Abstract
Objective
Atrioventricular valve surgery poses a risk of myocardial infarction due to the proximity of the coronary arteries. Percutaneous techniques also present a risk of coronary injury. Our objective was to identify, on the mitral and the tricuspid annuli, the zones of high risk given their proximity to the circumflex artery and the right coronary artery, respectively.
Methods
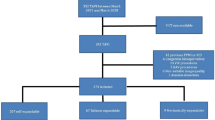
We dissected the courses of the circumflex artery and the right coronary artery in 25 explanted hearts. The distances were measured at reference points according to a clock-face model. Proximity was “very high”, “high”, or “relative” for distances of less than 5 mm, between 5 and 10 mm, or more than 10 mm, respectively.
Results
The mitral annulus zone of “high” proximity was located between “7:30” and “10:00” (minimum 6.5 mm at “9:30”). The tricuspid annulus zone of “very high” proximity was located between “1:30” and “3:00” (minimum 4.0 mm at “2:00”). The circumflex artery seemed closer to the mitral annulus in the hearts with left coronary dominance (n = 2), emphasizing the importance of the preoperative coronary angiography.
Conclusions
Zones at risk of coronary damage were identified on the mitral and the tricuspid annuli between “7:30” and “10:00”, and between “1:30” and “3:00”, respectively. Knowing them can help interventionists avoid ischemic complications. Based on an innovative clock-face orientation scheme in which the distance data were collected at multiple reference points on a superimposed template, our study provides an intuitive and detailed overview of the critical distances between valves and arteries.






Similar content being viewed by others
References
Pessa CJN, Gomes WJ, Catani R, Prates JC, Buffolo E. Anatomical relashionship between the posterior mitral valve annulus and the coronary arteries: implications to operative treatment. Braz J Cardiovasc Surg. 2004;19(4):372.
Al Aloul B, Sigurdsson G, Can I, Li J-M, Dykoski R, Tholakanahalli VN. Proximity of right coronary artery to cavotricuspid isthmus as determined by computed tomography. Pacing Clin Electrophysiol. 2010;33(11):1319–23.
Hiltrop N, Bennett J, Desmet W. Circumflex coronary artery injury after mitral valve surgery: a report of four cases and comprehensive review of the literature. Cathet Cardiovasc Intervent. 2017;89(1):78–92.
Díez-Villanueva P, Gutiérrez-Ibañes E, Cuerpo-Caballero GP, Sanz-Ruiz R, Abeytua M, Soriano J, et al. Direct injury to right coronary artery in patients undergoing tricuspid annuloplasty. Ann Thorac Surg. 2014;97(4):1300–5.
Miura Y, Takeuchi R, Terai Y, Nakai M, Yamazaki F, Tomoya O, et al. Right ventricular infarction caused by tricuspid ring annuloplasty. Gen Thorac Cardiovasc Surg. 2017;65(8):463–5.
Perier P, Hohenberger W, Lakew F, Batz G, Diegeler A. Rate of repair in minimally invasive mitral valve surgery. Ann Cardiothorac Surg. 2013;2(6):751–7.
Ender J, Selbach M, Borger MA, Krohmer E, Falk V, Kaisers UX, et al. Echocardiographic identification of iatrogenic injury of the circumflex artery during minimally invasive mitral valve repair. Ann Thorac Surg. 2010;89(6):1866–72.
Virmani R, Chun PK, Parker J, McAllister HA. Suture obliteration of the circumflex coronary artery in three patients undergoing mitral valve operation. Role of left dominant or codominant coronary artery. J Thorac Cardiovasc Surg. 1982;84(5):773–8.
Miura M, Zuber M, Gavazzoni M, Lin SI, Pozzoli A, Taramasso M, et al. Possible left circumflex artery obstruction in a cardioband transcatheter mitral annuloplasty caused by coronary kinking during cinching. JACC Cardiovasc Interv. 2019;12(6):600–1.
Sponga S, Bertrand OF, Philippon F, St Pierre A, Dagenais F, Charbonneau E, et al. Reversible circumflex coronary artery occlusion during percutaneous transvenous mitral annuloplasty with the Viacor system. J Am Coll Cardiol. 2012;59(3):288.
Ozturk C, Iyisoy A, Onrat E, Balta S, Celik T. The more proximal implantation of percutaneous mitral annuloplasty device due to the circumflex artery compression may be less beneficial. Int J Cardiol. 2016;209:46–8.
Maselli D, Guarracino F, Chiaramonti F, Mangia F, Borelli G, Minzioni G. Percutaneous mitral annuloplasty: an anatomic study of human coronary sinus and its relation with mitral valve annulus and coronary arteries. Circulation. 2006;114(5):377–80.
Bouleti C, Juliard J-M, Himbert D, Iung B, Brochet E, Urena M, et al. Tricuspid valve and percutaneous approach: no longer the forgotten valve! Arch Cardiovasc Dis. 2016;109(1):55–66.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bennani, F., Sebestyen, A., Grimont, P. et al. Relationships between coronary arteries and atrioventricular annuli: surgical and percutaneous implications. Gen Thorac Cardiovasc Surg 70, 132–138 (2022). https://doi.org/10.1007/s11748-021-01680-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-021-01680-8