Abstract
Unmet needs challenge clinical management of sepsis especially concerning patient profiling, enhancing recovery, and long-term sequelae. Here, we preliminarily focused on sclerostin (SOST) as a candidate biomarker to encompass such a broad range of clinical needs related to sepsis. Seventy-three septic patients were enrolled at internal medicine wards between January 2017 and December 2019 in this pilot study. Clinical examination and blood sample analyses were collected at enrollment and after 7 and 14 days. SOST levels were assessed on serum by ELISA. Thirty-day mortality was set as primary outcome. In-hospital and long-term mortality (2.5 years of median follow-up) were assessed as secondary outcomes. Patients were frail, elderly, and heterogeneous in terms of comorbidity burden. SOST levels were associated with age, cardiovascular comorbidities, and time to early death (30 days). When regression models were built, SOST displayed a high predictive value toward 30-day mortality (OR 13.459 with 95% CI 1.226–148.017) with ever better performance than validated scoring scales for critical ill patients. Such a predictive value of SOST was further confirmed for in-hospital (HR 10.089 with 95% CI 1.375–74.013) and long-term mortality (HR 5.061 with 95% CI 1.379–18.570). SOST levels generally decreased over 7 to 14 days after enrollment (p for trend < 0.001). The degree of this variation further predicted long-term mortality (HR for Δ SOST T0–day 14: 1.006 with 95% CI 1.001–1.011). Our results suggest a role for SOST in both short- and long-time prediction of worse outcome in septic elderly admitted to internal medicine wards.
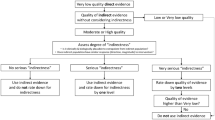
Graphical abstract

Highlights
-
Septic elderly patients are at high risk of worse outcome.
-
Sclerostin is marker of frailty and predictor of early and long-term mortality.
-
Sclerostin is associated with sepsis-related mortality in elderly.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The third international consensus definition of sepsis [1] upsets the traditional paradigm of this life-threatening condition. The shift toward dysregulated immune response as a leading determinant of organ damage has further highlighted the variability and complexity of host immune system and clinical outcome. Novel clinical phenotypes for sepsis with broad differences in clinical characteristics and organ dysfunction patterns are increasingly described [2]. They range from that with fewer, mild biochemical abnormalities, and organ dysfunction to those characterized by older age, greater comorbidity burden, and higher rate of renal impairment and shock. Inflammatory biomarkers may have a value in discriminating different phenotypes, but there are still far from a routine clinical application. However, incidence and costs of long-term sepsis-related mortality remain abysmal and constantly increasing. The mounting awareness on that claims for biomarkers of pre-existing disability and frailty [3, 4]. Sclerostin (SOST) is traditionally involved in bone metabolism and associated with frailty and mortality in elderly patients, with recent insights on cardiovascular (CV) risk and immune response [5,6,7]. Relevance of circulating SOST has been tested in septic patients admitted to intensive care units (ICU) and linked to renal/hepatic organ failure [8]. Besides an increase of 10 pmol/L in serum, SOST has been associated with 30% higher risk of CV mortality in general population [9]. In light of these pleiotropic activities on critical organs, SOST represents a candidate biomarker to encompass the trimodal pattern of sepsis-related mortality. Here, we focused on the role of SOST in a small cohort of elderly septic patients, aiming at preliminarily established its potential role in short- and long-term mortality.
Materials and methods
Patient enrollment
The monocentric observational study “Genoa-BASH SEPSIS” enrolled patients between January 2017 and December 2019 at the IRCCS Ospedale Policlinico San Martino in Genoa (Italy). Seventy-three patients were enrolled at the Internal Medicine and Infectious Disease Clinics. The overall follow-up lasted until 31st October 2021. According to the study protocol, all the enrolled patients fulfilled the sepsis-3 defining criteria, as stated by the “Third International Consensus Definition for Sepsis and Septic Shock”: i) suspected infection; ii) acute development of organ dysfunction (within 48 h from enrollment), represented by an increase in the Sequential [Sepsis-related] Organ Failure Assessment (SOFA) score ≥ 2. Quick SOFA (qSOFA) was also calculated as non-diagnostic score with high predictive value for in-hospital mortality outside of the ICU [10].
Sepsis-related exclusion criteria were the start of antibiotic therapy beyond 72 h prior to the enrollment and the inadequate source control within 96 h from the enrollment. Although not standardized, the latter is widely recognized as critical bias influencing treatment of sepsis and restoring of premorbid anatomy and function [11, 12]. Additional exclusion criteria were congestive heart failure with NYHA class III–IV, active cancer (localized, metastatic or under active treatment), hemodialytic treatment, and hepatic cirrhosis. Clinical profiling of enrolled patients included medical history and vital sign assessment. The study was conducted in accordance with the ethical standards of the responsible committee on human experimentation (Regional Ethic Committee approval number 487REG2016 of December 30th, 2016) and with the Helsinki Declaration of 1975. All patients gave informed consent before enrollment.
Laboratory assay
Blood samples were collected at the day of the enrollment, and then after 7 and 14 days. All samples were then stored at – 80 °C until analysis. Biochemical analyses were performed at central hospital laboratory with routine auto-analyzer and included blood cell count, biochemical assay, and blood gas assay. Circulating levels of SOST were measured at our research laboratory. SOST levels were measured on serum samples obtained from whole blood centrifugation. Colorimetric enzyme-linked immunosorbent assay was performed following manufacturer’s instructions (Quantikine, R&D Systems, Minneapolis, MN). The lower limit of detection for SOST was 31.3 pg/mL with mean intra- and inter-assay coefficients of variation below < 8%, as previously reported [13].
Study endpoints adjudication and power calculation
Thirty-day mortality has been set as the primary outcome of the present study. Considering the binary outcome of the present study design, our sample size (n = 73) does not satisfy the minimum sample size required for developing a clinical prediction model [14]. The results should be then considered as preliminary and deserving validation in further studies. Secondary outcomes of the study were in-hospital and overall mortality rates, also considering SOST levels rise/fall overtime. For these outcomes, patient follow-up has been managed through informatic records. The latter have been defined as for difference (Δ) of SOST levels at baseline (T0) with levels at days 7 and 14.
Statistical analyses
R, version 3.6.3 (R Foundation for Statistical Computing, Vienna, Austria); IBM SPSS Statistics, Version 23.0 (IBM CO., Armonk, NY); and GraphPad Prism 5 (GraphPad Software, Inc, La Jolla, CA) were used for statistical analysis. Categorical data were reported as absolute and relative frequencies and comparisons were drawn by Chi-square or Fisher’s exact test. When the normality assumption—tested by Shapiro–Wilk—was not demonstrated, continuous variables were presented as median and interquartile range (IQR) and intergroup comparisons were drawn by Mann–Whitney U test. Likewise, correlations coefficients were calculated by ranked Spearman’s correlation test. Friedman test was instead used for detecting differences in across multiple paired samples. For primary and secondary outcome estimation, we built univariate and adjusted logistic regression models, whose results are reported as odds ratio (OR) and 95% CI. For adjusted models, forward stepwise regression analysis was used, also to avoid overfitting in a quite small cohort. When necessary, variables included in logistic regression model were log-transformed. Model discrimination has been performed by ROC curve analysis, whereas bootstrap resampling performance was used for the internal model validation. Finally, univariate and adjusted Cox proportional hazards model (expressed as hazard ratio [HR] and 95% CI) was built to test overall survival through a forward stepwise regression analysis A two-sided p value < 0.05 was considered as statistically significant for all the statistical analyses.
Results
Cohort characteristics
Table 1 and Supplementary Tables 1 and 2 summarize clinical and biochemical features of the overall cohort (n = 73) at the enrollment and after categorization for the primary outcome.
Patients were very elderly (median age of 82 years), well balanced across sex (56.2% of men), and with relatively low comorbidity burden (median CIRS and Charlson 11 and 3, respectively). As expected, 30-day mortality was associated with a more severe sepsis as expressed by Glasgow coma scale (median 13 vs. 15; p = 0.013), quick SOFA (median 2 vs. 1; p = 0.002), APACHE II score (median 18 vs. 13; p = 0.014), and Kelly scale (median 2 vs. 1; p = 0.002). Conversely, the comorbidity burden was less relevant, as summarized by the CIRS scale (median 15 vs. 10; p = 0.042) and the Charlson comorbidity index (p = 0.548). Higher heart rate emerged as the most relevant clinical feature associated with 30-day mortality, alongside with anemia (median hemoglobin values 10.1 vs. 11.8; p = 0.022) and increased circulating levels of SOST (median 193 ng/mL vs. 132 ng/mL; p = 0.022). Concerning the latter, the most interesting association was with age (r = 0.370; p = 0.002) and cardiovascular comorbidities: diabetes, ischemic heart disease, and atrial fibrillation (Fig. 1 A and B, Table 2). Accordingly, linear correlations with CIRS scale (r = 0.425; p < 0.001) and NYHA class (r = 0.354; p = 0.005) were here reported (Fig. 1 C, Table 3). Further mention deserved the correlation between SOST and body temperature (r = – 0.278; p = 0.025) and platelet count (r = 0.249; p = 0.044).
SOST is associated with comorbidity burden and poor survival time. Sclerostin (SOST) distribution across fasting glycemia (A) and history of atrial fibrillation (B). Regarding continuous variables, SOST shows a positive significant correlation with CIRS scale (C) and time to death at 30 days (analysis limited to deceased patients) (D)
Serum SOST levels predict early death in elderly septic patients
An interesting observation was the significant inverse correlation between SOST and the time to death (r = 0.337; p = 0.005) (Fig. 1 D). Overall death incidence was 46.6% (n = 34) over a median follow-up period of 688 days (range 0 to 1061 days), whereas 30-days mortality occurred in 17 patients (Fig. 2A).
SOST is tightly correlated with early (30 days) death risk. Thirty-four patients (46.6%) deceased during follow-up. Among these, 17 deaths occurred within 30-days from enrollment and 15 during hospitalization (A). The latter accounted for 21.9% of patient discharge, whereas others were discharged at home (60.3%), in senior residences (15.1%) or admitted to ICU (4.1%) (B). Higher sclerostin (SOST) levels were associated with poor outcome (C). At logistic regression, SOST and heart rate were the only significant predictor of 30-day mortality (D)
In-hospital death represented the 21.9% of patient discharge and associated with higher baseline serum levels of SOST as compared with patients discharged at home (60.3%), in senior residences (15.1%) or admitted to intensive care unit (ICU) (4.1%) (Fig. 2 B and C). When logistic regression model was built, SOST emerged as predictor of 30-day mortality in septic patients (OR 13.459 with 95% CI 1.226 to 148.017) alongside with heart rate, comorbidity burden assessed by CIRS scale and validated scoring scales for critical ill patients: quick SOFA, APACHE II, Kelly. The forward stepwise regression approach highlighted the independent predictive value of SOST (adjOR 36.887 with 95% CI 1.535 to 886.360) and heart rate (adjOR 1.085 with 95% CI 1.028 to 1.145) (Fig. 2 D; Table S3). With a p value of 0.852, the Hosmer–Lemeshow test confirmed the good calibration of this model, whereas the result of ROC curve analysis indicated a good performance with an AUC of 0.825 (Table S5). Although not significant, the model performance was higher than other validated scoring scales for critical ill patients: quick SOFA, APACHE II, Kelly (Fig. 3 A). Internal validation with bootstrap resampling was finally performed. Based on 1000 bootstrap replicates, new estimate of the ORs was obtained (average of the 1000 ORs from the 1000 bootstrap samples). The OR estimated on the original dataset fall within the new bootstrap confidence intervals.
Predictive value of SOST toward mortality. The predictive value of sclerostin (SOST) toward 30-day mortality shows a trend of superiority as compared with toward other validated scores for clinical ill patients (A). Such a predictive value of SOST was also confirmed—alongside with Kelly scale—in the Cox regression model for the in-hospital mortality (B). SOST shows a predictive value toward long-term all-cause mortality (C) and a significant trend to lowering overtime (D)
Serum levels of SOST and secondary outcomes: a wide prediction of mortality in septic patients
The univariate and adjusted Cox proportional hazards regression models for in-hospital mortality confirmed the predictive role of SOST (adjHR 136.191 with 95% CI 6.919 to 2680.871) together with the Kelly scale (adjHR 5.422 with 95% CI 2.305 to 12.754) (Fig. 3 B and Table S4). Serum SOST was also independently associated with long-term mortality with a 15-fold increased risk (adjHR 15.282 with 95% CI 1.5842.106 to 147.463) (Fig. 3 C, Table S5). When overtime modification in circulating SOST levels was considered, a progressive fall at days 7 and 14 after enrollment was observed (Fig. 3 D). Like baseline levels, the extent to which SOST decreased at day 14 was identified as independent predictor of long-term mortality (adjHR for Δ SOST T0 – day 14: 1.009 with 95% CI 1.002 to 1.017) (Table S6).
Discussion
The major finding of this study is the demonstration of serum SOST as promising mortality predictor in elderly patients with sepsis. Death risk related to SOST levels progressively increases from 5-fold in long-term follow-up up to 10- and 13-fold for in-hospital and 30-day mortality, respectively. Nevertheless, the clinical relevance of SOST in critically ill patients is poorly investigated. A single case–control study has so far reported an association with renal, hepatic, and CV impairment, but not mortality [8]. Here, we confirmed the association with comorbidity burden as expressed by CIRS scale and—partially—Charlson comorbidity index, with special regard to CV risk factors: diabetes, ischemic heart disease, and atrial fibrillation. Predictive value of SOST also prevails on heart rate, widely used alone or within clinical scales [15]. However, we here consider one measure at enrollment, while overtime variability expresses a greater predictive power. Of further interest, the lack of correlation between SOST and qSOFA deserves to be discussed. qSOFA is traditionally described as prognostic scale with greater predictive value than SOFA for in-hospital mortality outside of the ICU [10]. Later clinical studies confirmed the suboptimal diagnostic performance of qSOFA [16,17,18], even questioning its predictive value [19, 20]. The rate of septic patients with qSOFA values < 2 was here quite higher (46.5%), but in line with recently reported elsewhere [17, 18]. Early sepsis identification in elderly still represents a demanding clinical challenge and accounts for strong efforts in implementing clinical predictive weapons [21,22,23]. This ultimately represents the rationale of the present study.
As biomarker of bone mineral density, serum levels of SOST may partially reflect the advanced age and frailty of enrolled patients, which are more prone to osteopenia/osteoporosis [24]. Similarly, SOST is implicated in CV health [25] and insulin sensitivity [13] but opposite finding on related adverse outcomes has been reported [9, 26]. Even taking into account the small sample size, there is a tendency to higher SOST levels in female. This seems partially in contrast with previous works.
[27]. We also acknowledge as a study limitation the lack of information about bone mass. Furthermore, the prognostic value of short-term variation in serum SOST may partially overcome this limitation, rather paying attention on the role of SOST as an acute-phase protein [28]. Indirect evidence indeed suggests an active role of SOST in the host immune response to infection. By targeting canonical Wnt signaling, SOST would have a relevant role in self-renewal and differentiation of hematopoietic stem cell within bone marrow niche [29]. Studies on Sost−/− recipient mice have demonstrated for SOST an inhibitory effect on proliferation and mobilization of myeloid progenitor. These suppression mechanisms would involve lymphoid cell also [30] and potentially platelet count. A positive correlation between SOST levels and platelets count was indeed observed here. Although never reported before, it can be related to the excess of acute-phase response [31]. Furthermore, only one experimental study has so far associated SOST inhibition with increased clearance of platelets and reduction of their count [32, 33].
Metabolic effects on circulating SOST is a topic of further interest. Thirty-day deceased patients showed a tendency toward higher body mass index and prevalence of diabetes. In contrast with previous literature [34, 35], we did not find any significant association between circulating SOST and dysmetabolic status. Furthermore, we have no data on any cardiovascular mortality in the study cohort. They would allow to solve this mismatch and are warranted in further studies.
Over time changes in SOST levels during sepsis and their association with outcomes—mainly time-to-event—further highlight a potential role of SOST as an acute-phase protein. Whereas any association of baseline levels might be related with a pre-existing frailty, such an acute reduction should be viewed as a feedback mechanism preventing a dysregulated host response to infection. In line, high baseline/persistently high SOST levels would sustain mortality risk through a dysregulated host response, in accordance with the third international consensus definitions for sepsis and septic shock (Sepsis-3) [1]. However, this finding needs to be further addressed as short-term changes in SOST levels have not yet been investigated. Rather, long-term changes in SOST levels have been previously reported as marker of aging, but also cardiometabolic health [28, 36, 37].
As additional finding, we set up a long-term follow-up that accomplishes the most recent view on sepsis pathophysiology. There is indeed an increasing awareness about a trimodal pattern of sepsis-related mortality that would last even 3 years after the event. Our findings extend the predictive value of baseline circulating SOST and its overtime variations over a median of 2.5 years. A so long follow-up may raise questions about an actual causal relationship, and this should be acknowledged as additional study limitation. However, the concept of long-term sepsis-related mortality is intrinsically far from any standardization. Advanced age, comorbidity burden, persistent immune dysfunction/inflammation, chronic catabolism, and discharge disposition differently tailor to each patient. Although preliminary and underpowered, SOST may rather reflect a dual role of SOST as a frailty biomarker and an active immune mediator, thus deserving future investigations. Furthermore, our study design gave the opportunity to investigate sepsis and related outcomes in a special setting of patients, poorly considered in previous studies. This field of research is indeed traditionally oriented on critical ill patient admitted to ICU, where patients are somehow selected and largely differ from those admitted in internal medicine wards in terms of median age, comorbidities, standard of care, and outcome. Even the incidence rate of sepsis admitted to internal medicine wards is quite higher (about 367 vs. 44 cases per 100,000 adult/year) [38] and patient heterogeneity is greater as well. The low number of patients enrolled in a long enrollment period may be the expression of this heterogeneity and the clinical challenge to face off. In daily practice, elderly patients admitted to internal medicine wards have a consistent comorbidity burden. When sepsis occurs, their clinical condition rapidly deteriorates and need monitoring at the emergency department. If not started at nursing home, antibiotic treatment is often urgent and empirically based. Far from a standardized approach, it is challenging to recognize an early (within 48 h) increase of SOFA score ≥ 2 in internal medicine wards. Downstream of such a complexity, identifying biomarkers reliable for clinical use is challenged by diversity in assay methods, all-cause mortality as the only outcome, and lack of pathophysiological link among the others [39]. Therefore, studies on biomarkers in sepsis generally do not answer to specific, clinically relevant questions, but rather report just diagnostic or prognostic values. We acknowledge this point as another intrinsic limitation of this unpowered study that should be then considered as pilot. Nevertheless, variations in time course and their prognostic relevance allowed us to hypothesize SOST as not innocent bystander in sepsis.
In conclusion, the present study provides preliminary evidence for a prognostic role of SOST in sepsis. Especially high baseline/persistently higher circulating levels of SOST may predict short- and long-term mortality in elderly patients with sepsis admitted in internal medicine wards. In line with the emerging needs of patients profiling, enhancing recovery from sepsis and get loaded of long-term sequelae, SOST may represent a long-lasting biomarker that is able to guide clinical decisions.
References
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M et al (2016) The Third International consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 315:801–810
Seymour CW, Kennedy JN, Wang S, Chang CH, Elliott CF, Xu Z et al (2019) Derivation, validation, and potential treatment implications of novel clinical phenotypes for sepsis. JAMA 321:2003–2017
Delano MJ, Ward PA (2016) The immune system’s role in sepsis progression, resolution, and long-term outcome. Immunol Rev 274:330–353
Barichello T, Generoso JS, Singer M, Dal-Pizzol F (2022) Biomarkers for sepsis: more than just fever and leukocytosis-a narrative review. Crit Care 26:14
Zheng J, Maerz W, Gergei I, Kleber M, Drechsler C, Wanner C et al (2019) Mendelian randomization analysis reveals a causal influence of circulating sclerostin levels on bone mineral density and fractures. J Bone Miner Res 34:1824–1836
Bovijn J, Krebs K, Chen CY, Boxall R, Censin JC, Ferreira T et al (2020) Evaluating the cardiovascular safety of sclerostin inhibition using evidence from meta-analysis of clinical trials and human genetics. Sci Transl Med. https://doi.org/10.1126/scitranslmed.aay6570
Donham C, Manilay JO (2020) The effects of sclerostin on the immune system. Curr Osteoporos Rep 18:32–37
Koch A, Weiskirchen R, Ludwig S, Buendgens L, Bruensing J, Yagmur E et al (2017) Relevance of serum sclerostin concentrations in critically ill patients. J Crit Care 37:38–44
Novo-Rodriguez C, Garcia-Fontana B, Luna-Del Castillo JD, Andujar-Vera F, Avila-Rubio V, Garcia-Fontana C et al (2018) Circulating levels of sclerostin are associated with cardiovascular mortality. PLoS ONE 13:e0199504
Seymour CW, Liu VX, Iwashyna TJ, Brunkhorst FM, Rea TD, Scherag A et al (2016) Assessment of clinical criteria for sepsis: for the third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 315:762–774
Timsit JF, Baleine J, Bernard L, Calvino-Gunther S, Darmon M, Dellamonica J et al (2020) Expert consensus-based clinical practice guidelines management of intravascular catheters in the intensive care unit. Ann Intensive Care 10:118
Lipsett PA (2022) The critical importance of timing of source control in patients with community-acquired sepsis. JAMA Surg 157:826–827
Carbone F, Nulli Migliola E, Bonaventura A, Vecchie A, De Vuono S, Ricci MA et al (2021) Circulating levels of sclerostin predict glycemic improvement after sleeve gastrectomy. Nutrients 13(2):623. https://doi.org/10.3390/nu13020623
Riley RD, Ensor J, Snell KIE, Harrell FE Jr, Martin GP, Reitsma JB et al (2020) Calculating the sample size required for developing a clinical prediction model. BMJ 368:m441
de Castilho FM, Ribeiro ALP, Nobre V, Barros G, de Sousa MR (2018) Heart rate variability as predictor of mortality in sepsis: A systematic review. PLoS ONE 13:e0203487
Umemura Y, Ogura H, Gando S, Kushimoto S, Saitoh D, Mayumi T et al (2017) Assessment of mortality by qSOFA in patients with sepsis outside ICU: A post hoc subgroup analysis by the Japanese Association for Acute Medicine Sepsis Registry Study Group. J Infect Chemother Off J Jpn Soc Chemother 23:757–762
Mignot-Evers L, Raaijmakers V, Buunk G, Brouns S, Romano L, van Herpt T et al (2021) Comparison of SIRS criteria and qSOFA score for identifying culture-positive sepsis in the emergency department: a prospective cross-sectional multicentre study. BMJ Open 11:e041024
Lee CC, Ho CY, Chen PL, Hsieh CC, Wang WYC, Lin CH et al (2021) Is qSOFA suitable for early diagnosis of sepsis among bacteremia patients in emergency departments? time for a reappraisal of Sepsis-3 criteria. Front Med 8:743822
Finkelsztein EJ, Jones DS, Ma KC, Pabon MA, Delgado T, Nakahira K et al (2017) Comparison of qSOFA and SIRS for predicting adverse outcomes of patients with suspicion of sepsis outside the intensive care unit. Crit Care 21:73
Tokioka F, Okamoto H, Yamazaki A, Itou A, Ishida T (2018) The prognostic performance of qSOFA for community-acquired pneumonia. J Intensive Care 6:46
Devia Jaramillo G, Ibanez PM (2022) Quick sequential organ failure assessment, sequential organ failure assessment, and procalcitonin for early diagnosis and prediction of death in elderly patients with suspicion of sepsis in the emergency department, based on Sepsis-3 definition. Gerontology 68:171–180
Guo Q, Li HY, Song WD, Liu H, Yu HQ, Li YH et al (2022) qSOFA predicted pneumonia mortality better than minor criteria and worse than CURB-65 with robust elements and higher convergence. Am J Emerg Med 52:1–7
Wright SW, Hantrakun V, Rudd KE, Lau CY, Lie KC, Chau NVV et al (2022) Enhanced bedside mortality prediction combining point-of-care lactate and the quick Sequential Organ Failure Assessment (qSOFA) score in patients hospitalised with suspected infection in southeast Asia: a cohort study. Lancet Glob Health 10:e1281–e1288
Lu JW, Syu RJ, Wang CH, Hsu BG, Tsai JP (2022) Serum Sclerostin level is negatively associated with bone mineral density in hemodialysis patients. Medicina (Kaunas) 58(3):385
Frysz M, Gergei I, Scharnagl H, Smith GD, Zheng J, Lawlor DA et al (2022) Circulating sclerostin levels are positively related to coronary artery disease severity and related risk factors. J Bone Miner Res 37:273–284
Kanbay M, Solak Y, Siriopol D, Aslan G, Afsar B, Yazici D et al (2016) Sclerostin, cardiovascular disease and mortality: a systematic review and meta-analysis. Int Urol Nephrol 48:2029–2042
Modder UI, Hoey KA, Amin S, McCready LK, Achenbach SJ, Riggs BL et al (2011) Relation of age, gender, and bone mass to circulating sclerostin levels in women and men. J Bone Miner Res 26:373–379
Weivoda MM, Youssef SJ, Oursler MJ (2017) Sclerostin expression and functions beyond the osteocyte. Bone 96:45–50
Yee CS, Manilay JO, Chang JC, Hum NR, Murugesh DK, Bajwa J et al (2018) Conditional deletion of sost in MSC-derived lineages identifies specific cell-type contributions to bone mass and B-cell development. J Bone Miner Res 33:1748–1759
Donham C, Chicana B, Robling AG, Mohamed A, Elizaldi S, Chi M et al (2021) Sclerostin depletion induces inflammation in the bone marrow of mice. Int J Mol Sci 22(17):9111
Schattner A, Kadi J, Dubin I (2019) Reactive thrombocytosis in acute infectious diseases: prevalence, characteristics and timing. Eur J Intern Med 63:42–45
Rudmann DG, Page TJ, Vahle JL, Chouinard L, Haile S, Poitout F et al (2012) Rat-specific decreases in platelet count caused by a humanized monoclonal antibody against sclerostin. Toxicol Sci 125:586–594
Behets GJ, Viaene L, Meijers B, Blocki F, Brandenburg VM, Verhulst A et al (2017) Circulating levels of sclerostin but not DKK1 associate with laboratory parameters of CKD-MBD. PLoS ONE 12:e0176411
Aznou A, Meijer R, van Raalte D, den Heijer M, Heijboer A, de Jongh R (2021) Serum sclerostin is negatively associated with insulin sensitivity in obese but not lean women. Endocr Connect 10:131–138
Martin Gonzalez C, Fernandez Rodriguez CM, Abreu Gonzalez P, Garcia Rodriguez A, Alvisa Negrin JC, Cabanas Perales E et al (2022) Sclerostin in excessive drinkers: relationships with liver function and body composition. Nutrients 14(13):2574
Dror N, Carbone J, Haddad F, Falk B, Klentrou P, Radom-Aizik S (2022) Sclerostin and bone turnover markers response to cycling and running at the same moderate-to-vigorous exercise intensity in healthy men. J Endocrinol Invest 45:391–397
Karampatsou SI, Paltoglou G, Genitsaridi SM, Kassari P, Charmandari E (2022) The effect of a comprehensive life-style intervention program of diet and exercise on four bone-derived proteins, FGF-23, osteopontin, NGAL and sclerostin, in overweight or obese children and adolescents. Nutrients 14(18):3772
Esteban A, Frutos-Vivar F, Ferguson ND, Penuelas O, Lorente JA, Gordo F et al (2007) Sepsis incidence and outcome: contrasting the intensive care unit with the hospital ward. Crit Care Med 35:1284–1289
Pierrakos C, Velissaris D, Bisdorff M, Marshall JC, Vincent JL (2020) Biomarkers of sepsis: time for a reappraisal. Crit Care 24:287
Funding
Open access funding provided by Università degli Studi di Genova within the CRUI-CARE Agreement. This research was funded by a grant from the Rete Cardiologica of Italian Ministry of Health (#2754291) to Prof. F. Montecucco. The research was funded by a grant from the Internal Medicine Department of the University of Genoa to Prof. Federico Carbone.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Luca Liberale is a co-inventor on the International Patent WO/2020/226993 filed in April 2020. The patent relates to the use of antibodies which specifically bind IL-1α to reduce various sequelae of ischemia–reperfusion injury to the central nervous system. Luca Liberale reports speaker fees outside of this work from Daichi-Sankyo. Aldo Bonaventura and Alessandra Vecchié received a travel grant from Kiniksa Pharmaceuticals Ltd. to attend the 2019 AHA Scientific Sessions and honoraria from Effetti s.r.l. (Milan, Italy) to collaborate on the medical website www.inflammology.org. The remaining authors have nothing to disclose related to this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tirandi, A., Arboscello, E., Ministrini, S. et al. Early sclerostin assessment in frail elderly patients with sepsis: insights on short- and long-term mortality prediction. Intern Emerg Med 18, 1509–1519 (2023). https://doi.org/10.1007/s11739-023-03223-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-023-03223-w