Abstract
Background
Older patients presenting to the emergency department (ED) after falling are increasingly prevalent. Falls are associated with functional decline and death. Biomarkers predicting short-term mortality might facilitate decisions regarding resource allocation and disposition. D-dimer levels are used to rule out thromboembolic disease, while copeptin and adrenomedullin (MR-proADM) may be used as measures of the patient`s stress level. These nonspecific biomarkers were selected as potential predictors for mortality.
Methods
Prospective, international, multicenter, cross-sectional observation was performed in two tertiary and two regional hospitals in Germany and Switzerland. Patients aged 65 years or older presenting to the ED after a fall were enrolled. Demographic data, Activities of Daily Living (ADL), and D-dimers were collected upon presentation. Copeptin and MR-proADM levels were determined from frozen samples. Primary outcome was 30-day mortality; and secondary outcomes were mortality at 90, 180, and 365 days.
Results
Five hundred and seventy-two patients were included. Median age was 83 [IQR 78, 89] years, 236 (67.7%) were female. Mortality overall was 3.1% (30 d), 5.4% (90 d), 7.5% (180 d), and 13.8% (365 d), respectively. Non-survivors were older, had a lower ADL index and higher levels of all three biomarkers. Elevated levels of MR-proADM and D-dimer were associated with higher risk of mortality. MR-proADM and D-dimer showed high sensitivity and low negative likelihood ratio regarding short-term mortality, whereas copeptin did not.
Conclusion
D-dimer and MR-proADM levels might be useful as prognostic markers in older patients presenting to the ED after a fall, by identifying patients at low risk of short-term mortality.
Trial registration
ClinicalTrials.gov Identifier: NCT02244983.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Falls are frequent in aging populations. Falls in older people present a major public health problem and are a challenge to emergency departments (ED) [1, 2]. Almost one-third of all adults aged 65 years and older report a fall at least once a year [3]. Up to 30% of all ED presentations in this age group are related to falls [1], and they may account for 74.3% of major trauma cases [4]. Falls in older adults seem to be associated with high injury severity, reduced mobility, functional decline, and death [5, 6].
Although the incidence and severity of fall-related complications steadily increase after the age of 60 [3, 4, 6, 7], age is not the only factor with an impact regarding risk of falling and related outcomes. Other factors, such as frailty, gender, and co-morbidity [6], are associated with adverse outcomes among patients presenting to the ED after a fall.
Importantly, ED presentation after a fall may be a warning sign of a range of serious conditions [8]. Older adults, particularly with a history of falls, require a thorough work-up, as the risk of secondary deterioration due to missed diagnoses [9] or delirium [10, 11] is considerable. However, such work-ups may lead to excessive hospitalization in a population at risk for long-term institutionalization [12], bearing the risk of additional morbidity and mortality [13, 14]. Thus, preventing avoidable hospital admissions is important to disposition planning in the ED [15].
To distinguish between patients at risk of short-term mortality and those potentially benefiting from rapid discharge is a multi-dimensional challenge. Age, acuity, complexity, and Activities of Daily Living (ADL) are some important dimensions, but a measure of stress level could be a novel, additional dimension. Stress-related biomarkers as mortality predictors could provide another useful tool for helping with difficult disposition decisions. Other approaches include observation [16], routine clinical chemistry [17], or decision analysis frameworks [18].
Multicenter observation studies on this topic are currently scarce and results vary considerably [19, 20]. As falls are associated with serious conditions [21] and both resource allocation and disposition are a challenge in these patients, there is a need for better risk stratification in older adults presenting with falls. We performed this multicenter study in an undifferentiated population to assess the stress response associated with a fall. We hypothesized that stress levels could be associated with morbidity and mortality—irrespective of the cause of the fall, age, gender, or ADL. Different stress response systems were examined for their predictive power in relation to 30-day mortality in patients admitted to the ED after a fall, using three different biomarkers such as copeptin, D-dimers, and the mid-regional fragment of adrenomedullin (MR-proADM). These biomarkers were selected for easy assessment in the ED, previous data on their prognostic value, and their association with an acute stress response.
Methods
This report is a secondary analysis of the prospective multicenter observational “Falls of Unknown Origin” (ClinicalTrials.gov Identifier: NCT02244983) study covering four EDs in Northwestern Switzerland and Germany (University Hospital Basel, University Hospital Charité Berlin (tertiary care hospitals), Cantonal Hospital Liestal, Cantonal Hospital Bruderholz (regional hospitals)). Data collection was performed between November 2014 and January 2018.
Patients, aged 65 years and older, who presented to the ED within 24 h after a fall and provided informed consent, were enrolled in the study. Transport accidents and accidents involving machinery were excluded as well as assault and intentional self-harm.
Age, sex, and ADL at presentation [22] were obtained by a designated study team. Blood samples were collected after inclusion and D-dimer levels were immediately determined, extra samples of serum and ethylenediaminetetraacetic acid (EDTA) were frozen at − 80 °C. After the trial’s conclusion, copeptin and MR-proADM were determined in batches from those frozen serum and EDTA samples.
Assays
A viscosity-based detection method with the STA-R system (Diagnostica Stago S.A.S., Asnières sur Seine, Cedex, France) was used to measure D-dimer levels, with detection rate ranging from 0.27 μg/mL up to 20 μg/mL. Citrate plasma for D-dimer estimation was centrifuged at 3500 rpm for 10 min before measurement.
EDTA plasma and serum samples were defrosted and centrifuged at 3400 rpm for 10 min to prepare the samples for measurement. For MR-proADM and copeptin measurements, automated sandwich chemiluminescence immunoassays on the BRAHMS KRYPTOR system (Thermo Scientific Biomarkers, Hennigsdorf, Germany) were used [23, 24].
The MR-proADM KRYPTOR has a detection range of 0.05–100 nmol/L and a functional assay sensitivity of 0.25 nmol/L.
The copeptin proAVP KRYPTOR has a detection range of 0.7–2000 pmol/L and a functional sensitivity of less than 1.59 pmol/L.
All laboratory personnel performing the assays were masked to the patients’ medical information and the purpose of the study.
We used two different cutoff’s for D-dimer: first, we evaluated a common used cutoff of 0.5 µg/mL; and second, we used an age-adjusted patient-individualized cutoff, which was derived by multiplying age by 10 µg/L, as suggested in patients over 50 years of age [25].
Strictly defined cutoffs for MR-proADM and copeptin do not exist. An arbitrary cutoff for MR-proADM was set at 0.75 nmol/L, which was recommended for safe discharge of patients with nonspecific complaints [26, 27]. For copeptin, we used the cutoff suggested by the assay (13.8 pmol/L).
Previous studies have used the first tertiles as cutoff for prognostication in both copeptin and MR-proADM [24, 26, 27]. Both cutoffs chosen above were comparable to the first tertiles of the respective marker in our population (0.72 nmol/L for MR-proADM and 12.23 pmol/L for copeptin).
Outcomes
Mortality
Mortality was followed-up after 30 days, 90 days, 180 days, and 1 year by questionnaires to the patients’ general practitioners, as well as from data from electronic health records, nursing homes, and hospital discharge reports, including in particular all hospitalized or transferred patients.
Gold standard diagnoses
After the 30-day follow-up period, independent outcome assessors reviewed all data obtained from electronic medical records, nursing homes, and hospital discharge reports and questionnaires by the patients’ general practitioners. The outcome assessors were two of four ED physicians with longstanding clinical experience. The outcome assessors were blinded to the study hypothesis. They reviewed all available patient records individually and jointly determined the final gold standard diagnoses. These diagnoses were recorded in written form and as codes according to the International Classification of Diseases and Related Health Problems 10th Revision (ICD-10).
Categorizations: injurious fall, non-injurious fall, and acute medical condition
The definition of injurious fall was used as defined by Rohacek [28]:
-
Any condition that requires invasive procedures, such as surgery
-
Any condition that requires prolonged monitoring, such as acute subdural hematoma
-
Any bone fractures
The definition of acute medical condition was used as defined by Rohacek [28]:
-
Any condition that requires specific medical therapy, such as antibiotics, diuretics, anticoagulants, or antihypertensive drugs
-
Any condition that requires invasive procedures, such as surgery, acute endoscopy, or coronary angiography
-
Any condition that requires prolonged monitoring, such as acute stroke, myocardial infarction, respiratory compromise, metabolic disorder, hemodynamic instability, intracranial or gastrointestinal bleeding, anaphylaxis, or suicidal tendency
Two reviewers independently classified all patients according to the following rule: if the definition of an injurious fall was fulfilled, the patient was classified as category 1 (injurious falls). If there was no injurious fall, but a serious medical condition was present according to the definition of Rohacek, the patient was classified as category 2. If no criteria for category 1 or category 2 were fulfilled, the patient was classified as category 3 (non-injurious fall). Differing assessments were discussed and summarized in a joint assessment.
Statistical methods
Descriptive statistics were expressed as counts and percentages or as medians with interquartile ranges (IQR). Group comparisons were performed using the Mann–Whitney U test for continuous and ordinal variables and the Fisher exact test for nominal variables.
Sensitivity, specificity, positive and negative likelihood ratios (LRs) were calculated for each biomarker cutoff as a measure of diagnostic accuracy, with 95% confidence intervals obtained from the Clopper–Pearson interval method. If sensitivity was 100%, a bootstrapping method was used to estimate negative LR [29].
To predict 30-day mortality for each biomarker (D-dimer, copeptin, MR-ProADM), univariate and multivariate logistic regression was performed, and odds ratios (ORs) were reported. Age, gender, and the Katz ADL were included as a covariate in multivariate analysis. Receiver operating characteristic (ROC) plots were constructed, and area under the curves (AUCs) were calculated for all biomarkers. Only cases with all three biomarkers available were used to construct ROC plots and calculate AUCs. Kaplan–Meier survival curves were drawn for illustrative purposes.
Correlation between all variables used in the regression analysis was quantified as Pearson correlation.
We performed completed case analysis, resulting in two different cohorts: cohort 1 contains all patients with both copeptin and MR-proADM levels available, and cohort 2 contains all patients with D-dimer levels measured at presentation.
All statistical analyses were conducted with the R program (Version 4.2.2, R core team, R Foundation for Statistical Computing. Vienna. Austria).
Ethics
This study was approved by the local ethics committee (identifier 2014-184, ww.eknz.ch) and conducted according to the principles of the Declaration of Helsinki.
Results
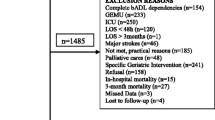
We included 572 patients with complete data in this analysis (Fig. 1). Median age was 83 years [IQR 77, 89], 67.7% of all patients were female, and 77.4% of patients were admitted as inpatients.
At 30-day follow-up, 18 (3.1%) of all included patients had died. Thirty-one (5.4%) died within 90 days and forty-three (7.5%) within 180 days. At the 365-day follow-up, 77 (13.5%) patients had died, while 495 (86.5%) survived. Details of the 18 patients that died within 30 days are shown in Supplemental Table 3.
Non-survivors were older (median 89 vs. 83 years) and had a lower median ADL index (4 vs. 5) compared to patients who survived 30 days (Table 1).
Around half (47.4%) of patients were classified as injurious fall, while around a quarter of patients were classified as acute medical condition (26.5%) and as non-injurious fall (26.1%). These rates were comparable compared to patients who survived 30 days (injurious falls: 47.8%, acute medical conditions: 25.5%, non-injurious falls: 26.6%) but differed significantly for non-survivors, where acute medical conditions accounted for the majority (55.6%) of cases, while injurious falls (37.5%) and non-injurious falls (12.5%) accounted for a smaller part.
In 554 patients, MR-proADM as well as copeptin levels were available (cohort 1), whereas D-dimer measurement was available in 356 patients (cohort 2). Three hundred forty-six cases were included in both cohort 1 and cohort 2 (Fig. 1). A comparison of the cohorts regarding baseline characteristics can be found in the Supplemental Table 1.
Cohort 1
Age and sex distribution as well as overall mortality in cohort 1 were comparable with the complete cohort. Median age was 83.5 years [IQR 77, 89], 67.7% of patients were female and 78% were admitted as inpatients.
At 30-day follow-up, 18 (3.2%) patients had died. Thirty-one (5.6%) died within 90 days and forty-three (7.8%) within 180 days. At the 365-day follow-up, 76 (13.7%) patients had died, while 478 (86.3%) survived. For more details, see Kaplan–Meier curves in Supplemental Figs. 1 and 2.
Based on our predefined cutoffs, 341 (61.6%) patients in cohort 1 had elevated MR-proADM, and 352 (63.5%) had elevated copeptin levels. Median copeptin levels were generally lower in females (17.6 vs. 27.3 pmol/L, p = < 0.001), and there were less females with copeptin levels above the cutoff (57.6% vs. 76%, p = < 0.001), while there was no difference in MR-proADM levels (0.84 vs. 0.9 nmol/L, p = 0.23 and 60.5% vs. 63.7%, p = 0.51).
Patients with MR-proADM levels above 0.75 nmol/L compared to patients with non-elevated MR-proADM levels were older (85 vs. 80 years, p = < 0.001) and had a higher mortality rate within 30 days (5 vs. 0.5% p = 0.008). Patients with elevated copeptin levels were older (85 vs. 81 years, p = < 0.001) and less likely to be female (61.4 vs. 78.7% p = < 0.001). There was no significantly higher mortality rate within 30 days between the groups with and without copeptin elevation (Supplemental Table 2).
Both, patients with elevated MR-proADM levels, and patients with elevated copeptin levels were more likely to be admitted as inpatients, but neither difference was statistically significant (MR-proADM: 80.6 vs. 73.6%, p = 0.059. Copeptin: 80.7 vs. 73.3%, p = 0.055).
In cohort 1, the levels of all biomarkers were significantly higher in non-survivors, as illustrated in Table 1, Fig. 2, and Supplemental Table 2.
In cohort 1, 94.4% of patients who died within 30 days and 93.5% of patients who died within 90 days had a MR-proADM level above the predefined cutoff.
Seventy-eight percent of patients who died within 30 days and 74.2% of patients who died within 90 days had a copeptin level above the predefined cutoff.
The predetermined MR-proADM cutoff showed high sensitivity (0.94, 95% CI 0.73–1.0) and low negative likelihood ratio (0.14, 95% CI 0.02–0.95), but low specificity (0.4, 95% CI 0.35–0.44) for mortality within 30 days.
The predetermined copeptin cutoff showed a sensitivity of 0.78 (95%CI: 0.52–0.94), a specificity of 0.37 (95% CI 0.33–0.41), and a negative likelihood ratio of 0.6 (95% CI 0.25–1.44) for mortality within 30 days (Table 2).
For elevated MR-pro-ADM levels, the odds ratio of dying within 30 days estimated with univariate logistic regression increased 11.12-fold (95% CI 2.26–201.2) compared to normal levels. After adjusting for age, sex, and ADL level at baseline, the odds ratio was 7.65 (95% CI 1.5–138.94) (Table 3).
Odds ratio of dying within a year estimated with univariate logistic regression increased 2.63-fold (95%CI 1.15–4.84) for elevated MR-pro-ADM levels. After adjusting for age, sex, and ADL Index at baseline, the odds ratio for mortality was 1.9 (95% CI 1.05–3.55).
For elevated copeptin levels, the odds ratio of dying within 30 days estimated with univariate logistic regression increased 2.05-fold (95% CI 0.72–7.31) compared to normal levels. After adjusting for age, sex and ADL level at baseline the odds ratio for mortality was 1.0 (95% CI 1.0–1.01).
Odds ratio of dying within a year estimated with univariate logistic regression increased 1.38-fold (95% CI 0.83–2.37) for elevated copeptin levels. After adjusting for age, sex, and ADL Index at baseline, the odds ratio for mortality was 0.97 (95% CI 0.56–1.72).
Adjusting for covariates resulted in change of odds ratio for dying within 30 days for both biomarkers; thus, AUC was only displayed for multivariate logistic regression (Table 3 and Fig. 3).
Cohort 2
Age and sex distribution as well as overall mortality in cohort 2 were comparable with the complete cohort. Median age was 83 years [IQR 78, 89], 66.3% of patients were female and 78.4% were admitted as inpatients. Eleven (3.1%) patients had died at 30-day follow-up, eighteen (5.1%) died within 90 days, and twenty-five (7%) within 180 days. At the 365-day follow-up, 43 (12.1%) patients had died, while 313 (87.9%) survived. For more details, see Kaplan–Meier curves in Supplemental Figs. 3 and 4.
In cohort 2, there were 321 (90.2%) patients with D-dimer levels above the usual cutoff (< 0.5 µg/mL), and 281 (78.9%) with D-Dimers above the age-adjusted cutoff (patient’s age /100 µg/mL) (Table 1).
Median D-dimer levels were higher in females (2.34 vs. 1.73 µg/mL, p = 0.017), and there were more females with D-dimer levels above the age-adjusted cutoff (82.6% vs. 71.7%, p = 0.02), but not above the usual cutoff (91.9% vs. 86.7%, p = < 0.132).
Patients with elevated D-dimer levels (cutoff > 0.5) were older (84 vs. 76 years, p < 0.001), more likely to be admitted as inpatients (80.1 vs. 62.9%, p = 0.029), and had higher mortality rate within 30 days (3.4% vs. 0) compared to patients with non-elevated D-dimer levels (Supplemental Table 2).
In cohort 2, the levels of all three biomarkers were significantly higher in non-survivors, as illustrated in Table 1, Fig. 2, and Supplemental Table 2.
In cohort 2, none of the 11 patients who died within 30 days and the 18 patients who died within 90 days had a D-dimer below the regular, or age-adjusted cutoff.
The regular D-dimer cutoff showed high sensitivity (1.0 95% CI 0.72–1.0) and low negative likelihood ratio (0.0, 95% CI 0.0–2.47), but low specificity (0.10, 95% CI 0.07–0.14). The age-adjusted cutoff shows a higher specificity (0.22, 95% CI 0.18–0.26) without loss of sensitivity (Table 2).
For elevated D-dimer levels, the univariate logistic regression shows an increased odds ratio for mortality within 30 days both for common threshold (OR 2.63 (95% CI 0.33–340.5)) as well as for age-adjusted threshold (OR 6.55 (95% CI 0.84–844.62)). After adjusting for age, sex, and ADL Index at baseline, the odds ratio for mortality within 30 days is 1.2 for common threshold (95% CI 0.12–163.39) and 3.08 for age-adjusted threshold (95% CI 0.36–402.4) (Table 3).
Odds ratio of dying within a year estimated with univariate logistic regression shows an increased odds ratio for elevated D-dimer levels both for common threshold (OR 1.93 (95% CI 0.61–9.71)) as well as for age-adjusted threshold (OR 2.52 (95% CI 1.01–8.02)). After adjusting for age, sex, and ADL Index at baseline, the odds ratio was 1.26 for common threshold (95% CI 0.37–6.54) and 1.98 for age-adjusted threshold (95% CI 0.76–6.46) (Fig. 3).
The correlation between all variables used in the regression analyses is shown in Supplemental Fig. 5.
Discussion
The main results of our study were the relatively low short-term mortality and the relatively high levels of stress biomarkers in patients presenting to the ED after a fall. Poor prognosis was associated with serious underlying conditions rather than injury pattern.
Patients with low D-dimer and low MR-proADM levels had a low risk of short-term mortality. Although this group was a minority, D-dimers and MR-proADM may be used as “rule-out” tests regarding mortality in patients presenting after a fall. These results are in line with findings in other ED populations with favorable prognoses when biomarker levels were low [26, 30].
The low short-term mortality in patients with negative D-dimer levels was not affected by the use of an age-adjusted cutoff (patient's age/100 µg/mL) [25], but more patients could be ruled out.
Both MR-proADM and D-dimer elevation were shown to be predictive of short-term mortality in our study. Copeptin, which has shown predictive value in previous studies in other populations [31], was outperformed by MR-proADM, as well as by D-dimers, and it correlated with MR-proADM levels.
The rationale for choosing these biomarkers as potential predictors merits discussion:
D-dimers are commonly used to rule out thromboembolic disease, and were elevated in up to 50% in certain ED cohorts [32]. It has been suggested that D-dimers might be used as a non-specific prognostic marker [30, 32, 33], even in a high-risk geriatric population of ED patients presenting with non-specific complaints [34], such as falls of unknown origin. On the other hand, routine assessment of D-dimer levels may be criticized for the possible subsequent search for thromboembolism in case of elevation and the resulting expose to radiation and elevated costs. However, elevated D-dimers should not be taken as an isolated reason for such examinations.
Copeptin, apart from its merits in polyuria-polydipsia syndrome [35], may be used as a measure of a patient’s stress level [31] and can also be used to rule out myocardial infarction in the ED [36].
MR-proADM, as a surrogate for adrenomedullin, rises in response to inflammatory and physiological stress [37].
Copeptin and MR-proADM have both shown to have prognostic value in patients presenting with sepsis, heart disease, lower respiratory tract infections, and chronic obstructive pulmonary disease (COPD) [31, 37,38,39,40]. In patients presenting with nonspecific complaints (NSCs), both biomarkers have shown useful prognostic properties [24, 26]. Taken together, the selected biomarkers have been shown to be nonspecific markers of physiologic stress in patients presenting to the ED, and were, therefore, candidates for risk stratification in older patients with falls.
As disposition decisions are difficult in the population studied, stress-marker testing could deliver additional important information and also ameliorate throughput and output of these patients in the ED in times of ED crowding and overload. Although age, acuity, morbidity, and the amount of daily support received are essential considerations for disposition, no current evidence-based framework is convincing. To reduce unnecessary hospital admissions in older patients with nonspecific complaints (a majority accompanied by falls), observation has been suggested [16]. This may lead to more appropriate disposition but depends on the availability of observation units. The reason for observation is mostly indecision due to a lack of a solid prognosis. In unselected ED cohorts, routine clinical chemistry may be used for prediction, but this has never been shown to aid disposition decisions in older patients. Furthermore, there are only a few interventional studies on the use of biomarkers in helping with disposition decisions [27, 41], and in all of them, overruling of algorithms by clinicians was a challenge and a potential bias.
The findings of this study could support ED physicians in identifying patients at low risk of short-term mortality assisting with discharge decisions in these patients. However, mortality is only one preventable outcome, and for older patients, certain outcomes, such as dependency, may be even less desirable [42]. ED physicians tend to take conservative decisions in older patients, as they fear short-term mortality, and identifying low risk patients could potentially reduce unnecessary hospitalizations.
Limitations
While this study tried to eliminate geographic bias by the inclusion of four different centers in two different countries, the study population predominantly consisted of European natives, limiting the generalizability of the results. Since not all three biomarkers could be examined in all patients of the study population, a possible selection error may have occurred. Because mortality was low for both cohorts, the ORs may be inflated. Patients were only included during day shift, and it is possible that falls at night have more serious consequences. Further, patients in need of life-saving interventions (ESI 1; MTS 1) could not be included due to ethical considerations.
Conclusion
This study shows that D-dimer and MR-proADM levels could be useful prognostic markers in older patients presenting to the ED after a fall, particularly by identifying patients at low risk of short-term mortality. Copeptin did not provide additional predictive value in this population.
Data availability
The data analyzed during the presented study are available upon reasonable request from the corresponding author.
Abbreviations
- ED:
-
Emergency department
- MR-proADM:
-
Mid-regional proadrenomedullin
- ADL:
-
Activities of daily living
- IQR:
-
Interquartile range
- EDTA:
-
Ethylenediaminetetraacetic acid
- OR:
-
Odds ratio
- ROC:
-
Receiver operating characteristic
- AUC:
-
Area under the curve
- COPD:
-
Chronic obstructive pulmonary disease
- NSC:
-
Nonspecific complaint
- ESI:
-
Emergency severity index
- MTS:
-
Manchester triage system
- LR + :
-
Positive likelihood ratio
- LR-:
-
Negative likelihood ratio
- CI:
-
Confidence interval
References
Close JC, Lord SR, Antonova EJ, Martin M, Lensberg B, Taylor M et al (2012) Older people presenting to the emergency department after a fall: a population with substantial recurrent healthcare use. Emerg Med J 29(9):742–747. https://doi.org/10.1136/emermed-2011-200380
Samaras N, Chevalley T, Samaras D, Gold G (2010) Older patients in the emergency department: a review. Ann Emerg Med 56(3):261–269. https://doi.org/10.1016/j.annemergmed.2010.04.015
Rubenstein LZ, Josephson KR (2002) The epidemiology of falls and syncope. Clin Geriatr Med 18(2):141–158. https://doi.org/10.1016/s0749-0690(02)00002-2
NSW Agency for Clinical Innovation. Major Trauma in NSW: 2019-20. Sydney: ACI; 2020. https://aci.health.nsw.gov.au/__data/assets/pdf_file/0005/629114/ACI-Major-trauma-NSW-2019-20-report.pdf. Accessed 23 August 2022
Hammouda N, Carpenter CR, Hung WW, Lesser A, Nyamu S, Liu S et al (2021) Moving the needle on fall prevention: a geriatric emergency care applied research (GEAR) Network scoping review and consensus statement. Acad Emerg Med 28(11):1214–1227. https://doi.org/10.1111/acem.14279
Kojima G (2015) Frailty as a predictor of future falls among community-dwelling older people: a systematic review and meta-analysis. J Am Med Dir Assoc 16(12):1027–1033. https://doi.org/10.1016/j.jamda.2015.06.018
Carpenter CR, Arendts G, Hullick C, Nagaraj G, Cooper Z, Burkett E (2017) Major trauma in the older patient: evolving trauma care beyond management of bumps and bruises. Emerg Med Australas 29(4):450–455. https://doi.org/10.1111/1742-6723.12785
Causes of falls (2021) https://www.nhsinform.scot/healthy-living/preventing-falls/causes-of-falls. Accessed 12 Sep 2022
Peng A, Rohacek M, Ackermann S, Ilsemann-Karakoumis J, Ghanim L, Messmer AS et al (2015) The proportion of correct diagnoses is low in emergency patients with nonspecific complaints presenting to the emergency department. Swiss Med Wkly 145:w14121. https://doi.org/10.4414/smw.2015.14121
Hasemann W, Grossmann FF, Stadler R, Bingisser R, Breil D, Hafner M et al (2018) Screening and detection of delirium in older ED patients: performance of the modified confusion assessment method for the emergency department (mCAM-ED). A two-step tool. Intern Emerg Med 13(6):915–922. https://doi.org/10.1007/s11739-017-1781-y
Lewis LM, Miller DK, Morley JE, Nork MJ, Lasater LC (1995) Unrecognized delirium in ED geriatric patients. Am J Emerg Med 13(2):142–145. https://doi.org/10.1016/0735-6757(95)90080-2
Nihtilä EK, Martikainen PT, Koskinen SV, Reunanen AR, Noro AM, Häkkinen UT (2008) Chronic conditions and the risk of long-term institutionalization among older people. Eur J Public Health 18(1):77–84. https://doi.org/10.1093/eurpub/ckm025
Steventon ADS, Friebel R, Gardner T, Thorlby R (2018) Briefing: Emergency hospital admissions in England: which may be avoidable and how?. https://reader.health.org.uk/emergency-admissions. Accessed 26 Aug 2022.
Mudge AM, McRae P, Hubbard RE, Peel NM, Lim WK, Barnett AG et al (2019) Hospital-associated complications of older people: a proposed multicomponent outcome for acute care. J Am Geriatr Soc 67(2):352–356. https://doi.org/10.1111/jgs.15662
van den Broek S, Heiwegen N, Verhofstad M, Akkermans R, van Westerop L, Schoon Y et al (2020) Preventable emergency admissions of older adults: an observational mixed-method study of rates, associative factors and underlying causes in two Dutch hospitals. BMJ Open 10(11):e040431. https://doi.org/10.1136/bmjopen-2020-040431
Misch F, Messmer AS, Nickel CH, Gujan M, Graber A, Blume K et al (2014) Impact of observation on disposition of elderly patients presenting to emergency departments with non-specific complaints. PLoS ONE 9(5):e98097. https://doi.org/10.1371/journal.pone.0098097
Mueller OS, Rentsch KM, Nickel CH, Bingisser R (2021) Disposition decision support by laboratory based outcome prediction. J Clin Med. https://doi.org/10.3390/jcm10050939
Capan M, Pigeon J, Marco D, Powell J, Groner K (2018) We all make choices: a decision analysis framework for disposition decision in the ED. Am J Emerg Med 36(3):450–454. https://doi.org/10.1016/j.ajem.2017.11.018
Gerber LM, Ni Q, Härtl R, Ghajar J (2009) Impact of falls on early mortality from severe traumatic brain injury. J Trauma Manag Outcomes 3:9. https://doi.org/10.1186/1752-2897-3-9
Blomaard LC, Mooijaart SP, van Meer LJ, Leander J, Lucke JA, de Gelder J et al (2021) Geriatric screening, fall characteristics and 3- and 12 months adverse outcomes in older patients visiting the emergency department with a fall. Scand J Trauma Resusc Emerg Med 29(1):43. https://doi.org/10.1186/s13049-021-00859-5
Nemec M, Koller MT, Nickel CH, Maile S, Winterhalder C, Karrer C et al (2010) Patients presenting to the emergency department with non-specific complaints: the Basel Non-specific Complaints (BANC) study. Acad Emerg Med 17(3):284–292. https://doi.org/10.1111/j.1553-2712.2009.00658.x
Katz S, Downs TD, Cash HR, Grotz RC (1970) Progress in development of the index of ADL. Gerontologist 10(1):20–30. https://doi.org/10.1093/geront/10.1_part_1.20
Caruhel P, Mazier C, Kunde J, Morgenthaler NG, Darbouret B (2009) Homogeneous time-resolved fluoroimmunoassay for the measurement of midregional proadrenomedullin in plasma on the fully automated system B.R.A.H.M.S KRYPTOR. Clin Biochem 42(7–8):725–728. https://doi.org/10.1016/j.clinbiochem.2009.01.002
Nickel CH, Ruedinger J, Misch F, Blume K, Maile S, Schulte J et al (2011) Copeptin and peroxiredoxin-4 independently predict mortality in patients with nonspecific complaints presenting to the emergency department. Acad Emerg Med 18(8):851–859. https://doi.org/10.1111/j.1553-2712.2011.01126.x
Douma RA, le Gal G, Söhne M, Righini M, Kamphuisen PW, Perrier A et al (2010) Potential of an age adjusted D-dimer cut-off value to improve the exclusion of pulmonary embolism in older patients: a retrospective analysis of three large cohorts. BMJ 340:c1475. https://doi.org/10.1136/bmj.c1475
Nickel CH, Messmer AS, Geigy N, Misch F, Mueller B, Dusemund F et al (2013) Stress markers predict mortality in patients with nonspecific complaints presenting to the emergency department and may be a useful risk stratification tool to support disposition planning. Acad Emerg Med 20(7):670–679. https://doi.org/10.1111/acem.12172
Nickel CH, Messmer AS, Ghanim L, Ilsemann-Karakoumis J, Giersdorf S, Hertel S et al (2016) Adrenomedullin for risk stratification of emergency patients with nonspecific complaints: an interventional multicenter pilot study. Medicine (Baltimore) 95(1):e2395. https://doi.org/10.1097/MD.0000000000002395
Rohacek M, Nickel CH, Dietrich M, Bingisser R (2015) Clinical intuition ratings are associated with morbidity and hospitalisation. Int J Clin Pract 69(6):710–717. https://doi.org/10.1111/ijcp.12606
Marill KA, Chang Y, Wong KF, Friedman AB (2017) Estimating negative likelihood ratio confidence when test sensitivity is 100%: a bootstrapping approach. Stat Methods Med Res 26(4):1936–1948. https://doi.org/10.1177/0962280215592907
Lyngholm LE, Nickel CH, Kellett J, Chang S, Cooksley T, Brabrand M (2019) A negative D-dimer identifies patients at low risk of death within 30 days: a prospective observational emergency department cohort study. QJM 112(9):675–680. https://doi.org/10.1093/qjmed/hcz140
Nickel CH, Bingisser R, Morgenthaler NG (2012) The role of copeptin as a diagnostic and prognostic biomarker for risk stratification in the emergency department. BMC Med 10:7. https://doi.org/10.1186/1741-7015-10-7
Nickel CH, Kellett J, Cooksley T, Lyngholm LE, Chang S, Imfeld S et al (2021) The diagnoses and outcomes of emergency patients with an elevated d-dimer over the next 90 days. Am J Med 134(2):260–6.e2. https://doi.org/10.1016/j.amjmed.2020.06.009
Lyngholm L, Nickel CH, Kellett J, Chang S, Cooksley T, Brabrand M (2020) Normal gait, albumin and d-dimer levels identify low risk emergency department patients: a prospective observational cohort study with 365-day 100% follow-up. QJM 113(2):86–92. https://doi.org/10.1093/qjmed/hcz226
Nickel CH, Kuster T, Keil C, Messmer AS, Geigy N, Bingisser R (2016) Risk stratification using D-dimers in patients presenting to the emergency department with nonspecific complaints. Eur J Intern Med 31:20–24. https://doi.org/10.1016/j.ejim.2016.03.006
Christ-Crain M, Fenske W (2016) Copeptin in the diagnosis of vasopressin-dependent disorders of fluid homeostasis. Nat Rev Endocrinol 12(3):168–176. https://doi.org/10.1038/nrendo.2015.224
Mueller C, Möckel M, Giannitsis E, Huber K, Mair J, Plebani M et al (2018) Use of copeptin for rapid rule-out of acute myocardial infarction. Eur Heart J Acute Cardiovasc Care 7(6):570–576. https://doi.org/10.1177/2048872617710791
Schuetz P, Litke A, Albrich WC, Mueller B (2013) Blood biomarkers for personalized treatment and patient management decisions in community-acquired pneumonia. Curr Opin Infect Dis 26(2):159–167. https://doi.org/10.1097/QCO.0b013e32835d0bec
Christ-Crain M, Morgenthaler NG, Struck J, Harbarth S, Bergmann A, Müller B (2005) Mid-regional pro-adrenomedullin as a prognostic marker in sepsis: an observational study. Crit Care 9(6):R816–R824. https://doi.org/10.1186/cc3885
Maisel A, Mueller C, Nowak RM, Peacock WF, Ponikowski P, Mockel M et al (2011) Midregion prohormone adrenomedullin and prognosis in patients presenting with acute dyspnea: results from the BACH (Biomarkers in Acute Heart Failure) trial. J Am Coll Cardiol 58(10):1057–1067. https://doi.org/10.1016/j.jacc.2011.06.006
Stolz D, Christ-Crain M, Morgenthaler NG, Miedinger D, Leuppi J, Müller C et al (2008) Plasma pro-adrenomedullin but not plasma pro-endothelin predicts survival in exacerbations of COPD. Chest 134(2):263–272. https://doi.org/10.1378/chest.08-0047
Gonzalez Del Castillo J, Clemente-Callejo C, Llopis F, Irimia A, Oltra-Hostalet F, Rechner C et al (2021) Midregional proadrenomedullin safely reduces hospitalization in a low severity cohort with infections in the ED: a randomized controlled multi-centre interventional pilot study. Eur J Intern Med 88:104–113. https://doi.org/10.1016/j.ejim.2021.03.041
Livingston DH, Tripp T, Biggs C, Lavery RF (2009) A fate worse than death? Long-term outcome of trauma patients admitted to the surgical intensive care unit. J Trauma 67(2):341–348. https://doi.org/10.1097/TA.0b013e3181a5cc34
Acknowledgements
We would like to thank Ms. Alexandra Malinovska for her many contributions to the study. We would like to thank Ms. Jeannette-Marie Busch and Mr. Henk Riedel for their valuable discussions and helpful suggestions for the manuscript. We thank Dr. Nicolas Geigy for supervising the study at the Bruderholz Cantonal Hospital. We thank the clinical and laboratory staff for their technical assistance and all participants for their contribution to the study.
Funding
Open access funding provided by University of Basel. This study was supported by the Scientific Funds of the Emergency Department of the University Hospital Basel. The funding agency had no bearing on the study design, data collection and analysis, or writing of the manuscript.
Author information
Authors and Affiliations
Contributions
R. Bingisser acquired funding for the study. R. Bingisser and C.H. Nickel conceived the study. L. Arntz, L. Picking-Pitasch, J. Zuppinger, K. Delport Lehnen, and L. Hafner collected data. R. Bingisser, R Somasundaran, Joerg Leuppi, and K. Delport Lehnen supervised the conduct of the trial and data collection. L. Terhalle analyzed the data. L. Terhalle, I. Arnold, R. Bingisser, and C.H. Nickel interpreted the data. L. Terhalle, F. Hoffmann, I. Arnold, C.H. Nickel, and R. Bingisser wrote and revised the manuscript. All authors reviewed the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no conflicts of interest to disclose.
Ethical approval, Human and animal rights
This study was approved by the local ethics committee (identifier 2014-184, ww.eknz.ch) and conducted according to the principles of the Declaration of Helsinki.
Informed consent
Patients, aged 65 years and older, who presented to the ED within 24 h after a fall and provided informed consent, were enrolled in the study
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Terhalle, L., Arntz, L., Hoffmann, F. et al. Nonspecific stress biomarkers for mortality prediction in older emergency department patients presenting with falls: a prospective multicenter observational study. Intern Emerg Med (2024). https://doi.org/10.1007/s11739-024-03693-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11739-024-03693-6