Abstract
During the last decade, the CHA2DS2-VASc score has been used for stratifying the mortality risk in both atrial fibrillation (AF) and non-AF patients. However, no previous study considered this score as a prognostic indicator in non-AF patients with mild-to-moderate idiopathic pulmonary fibrosis (IPF). All consecutive non-AF patients with mild-to-moderate IPF, diagnosed between January 2016 and December 2018 at our Institution, entered this study. All patients underwent physical examination, blood tests, spirometry, high-resolution computed tomography and transthoracic echocardiography. CHA2DS2-VASc score, Gender-Age-Physiology (GAP) index and Charlson Comorbidity Index (CCI) were determined in all patients. Primary endpoint was all-cause mortality, while the secondary endpoint was the composite of all-cause mortality and rehospitalizations for all causes over mid-term follow-up. 103 consecutive IPF patients (70.7 ± 7.3 yrs, 79.6% males) were retrospectively analyzed. At the basal evaluation, CHA2DS2-VASc score, GAP index and CCI were 3.7 ± 1.6, 3.6 ± 1.2 and 5.5 ± 2.3, respectively. Mean follow-up was 3.5 ± 1.3 yrs. During the follow-up period, 29 patients died and 43 were re-hospitalized (44.2% due to cardiopulmonary causes). On multivariate Cox regression analysis, CHA2DS2-VASc score (HR 2.15, 95% CI 1.59–2.91) and left ventricular ejection fraction (LVEF) (HR 0.91, 95% CI 0.86–0.97) were independently associated with all-cause mortality in IPF patients. CHA2DS2-VASc score (HR 1.66, 95% CI 1.39–1.99) and LVEF (HR 0.94, 95% CI 0.90–0.98) also predicted the secondary endpoint in the same study group. CHA2DS2-VASc score > 4 was the optimal cut-off for predicting both outcomes. At mid-term follow-up, a CHA2DS2-VASc score > 4 predicts an increased risk of all-cause mortality and rehospitalizations for all causes in non-AF patients with mild-to-moderate IPF.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Idiopathic pulmonary fibrosis (IPF) is a chronic, progressive, interstitial lung disease of unknown cause, with a median survival of about 2.5–5 years after definite diagnosis [1]. Its prevalence is increasing worldwide [2].
In addition to the adverse effects caused by pulmonary fibrosis, IPF patients have an increased risk of adverse cardiovascular manifestations, such as pulmonary hypertension, right heart failure, coronary artery disease (CAD), cardiac arrhythmias and stroke [3,4,5]. Indeed, after respiratory failure, cardiovascular disease is the second main cause of death in these patients [5].
For this reason, it is mandatory to research prognostic indicators that could independently predict the risk of death and/or cardiovascular events in IPF patients.
During the last decade, several biochemical, spirometric, radiological and echocardiographic prognostic indicators [6,7,8,9,10,11,12,13,14,15,16,17,18,19,20] have been separately investigated in IPF patients. In addition, a number of clinical scores evaluating comorbid conditions, such as the coronary artery calcification (CAC) score [21], the Gender-Age-Physiology (GAP) index [22] and the Charlson comorbidity index (CCI) [23], have been employed for predicting the risk of mortality and/or adverse clinical events in IPF patients.
Given the association between IPF and increased risk of cardiovascular and thromboembolic events [24], the CHA2DS2-VASc (Congestive heart failure or left ventricular dysfunction, Hypertension, Age ≥ 75 years, Diabetes, Stroke/TIA, Vascular disease, Age 65–74 years, and Sex category) score might improve the prognostic risk stratification of these patients. This score, developed by Lip GY et al. [25] in 2010, is actually recommended for estimating thromboembolic risk and deciding on anticoagulation therapy in atrial fibrillation (AF) patients [26, 27]. In the last few years, the incremental prognostic role of CHA2DS2-VASc score has been demonstrated in several cardiovascular [28,29,30,31,32,33] and non-cardiovascular diseases [34, 35], irrespective of AF presence.
Whether the CHA2DS2-VASc score stratifies mortality risk in non-AF patients with mild-to-moderate IPF is unknown and, as far as we know, literature data are missing.
Accordingly, the present study was primarily designed to investigate whether the CHA2DS2-VASc score can predict the primary outcome of “all‐cause mortality” over a medium-term follow-up in a consecutive population of IPF patients without severe pulmonary hypertension and with no evidence of AF. The prognostic value of other clinical scores, such as the HAS-BLED (Hypertension, Abnormal renal/liver function, Stroke, Bleeding history or predisposition, Labile international normalized ratio, Elderly > 65 years, Drugs/alcohol concomitantly) score [36], the CAC score, the GAP index and the CCI was also examined in the same study population.
METHODS
Patient selection
All consecutive patients with mild-to-moderate IPF, followed at the Division of Pneumology of San Giuseppe Hospital, a tertiary reference center for interstitial lung diseases in Italy, between January 2016 and December 2018, were retrospectively analyzed. The study period was chosen to provide at least three years of follow-up on participants.
Diagnosis of IPF was made according to the latest clinical practice guidelines [1] by adopting a multidisciplinary approach involving pulmonologists, radiologists, and pathologists experienced in the diagnosis of interstitial lung disease, especially for those patients with a radiological pattern of probable usual interstitial pneumonia (UIP) or indeterminate for UIP.
Inclusion criteria were: 1) mild-to-moderate IPF defined by forced vital capacity (FVC) > 50% and diffusing capacity of the lungs for carbon monoxide (DLCO) > 35% and by a tricuspid regurgitation velocity (TRV) < 3.4 m/sec, as noninvasively assessed by two-dimensional (2D) transthoracic echocardiography (TTE) [37]; 2) no evidence of AF; 3) IPF patients who had undergone a multi-instrumental approach comprehensive of blood tests, spirometry and DLCO, six-minute walking test (6MWT), high resolution computed tomography (HRCT), electrocardiography (ECG) and 2D-TTE; 4) hemodynamic stability for at least three months at the time of enrollment.
Criteria of exclusion were the following: FVC ≤ 50%; DLCO ≤ 35%; IPF patients with a diagnosis of AF based on 12-lead ECG or 24-h ECG Holter or cardiac telemetry monitoring in hospitalized patients and/or with a history of chronic AF; IPF patients with a high probability of severe pulmonary hypertension; IPF patients with congestive right heart failure at basal evaluation; IPF patients without complete spirometry, ECG and echocardiographic data.
Following demographic, anthropometric, clinical and biochemical parameters were collected from the patients’ hospital medical charts: anagraphic age; body surface area; body mass index; prevalence of following cardiovascular risk factors: smoking history and smoking exposure pack-years, hypertension (defined as arterial blood pressure persistently ≥ 140/90 mmHg or treatment with one or more anti-hypertensive drugs), type 2 diabetes mellitus (defined as a fasting serum glucose level ≥ 126 mg/dl confirmed by several tests performed in different days or treatment with one or more oral or parenteral hypoglycemic agents) and dyslipidemia (defined as serum total cholesterol ≥ 200 mg/dl, serum HDL-cholesterol ≤ 40 mg/dl and serum triglycerides ≥ 150 mg/dl); history of CAD (previous acute coronary syndrome, previous percutaneous and/or surgical coronary revascularization); history of stroke and/or transient ischemic attack; information concerning the patient’s atherosclerotic disease burden, such as the degree of carotid artery stenosis, coronary artery calcification and lower extremity peripheral artery disease; pulmonary function tests; the total distance walked during 6MWT; electrocardiographic data (heart rate and pattern of intraventricular conduction); the main comorbidities, such as cancers, chronic obstructive pulmonary disease (COPD), obstructive sleep apnea syndrome (OSAS), gastroesophageal reflux disease (GERD), hypothyroidism and mixed anxiety–depressive disorder; blood tests comprehensive of complete blood count for determining hemoglobin concentration and red cell distribution width (RDW), serum levels of creatinine and estimated glomerular filtration rate (eGFR) [38], serum levels of C-reactive protein (CRP), N-terminal pro-B-type natriuretic peptide (NT-proBNP) and total cholesterol; finally, the current medical treatment.
At the basal evaluation, each patient underwent accurate anamnesis, complete physical examination comprehensive of spirometry, DLCO and 6MWT, arterial blood gases, blood analysis, HRCT, 12-lead ECG and finally conventional 2D-TTE.
All procedures were performed according to the ethical standards of the institutional research committee and to the Declaration of Helsinki (1964) and its subsequent amendments or equivalent ethical standards. The study protocol was authorized by the local Ethics Committee (Committee’s reference number 544/202).
Clinical prognostic scores
For each IPF patient, following scores were retrospectively calculated: 1) the CHA2DS2-VASc [Congestive heart failure or left ventricular dysfunction (1 point), Hypertension (1 point), Age ≥ 75 years (2 points), Diabetes (1 point), Stroke/TIA (2 points), Vascular disease (1 point), Age 65–74 years (1 point), and Sex category (female; 1 point)] score [25]; 2) the HAS-BLED [Hypertension (1 point), Abnormal renal/liver function (1 or 2 points), Stroke (1 point), Bleeding history or predisposition (1 point), Labile international normalized ratio (1 point), Elderly (> 65 years) (1 point), Drugs/alcohol concomitantly (1 or 2 points)] score [36]; 3) the GAP index, which assigned 1 point for male sex, age 61–65 years, FVC 50–75% and DLCO 36–55%; 2 points for age > 65 years, FVC < 50%, DLCO ≤ 35%; 3 points for inability to perform spirometry [22]; 4) the CCI, which assigned 1 point for each of the following comorbidities: myocardial infarction, congestive heart failure, peripheral vascular disease, dementia, cerebrovascular disease, chronic lung disease, connective tissue disease, ulcer, chronic liver disease, diabetes; 2 points for each of hemiplegia, moderate or severe kidney disease, diabetes with end-organ damage, tumor, leukemia, lymphoma; 3 points for moderate or severe liver disease; and 6 points for tumor metastasis or AIDS [23].
High-resolution computed tomography
At the time of diagnosis, all IPF patients underwent HRCT examination. CT scans were interpreted by two expert radiologists (R.T. and M.Z.) which independently described the pattern of fibrosis and measured the CAC score according to the Agatston method [39]. The amount of CAC was quantified using semiautomatic software (CaScoring, Syngo.via VB30A, Siemens Healthineers). Notably, the software employed a deep-learning approach based on two consecutive convolutional neural networks to detect calcifications and to label them according to the affected vascular bed. In this study, the total amount of calcification detected in the coronary arteries (CAC score) was calculated. Only voxels with an intensity of at least 130 Hounsfield unit (HU), which is the standard threshold for calcium scoring, were taken into consideration [40]. The calcified plaques were assigned manually to their respective coronary artery by a mouse click, with a subsequent automatic evaluation of the lesions by a 3D segmentation algorithm.
Conventional echoDoppler examination
All echocardiograms were performed by the same expert cardiologist (A.S.) using a Philips Sparq ultrasound machine (Philips, Andover, Massachusetts, USA) with a 2.5 MHz transducer. All parameters were measured according to the Recommendations of the American Society of Echocardiography and the European Association of Cardiovascular Imaging [41, 42].
Following M-mode and 2D echocardiographic parameters were recorded: (1) relative wall thickness; (2) left ventricular mass index, calculated by the Deveraux formula; (3) left ventricular end-diastolic volume index, left ventricular end-systolic volume index and left ventricular ejection fraction (LVEF) estimated with the biplane modified Simpson’s method [41]; (4) left atrial volume index; (5) right ventricular inflow tract, right ventricular to left ventricular (LV) basal diameter ratio and tricuspid annular plane systolic excursion (TAPSE) from the apical four-chamber view; 6) finally, the inferior vena cava (IVC) diameter from a subcostal view.
Doppler measurements included the E/A ratio and the average E/e’ ratio, the latter as an index of left ventricular filling pressure [42]. Systolic pulmonary artery pressure (SPAP) was derived by the modified Bernoulli equation, where SPAP = 4 x (tricuspid regurgitation velocity)2 + right atrial pressure [37]. The latter was estimated from IVC diameter and collapsibility.
Degree of valvulopathy was assessed according to the AHA/ACC recommendations for the management of patients with valvular heart disease [43].
Endpoint definition
The primary endpoint of the study was to identify the independent predictors of “all-cause mortality” in a consecutive cohort of IPF patients without severe pulmonary hypertension, over a medium-term follow-up.
The secondary endpoint was to evaluate the independent predictors of the composite of “all-cause mortality and rehospitalizations for all causes” in the same study group.
Causes of death and rehospitalizations for each IPF patient were determined by accessing medical records available in the hospital archive and/or from telephone interviews.
Statistical analysis
For statistical power calculation, we hypothesized that, on the basis of available literature data [44, 45], by dividing IPF patients into two main categories (those with CHA2DS2-VASc score > 4 and those with CHA2DS2-VASc score ≤ 4), IPF patients with CHA2DS2-VASc score > 4 might have a significantly higher risk of all-cause mortality than those with CHA2DS2-VASc score ≤ 4. Assuming that IPF patients with CHA2DS2-VASc score > 4 and those with CHA2DS2-VASc score ≤ 4 might have 3-year mortality of 20 and 9%, respectively, a sample size of 103 IPF patients would reach a statistical power of 100% for determining a statistically significant difference between mortality rates, using a two-tailed t test with type I error at 5%.
For the whole cohort of IPF patients included, continuous data were summarized as mean ± standard deviation, while categorical data were presented as number (percentage).
Univariate Cox regression analysis was performed to evaluate the effect of the main demographics and anthropometrics, cardiovascular risk factors, clinical predictive scores (expressed as continuous variables), biochemical parameters, ECG and echoDoppler variables and discharge medical treatment, on the occurrence of both primary and secondary endpoints during the follow-up period, in the whole study population. For each variable investigated, correspondent hazard ratios with 95% confidence intervals (CIs) were calculated. Only the variables with the statistically significant association on univariate analysis (p value < 0.05) were thereafter included in the multivariate Cox regression model.
The receiver operating characteristics (ROC) curve analysis was performed to establish the sensitivity and specificity of the CHA2DS2-VASc score for predicting the above-mentioned endpoints. Area under the curve (AUC) was estimated. The optimal cutoff of CHA2DS2-VASc score was calculated using the maximum value of the Youden Index (determined as sensitivity + [1-specificity]).
Kaplan–Meier survival curves were designed to measure differences between CHA2DS2-VASc score categories in the rates of “all-cause mortality” and “all-cause mortality and rehospitalizations for all causes” respectively, over a mid-term follow-up, for the whole study population.
Statistical analysis was performed with SPSS version 26 (SPSS Inc., Chicago, Illinois, USA), with two-tailed p values below 0.05 deemed statistically significant.
Results
Between January 2016 and December 2018, 170 patients referred to our Division of Pneumology received a diagnosis of IPF, confirmed by adopting a multidisciplinary approach: among them, 18 patients with AF and 49 patients with severe pulmonary hypertension were excluded from the present study according to the above-mentioned exclusion criteria. The remaining 103 IPF patients (mean age 70.7 ± 7.3 yrs) were retrospectively analyzed.
All clinical parameters recorded in the study population at baseline are summarized in Table 1.
As expected, IPF patients were predominantly men (79.6%) with a smoking history (80.6%) and a moderate prevalence of hypertension (57.3%) and dyslipidemia (51.4%). Moreover, they showed a moderate atherosclerotic disease burden, expressed by more than mild carotid artery stenosis in 30.1% of patients, diffuse CAC on HRCT in 48.5% of patients and polidistrectual vasculopathy in 13.6% of patients.
Blood tests revealed chronic renal failure (eGFR < 60 ml/min/1.73 m2) in 16.5% of patients; in addition, the whole series of IPF patients was found with a mild chronic inflammation (serum CRP 1.2 ± 1.6 mg/dl; normal value < 0.05 mg/dl) and a moderate increase in serum NT-proBNP levels (384.8 ± 912.0 pg/ml; normal value < 125 pg/ml).
The values of the CHA2DS2-VASc score (3.7 ± 1.6) and HAS-BLED score (2.6 ± 1.7) measured in our study population at baseline suggested a moderate-to-high risk for thromboembolic and hemorrhagic events, respectively.
Main non-cardiovascular comorbidities detected in our cohort of IPF patients were GERD, COPD and hypothyroidism; cancers and OSAS were observed less frequently. GAP index was 3.6 ± 1.2, whereas the CCI score was 5.5 ± 2.3, indicating high comorbidity.
Concerning the pharmacological treatment, less than half of IPF patients were regularly treated with cardioprotective drugs. Notably, oral anticoagulants, beta-blockers and statins were prescribed in only 10.7%, 35.9% and 33% of IPF patients. In addition, 42.7% of IPF patients were in oxygen therapy; approximately one-third of IPF patients (30.1%) received a low dose of oral corticosteroids (< 10 mg/die); finally, 37.9% and 54.4% of IPF patients were treated with pirfenidone and nintedanib, respectively.
Table 2 lists all instrumental variables detected by HRCT, spirometry, ECG and conventional TTE, respectively, in our cohort of IPF patients, at basal evaluation.
Concerning the radiological findings, the definite UIP pattern at HRCT was the prevalent pattern (62.1% of cases), followed by a pattern of probable UIP (23.3% of cases), whereas an indeterminate pattern was detected in 14.6% of cases. CAC score at basal evaluation was 768.9 ± 998.4 HU.
Analysis of spirometric parameters revealed that FVC (81.8 ± 17.9% of predicted) and forced expiratory volume in the first second (FEV1) (86.0 ± 17.8% of predicted) were slightly impaired, while DLCO (52.0 ± 15.5% of predicted) was moderately reduced. 58.2% of IPF patients had a restrictive pattern. Moreover, IPF patients showed a moderate decrease in pulse oximetry and a moderate reduction in effort tolerance during the 6MWT.
On resting ECG, the heart rate was normal (73.3 ± 11.4 bpm) and 17.5% of IPF patients had delayed intraventricular conduction.
Conventional TTE examination showed normal biventricular and biatrial cavity chamber sizes. The LV concentric remodeling was the most common LV geometric pattern detected in IPF patients (49.5% of total), followed by normal LV geometry (34.0% of cases); on the other hand, LV concentric hypertrophy (10.7% of cases) and LV eccentric hypertrophy (5.8% of cases) were rarely detected. The great majority of IPF patients (75.7%) had preserved LV systolic function (LVEF ≥ 55%), whereas 25 patients (24.3% of total) presented LV systolic dysfunction (LVEF < 55%). Among IPF patients with LV systolic dysfunction, the vast majority (23 patients, 92% of total) showed a mild reduction in systolic function (LVEF between 45 and 54%), whereas only two patients had LVEF < 45%. Analysis of LV diastolic function revealed that grade 1 diastolic dysfunction was the most frequently detected LV diastolic filling pattern (95.2% of patients), while a pseudonormal filling pattern of the left ventricle was rarely detected (4.8% of patients). Moreover, left ventricular filling pressures measured in IPF patients were in the gray zone of 8 to 13 (average E/e’ ratio 11.6 ± 3.1). In addition, we observed a low prevalence of valvular heart disease: a more than mild mitral regurgitation and aortic regurgitation was observed in 14.6% and 7.8% of IPF patients, respectively, while no IPF patient was diagnosed with aortic stenosis. Finally, a mild pulmonary hypertension (TRV 2.9 ± 0.4 m/sec) was detected in our cohort of IPF patients. Only 23 patients (22.3% of the total) were found with right ventricular systolic dysfunction, expressed by reduced TAPSE (< 20 mm).
Survival analysis
Mean follow-up time was 3.5 ± 1.3 yrs. During the follow-up period, 29 in-hospital deaths and 43 rehospitalizations were recorded. Rehospitalizations were secondary to 1) cardiovascular causes (18.6%): acute ischemic stroke/transient ischemic attack (6 patients) and acute coronary syndrome (2 patients); 2) cardiopulmonary causes (44.2%): right heart failure (11 patients) and acute pulmonary embolism (8 patients); 3) pulmonary causes (37.2%): acute respiratory failure secondary to IPF progression (7 patients), pneumonia (6 patients), pneumomediastinum (2 patients) and pneumothorax (1 patient).
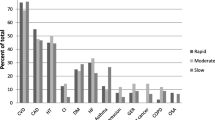
Univariate and multivariate Cox regression analysis performed for identifying the main independent predictors of “all-cause mortality” during the follow-up period in the whole study population is reported in Table 3. CHA2DS2-VASc score (HR 2.15, 95% CI 1.59–2.91, p < 0.001) and LVEF (HR 0.91, 95% CI 0.86–0.97, p = 0.003) were the only variables that resulted independently associated with the above-mentioned outcome. A CHA2DS2-VASc score > 4 (90% sensitivity, 99% specificity, AUC = 0.97) and an LVEF < 55% (65% sensitivity and 69% specificity, AUC = 0.69) showed the greatest sensitivity and specificity for predicting the primary endpoint in the whole study population.
On multivariate Cox regression analysis performed for detecting the variables independently associated with the composite of “all-cause mortality and rehospitalizations for all causes” in the whole study population, only CHA2DS2-VASc score (HR 1.66, 95% CI 1.39–1.99, p < 0.001) and LVEF (HR 0.94, 95% CI 0.90–0.98, p = 0.003) maintained statistical significance. A CHA2DS2-VASc score > 4 (64% sensitivity, 100% specificity, AUC = 0.91) and an LVEF < 55% (51% sensitivity and 99% specificity, AUC = 0.75) were the best cut-off values for predicting the secondary endpoint in the whole study population.
Fig. 1 illustrates prognostic ROC curves and Kaplan-Meier survival curves drawn to compare the rates of the endpoint “all-cause mortality” (Panels A1 and A2) and the endpoint “all-cause mortality and rehospitalizations for all causes” (Panels B1 and B2) in IPF patients, categorized according to CHA2DS2-VASc score ≤4 and >4, respectively.-
Prognostic ROC curves and Kaplan–Meier survival curves were drawn to compare the rates of the endpoint “all-cause mortality” (Panels A1 and A2) and the endpoint “all-cause mortality + rehospitalizations for all causes” (Panels B1 and B2) in IPF patients, categorized according to CHA2DS2-VASc score ≤ 4 and > 4, respectively. AUC, area under the curve; CHA2DS2-VASc, Congestive heart failure or left ventricular dysfunction, Hypertension, Age ≥ 75 years, Diabetes, Stroke/TIA, Vascular disease, Age 65–74 years, and Sex category; IPF, idiopathic pulmonar fibrosis; ROC, receiver operating characteristics
Discussion
Main findings of the study
This monocentric study, specifically designed to evaluate the main indicators of adverse clinical outcomes in a consecutive cohort of non-AF patients with mild-to-moderate IPF, demonstrated that: (1) the CHA2DS2-VASc score was independently associated with “all-cause mortality” and with the composite of “all-cause mortality and rehospitalizations for all causes” in the whole study population, over a medium-term follow-up; (2) the CHA2DS2-VASc score showed an incremental prognostic value over the individual components of the score, over other clinical (GAP, CCI and HAS-BLED) and radiological (CAC) scores and over biochemical predictors, such as RDW, eGFR, CRP and NT-proBNP; (3) IPF patients had a significantly increased prevalence of adverse cardiovascular and cardiopulmonary events; (4) “all-cause deaths” were recorded within 4 yrs after hospital discharge in the great majority of IPF patients.
Our results revealed that a CHA2DS2-VASc score > 4 at basal evaluation allowed us to distinguish, among IPF patients, those with an increased probability of all-cause mortality, over a medium-term follow-up. Notably, IPF patients with a CHA2DS2-VASc score > 4 had about a twofold higher risk of mortality and rehospitalizations for all causes than those with a CHA2DS2-VASc score ≤ 4. This finding could be related to the older age, to the increased prevalence of hypertension, chronic renal failure and congestive clinical signs and to the higher atherosclerotic disease burden detected in most patients with CHA2DS2-VASc score > 4. On the other hand, IPF patients with CHA2DS2-VASc score ≤ 4 had a significantly increased probability of event-free survival over the follow-up period.
LVEF assessed by 2D-TTE examination was another independent prognostic indicator of increased risk of mortality and adverse clinical events in IPF patients.
Comparison with other studies and interpretation of results
Consistent with the literature data [46,47,48], our findings confirmed the poor prognosis of IPF patients. Indeed, approximately one-third of the IPF patients enrolled (28.1%) died within 4 years of follow-up.
To the best of our knowledge, no previous study employed the CHA2DS2-VASc score for the mortality risk stratification of a retrospective cohort of IPF patients without severe pulmonary hypertension and no evidence of AF.
The CHA2DS2-VASc score was originally developed for stroke risk stratification of nonvalvular AF patients, particularly for detecting patients at low risk who require no antithrombotic therapy [49, 50].
Although current guidelines recommend using the CHA2DS2-VASc score for evaluating embolic risk in AF patients [26, 27], during the last decade this score has been assessed in many categories of patients without AF. Notably, a number of studies have tested the predictive value of CHA2DS2-VASc score for clinical outcomes different from stroke such as death, heart failure hospitalizations and cardiac hospitalizations in various cardiovascular and non-cardiovascular diseases [28,29,30,31,32,33,34,35]. In particular, CHA2DS2-VASc score has been strongly associated with major adverse cardiac outcomes in non-AF community populations [28] and in the following categories of non-AF patients: patients discharged after an acute coronary syndrome and/or acute myocardial infarction [29]; heart failure patients [30, 31]; patients with arterial hypertension [32]; patients with peripheral artery disease [33]; finally patients with COPD [34] and SARS-CoV-2 [35].
The results of our study revealed that approximately two-thirds of rehospitalizations observed in IPF patients during the study period were related to cardiovascular and cardiopulmonary causes. The increased prevalence of adverse cardiovascular events over a medium-term follow-up may have been favoured by the high atherosclerotic disease burden and the concomitant comorbid conditions (especially cancers and COPD) detected in our study population. Secondly, our cohort of IPF patients was undertreated with cardioprotective drugs, especially beta-blockers and statins. This finding was in alignment with the literature data [51] and with our previous findings [52].
In addition, our findings highlighted the high negative predictive value of a CHA2DS2-VASc score ≤ 4 for future major adverse clinical events over the follow-up period, similarly to that observed by previous authors in AF patients [53].
The present study also revealed that IPF patients with left ventricular systolic dysfunction (LVEF < 55%) had an increased risk of both mortality and rehospitalizations during the follow-up period. The impairment in LV systolic function, detected in 24.3% of our cohort of patients, was predominantly of mild degree (LVEF between 45 and 55%). This finding was in alignment with what observed by previous authors [54, 55], which demonstrated the absence of a significant reduction in LVEF in IPF patients at an early stage of the disease; on the other hand, a subclinical myocardial dysfunction, expressed by the early impairment in left ventricular global longitudinal strain [54] and left atrial reservoir strain [55], was detected by 2D speckle tracking echocardiography (2D-STE) in the same patients.
Implications for clinical practice
In light of our findings, the CHA2DS2-VASc score assessment could be employed for the routine clinical evaluation of IPF patients, for better prognostic risk stratification of IPF patients without advanced lung disease.
Given that the CHA2DS2-VASc score is simple and only based on the clinical history and no laboratory or imaging parameters, it has the great advantage that it can be quickly calculated, at the patient’s bedside also. Moreover, IPF patients with CHA2DS2-VASc score > 4, given the highest cardiovascular risk profile, would need a more intensive treatment of comorbidities, a closer clinical follow-up and/or uptitration of cardioprotective drugs, such as beta-blockers and statins.
Limitations
Main limitations of the present study were its retrospective nature, the monocentric design, the lack of external validation and the limited number of IPF patients included, due to the rarity of the disease. However, the great number of major adverse clinical outcomes detected over a mid-term follow-up allowed us to perform an accurate survival analysis in this study group.
Despite the prognostic relevance of myocardial strain parameters assessed by 2D-STE in various clinical settings [56,57,58], the present study did not evaluate their prognostic role in IPF patients, due to the retrospective design of the study.
Finally, inflammatory biomarkers, including Krebs von den Lungen-6 (KL-6), surfactant protein-A (SP-A) and D (SP-D), matrix metalloproteinase-7 (MMP-7), were not assessed in our study population. However, even if these markers have been identified as having a potential diagnostic and prognostic value in IPF [8,9,10,11], they are not yet considered applicable for routine risk assessment of these patients.
Conclusions
CHA2DS2-VASc score is independently associated with all-cause mortality and rehospitalizations for all causes over a medium-term follow-up in non-AF patients with non-advanced IPF.
A CHA2DS2-VASc score > 4 allows us to identify, among IPF patients, those with increased risk of mortality and for whom additional preventive measures might be beneficial to improve outcomes.
Further multicentric prospective studies are needed to confirm the present results.
Data Availability
The data underlying this article will be shared on reasonable request to the corresponding author.
Abbreviations
- 2D:
-
Two-dimensional
- 6MWT:
-
Six-minute walking test
- ACEIs:
-
Angiotensin-converting enzyme inhibitors
- AF:
-
Atrial fibrillation
- ARBs:
-
Angiotensin II receptor blockers
- AUC:
-
Area under the curve
- CAC:
-
Coronary artery calcification
- CAD:
-
Coronary artery disease
- CCI:
-
Charlson comorbidity index
- CHA2DS2-VASc:
-
Congestive heart failure or left ventricular dysfunction, Hypertension, Age ≥ 75 years, Diabetes, Stroke/TIA, Vascular disease, Age 65–74 years, and Sex category
- CIs:
-
Confidence intervals
- COPD:
-
Chronic obstructive pulmonary disease
- CRP:
-
C-reactive protein
- DLCO:
-
Diffusing capacity of the lungs for carbon monoxide
- ECG:
-
Electrocardiography
- eGFR:
-
Estimated glomerular filtration rate
- FEV1:
-
Forced expiratory volume in the first second
- FVC:
-
Forced vital capacity
- GAP:
-
Gender-age-physiology
- GERD:
-
Gastroesophageal reflux disease
- HAS-BLED:
-
Hypertension, Abnormal renal/liver function, Stroke, Bleeding history or predisposition, Labile international normalized ratio, Elderly (> 65 years), Drugs/alcohol concomitantly
- HRCT:
-
High-resolution computed tomography
- HU:
-
Hounsfield unit
- IPF:
-
Idiopathic pulmonary fibrosis
- IVC:
-
Inferior vena cava
- LV:
-
Left ventricular
- LVEF:
-
Left ventricular ejection fraction
- NT-proBNP:
-
N-terminal pro-brain natriuretic peptide
- OSAS:
-
Obstructive sleep apnea syndrome
- RDW:
-
Red cell distribution width
- ROC:
-
Receiver operating characteristics
- SPAP:
-
Systolic pulmonary artery pressure
- STE:
-
Speckle tracking echocardiography
- TAPSE:
-
Tricuspid annular plane systolic excursion
- TRV:
-
Tricuspid regurgitation velocity
- TTE:
-
Transthoracic echocardiography
- UIP:
-
Usual interstitial pneumonia
References
Raghu G, Remy-Jardin M, Myers JL et al (2018) Diagnosis of idiopathic pulmonary fibrosis. an official ATS/ERS/JRS/ALAT clinical practice guideline. Am J Respir Crit Care Med 198:e44–e68
Wakwaya Y, Brown KK (2019) Idiopathic pulmonary fibrosis: epidemiology, diagnosis andoutcomes. Am J Med Sci 357:359–369
Raghu G, Amatto VC, Behr J, Stowasser S (2015) Comorbidities in idiopathic pulmonary fibrosis patients: a systematic literature review. Eur Respir J 46:1113–1130
van Cleemput J, Sonaglioni A, Wuyts WA, Bengus M, Stauffer JL, Harari S (2019) Idiopathic pulmonary fibrosis for cardiologists: differential diagnosis, cardiovascular comorbidities, and patient management. Adv Ther 36:298–317
King TE Jr, Albera C, Bradford WZ et al (2014) All-cause mortality rate in patients with idiopathic pulmonary fibrosis. Implications for the design and execution of clinical trials. Am J Respir Crit Care Med 189:825–831
Karampitsakos T, Torrisi S, Antoniou K et al (2021) Increased monocyte count and red cell distribution width as prognostic biomarkers in patients with Idiopathic Pulmonary Fibrosis. Respir Res 22:140
Zhuang Y, Zhou Y, Qiu X, Xiao Y, Cai H, Dai J (2020) Incidence and impact of extra-pulmonary organ failures on hospital mortality in acute exacerbation of idiopathic pulmonary fibrosis. Sci Rep 10:10742
Satoh H, Kurishima K, Ishikawa H, Ohtsuka M (2006) Increased levels of KL-6 and subsequent mortality in patients with interstitial lung diseases. J Intern Med 260:429–434
Kinder BW, Brown KK, McCormack FX et al (2009) Serum surfactant protein-A is a strong predictor of early mortality in idiopathic pulmonary fibrosis. Chest 135:1557–1563
Ikeda K, Shiratori M, Chiba H et al (2017) Serum surfactant protein D predicts the outcome of patients with idiopathic pulmonary fibrosis treated with pirfenidone. Respir Med 131:184–191
Rosas IO, Richards TJ, Konishi K et al (2008) MMP1 and MMP7 as potential peripheral blood biomarkers in idiopathic pulmonary fibrosis. PLoS Med 5:e93
Song JW, Song JK, Kim DS (2009) Echocardiography and brain natriuretic peptide as prognostic indicators in idiopathic pulmonary fibrosis. Respir Med 103:180–186
Snyder L, Neely ML, Hellkamp AS et al (2019) Predictors of death or lung transplant after a diagnosis of idiopathic pulmonary fibrosis: insights from the IPF-PRO Registry. Respir Res 20:105
Alhamad EH, Cal JG (2020) Predictors of mortality in interstitial lung disease patients without pulmonary hypertension. Ann Thorac Med 15:238–243
Rivera-Lebron BN, Forfia PR, Kreider M, Lee JC, Holmes JH, Kawut SM (2013) Echocardiographic and hemodynamic predictors of mortality in idiopathic pulmonary fibrosis. Chest 144:564–570
Chen X, Guo J, Yu D, Jie B, Zhou Y (2021) Predictors of mortality in progressive fibrosing interstitial lung diseases. Front Pharmacol 12:754851
Sonaglioni A, Caminati A, Nicolosi GL, Lombardo M, Harari S (2022) Incremental prognostic value of arterial elastance in mild-to-moderate idiopathic pulmonary fibrosis. Int J Cardiovasc Imaging. https://doi.org/10.1007/s10554-022-02541-y. (Epub ahead of print. PMID: 35103898)
Nathan SD, Weir N, Shlobin OA et al (2011) The value of computed tomography scanning for the detection of coronary artery disease in patients with idiopathic pulmonary fibrosis. Respirology 16:481–486
Kreuter M, Ehlers-Tenenbaum S, Palmowski K et al (2016) Impact of comorbidities on mortality in patients with idiopathic pulmonary fibrosis. PLoS ONE 11:e0151425
Caminati A, Lonati C, Cassandro R et al (2019) Comorbidities in idiopathic pulmonary fibrosis: an underestimated issue. Eur Respir Rev 28:190044
Caminati A, Zompatori M, Fuccillo N et al (2022) Coronary artery calcium score is a prognostic factor for IPF progression and mortality. Minerva Med. https://doi.org/10.23736/S0026-4806.22.08018-1. (Epub ahead of print. PMID: 35671002)
Ley B, Ryerson CJ, Vittinghoff E et al (2012) A multidimensional index and staging system for idiopathic pulmonary fibrosis. Ann Intern Med 156:684–691
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Keramidas G, Gourgoulianis KI, Kotsiou OS (2021) Venous thromboembolic disease in chronic inflammatory lung diseases: knowns and unknowns. J Clin Med 10:2061
Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ (2010) Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest 137:263–272
January CT, Wann LS, Calkins H et al (2019) 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American college of cardiology/American heart association task force on clinical practice guidelines and the heart rhythm society. J Am Coll Cardiol 74:104–132
Hindricks G, Potpara T, Dagres N et al (2021) 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European association for cardio-thoracic surgery (EACTS): the task force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) developed with the special contribution of the European heart rhythm association (EHRA) of the ESC. Eur Heart J 42:373–498
Lip GY, Lin HJ, Chien KL et al (2013) Comparative assessment of published atrial fibrillation stroke risk stratification schemes for predicting stroke, in a non-atrial fibrillation population: the Chin-Shan community cohort study. Int J Cardiol 168:414–419
Kim KH, Kim W, Hwang SH et al (2015) The CHA2DS2VASc score can be used to stratify the prognosis of acute myocardial infarction patients irrespective of presence of atrial fibrillation. J Cardiol 65:121–127
Melgaard L, Gorst-Rasmussen A, Lane DA, Rasmussen LH, Larsen TB, Lip GY (2015) Assessment of the CHA2DS2-VASc Score in Predicting Ischemic Stroke, thromboembolism, and death in patients with heart failure with and without atrial fibrillation. JAMA 314:1030–1038
Sonaglioni A, Lonati C, Rigamonti E et al (2022) CHA2DS2-VASc score stratifies mortality risk in heart failure patients aged 75 years and older with and without atrial fibrillation. Aging Clin Exp Res 34:1707–1720
Mazzone C, Cioffi G, Carriere C et al (2017) Predictive role of CHA2DS2-VASc score for cardiovascular events and death in patients with arterial hypertension and stable sinus rhythm. Eur J Prev Cardiol 24:1584–1593
Yalim Z, Aldemir M, Yalim SA (2020) Assessment of the relationship between death and CHA2DS2-VASc score in peripheral artery disease. Int Angiol 39:509–516
Ooi H, Chen LH, Ni YL et al (2018) CHA2DS2-VASc scores predict major adverse cardiovascular events in patients with chronic obstructive pulmonary disease. Clin Respir J 12:1038–1045
Katkat F, Karahan S, Varol S, Kalyoncuoglu M, Okuyan E (2021) Mortality prediction with CHA2DS2-VASc, CHA2DS2-VASc-HS and R2CHA2DS2-VASc score in patients hospitalized due to COVID-19. Eur Rev Med Pharmacol Sci 25:6767–6774
Pisters R, Lane DA, Nieuwlaat R, de Vos CB, Crijns HJ, Lip GY (2010) A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey. Chest 138:1093–1100
Humbert M, Kovacs G, Hoeper MM et al (2022) 2022 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Heart J 43:3618–3731
Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D (1999) A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. modification of diet in renal disease study group. Ann Intern Med 130:461–470
Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M Jr, Detrano R (1990) Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol 15:827–832
Ohnesorge B, Flohr T, Fischbach R et al (2002) Reproducibility of coronary calcium quantification in repeat examinations with retrospectively ECG-gated multisection spiral CT. Eur Radiol 12:1532–1540
Lang RM, Badano LP, Mor-Avi V et al (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American society of echocardiography and the European association of cardiovascular imaging. J Am Soc Echocardiogr 28:1-39.e14
Nagueh SF, Smiseth OA, Appleton CP et al (2016) Recommendations for the evaluation of left ventricular diastolic function by echocardiography: An update from the American society of echocardiography and the European association of cardiovascular Imaging. J Am Soc Echocardiogr 29:277–314
Nishimura RA, Otto CM, Bonow RO et al (2017) 2017 AHA/ACC focused update of the 2014 AHA/ACC guideline for the management of patients with valvular Heart disease: A report of the American college of Cardiology/American heart association task force on clinical practice guidelines. Circulation 135:e1159–e1195
Paoletti Perini A, Bartolini S, Pieragnoli P et al (2014) CHADS2 and CHA2DS2-VASc scores to predict morbidity and mortality in heart failure patients candidates to cardiac resynchronization therapy. Europace 16:71–80
Wang BY, Lin FY, Ku MS, Wang YH, Lee KY, Ho SW (2021) CHA2DS2-VASc score for major adverse cardiovascular events stratification in patients with pneumonia with and without atrial fibrillation. J Clin Med 10:4093
Richeldi L, Collard HR, Jones MG (2017) Idiopathic pulmonary fibrosis. Lancet 389:1941–1952
Harari S, Madotto F, Caminati A, Conti S, Cesana G (2016) Epidemiology of Idiopathic pulmonary fibrosis in northern italy. PLoS ONE 11:e0147072
Harari S, Davì M, Biffi A et al (2020) Epidemiology of idiopathic pulmonary fibrosis: a population-based study in primary care. Intern Emerg Med 15:437–445
Lip GY, Lane DA (2014) Modern management of atrial fibrillation requires initial identification of “low-risk” patients using the CHA2DS2-VASc score, and not focusing on “high-risk” prediction. Circ J 78:1843–1845
Chan YH, Wu LS, Chang SH et al (2016) Young male patients with atrial fibrillation and CHA2DS2-VASc score of 1 may not need anticoagulants: a nationwide population-based study. PLoS ONE 11:e0151485
Hubbard RB, Smith C, Le Jeune I, Gribbin J, Fogarty AW (2008) The association between idiopathic pulmonary fibrosis and vascular disease: a population-based study. Am J Respir Crit Care Med 178:1257–1261
Sonaglioni A, Caminati A, Lipsi R, Lombardo M, Harari S (2021) Association between C-reactive protein and carotid plaque in mild-to-moderate idiopathic pulmonary fibrosis. Intern Emerg Med 16:1529–1539
Proietti M, Farcomeni A, Romiti GF et al (2020) Association between clinical risk scores and mortality in atrial fibrillation: systematic review and network meta-regression of 669,000 patients. Eur J Prev Cardiol 27:633–644
Buonauro A, Santoro C, Galderisi M et al (2020) Impaired right and left ventricular longitudinal function in patients with fibrotic interstitial lung diseases. J Clin Med 9:587
Sonaglioni A, Caminati A, Lipsi R et al (2020) Early left atrial dysfunction in idiopathic pulmonary fibrosis patients without chronic right heart failure. Int J Cardiovasc Imaging 36:1711–1723
Sonaglioni A, Lonati C, Lombardo M et al (2019) Incremental prognostic value of global left atrial peak strain in women with new-onset gestational hypertension. J Hypertens 37:1668–1675
Sonaglioni A, Vincenti A, Baravelli M et al (2019) Prognostic value of global left atrial peak strain in patients with acute ischemic stroke and no evidence of atrial fibrillation. Int J Cardiovasc Imaging 35:603–613
Sonaglioni A, Nicolosi GL, Rigamonti E, Lombardo M (2021) Incremental prognostic role of left atrial reservoir strain in asymptomatic patients with moderate aortic stenosis. Int J Cardiovasc Imaging 37:1913–1925
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
AS, AC, MR, DE, AG: Conceptualization; Data curation; Investigation; Methodology; Software; Visualization; Writing—original draft. RT, MZ: Data curation; Methodology; Writing—review and editing. ML, SH.: Conceptualization; Supervision; Validation; Writing—review & editing.
Corresponding author
Ethics declarations
Conflict of interest
We wish to confirm that there are no conflicts of interest associated with this publication. Andrea Sonaglioni declares that he has no conflict of interest. Antonella Caminati reports personal fees from Roche and Boehringer Ingelheim, outside the submitted work. Margherita Re declares that she has no conflict of interest. Davide Elia declares that he has no conflict of interest. Roberta Trevisan declares that she has no conflict of interest. Alberto Granato declares that he has no conflict of interest. Maurizio Zompatori declares that he has no conflict of interest. Michele Lombardo declares that he has no conflict of interest. Sergio Harari reports grants and personal fees from AstraZeneca and Boehringer Ingelheim, outside the submitted work.
Human and animal rights
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
The need for informed consent was not required due to the retrospective nature of this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sonaglioni, A., Caminati, A., Re, M. et al. Prognostic role of CHA2DS2-VASc score for mortality risk assessment in non-advanced idiopathic pulmonary fibrosis: a preliminary observation. Intern Emerg Med 18, 755–767 (2023). https://doi.org/10.1007/s11739-023-03219-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-023-03219-6