Abstract
Pain is a multidimensional experience, potentially rendering unidimensional pain scales inappropriate for assessment. Prior research highlighted their inadequacy as reliable indicators of analgesic requirement. This systematic review aimed to compare multidimensional with unidimensional pain scales in assessing analgesic requirements in the emergency department (ED). Embase, Medline, CINAHL, and PubMed Central were searched to identify ED studies utilizing both unidimensional and multidimensional pain scales. Primary outcome was desire for analgesia. Secondary outcomes were amount of administered analgesia and patient satisfaction. Two independent reviewers screened, assessed quality, and extracted data of eligible studies. We assessed risk of bias with the ROBINS-I tool and provide a descriptive summary. Out of 845 publications, none met primary outcome criteria. Three studies analyzed secondary outcomes. One study compared the multidimensional Defense and Veterans Pain Rating Scale (DVPRS) to the unidimensional Numerical Rating Scale (NRS) for opioid administration. DVPRS identified more patients with moderate instead of severe pain compared to the NRS. Therefore, the DVPRS might lead to a potential reduction in opioid administration for individuals who do not require it. Two studies assessing patient satisfaction favored the short forms (SF) of the Brief Pain Inventory (BPI) and McGill Pain Questionnaire (MPQ) over the Visual Analogue Scale (VAS) and the NRS. Limited heterogenous literature suggests that in the ED, a multidimensional pain scale (DVPRS), may better discriminate moderate and severe pain compared to a unidimensional pain scale (NRS). This potentially impacts analgesia, particularly when analgesic interventions rely on pain scores. Patients might prefer multidimensional pain scales (BPI-SF, MPQ-SF) over NRS or VAS for assessing their pain experience.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pain is defined as an unpleasant sensory and emotional experience [1]. Up to 78% of patients present to the emergency department (ED) with a pain-related chief compliant [2]. Oligoanalgesia remains an ongoing issue in the acute care setting [3]. Several factors lead to inappropriate analgesia administration and consequently to under-treated pain and patient dissatisfaction [4]. The successful management of pain in the ED is fundamental to avoid long-term consequences of under-treated acute pain such as chronic pain, delayed recovery or readmission, poorer quality of life, impaired sleep, and impaired physical function [5, 6]. On the other hand, overtreatment of pain, e.g., with opioids, has become a significant global public health crisis in recent years. Opioid-related morbidity and mortality has led to significant social and economic impact [7, 8].
An accurate assessment of patients’ pain allows an appropriate treatment of pain [9]. In daily routine, numerical or descriptive unidimensional scales such as the visual analogue scale (VAS), the numeric rating scale (NRS), or the verbal rating scale (VRS) are predominantly used. Because of their quick, immediate and easy applicability, these scales have become popular tools to quantify pain intensity and pain relief [10]. These scales, however, consider only intensity as the sole characteristic. Consequently, the question arises as to how these scales can direct appropriate administration of analgesia [11,12,13]. Limitations of pain scales have been articulated previously. For instance, it was shown that their performance regarding prediction of desire for analgesia is poor [14, 15]. Furthermore, it was observed that pain scores might be determined rather by the emotional dimension of pain than the sensorial one [16].
It has been suggested that multidimensional pain scales address the complexity of pain sensation more adequately by including intensity, location, affective and sensory qualities [17]. They are mainly used in the context of chronic pain [18,19,20]. For the ED setting, there is scarce information on their use to direct analgesia [14, 21]. Because of these potential advantages compared to unidimensional pain scales, we hypothesized that multidimensional pain scales might more effectively distinguish between patients requiring analgesia and those not. This might potentially help to counteract the imbalance between oligoanalgesia and overtreatment. Therefore, the question arises if multidimensional pain scales are a more appropriate tool for assessment of analgesia in the ED. Thus, the aim of this review was to compare multidimensional with unidimensional pain scales in assessing the patient’s analgesic requirement (defined as desire for pain medication, amount of administered analgesia, or patient satisfaction) in the ED.
Methods
The review protocol was registered on the international Prospective Register of Systematic Reviews (PROSPERO; CRD42022301926). The systematic review was conducted and reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statements [22].
Eligibility criteria
Studies that included ED patients ≥ 18 years with any painful condition, of which pain assessment was performed with at least one unidimensional pain scale (VAS, NRS, VRS, or faces pain scale/FPS), and at least one multidimensional pain scale were eligible. Studies analyzing the desire of patients for analgesia, the amount of administered analgesia, or patient satisfaction according to the pain management scales were included. Non-original articles (i.e., editorials, letters and reviews), meta-analyses, case-reports, conference abstracts, and trial registry entries were excluded.
Search strategy
Embase (embase.com), MEDLINE (Ovid), the cumulative index to nursing and allied health literature (CINAHL, EBSCOhost) and PubMed Central (US National Library of Medicine) were searched from inception to 22th November 2021. The search strings were composed by an information specialist (C.A.-H.) and peer-reviewed by a second information specialist (Hannah Ewald; see SearchStrategies as supplemental material). The bibliographic database search used database-specific subject headings and text word synonyms for ED, multidimensional, and unidimensional pain scales for studies on adult patients. In CINAHL and PubMed Central, names of pain scales were searched in full text. No limits, language or publication date restrictions were applied. To complement the database searches, both the cited and the citing literature of included articles were extracted from lens.org, Scopus, and the Web of Science and screened for eligibility.
Outcome measures
Desire for analgesia was defined as the primary outcome. Amount of administered analgesia, and/or patient satisfaction were the secondary outcomes. A narrative synthesis of the data was adopted to meet the review aims. The narrative synthesis of the findings from the included studies considered the type of intervention (pain scales used), target population characteristics, and type of outcome. Additional outcomes of interest were reported during the data extraction process.
Data collection process
Duplicate records were removed before screening using EndNote 20 and the Bramer method [23]. Two authors (E.C. and B.M.) independently screened the titles and abstracts of all search results. Full texts of selected records were retrieved and independently reviewed for eligibility by the same authors. The same screening method was applied to records identified from backward and forward citation tracking. Discrepancies were resolved by discussion between the reviewing authors. The following data were extracted from included full texts and entered into a standardized Microsoft Excel (Microsoft Corporation, 2016) form: authors and year of publication, country of study, study design, study population, triage category, chief complaint at admission, unidimensional scale(s) with score, multidimensional scale(s) with score, desire of analgesia/pain medication, amount of administered analgesia, and patient satisfaction. The same authors independently extracted data and resolved discrepancies by discussion.
Quality assessment
We used the Cochrane ROBINS-I tool (Risk Of Bias In Non-randomized Studies of Interventions) to assess risk of bias of observational studies [24]. ROBINS-I assessed baseline and time-varying confounding, co-interventions, selection bias, classification bias, missing data, and bias in outcome measurement. Two authors (E.C. and B.M.) independently assessed the risk of bias of the included studies. Discrepancies were resolved by consensus. Results were reported through graphical representation of bias for each outcome [25].
Results
Study selection
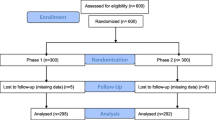
The database search returned 651 records of which 142 duplicates were removed. 509 records were analyzed through title and abstract screening and 495 records were excluded, with a total of 14 records remaining for full text screening [26,27,28,29,30,31,32,33,34,35,36,37,38]. Additional 336 papers were retrieved by citation tracking, of which 11 full-text records were assessed [9, 29, 39,40,41,42,43,44,45,46,47]. None of the studies met the criteria for the primary outcome. Three studies were included for analysis of the secondary outcomes [28, 30, 34] (Fig. 1).
Study characteristics
Given the heterogeneity of study methods and outcome measures, statistical comparisons and syntheses between included studies were not possible. None of the studies analyzed desire for analgesia (primary outcome). One study analyzed the amount of administered analgesia in the context of opioid administration and prescription [30]. Two studies referred to patient satisfaction expressed as pain scale preference [28, 34]. The main characteristics of the included studies are summarized in Table 1. All studies were monocentric and prospective. VAS [34] or NRS [28, 34] were used as unidimensional pain scale, whereas the short form (SF) of the Brief Pain Inventory (BPI) [28, 34] or the McGill Pain Questionnaire (MPQ) [34], and the Defense and Veterans Pain Rating Scale (DVPRS) [30] were used as multidimensional pain scale. None of the studies compared the same pain scales (VAS vs BPI-SF and MPQ-SF [34], NRS vs BPI-SF [28], NRS vs DVPRS [30]). All outcomes are reported in Table 2.
Amount of analgesia
One study analyzed the use of NRS and DVPRS, comparing sociodemographic and treatment data in patients revisiting the ED within 30 days of an index visit [30]. Of the 389 patients enrolled, 259 (67%) of patients returned because of pain, 129 (51%) for acute pain, and 48 (18%) for chronic pain. In the group of patients returning to the ED for pain, 119 (46%) reported use of opioid medications at home. The results of the two scales were positively correlated, but the DVPRS was better than the NRS at differentiating between moderate and severe of pain, leading to an 8% reduction in the scores for severe pain. For both scales, there was a positive correlation observed between pain scores and the proportion of patients who received opioid treatment in the ED, as well as those who were prescribed opioids upon discharge. However, the authors concluded that the use of the DPVRS could potentially reduce opioid administrations and prescriptions, because of the better discrimination between moderate and severe pain.
Patient satisfaction
Two studies showed a preference of patients for the BPI-SF (50–73%) in comparison with the VAS, NRS, or the MPQ-SF [28, 34]. Furthermore, associations between race and BPI-SF preference (black patients 96% vs white patients 69%) and between type of pain and BPI-SF preference were shown, with musculoskeletal pain being associated with the highest preference for the BPI-SF. We surmise that the study of Martinez et al. [34] is lacking information on the use of the SF of the scales used (MPQ and BPI), because due to the reported time required to administer the pain scale, only the use of the SF would have been possible.
Additional outcomes of interest
The two studies analyzing patients’ preference both used the BPI-SF [28, 34]. Time required to administer the pain scale was similar (3 min vs 3 min and 47 s ± 1 min and 35 s). In the study by Martinez et al. [34] that considered also other settings than the ED, none of the patients in the rheumatologic clinic as well as none of the caregivers in the orthopedic ward preferred the VAS. In the orthopedic ward, all caregivers preferred the BPI-SF.
Quality assessment
The two studies analyzing patients’ preference [28, 34] presented serious risk of bias, because of lacking information concerning outcome assessment, i.e., lacking a description of how preference was determined. The study of Sheikh et al. showed moderate risk of bias including only patients revisiting the ED [30]. Risk of Bias analysis is summarized in Fig. 2.
Discussion
This systematic review compared multidimensional with unidimensional pain scales to assess patients’ analgesic requirement in the ED. No study was found for the primary outcome, i.e., desire for analgesia. Three studies met the inclusion criteria for secondary outcomes. In one of the three included studies, a multidimensional pain scale (DVPRS) identified more patients with moderate instead of severe pain compared to a unidimensional pain scale (NRS). The authors speculated that, if analgesia was based on the score of the pain scale (as commonly specified in pain management protocols), use of DVPRS could potentially reduce opioid treatment and prescriptions [30]. In the other two studies, patients preferred multidimensional (BPI-SF, MPQ-SF) compared to unidimensional (NRS) pain scales to assess their pain experience [28, 34].
Even though the development and use of multidimensional tools to improve pain control in the acute setting was previously mentioned [11], the corresponding literature was found to be scarce. This highlights the limited use of multidimensional pain scales in the ED as well as the poor consideration of a pragmatic outcome such as patient’s analgesic requirement. Despite considering other outcomes, no other studies compared the use of multidimensional with unidimensional pain scales in the ED.
The question arises as to whether a pain scale should be used at all. For example, in daily practice, ED clinicians will frequently prescribe analgesia based on reaching a certain score on a pain scale or their own judgment of adequacy, rather than until the patient states to feel comfortable [48, 49]. This approach may stem from a reluctance to acknowledge patient-reported scores in pain assessment, as ED staff often believe they can determine the correct pain score [13]. However, even if a correct pain score exists, staff and patients differ in their estimates [50]. Nevertheless, despite the absence of an ideal pain tool for ED patients, the lack of pain assessment has been identified as one of the most problematic barriers to achieve optimal pain control [51].
The rare use of multidimensional pain scales in the ED might be explained by the length of questionnaires. However, short forms have been developed that take an average of 3–4 min to be performed. It is unknown whether this is reasonable for an ED population. The BPI-SF, for example, has been tested in one ED for certain facets of feasibility [28]. Two parameters were investigated: the time needed to complete the questionnaire, and the patient’s preference for BPI-SF versus NRS. The authors found that the mean time to complete the form was less than 4 min and that 73% of patients preferred BPI-SF over NRS. In addition, the severity of pain as assessed on the two scales was found to correspond with each other. As a result, the authors concluded that BPI-SF could be used instead of NRS to provide a more comprehensive measurement of pain. However, neither the usefulness nor the impact of BPI-SF on pain management were investigated. The BPI-SF has been used otherwise in various acute pain conditions, such as acute low back pain [52] and post-operative pain [53]. It considers two dimensions of pain: severity and its impact on daily functions. Thus, by measuring the interference of pain with the patient’s ability to perform daily tasks, BPI-SF provides a more objective measure than subjective pain ratings alone. Therefore, the use of BPI-SF could potentially lead to an improvement in the evaluation of pain. However, pain interference is typically assessed weeks after the onset of symptoms [52, 53], so that its significance during the initial hours remains unknown. In addition, it appears that pain severity initially correlates with pain interference [28], raising questions about the added value of assessing interference. An intriguing alternative perspective would be to target analgesia based on interference rather than intensity. For instance, in acute musculoskeletal pain in which restoring functionality might be the primary goal, scales evaluating daily function may be more suitable than those that focus solely on pain relief. In fact, patients with musculoskeletal pain in this review had the highest proportion preferring the BPI-SF as compared to patients with chest pain or abdominal pain [28]. The question arises as to whether a specific pain scale should be used for a particular pain condition. Numerous multidimensional pain scales have been developed within this purpose. For example, organ-related pain scales such as the Ocular Pain Assessment Survey (OPAS) [54], the Neck Pain and Disability Scale [55], or the ROwan Foot Pain Assessment Questionnaire (ROFPAQ) [56]. Other examples are disease-related pain scales, such as the Sickle Cell Disease Pain Burden Interview-Youth (SCPBI-Y) [57], or the Rheumatoid Arthritis Pain Scale (RAPS) [58]. However, all these scales were developed for longer-term outcomes, and not for the ED setting. For instance, in one study, the subscale examining pain interference (in vocational, social, and family functioning) of the multidimensional pain inventory (MPI), a multidimensional pain scale, identified patients developing persistent oro-facial pain who experienced unfavorable outcomes (pain-related disability measured with the Graded Chronic Pain Scale) [59]. The authors concluded that MPI might have a potential clinical relevance by helping to identify such individuals. However, even if such scales could aid in managing the follow-up of ED patients, they would not assist in immediately identifying patients in need of analgesia. It is of paramount importance to detect pain in ED patients and, accordingly, to provide an adequate amount of analgesia. Therefore, the ideal pain scale should not only identify patients in pain, but also those who require analgesia. Future research might prioritize the development of a new, possibly multidimensional pain scale for the ED setting by defining the “need for analgesia” as a measurable outcome. In addition, “adequacy of analgesia” should be defined as well, such as when a patient experiences pain relief, e.g., feels comfortable.
Limitations
The comparison among the three studies is limited by their heterogeneity in endpoints, pain scales and enrolled patient cohorts. In addition, none of the studies compared unidimensional with multidimensional pain scale in a randomized design. This might have answered the hypothesis that multidimensional pain scales could more effectively distinguish between patients requiring analgesia and those not. The study of Sheikh et al. considering administration and prescription of analgesia with NRS and DVPRS used both scales alongside. Accordingly, it was not possible to directly compare administration and prescription of analgesia based on the pain scale used. In addition, they only included patients revisiting the ED leading possibly to selection bias. The two studies assessing patients’ preference had a high risk of bias. Finally, they did not specify which kind of pain experienced these patients. In addition, we assumed that patients’ preference for a pain scale would match patient satisfaction, which might not be the same. The study of Martinez et al. was limited by its small and male-biased sample size, which may have compromised its validity. The study of Im et al. was biased towards female participants. Finally, we have emphasized that pain assessment is the cornerstone of pain management. However, it is important to acknowledge that there might be other aspects to consider, such as the pure description of the pain experience itself, independent of pain management.
Conclusions
In the ED setting, a multidimensional pain scale (DVPRS) might be able to discriminate between patients with moderate and severe pain more effectively when compared to a unidimensional pain scale (NRS). This suggests that the use of multidimensional pain scales may have implications in pain management, especially for patients potentially misclassified with severe pain by unidimensional pain scales. Based on the little heterogenous available data, patients have shown a preference for multidimensional pain scales such as BPI-SF, and MPQ-SF compared to NRS or VAS for assessing their pain experience.
References
Raja SN, Carr DB, Cohen M, Finnerup NB, Flor H, Gibson S, Keefe FJ, Mogil JS, Ringkamp M, Sluka KA, Song XJ, Stevens B, Sullivan MD, Tutelman PR, Ushida T, Vader K (2020) The revised international association for the study of pain definition of pain: concepts, challenges, and compromises. Pain 161(9):1976–1982. https://doi.org/10.1097/j.pain.0000000000001939
Tanabe P, Buschmann M (1999) A prospective study of ED pain management practices and the patient’s perspective. J Emerg Nurs 25 (3):171–177. https://doi.org/10.1016/S0099-1767(99)70200-X
Decosterd I, Hugli O, Tamchès E, Blanc C, Mouhsine E, Givel JC, Yersin B, Buclin T (2007) Oligoanalgesia in the emergency department: short-term beneficial effects of an education program on acute pain. Ann Emerg Med 50(4):462–471. https://doi.org/10.1016/j.annemergmed.2007.01.019
Rupp T, Delaney KA (2004) Inadequate analgesia in emergency medicine. Ann Emerg Med 43(4):494–503. https://doi.org/10.1016/j.annemergmed.2003.11.019
Sinatra R (2010) Causes and consequences of inadequate management of acute pain. Pain Med 11(12):1859–1871. https://doi.org/10.1111/j.1526-4637.2010.00983.x
Lovrincevic M, Kotob F, Santarosa J (2005) Pain management in the trauma setting. Seminars Anesthesia Perioper Med Pain 24(1):34–40. https://doi.org/10.1053/j.sane.2004.11.002
Bohnert ASB, Ilgen MA (2019) Understanding Links among opioid use, overdose, and suicide. Engl J Med 380(1):71–79
Weiner SG, Baker O, Bernson D, Schuur JD One-year mortality of patients after emergency department treatment for nonfatal opioid overdose. (1097–6760 (Electronic))
Bhakta HC, Marco CA (2014) Pain management: Association with patient satisfaction among emergency department patients. J Emerg Med 46(4):456–464. https://doi.org/10.1016/j.jemermed.2013.04.018
Ho K, Spence J, Murphy MF (1996) Review of pain-measurement tools. Ann Emerg Med 27(4):427–432. https://doi.org/10.1016/S0196-0644(96)70223-8
Ducharme J (2005) The future of pain management in emergency medicine. Emerg Med Clin North Am 23(2):467–475. https://doi.org/10.1016/j.emc.2004.12.011
Gordon DB (2015) Acute pain assessment tools: let us move beyond simple pain ratings. Curr Opinion Anesthesiol. https://doi.org/10.1097/ACO.0000000000000225
Sampson FC, Goodacre SW, O’Cathain A (2019) The reality of pain scoring in the emergency department: findings from a multiple case study design. Ann Emerg Med 74(4):538–548. https://doi.org/10.1016/j.annemergmed.2019.02.018
Blumstein HA, Moore D (2003) Visual analog pain scores do not define desire for analgesia in patients with acute pain. Acad Emerg Med 10(3):211–214. https://doi.org/10.1197/aemj.10.3.211
Schweizer L, Sieber R, Nickel CH, Minotti B (2022) Ability of pain scoring scales to differentiate between patients desiring analgesia and those who do not in the emergency department. Am J Emerg Med 57:107–113
Crawford Clark W, Yang JC, Tsui SL, Ng KF, Bennett Clark S (2002) Unidimensional pain rating scales: a multidimensional affect and pain survey (MAPS) analysis of what they really measure. Pain 98(3):241–247. https://doi.org/10.1016/S0304-3959(01)00474-2
Wagemakers SH, Van Der Velden JM, Gerlich AS, Hindriks-Keegstra AW, van Dijk J, Verhoeff J (2019) A systematic review of devices and techniques that objectively measure patients’ pain. Pain Phys 22(1):1
Vellucci R (2012) Heterogeneity of chronic pain. Clin Drug Investig 32(SUPPL. 1):3–10. https://doi.org/10.2165/11630030-000000000-00000
Turk DC, Rudy TE (1987) Towards a comprehensive assessment of chronic pain patients. Behav Res Ther 25(4):237–249. https://doi.org/10.1016/0005-7967(87)90002-7
Stroud MW, Thorn BE, Jensen MP, Boothby JL (2000) The relation between pain beliefs, negative thoughts, and psychosocial functioning in chronic pain patients. Pain 84(2–3):347–352. https://doi.org/10.1016/S0304-3959(99)00226-2
Scher C, Petti E, Meador L, Van Cleave JH, Liang E, Reid MC (2020) Multidimensional pain assessment tools for ambulatory and inpatient nursing practice. Pain Manag Nurs 21(5):416–422. https://doi.org/10.1016/j.pmn.2020.03.007
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. The BMJ. https://doi.org/10.1136/bmj.n71
Bramer WM, Giustini D, De Jong GB, Holland L, Bekhuis T (2016) De-duplication of database search results for systematic reviews in endnote. J Med Libr Assoc 104(3):240–243. https://doi.org/10.3163/1536-5050.104.3.014
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, Henry D, Altman DG, Ansari MT, Boutron I, Carpenter JR, Chan AW, Churchill R, Deeks JJ, Hróbjartsson A, Kirkham J, Jüni P, Loke YK, Pigott TD, Ramsay CR, Regidor D, Rothstein HR, Sandhu L, Santaguida PL, Schünemann HJ, Shea B, Shrier I, Tugwell P, Turner L, Valentine JC, Waddington H, Waters E, Wells GA, Whiting PF, Higgins JP (2016) ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ (Online) 355:4–10. https://doi.org/10.1136/bmj.i4919
McGuinness LA, Higgins JPT (2021) Risk-of-bias VISualization (robvis): an R package and Shiny web app for visualizing risk-of-bias assessments. Res Synthesis Methods 12(1):55–61. https://doi.org/10.1002/jrsm.1411
Stanik-Hutt JA, Soeken KL, Belcher AE, Fontaine DK, Gift AG (2001) Pain experiences of traumatically injured patients in a critical care setting. Am J Crit Care 10(4):252–259. https://doi.org/10.4037/ajcc2001.10.4.252
Geçiren T, Hastaların A, Düzeyi M (2007) Travma Geçiren Hastaların Ağrı Yönetimine İlişkin Memnuniyet Düzeyi. Turkiye Klinikleri J Med Sci 27(5):687–694
Im DD, Jambaulikar GD, Kikut A, Gale J, Weiner SG (2020) Brief pain inventory-short form: a new method for assessing pain in the emergency department. Pain Mede (United States) 21(12):3263–3269. https://doi.org/10.1093/PM/PNAA269
Yakupov EZ, Troshina YV, Kashapova AO, Nasrieva AM, Chizh RS (2020) The results of an open observational study on multimodal effects of the efficacy and safety of supplement neurouridine in patients with nonspecific low back pain (MULTINEURO-1). Zh Nevrol Psikhiatr Im S S Korsakova 120(9):53–59. https://doi.org/10.17116/jnevro202012009153
Sheikh S, Fishe J, Norse A, Henson M, James D, Sher W, Lott M, Kalynych C, Hendry P (2021) Comparing pain intensity using the numeric rating scale and defense and veterans pain rating scale in patients revisiting the emergency department. Cureus. https://doi.org/10.7759/cureus.17501
Downey LVA, Zun LS (2009) The effects of deep breathing training on pain management in the emergency department. South Med J 102(7):688–692. https://doi.org/10.1097/SMJ.0b013e3181a93fc5
Phelan C (2010) An innovative approach to targeting pain in older people in the acute care setting. Contemp Nurse 35(2):221–233
Downey LV, Zun LS (2010) Pain management in the emergency department and its relationship to patient satisfaction. J Emerg Trauma Shock 3(4):326–330. https://doi.org/10.4103/0974-2700.70749
Martinez JE, Grassi DC, Marques LG (2011) Analysis of the applicability of different pain questionnaires in three hospital settings: outpatient clinic, ward and emergency unit. Rev Bras Reumatol 51(4):299–308
Jones L, Borstov A, Fillingim R, Peak D, Kurz M, Hendry P, Rathlev N, Swor R, Domeier R, Damiron K, Pearson C, Kaushik S, Feldman J, McLean S (2016) (100) African Americans experience a greater burden of acute pain after motor vehicle collision than European Americans. J Pain 17(4):S1–S1. https://doi.org/10.1016/j.jpain.2016.01.003
Zanella S, Buccelletti F, Franceschi F, Vassiliadis A, Ramponi C, Sivolella S, Zanoni A, Lumachi F (2018) Transnasal sphenopalatine ganglion blockade for acute facial pain: A prospective randomized case-control study. Eur Rev Med Pharmacol Sci 22(1):210–216. https://doi.org/10.26355/eurrev-201801-14119
Rampakakis E, Monsanto HA, Stutz M, Psaradellis E, Mejia G, Carillo AE, Zapata-Cardenas A, Molina DC, Molina de Salazar DI, Pradilla Vesga OE, Beltran-Rodriguez C, Johnson K (2019) Pin18 burden of illness of herpes zoster in colombia: an observational study. Value Health Regional Issues 19:S43–S43. https://doi.org/10.1016/j.vhri.2019.08.249
Twining J, Padula C (2019) Pilot testing the Clinically Aligned Pain Assessment (CAPA) measure. Pain Manag Nurs 20(5):462–467. https://doi.org/10.1016/j.pmn.2019.02.005
Kremer E, Hampton Atkinson J, Ignelzi RJ (1981) Measurement of pain: patient preference does not confound pain measurement. Pain 10(2):241–248. https://doi.org/10.1016/0304-3959(81)90199-8
Jensen MP, Karoly P, Fau-Braver S, Braver S (1986) The measurement of clinical pain intensity: a comparison of six methods. Pain 27(1):117–126
Althagafi SM (2021) Hughes JA (2022) Identifying the relationship between patient-reported outcomes and treatment with opiates in the adult emergency department – A cross-sectional study. Int Emerg Nurs 62:101152–101152. https://doi.org/10.1016/j.ienj.2022.101152
Melzack R, Fau-Torgerson WS, Torgerson WS (1971) On the language of pain. Anesthesiology 34(1):50–59
Katz J, Melzack R (1999) Measurement of pain. Clin North Am 79(2):231–252
Kelly AM, Gunn BD (2008) Acute pain management in the emergency department Clinical Pain Management Second Edition. Acute Pain. https://doi.org/10.1201/b13460-20
Polomano RC, Galloway KT, Kent ML, Brandon-Edwards H, Kwon KN, Morales C, Buckenmaier CT (2016) Psychometric testing of the defense and veterans pain rating scale (DVPRS): a new pain scale for military population. Pain Medicine (United States) 17(8):1505–1519. https://doi.org/10.1093/pm/pnw105
Shafshak TS, Elnemr R (2021) The visual analogue scale versus numerical rating scale in measuring pain severity and predicting disability in low back pain. J Clin Rheumatol 27(7):282–285. https://doi.org/10.1097/RHU.0000000000001320
Göransson KE, Heilborn U, Djärv T (2016) Patients’ perspectives on the insufficiency of scales to rate their pain in the ED. Am J Emerg Med 34(11):2246–2247
Ducharme J (2018) Acute pain management in the Year 2018 — a review opioids and opiophobia improving pain care in the ED pain assessment — what is its role. J Acute Med 8(1235):53–59. https://doi.org/10.6705/j.jacme.201806
Giusti GD, Reitano B, Gili A (2018) Pain assessment in the emergency department. Correlation between pain rated by the patient and by the nurse. An observational study. Acta Biomedica 89 (6):64–70. https://doi.org/10.23750/abm.v89i4-S.7055
Marquié L, Raufaste E, Lauque D, Mariné C, Ecoiffier M, Sorum P (2003) Pain rating by patients and physicians: evidence of systematic pain miscalibration. Pain 102(3):289–296. https://doi.org/10.1016/s0304-3959(02)00402-5
Wells N, Pasero C, McCaffery M (2008) Improving the quality of care through pain assessment and management. BTI - patient safety and quality: an evidence-based handbook for nurses
Jones CMP, Day RO, Koes BW, Latimer J, Maher CG, McLachlan AJ, Billot L, Shan S, Lin CC (2023) Opioid analgesia for acute low back pain and neck pain (the OPAL trial): a randomised placebo-controlled trial. Lancet 402(10398):304–312. https://doi.org/10.1016/s0140-6736(23)00404-x
Chumbley GM, Thompson L, Swatman JE, Urch C (2019) Ketamine infusion for 96 hr after thoracotomy: Effects on acute and persistent pain. Eur J Pain 23(5):985–993. https://doi.org/10.1002/ejp.1366
Qazi Y, Hurwitz S, Khan S, Jurkunas UV, Dana R, Hamrah P (2016) Validity and reliability of a novel Ocular Pain Assessment Survey (OPAS) in quantifying and monitoring corneal and ocular surface pain. Ophthalmology 123(7):1458–1468. https://doi.org/10.1016/j.ophtha.2016.03.006
Jorritsma W, Dijkstra PU, de Vries GE, Geertzen JH, Reneman MF (2012) Detecting relevant changes and responsiveness of Neck Pain and Disability Scale and Neck Disability Index. Eur Spine J 21(12):2550–2557. https://doi.org/10.1007/s00586-012-2407-8
Rowan K (2001) The development and validation of a multi-dimensional measure of chronic foot pain: the ROwan Foot Pain Assessment Questionnaire (ROFPAQ). Foot Ankle Int 22(10):795–809. https://doi.org/10.1177/107110070102201005
Zempsky WT, O’Hara EA, Santanelli JP, Palermo TM, New T, Smith-Whitley K, Casella JF (2013) Validation of the sickle cell disease pain burden interview-youth. J Pain 14(9):975–982. https://doi.org/10.1016/j.jpain.2013.03.007
Anderson DL (2001) Development of an instrument to measure pain in rheumatoid arthritis: Rheumatoid Arthritis Pain Scale (RAPS). Arthritis Rheum 45(4):317–323. https://doi.org/10.1002/1529-0131(200108)45:4%3c317::Aid-art343%3e3.0.Co;2-x
Allison JA-O, Penlington CA-O, Durham JA-O (2021) DEEP Study: Utility of the multidimensional pain inventory in persistent oro-facial pain. J Oral Rehabilit 48(11):1210–1218
Acknowledgements
Hannah Ewald, University Medical Library, University of Basel, Basel, Switzerland for peer-reviewing the search string.
Funding
Open access funding provided by University of Basel.
Author information
Authors and Affiliations
Contributions
Conceptualization: Bruno Minotti, Christian Hans Nickel; Methodology: Bruno Minotti, Christian Appenzeller-Herzog, Christian Hans Nickel; Formal analysis and investigation: Elena Crisman, Bruno Minotti, Christian Appenzeller-Herzog; Writing original draft: Elena Crisman; Writing review and editing: all authors.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Human and animal rights
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Crisman, E., Appenzeller-Herzog, C., Tabakovic, S. et al. Multidimensional versus unidimensional pain scales for the assessment of analgesic requirement in the emergency department: a systematic review. Intern Emerg Med (2024). https://doi.org/10.1007/s11739-024-03608-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11739-024-03608-5