respectively. About two thirds of the patients underwent lobectomy, followed in frequency by pneumonectomy and sleeve resection, respectively.
Overall comorbidities and complications
A large majority of the patient sample (N = 957, 78.9%) had at least one identified comorbidity. The overall postoperative complication rate was 38.6% (N = 471). The occurrence of comorbidities overall and comparisons of the occurrence of complications in patients with versus without each analyzed comorbidity are reported in Table 3. According to our multivariate logistic regression analysis performed to detect independent influencing factors on postoperative complication rate, none of the analyzed comorbidities was a significant influencing factor. However, overall complication risk was influenced by some patient characteristics. Specifically, as shown in Fig. 1, complication risk was found to be positively associated with older age (p < 0.001), lower BMI (p = 0.008), and lower FEV1 (p = 0.008).
Furthermore, there was no multicollinearity among variables, assuring the independence of each influencing factor included in this multivariate logistic regression.
Pulmonary complications
Two factors were found to be significant predictors of a higher rate of pulmonary complications, namely a low (underweight) BMI (p < 0.001) and a high pack year smoking history (p = 0.003). A low FEV1 had a non-significant trend toward being inversely related to the incidence of pulmonary complications (p = 0.065). Surprisingly, COPD was not found to be related to postoperative pulmonary complication risk (p = 0.525). Despite increased age being a negative prognostic factor for survival and the overall occurrence of complications, it was not associated with a higher pulmonary complication rate specifically (p = 0.619).
Cardiovascular complications
Patients with arterial hypertension (p = 0.031) and older patients (p < 0.001) were found to be at significantly elevated risk of postoperative cardiac complications. Pneumonectomy was identified as an independent risk factor for cardiac complications (p = 0.016). Whereas the cardiovascular comorbidities of CAD and peripheral artery disease did not have significant influences on the occurrence of cardiac complications (p = 0.096 and p = 0.225), patients with a history of myocardial infarction appeared to be potentially at a reduced risk of cardiac complications (OR = 0.283). However, there was only a near-significant trend (p = 0.052) and the group with a history of myocardial infarction was small (N = 35).
Gastrointestinal complications
The incidence of gastrointestinal complications was very low. Only 36 (3.0%) of the 1219 patients were affected, including 9 patients who suffered from postoperative ileus. Other gastrointestinal complications included bleeding, ischemia, and colitis. No further analysis in regard to predictive factors was feasible given the small number of patients affected.
Survival
Cox proportional-hazard analysis showed that increased age (HR = 1.02, confidence interval (CI) = 1.01–1.03), lower BMI (HR = 0.96, CI = 0.94–0.98), and lower FEV1 (HR = 0.99, CI = 0.98–0.99) were independent negative influencing factors on overall survival (all p < 0.001). Female patients showed a better survival than their male counterparts (HR = 0.77, CI = 0.63–0.94, p = 0.009). COPD GOLD stage I (HR = 0.70, CI = 0.49–1.00, p = 0.051) and II (HR = 0.73, CI = 0.57–0.95, p = 0.019) were associated with a longer overall survival. The group of patients with COPD GOLD III likewise had a lower HR (0.76, CI = 0.50–1.15), but this finding was not significant (p = 0.191). All other tested comorbidities did not have a significant influence on overall survival.
Because tumor and surgical characteristics are well-established factors that affect survival, they were included in the Cox proportional-hazard analysis as confounding factors. As expected, the analysis showed that higher tumor stage and an open surgical access were negative prognostic factors for survival. All variables that were included in the Cox proportional-hazard model are shown in Fig. 2.
Operative mortality
The overall surgical mortality was 1.56% (n = 19). The biggest group were patients who died due to multi-organ failure caused by sepsis (n = 9). Five patients died postoperatively as a result of ARDS. Two patients suffered massive pulmonary embolisms which led to death. Another two patients died due to substantial postoperative myocardial infarctions. One patient died after a bilateral thromboembolic occlusion of the internal carotid artery.
Discussion
At the time of NSCLC diagnosis, many patients have serious comorbidities. The high frequency of comorbidities is mainly due to the common risk factor of an extensive history of tobacco use. Furthermore, the median age of patients with lung cancer is around 70 years, which increases the likelihood of pre-existing age-related disease like renal insufficiency or cardiac disease [10]. For these reasons, it is critical to understand the impact of comorbidities on postoperative complications and survival after NSCLC tumor resection.
In the present study, we found that the prevalence of serious comorbidity in patients with NSCLC was quite high, especially in elderly patients.
Although there is a widespread belief amongst clinicians that patients with comorbidities are at an increased risk of postoperative complications, we found that some patient characteristics were more predictive of postoperative problems than any specific comorbidity. In particular, complication risk was found to be significantly associated with older age, a low BMI, and a low preoperative FEV1, affirming the findings of several previous studies [11,12,13].
None of the analyzed comorbidities was found to be an independent predictor of whether or not a patient would suffer complications overall. However, looking at system specific comorbidities and complications, some correlations could be found. Pulmonary complications were the most frequent complications after lung resections. Similar to a study from Im et al., our analysis indicated that patients with a low BMI and patients with a high pack year count did have a higher rates of pulmonary complications [11]. The effect of smoking as a prognostic factor for pulmonary complications, independent of lung function, can be explained by ciliary damage that impedes mucus clearance, which in turn puts patients at risk of pneumonia [14]. However, none of the analyzed comorbidities—not even COPD—affected the incidence of pulmonary complications significantly.
The most prevalent cardiac complication was atrial arrhythmia, followed by postoperative hypertension; only three patients suffered from a postoperative myocardial infarction. A vast variety of risk factors for atrial fibrillation after pulmonary resection has been reported [15,16,17]. The present observations of arterial hypertension, higher age, and pneumonectomy being found to be significant independent prognostic factors of a higher cardiac complication rate are not surprising given that hypertension leads to hypertensive heart disease and thus to architectural changes in the myocardium that leave it more susceptible to the development of arrhythmias [18]. The manipulation of the pulmonary veins during pneumonectomy may trigger arrhythmias after this type of surgery [15].
Although patients with CAD had a higher rate of cardiac complications overall, the presence of CAD as a comorbidity was not found to be a significant influencing factor in our multivariate logistic regression (p = 0.268). Moreover, because patients with CAD generally have arterial hypertension, it is likely that systemic hypertension was a confounding factor. There are conflicting reports regarding the influence of peripheral vascular disease on postoperative complication [17, 19]. However, in this study, the presence of peripheral artery disease did not influence the occurrence of postoperative cardiac complications. Our finding suggestive of a lower incidence of cardiac complications among patients with a history of myocardial infarction should be considered with caution given that there were only 35 patients in this comorbidity group. It is possible that these patients were assessed more carefully preoperatively or protected by medications they were already taking. Notwithstanding, it would be of interest to examine whether this association would be reproduced in a larger study population.
Many patients who have NSCLC suffer from severe comorbidities that themselves have a direct negative impact on survival and that may be a counter-indication for the use of preferred antineoplastic therapies. Our findings of better survival among COPD patients (significant for GOLD I and II patients) than among patients without COPD contrasts with previous data [20]. There is no clear explanation for these results, though it is possible that other underlying disease not included in our analysis may have affected the results. No other comorbidities included in this study were found to influence survival. Although the presently obtained slightly elevated HR for hypertension was not significant, one would expect that arterial hypertension would be associated with a shorter overall survival, especially if not well managed. It would be of interest in the future to track disease free survival in addition to, or instead of, overall survival.
Our overall survival data indicate that patient characteristics are more important predictors of postoperative survival among NSCLC patients than comorbidities. Increased age, a low BMI, and a low preoperative FEV1 were independent prognostic factors found to be negatively related to overall survival, consistent with previous studies [21, 22].
The present analysis showed that a more advanced age was associated with both a higher complication rate and reduced overall survival. Age-related risks include changes to rib cage calcification, reduced vertebral height due to osteoporosis, and overall deterioration of the immune response leading to a higher susceptibility to infection [23, 24]. The aforementioned anatomical changes result in lower chest wall compliance and reduced inspiratory expansion. Older patients are also more likely to suffer from heart disease and compromised kidney function. However, our multivariate analysis showed age to be an independent influencing factor, while comorbidities per se were mostly not significantly related to postoperative outcome. Hence, it appears that the influence of age on complication rate involves factors not explicitly included in the analysis and, thus, not measured in routine preoperative evaluations [25].
Male sex was an independent, negative prognostic factor for survival. Given that we tracked overall survival and not disease-free survival, this effect could be consequent to women living longer in general. Several hypotheses have been proposed to explain the longevity of women, from the influence of estrogen to the role of mitochondria [26, 27].
The operative mortality in this dataset was 1.56%. This result is at the lower end of the ranges observed by other authors [28, 29].
Conclusion
In the present study, increased age, a low BMI, and a low FEV1 were independently associated with a higher risk of postoperative complications and shorter survival in NSCLC patients who have undergone anatomical lung resections. Although older patients should not be excluded from surgery based on age alone, their BMI and FEV1 should be considered in the preoperative assessment.
Comorbidities were common amongst patients undergoing anatomical lung resection for NSCLC. However, almost all of them were not found to have a major effect on complications or survival. Only cardiac complications were found to occur more frequently in patients already suffering from arterial hypertension. In summary, this study showed that none of the included comorbidities alone should be an exclusion criterion for surgical treatment for NSCLC.
Abbreviations
- NSCLC:
-
Non-small cell lung cancer
- FEV1:
-
1-S forced expiratory volume
- COPD:
-
Chronic obstructive pulmonary disease
- ECG:
-
Electrocardiogram
- CAD:
-
Coronary artery disease
- SPSS:
-
Statistical Package for Social Sciences
- OR:
-
Odds ratio
- HR:
-
Hazard ratio
- BMI:
-
Body mass index
- CI:
-
Confidence interval
References
Krebsliga, Krebs in der Schweiz: wichtige Zahlen, 2012–2016. August 2020.
Battafarano RJ, Piccirillo JF, Meyers BF, Hsu HS, Guthrie TJ, Cooper JD, et al. Impact of comorbidity on survival after surgical resection in patients with stage I non-small cell lung cancer. J Thorac Cardiovasc Surg. 2002;123(2):280–7.
NICER, National institute for cancer epidemiology and registration, Cancer prevalence in Switzerland 2005–2020.
Blanco R, Maestu I, de la Torre MG, Cassinello A, Nuñez I. A review of the management of elderly patients with non-small-cell lung cancer. Ann Oncol. 2015;26(3):451–63.
Vogelmeier CF, Criner GJ, Martínez FJ, Anzueto A, Barnes PJ, Bourbeau J, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 report: GOLD Executive Summary. Arch Bronconeumol. 2017;53(3):128–49.
Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med. 1998;15(7):539–53.
Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, Fan L, Camporota E, et al. Acute respiratory distress syndrome: the Berlin Definition. JAMA. 2012;307(23):2526–33.
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315(8):801–10.
Jacobs JP, Mavroudis C, Jacobs ML, Maruszewski B, Tchervenkov CI, Lacour-Gayet FG, Taskforce, J.E.-S.C.D. Committee, et al. What is operative mortality? Defining death in a surgical registry database: a report of the STS Congenital Database Taskforce and the Joint EACTS-STS Congenital Database Committee. Ann Thorac Surg. 2006;81(5):1937–41.
Leduc C, Antoni D, Charloux A, Falcoz PE, Quoix E. Comorbidities in the management of patients with lung cancer. Eur Respir J. 2017;49(3):1601721.
Im Y, Park HY, Shin S, Shin SH, Lee H, Ahn JH, et al. Prevalence of and risk factors for pulmonary complications after curative resection in otherwise healthy elderly patients with early stage lung cancer. Respir Res. 2019;20(1):136.
Ferguson MK, Im HK, Watson S, Johnson E, Wigfield CH, Vigneswaran WT. Association of body mass index and outcomes after major lung resection. Eur J Cardiothorac Surg. 2014;45(4):e94-99 (discussion e99).
Benattia A, Debeaumont D, Guyader V, Tardif C, Peillon C, Cuvelier A, et al. Physiologic assessment before video thoracoscopic resection for lung cancer in patients with abnormal pulmonary function. J Thorac Dis. 2016;8(6):1170–8.
Xavier RF, Ramos D, Ito JT, Rodrigues FM, Bertolini GN, Macchione M, et al. Effects of cigarette smoking intensity on the mucociliary clearance of active smokers. Respiration. 2013;86(6):479–85.
Hollings DD, Higgins RS, Faber LP, Warren WH, Liptay MJ, Basu S, et al. Age is a strong risk factor for atrial fibrillation after pulmonary lobectomy. Am J Surg. 2010;199(4):558–61.
Iwata T, Nagato K, Nakajima T, Suzuki H, Yoshida S, Yoshino I. Risk factors predictive of atrial fibrillation after lung cancer surgery. Surg Today. 2016;46(8):877–86.
Onaitis M, D’Amico T, Zhao Y, O’Brien S, Harpole D. Risk factors for atrial fibrillation after lung cancer surgery: analysis of the Society of Thoracic Surgeons general thoracic surgery database. Ann Thorac Surg. 2010;90(2):368–74.
Afzal MR, Savona S, Mohamed O, Mohamed-Osman A, Kalbfleisch SJ. Hypertension and arrhythmias. Heart Fail Clin. 2019;15(4):543–50.
Lembicz M, Gabryel P, Brajer-Luftmann B, Dyszkiewicz W, Batura-Gabryel H. Comorbidities with non-small cell lung cancer: Is there an interdisciplinary consensus needed to qualify patients for surgical treatment? Ann Thorac Med. 2018;13(2):101–7.
Zhai R, Yu X, Shafer A, Wain JC, Christiani DC. The impact of coexisting COPD on survival of patients with early-stage non-small cell lung cancer undergoing surgical resection. Chest. 2014;145(2):346–53.
Takada K, Shimokawa M, Akamine T, Ono Y, Haro A, Osoegawa A, et al. Association of low body mass index with poor clinical outcomes after resection of non-small cell lung cancer. Anticancer Res. 2019;39(4):1987–96.
Roth K, Nilsen TI, Hatlen E, Sørensen KS, Hole T, Haaverstad R. Predictors of long time survival after lung cancer surgery: a retrospective cohort study. BMC Pulm Med. 2008;8:22.
Lalley PM. The aging respiratory system–pulmonary structure, function and neural control. Respir Physiol Neurobiol. 2013;187(3):199–210.
Lowery EM, Brubaker AL, Kuhlmann E, Kovacs EJ. The aging lung. Clin Interv Aging. 2013;8:1489–96.
Brunelli A, Kim AW, Berger KI, Addrizzo-Harris DJ. Physiologic evaluation of the patient with lung cancer being considered for resectional surgery: diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013;143(5 Suppl):e166S-e190S.
Viña J, Sastre J, Pallardó F, Borrás C. Mitochondrial theory of aging: importance to explain why females live longer than males. Antioxid Redox Signal. 2003;5(5):549–56.
Viña J, Borrás C, Gambini J, Sastre J, Pallardó FV. Why females live longer than males? Importance of the upregulation of longevity-associated genes by oestrogenic compounds. FEBS Lett. 2005;579(12):2541–5.
Husain ZA, Kim AW, Yu JB, Decker RH, Corso CD. Defining the high-risk population for mortality after resection of early stage NSCLC. Clin Lung Cancer. 2015;16(6):e183–7.
Dogru MV, Sezen CB, Aker C, Girgin O, Kilimci U, Erduhan S, et al. Evaluation of factors affecting morbidity and mortality in pneumonectomy patients. Acta Chir Belg. 2020;10(1080/00015458):1753147.
Acknowledgements
This paper was edited by Dr. Ann Power Smith, a professional scientific editor at Write Science Right.
Funding
Open Access funding provided by Universität Zürich.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Benker, M., Citak, N., Neuer, T. et al. Impact of preoperative comorbidities on postoperative complication rate and outcome in surgically resected non-small cell lung cancer patients. Gen Thorac Cardiovasc Surg 70, 248–256 (2022). https://doi.org/10.1007/s11748-021-01710-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-021-01710-5