Abstract
In heart failure (HF), congestion is a key pathophysiologic hallmark and a major contributor to morbidity and mortality. However, the presence of congestion is often overlooked in both acute and chronic settings, particularly when it is not clinically evident, which can have important clinical consequences. Ultrasound (US) is a widely available, non-invasive, sensitive tool that might enable clinicians to detect and quantify the presence of (subclinical) congestion in different organs and tissues and guide therapeutic strategies. In particular, left ventricular filling pressures and pulmonary pressures can be estimated using transthoracic echocardiography; extravascular lung water accumulation can be evaluated by lung US; finally, systemic venous congestion can be assessed at the level of the inferior vena cava or internal jugular vein. The Doppler evaluation of renal, hepatic and portal venous flow can provide additional valuable information. This review aims to describe US techniques allowing multi-organ evaluation of congestion, underlining their role in detecting, monitoring, and treating volume overload more objectively.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
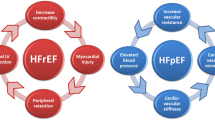
Heart failure (HF) is a complex clinical syndrome characterised by the presence of symptoms (e.g. dyspnea, fatigue) and signs (e.g. elevated jugular venous pressure, pulmonary crackles, and peripheral oedema) due to structural and/or functional abnormalities of the heart that lead to inadequate cardiac output and/or abnormally elevated filling pressures [1]. Congestion, defined as extracellular fluid accumulation, is a central feature of HF and carries serious prognostic implications [1, 2]. From a pathophysiologic point of view, congestion develops due to salt and water retention by the kidney, resulting in elevated ventricular filling pressures; this, in turn, leads to augmented pressures in the pulmonary and/or systemic venous compartment (i.e., intravascular congestion) and subsequent fluid leakage in the extravascular space (i.e., extravascular or tissue congestion) [3]. There is little evidence to suggest that treatment targeting congestion (e.g., with diuretics) modifies the natural history of HF [1]. Still, decongestive therapies are a cornerstone in the treatment of symptoms and signs in both acute and chronic HF, and are lifesaving for patients in pulmonary oedema [1]. Furthermore, timely detection and management of elevated venous pressures and fluid accumulation have been shown to offset the risk of HF-related events [4,5,6]. In the clinical setting, the physical examination remains an essential first step in assessing congestion in patients with suspected or established HF [6]. However, clinical assessment alone has inherent limitations [3], highlighting the importance of a more sensitive, objective evaluation of congestion [7, 8]. Cardiomyocytes release natriuretic peptides in response to pressure and volume overload; their measurement is recommended in the diagnostic workup of suspected HF and offers valuable prognostic information [9]. However, natriuretic peptide levels are influenced by various factors, such as age, body mass index, and atrial fibrillation [1], that may hamper the reliability of this bio-humoural marker as a proxy for fluid overload, and laboratory testing is time-consuming [10, 11]. The gold standard to assess congestion is right heart catheterisation (RHC) [12], which enables the direct measurement of right atrial pressure (RAP), commonly used as an index of central venous pressure (CVP), and pulmonary capillary wedge pressure (PCWP). However, routine RHC has several limitations due to its invasive nature. Ultrasound (US) offers a non-invasive, real-time evaluation which can assist clinicians in diagnosing congestion [10], monitoring the effect of diuretic therapy [10], and predicting outcomes [3] at the same time as an echocardiogram. Integrating these methods addresses the limitations of relying on a single diagnostic tool, offering a more accurate and comprehensive assessment of a patient’s hemodynamic status [3, 13].
The US-based assessment of congestion aims to estimate ventricular filling pressures [10] and identify lung parenchymal [14] and systemic venous congestion through the evaluation of the inferior vena cava [15], internal jugular veins [10], portal and hepatic veins [16], and intrarenal venous flow [10] (Fig. 1). With this background and drawing upon recent advancements in US technology and clinical guidelines, this review aims to summarize the role of novel US techniques in the early detection, monitoring, and management of fluid overload.
Ultrasound methods to detect and quantify congestion
Cardiac US. Transthoracic echocardiography enables a detailed assessment of cardiac structure and function, and a non-invasive estimation of both left ventricular filling pressures (LVFP) and pulmonary pressures [12]. The ratio of early transmitral flow velocity to early diastolic myocardial velocity (E/e’) is generally accepted as a proxy for LVFP and used to evaluate diastolic dysfunction [17, 18]. Assessment of left atrial size and function are also important markers that estimate LVFP and stratify cardiovascular risk [19, 20]. However, quantification of LVFP using echocardiography lacks universal agreement [10]. More recently, an equation has been proposed to estimate pulmonary capillary wedge pressure from standard echocardiographic variables [12]. Said equation was validated against the gold standard of RHC, which shows the potential utility of echocardiography in this setting, especially when an invasive evaluation is not necessary (e.g., in low-risk patients with stable HF), is unfeasible or carries excessive risk. On the other hand, measuring the peak tricuspid regurgitation velocity allows the estimation of the systolic pulmonary arterial pressures. Elevated pressures in the pulmonary circulation are associated with fluid extravasation in the lung interstitium and parenchyma [21].
Lung ultrasound (LUS). LUS is a valuable tool for detecting and quantifying extravascular lung fluid by evaluating B-lines. B-lines are vertical hyperechoic reverberation artefacts arising from the pleural line and extending to the bottom of the ultrasound screen and indicate the presence of extravascular lung water [14] (Fig. 2). In patients with HF, B-lines exhibit rapid changes in response to therapies that modify intravascular volume or pulmonary pressures. For instance, their number reduces during renal dialysis or after treatment with loop diuretics, while they might increase with exercise [21,22,23,24,25,26,27]. In patients presenting to the emergency room with acute dyspnoea, LUS has shown superior sensitivity and specificity in diagnosing interstitial pulmonary oedema compared to clinical examination or chest X-ray [28, 29]. However, B-lines are not exclusive of HF, as they can also appear in non-cardiogenic pulmonary oedema (such as acute respiratory distress syndrome) [30] and interstitial lung disease [30, 31], and might be low in patients who are obese [32].
From a technical point of view, LUS can be performed rapidly with the patient in the supine position, placing the phased array or linear transducer either perpendicularly or transversely to the ribs on the anterior thorax, preferably using an eight-zone protocol (four symmetrical zones per each hemithorax) [10]. Maintaining consistent patient positioning during serial exams is advisable, as the count of B-lines can vary with changes in position, typically increasing when the patient is supine [33]. There are several methods to evaluate B-lines, which include both scoring and counting approaches. In scoring methods, a specific intercostal space with a minimum number of B-lines (i.e., ≥ 3) is marked as positive, and the total number of positive zones is recorded [28, 34]. Alternatively, B-lines can be individually counted within a specific area of the chest or approximated by the proportion of the sector area they cover beneath the pleural line [35, 36]. The quantitative technique is more precise and reliable in terms of consistency within and between different observers [37, 38]. A cut-off value of ≥ 3 B-lines in at least two zones per hemithorax has been proposed to identify acute HF with high sensitivity and specificity [28]. In chronic HF, a higher number of B-lines is associated with an increased risk of subsequent HF admissions and mortality, even in patients with few or no symptoms [3, 23, 39].
Inferior vena cava (IVC). The diameter of the IVC and its respiratory changes are regarded as indicators of CVP [40]. From a pathophysiologic point of view, a high CVP leads to IVC distention and, eventually, to reduced collapsibility during inspiration [40]. Thus, US evaluation of the IVC is valuable for assessing systemic venous congestion, monitoring a patient’s response to diuretic treatment, and predicting outcomes [40]. Importantly, many ambulatory patients with chronic HF who are presumed to be clinically free from congestion are subsequently found to have a dilated and/or non-collapsing IVC, which is associated with elevated natriuretic peptides and an increased risk of poorer outcomes, regardless of LVEF [3, 39, 41]. Furthermore, in patients discharged after a hospitalisation due to acute decompensated HF, the presence of a persistently dilated IVC before discharge is associated with a high risk of rehospitalisation [42]. Surprisingly, invasive studies on patients undergoing RHC revealed only a modest correlation between RAP and the diameter of the IVC measured by echocardiography [40]; this correlation is even weaker in patients mechanically ventilated, as positive intrathoracic pressures generated by mechanical ventilation cause IVC dilation and reduce its collapsibility [43].
To perform an accurate ultrasound evaluation of the IVC, a phased array or curvilinear transducer should be used with the patient lying supine. The diameter of the IVC should be measured in the subcostal long-axis view, 1–2 cm proximal to its connection with the right atrium. The IVC diameter should be measured throughout the respiratory cycle at the same sagittal level, perpendicular to the long axis of the IVC (a 3D probe may assist in the measurement, thanks to the possibility of imaging long-axis and short-axis IVC simultaneously; Fig. 3A) [15]. It is recommended that an IVC diameter < 2.1 cm, collapsing by more than 50% with inspiration, suggests normal RAP, typically around 3 mmHg (range 0–5 mmHg). Conversely, an IVC diameter greater than 2.1 cm with inspiratory collapse < 50% indicates very high RAP (range 10–20 mmHg) [15]. As a potential limitation, not all patients can tolerate the assessment of IVC, and prolonged training and experience are required to identify and evaluate IVC in most patients [44].
Internal jugular vein (IJV). IJV distension is a proxy for CVP and represents an additional strategy to evaluate systemic venous congestion. Similar to the IVC, IJV distension is associated with a high risk of HF hospitalisation and disease progression [45]. A clinically distended IJV is a powerful marker of poor prognosis in patients with heart failure [45]. However, estimating JVP only by physical exam is often challenging, as the reliability of the evaluation depends on the clinician’s experience, examination time, body size, and intra-thoracic pressure fluctuations [46]. US-based IJV evaluation allows for precise assessment of the diameter of the IJV and its variations during the Valsalva manoeuvre [10] and identifies patients with higher RAP at greater risk [45, 47].
The right IJV lies close to the carotid artery beneath the sternocleidomastoid muscle, allowing easy access for ultrasound examination. For precise evaluation, the patient is studied in a semi-supine position, with the head and neck elevated at approximately 45 degrees, using a high-frequency linear transducer positioned below the jaw angle along the sternocleidomastoid muscle, moving downward toward the angle of Louis [10]. Evaluations performed with the patient in the supine or sitting position should be avoided as they are associated with overdistension and collapse of the IJV, respectively. During the US examination, the diameter of the IJV is measured both at rest and during the Valsalva manoeuvre, either with M-mode or 2D-US (Fig. 3B). The JVD (Jugular Venous Distensibility) ratio is also calculated as the ratio of the IJV diameter during Valsalva to the IJV diameter at rest; this parameter is consistent across different observers [10]. In euvolemic patients with HF, the resting IJV diameter is usually ~ 0.15 cm and increases 5–6 times (i.e., up to 1 cm) during a Valsalva manoeuvre [48, 49]. The maximal diameter achievable during Valsalva remains largely consistent across patients due to the limited compliance of the vessel. Therefore, fluid overload is associated with increased IJV diameter at rest and, in turn, a lower JVD ratio (< 4). [39, 48, 49]. A reduced JVD ratio correlates with more severe symptoms, elevated natriuretic peptides, right ventricular dysfunction, and tricuspid regurgitation [48], but not with LVEF. It also predicts an increased risk of HF-related hospitalisations and death independently of natriuretic peptides [39, 46, 49]. Furthermore, some studies have suggested that the cross-sectional area of the IJV, measured during the Valsalva manoeuvre, might be a more reliable index of RAP [50, 51]. Again, significant variations in the IJV area during Valsalva usually indicate normal CVP and are associated with better prognostic outcomes [50, 51].
One potential limitation of the US evaluation of the IJV is the difficulty in avoiding excess pressure with consequent IJV compression during the examination [52]. This issue may affect the reliability of the measurements and introduce interobserver and intraobserver variability, especially when estimating the volume status and fluid responsiveness in critically ill patients. Therefore, care must be taken to apply the minimum pressure required for the examination [52]. Furthermore, the Valsalva manoeuvre, crucial for effective measurement, can be particularly challenging for acutely unwell patients. For such cases, alternative techniques such as passive leg raising might be considered to estimate CVP, though their impact on the IJV diameter needs further investigation.
Liver US. Doppler evaluation of venous blood flow from the splanchnic district to the liver (i.e., portal venous flow, PVF) and from the liver to the heart (i.e., hepatic venous flow, HVF; Fig. 4) refines the characterisation of systemic congestion and its impact on abdominal organs in HF [16, 53]. Under normal conditions, due to the distensible nature of the hepatic veins, HVF is pulsatile, reflecting the dynamic changes in RAP with each cardiac cycle [16]. The typical waveform observed in the hepatic veins is triphasic, with S- and D-waves directed towards the heart (and away from the liver), indicating systolic and early diastolic right atrial filling; the S-wave is physiologically higher than the D-wave. During late diastole, in the absence of arrhythmias such as atrial fibrillation, the atrial contraction generates a brief A-wave directed towards the liver (and away from the heart). Since venous wall distensibility diminishes as the distance from the right atrium increases, venous flow becomes continuous in more peripheral systemic veins. In particular, the portal vein is at least partially insulated from the right atrium by the resistance of hepatic sinusoids; as a consequence, physiological PVF is continuous or only mildly pulsatile and displays a hepatopetal direction (i.e., it is directed towards the liver) [16, 53]. However, in the presence of worsening venous congestion, the compliance of the IVC reaches a plateau, and the amount of pressure transmitted upstream from the right atrium increases. This results in venous dilation and loss of the physiologic triphasic waveform in the hepatic veins, with a blunted or even reversed S-wave (especially if significant tricuspid regurgitation is present) and the appearance of a positive V-wave indicating right atrial overfilling with subsequent flow recoil towards the liver. Likewise, a shift from continuous to pulsatile PVF may appear, possibly with a brief flow reversal phase (i.e., hepatofugal PVF) during systole in most severe cases [54]. The severity of the alterations in flow dynamics in the portal vein can be quantitatively assessed using parameters like the pulsatility fraction, calculated as the difference between the maximal and minimal PVF velocities, divided by maximal PVF velocity and expressed as a percentage. While no agreed-upon cut-points exist for this parameter, an increased PVF pulsatility fraction has been associated with right ventricular dysfunction and increased CVP [16, 55, 56].
Right. Doppler evaluation of portal vein flow (PVF). A Healthy subject; PVF pulsatility fraction = 7%. B Outpatient with HF with mildly abnormal PVF (pulsatility fraction = 42%.). C Patient hospitalised due to acute HF showing systolic flow reversal (hepatofugal PVF). HF: heart failure. PVF: portal venous flow. Left. Doppler evaluation of hepatic venous flow (HVF). (1) Healthy subject with typical triphasic HVF: the S-wave is higher than the D-wave, with a brief A-wave generated by atrial contraction. (2) Patient with heart failure and atrial fibrillation, showing a blunted S-wave without the A-wave. (3) Patient with severe tricuspid regurgitation and atrial fibrillation, showing a reversed S-wave without the A-wave
The patient is typically supine or in left lateral decubitus for Doppler evaluation of the hepatic and portal veins. Liver vessels can be identified by positioning a curvilinear or phased array probe in the mid-to-posterior axillary line with the probe marker directed toward the patient’s head and color Doppler imaging with the flow scale adjusted to low-flow velocities (preferably ≤ 20 cm/s) [16]. Measurements should be performed during a breath-hold to mitigate any distortions caused by breathing [16]. Doppler evaluation of the HVF and PVF presents specific challenges. Even in patients with severe tricuspid regurgitation, HVF might not be impaired if the compliance of the right atrium is maintained; this indicates that the evaluation of HVF could potentially underestimate the degree of venous congestion [57]. On the other hand, pulsatile PVF can be observed in healthy, thin individuals and patients with arteriovenous malformations [57]. Also, patients with increased liver stiffness, e.g., liver cirrhosis or metabolic dysfunction-associated steatotic liver disease, may have a non-pulsatile PVF despite severe venous congestion due to a lack of pressure transmission from the right atrium through the liver sinusoid [57].
Renal venous flow (RVF). Doppler-derived evaluation of RVF is emerging as a valuable tool in managing HF, though its clinical usefulness is still under investigation [10]. In euvolemic patients, RVF is continuous, with negligible fluctuations during the cardiac cycle. As CVP increases and intravascular congestion worsens, these fluctuations increase in magnitude, resulting in discontinuous RVF, which can be further categorised qualitatively as pulsatile, biphasic, or even monophasic (Fig. 5). Quantitative metrics such as the venous impedance index (VII) and venous discontinuity index (VDI) further refine the characterisation of renal congestion. The VII is calculated as the difference between the maximum and minimum flow velocities, divided by the maximum flow velocity and expressed as a percentage [3, 10]. Thus, a higher VII indicates increased impedance, with a score of 0 denoting uniform flow and 1 indicating complete flow interruption during the cardiac cycle [3, 10]. Conversely, the VDI is defined as the proportion of the cardiac cycle where flow is absent, again expressed as a percentage [10]. Abnormal RVF patterns correlate with heightened CVP and poorer prognosis in both acute and chronic HF [58, 59]. This is not surprising, as in the presence of elevated CVP, pressure in the interstitium of the encapsulated kidneys is also raised [54], which may lead to further deregulated release of neurohormones, partial collapse of the nephrons, and renal ischaemia, increasing the risk of acute kidney injury [60, 61, 10]. Interestingly, changes in RVF may precede alterations in other echographic indices of congestion, highlighting RVF as a potential early indicator of fluid overload and diuretic response [10].
The patient is placed in the left lateral decubitus position to perform Doppler-derived RVF acquisition and the right kidney is scanned longitudinally during an end-expiratory breath-hold [3], with a convex transducer or phased array aligned at the lowest intercostal view [10]. Color-Doppler imaging (set for peak velocities ≤ 20 cm/s) allows the identification of interlobar veins. The ECG signal is useful for synchronising the RVF signal with the cardiac cycle, ensuring precise timing of measurements [3]. Noteworthy, RVF evaluation may be technically challenging and result in suboptimal recordings if the sonographer is unfamiliar with the technique, albeit we observed a rapid learning curve [3]. Additionally, intrinsic renal diseases could alter intrarenal Doppler venous waveforms, further complicating the interpretation of results [57].
Conclusions: gap of knowledge and next steps
Identifying and effectively managing fluid overload are critical steps to improve the well-being and prognosis of patients with HF [4]. US is widely available, and several techniques have emerged as reliable, radiation-free, low-cost, non-invasive solutions to evaluate congestion in patients with HF (Table 1). Particularly, serial LUS and IVC evaluations are emerging as valuable tools to tailor diuretic therapy in HF, with encouraging results from preliminary randomised controlled trials [62]. Furthermore, US can reduce the need for radiation-based imaging techniques like chest X-rays and CT scans, lowering radiation exposure, patient transport needs, and hospital costs [35]. However, these techniques are limited by constraints that can hinder their utility in specific situations. Such limitations could be offset by integrating multiple US findings in scoring systems such as the Venous Excess UltraSound (VExUS) scoring system [16, 54]. Indeed, the VExUS score, which incorporates US evaluation of the IVC, HVF, PVF, and RVF, has been proposed to refine the assessment of systemic congestion and enhance clinical decision-making, especially in intensive care settings [16, 63]. Recent findings suggest that specific markers included in the VExUS score—such as intra-renal patterns and PV pulsatility—can improve risk stratification, albeit evidence is still insufficient to support the routine use of the VExUS score to guide decongestion (64). Given that a multi-organ approach can be time-consuming, further research should focus on optimising the combination of ultrasound techniques to develop the most efficient diagnostic algorithm and ultimately improve patient outcomes.
References
McDonagh TA, Metra M, Adamo M et al (2021) 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J 42(36):3599–3726
Harjola V-P, Mullens W, Banaszewski M et al (2017) Organ dysfunction, injury and failure in acute heart failure: from pathophysiology to diagnosis and management. A review on behalf of the Acute Heart Failure Committee of the Heart Failure Association (HFA) of the European Society of Cardiology (ESC). Eur J Heart Fail 19(7):821–836
Pugliese NR, Pellicori P, Filidei F et al (2023) The incremental value of multi-organ assessment of congestion using ultrasound in outpatients with heart failure. Eur Hear J Cardiovasc Imaging 24:961–971
Abraham WT, Adamson PB, Bourge RC et al (2011) Wireless pulmonary artery haemodynamic monitoring in chronic heart failure: a randomised controlled trial. Lancet 377(9766):658–666
Lindenfeld JA, Zile MR, Desai AS et al (2021) Haemodynamic-guided management of heart failure (GUIDE-HF): a randomised controlled trial. Lancet 398(10304):991–1001
Girerd N, Seronde M-F, Coiro S et al (2018) Integrative assessment of congestion in heart failure throughout the patient journey. JACC Hear Fail 6(4):273–285
Mullens W, Damman K, Harjola VP et al (2019) The use of diuretics in heart failure with congestion — a position statement from the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail 21(2):137–155
Correale M, Fioretti F, Tricarico L et al (2023) The role of congestion biomarkers in heart failure with reduced ejection fraction. J Clin Med 12(11):3834
Ponikowski P, Voors AA, Anker SD et al (2016) 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J 37(27):2129–2200
Pellicori P, Platz E, Dauw J et al (2021) Ultrasound imaging of congestion in heart failure: examinations beyond the heart. Eur J Heart Fail 23(5):703–712
Lee KK, Doudesis D, Anwar M et al (2022) Development and validation of a decision support tool for the diagnosis of acute heart failure: systematic review, meta-analysis, and modelling study. BMJ 377:e068424
Chubuchny V, Pugliese NR, Taddei C et al (2021) A novel echocardiographic method for estimation of pulmonary artery wedge pressure and pulmonary vascular resistance. ESC Hear Fail. https://doi.org/10.1002/ehf2.13183
Gheorghiade M, Follath F, Ponikowski P et al (2010) Assessing and grading congestion in acute heart failure: a scientific statement from the acute heart failure committee of the heart failure association of the European society of cardiology and endorsed by the European society of intensive care medicine. Eur J Heart Fail 12(5):423–433
Volpicelli G, Elbarbary M, Blaivas M et al (2012) International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med. https://doi.org/10.1007/s00134-012-2513-4
Lang RM, Badano LP, Mor-Avi V et al (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American society of echocardiography and the European association of cardiovascular imaging. Eur Heart J Cardiovasc Imaging 16(3):233–271
Argaiz ER (2021) VExUS nexus: bedside assessment of venous congestion. Adv Chronic Kidney Dis 28(3):252–261
Sharifov OF, Schiros CG, Aban I, Denney TS, Gupta H (2016) Diagnostic accuracy of tissue doppler index E/e' for evaluatingleft ventricular filling pressure and diastolic dysfunction/heart failure with preserved ejection fraction: a systematicreview and meta-analysis. J Am Heart Assoc 5(1):e002530. https://doi.org/10.1161/JAHA.115.002530
Nagueh SF, Smiseth OA, Appleton CP et al (2016) Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 29(4):277–314
Pellicori P, Cleland JGF (2024) Atrial myopathy and heart failure with preserved ejection fraction: when a label does more harm than good? Eur J Heart Fail 26:299–301
Pugliese NR, De Biase N, Conte L et al (2021) Cardiac reserve and exercise capacity: insights from combined cardiopulmonary and exercise echocardiography stress testing. J Am Soc Echocardiogr 34(1):38–50
Reddy YNV, Obokata M, Wiley B et al (2019) The haemodynamic basis of lung congestion during exercise in heart failure with preserved ejection fraction. Eur Heart J 40(45):3721–3730
Scali MC, Cortigiani L, Simionuc A, Gregori D, Marzilli M, Picano E (2017) Exercise-induced B-lines identify worse functional and prognostic stage in heart failure patients with depressed left ventricular ejection fraction. Eur J Heart Fail 19(11):1468–1478
Pugliese NR, De Biase N, Gargani L et al (2021) Predicting the transition to and progression of heart failure with preserved ejection fraction: a weighted risk score using bio-humoural, cardiopulmonary, and echocardiographic stress testing. Eur J Prev Cardiol 28(15):1650–1661
Del PL, De BN, Di FV et al (2023) Combining cardiopulmonary exercise testing with echocardiography: a multiparametric approach to the cardiovascular and cardiopulmonary systems. Eur Hear J Imaging Methods Pract 1(1):1–12
Pugliese NR, Mazzola M, Madonna R et al (2022) Exercise-induced pulmonary hypertension in HFpEF and HFrEF: different pathophysiologic mechanism behind similar functional impairment. Vascul Pharmacol 144:106978
Pugliese NR, Mazzola M, Fabiani I et al (2020) Haemodynamic and metabolic phenotyping of hypertensive patients with and without heart failure by combining cardiopulmonary and echocardiographic stress test. Eur J Heart Fail. https://doi.org/10.1002/ejhf.1739
Pugliese NR, Fabiani I, Santini C et al (2019) Value of combined cardiopulmonary and echocardiography stress test to characterize the haemodynamic and metabolic responses of patients with heart failure and mid-range ejection fraction. Eur Heart J Cardiovasc Imaging 20(7):828–836
Pivetta E, Goffi A, Nazerian P et al (2019) Lung ultrasound integrated with clinical assessment for the diagnosis of acute decompensated heart failure in the emergency department: a randomized controlled trial. Eur J Heart Fail 21(6):754–766
Buessler A, Chouihed T, Duarte K et al (2019) Accuracy of several lung ultrasound methods for the diagnosis of acute heart failure in the ED. Chest. https://doi.org/10.1016/j.chest.2019.07.017
Copetti R, Soldati G, Copetti P (2008) Chest sonography: a useful tool to differentiate acute cardiogenic pulmonary edema from acute respiratory distress syndrome. Cardiovasc Ultrasound 6:1–10
Wang Y, Gargani L, Barskova T, Furst DE, Cerinic MM (2017) Usefulness of lung ultrasound B-lines in connective tissue disease-associated interstitial lung disease: a literature review. Arthritis Res Ther 19(1):206
Palazzuoli A, Ruocco G, Franci B et al (2020) Ultrasound indices of congestion in patients with acute heart failure according to body mass index. Clin Res Cardiol 109(11):1423–1433
Frasure SE, Matilsky DK, Siadecki SD, Platz E, Saul T, Lewiss RE (2015) Impact of patient positioning on lung ultrasound findings in acute heart failure. Eur Hear J Acute Cardiovasc Care 4(4):326–332
Pivetta E, Baldassa F, Masellis S, Bovaro F, Lupia E, Maule MM (2018) Sources of variability in the detection of B-lines. Using Lung Ultrasound Ultrasound Med Biol 44(6):1212–1216
Platz E, Campbell RT, Claggett B et al (2019) Lung ultrasound in acute heart failure: prevalence of pulmonary congestion and short- and long-term outcomes. JACC Hear Fail 7(10):849–858
Platz E, Lewis EF, Uno H et al (2016) Detection and prognostic value of pulmonary congestion by lung ultrasound in ambulatory heart failure patients. Eur Heart J 37(15):1244–1251
Jambrik Z, Monti S, Coppola V et al (2004) Usefulness of ultrasound lung comets as a nonradiologic sign of extravascular lung water. Am J Cardiol 93(10):1265–1270
Gargani L, Sicari R, Raciti M et al (2016) Efficacy of a remote web-based lung ultrasound training for nephrologists and cardiologists: a lust trial sub-project. Nephrol Dial Transplant 31(12):1982–1988
Pellicori P, Shah P, Cuthbert J et al (2019) Prevalence, pattern and clinical relevance of ultrasound indices of congestion in outpatients with heart failure. Eur J Heart Fail 21(7):904–916
Kircher BJ, Himelman RB, Schiller NB (1990) Noninvasive estimation of right atrial pressure from the inspiratory collapse of the inferior vena cava. Am J Cardiol 66(4):493–496
Pellicori P, Carubelli V, Zhang J et al (2013) IVC diameter in patients with chronic heart failure: relationships and prognostic significance. JACC Cardiovasc Imaging 6(1):16–28
Goonewardena SN, Gemignani A, Ronan A et al (2008) Comparison of hand-carried ultrasound assessment of the inferior vena cava and N-terminal pro-brain natriuretic peptide for predicting readmission after hospitalization for acute decompensated heart failure. JACC Cardiovasc Imaging 1(5):595–601
Nagueh SF, Kopelen HA, Zoghbi WA (1996) Relation of mean right atrial pressure to echocardiographic and Doppler parameters of right atrial and right ventricular function. Circulation 93(6):1160–1169
Zisis G, Yang Y, Huynh Q et al (2022) Nurse-provided lung and inferior vena cava assessment in patients with heart failure. J Am Coll Cardiol 80(5):513–523
Drazner MH, Rame JE, Stevenson LW, Dries DL (2001) Prognostic importance of elevated jugular venous pressure and a third heart sound in patients with heart failure. N Engl J Med 345(8):574–581
Pellicori P, Clark AL, Kallvikbacka-Bennett A et al (2017) Non-invasive measurement of right atrial pressure by near-infrared spectroscopy: preliminary experience. A report from the SICA-HF study. Eur J Heart Fail 19(7):883–892
Ammirati E, Marchetti D, Colombo G et al (2024) Estimation of right atrial pressure by ultrasound-assessed jugular vein distensibility in patients with heart failure. Circ Hear Fail 17(2):E010973
Pellicori P, Kallvikbacka-Bennett A, Zhang J et al (2014) Revisiting a classical clinical sign: jugular venous ultrasound. Int J Cardiol 170(3):364–370
Pellicori P, Kallvikbacka-Bennett A, Dierckx R et al (2015) Prognostic significance of ultrasound-assessed jugular vein distensibility in heart failure. Heart 101(14):1149–1158
Simon MA, Kliner DE, Girod JP, Moguillansky D, Villanueva FS, Pacella JJ (2010) Detection of elevated right atrial pressure using a simple bedside ultrasound measure. Am Heart J 159(3):421–427
Simon MA, Schnatz RG, Romeo JD, Pacella JJ (2018) Bedside ultrasound assessment of jugular venous compliance as a potential point-of-care method to predict acute decompensated heart failure 30-day readmission. J Am Heart Assoc 7(15):1–8
Parenti N, Scalese M, Palazzi C, Agrusta F, Cahill J, Agnelli G (2019) Role of internal jugular vein ultrasound measurements in the assessment of central venous pressure in spontaneously breathing patients : a systematic review. J Acute Med 9(2):39–48
Interactions C (2019) Heart failure and liver disease. JACC: Heart Fail 7(2):87–97
Bhardwaj V, Vikneswaran G, Rola P et al (2020) Combination of inferior vena cava diameter, hepatic venous flow, and portal vein pulsatility index: venous excess ultrasound score (vexus score) in predicting acute kidney injury in patients with cardiorenal syndrome: a prospective cohort study. Indian J Crit Care Med 24(9):783–789
Kumar KN, Nagaraja PS (2020) Portal venous pulsatility fraction, a novel transesophageal echocardiographic marker for right ventricular dysfunction in cardiac surgical patients. Ann Card Anaesth 23:39–42
Eljaiek R, Cavayas YA, Rodrigue E et al (2019) High postoperative portal venous flow pulsatility indicates right ventricular dysfunction and predicts complications in cardiac surgery patients. Br J Anaesth 122(2):206–214
Rola P, Miralles-Aguiar F, Argaiz E et al (2021) Clinical applications of the venous excess ultrasound (VExUS) score: conceptual review and case series. Ultrasound J. https://doi.org/10.1186/s13089-021-00232-8
Iida N, Seo Y, Sai S et al (2016) Clinical implications of intrarenal hemodynamic evaluation by doppler ultrasonography in heart failure. JACC Hear Fail 4(8):674–682
Mullens W, Abrahams Z, Francis GS et al (2009) Importance of venous congestion for worsening of renal function in advanced decompensated heart failure. J Am Coll Cardiol 53(7):589–596
De VR, Ariano C, Fusco A et al (2012) Ultrasound evaluation of the inferior vena cava collapsibility index in congestive heart failure patients treated with intravenous diuretics : new insights about its relationship with renal function : An observational study. Anadolu Kardiyol Derg. https://doi.org/10.5152/akd.2012.121
Zhang L, Chen Z, Diao Y, Yang Y, Fu P (2015) Associations of fluid overload with mortality and kidney recovery in patients with acute kidney injury: a systematic review and meta-analysis. J Crit Care 30(4):860.e7–13
Rastogi T, Bozec E, Pellicori P et al (2022) Prognostic value and therapeutic utility of lung ultrasound in acute and chronic heart failure: a meta-analysis. JACC Cardiovasc Imaging 15:950–952
Torres-Arrese M, Mata-Martínez A, Luordo-Tedesco D et al (2023) Usefulness of systemic venous ultrasound protocols in the prognosis of heart failure patients: results from a prospective multicentric study. J Clin Med 12(4):1281
Rocca E, Zanza C, Longhitano Y et al (2023) Lung ultrasound in critical care and emergency medicine : clinical review. Adv Respiratory Med 91:203–223
Galiè N, Humbert M (2015) 2015 ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension: the joint task force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS). Eur Hear J 37:67–119
Funding
Open access funding provided by Università di Pisa within the CRUI-CARE Agreement. The research leading to these results has received funding from the European Union - NextGenerationEU through the Italian Ministry of University and Research under PNRR - M4C2-I1.3 Project PE_00000019 "HEAL ITALIA" to Stefano Taddei, CUP I53C22001440006. The views and opinions expressed are those of the authors only and do not necessarily reflect those of the European Union or the European Commission. Neither the European Union nor the European Commission can be held responsible for them.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares that (s)he has no relevant or material financial interests that relate to the research described in this paper.
Informed consent
For this type of study, formal consent is not required.
Human and animal rights
This article does not contain any studies with human participants or animal performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Di Fiore, V., Del Punta, L., De Biase, N. et al. Integrative assessment of congestion in heart failure using ultrasound imaging. Intern Emerg Med (2024). https://doi.org/10.1007/s11739-024-03755-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11739-024-03755-9