Abstract
Background
The subsequent waves of the COVID-19 pandemic in Italy had a major impact on cardiac care.
Methods
A survey to evaluate the dynamic changes in arrhythmia care during the first five waves of COVID-19 in Italy (first: March–May 2020; second: October 2020–January 2021; third: February–May 2021; fourth: June–October 2021; fifth: November 2021–February 2022) was launched.
Results
A total of 127 physicians from arrhythmia centers (34% of Italian centers) took part in the survey. As compared to 2019, a reduction in 40% of elective pacemaker (PM), defibrillators (ICD), and cardiac resynchronization devices (CRT) implantations, with a 70% reduction for ablations, was reported during the first wave, with a progressive and gradual return to pre-pandemic volumes, generally during the third–fourth waves, slower for ablations. For emergency procedures (PM, ICD, CRT, and ablations), recovery from the initial 10% decline occurred in most cases during the second wave, with some variability. However, acute care for atrial fibrillation, electrical cardioversions, and evaluations for syncope showed a prolonged reduction of activity. The number of patients with devices which started remote monitoring increased by 40% during the first wave, but then the adoption of remote monitoring declined.
Conclusions
The dramatic and profound derangement in arrhythmia management that characterized the first wave of the COVID-19 pandemic was followed by a progressive return to the volume of activities of the pre-pandemic periods, even if with different temporal dynamics and some heterogeneity. Remote monitoring was largely implemented during the first wave, but full implementation is needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The infection by Sars-Cov-2 was recognized by the World Health Organization as a pandemic on March 11, 2020, and Italy was the first European country affected by the impact of COVID-19, with the need to take urgent decisions both for limiting the transmission across the country and for the organization of care, with important implications for management of cardiovascular diseases, both in patients affected and not affected by Sars-Cov-2 [1,2,3,4,5,6,7,8].
The impact of the first wave of COVID-19, in 2020 was devastating and many reports in literature were addressed to analyze the difficulties in the provision of care, both in the emergency and chronic care settings [9, 10]. In the field of cardiology, the dramatic worsening in the outcome of patients with cardiac arrest and myocardial infarction, that occurred in the first wave of COVID-19, related to delay in hospital admission, was clearly outlined [11,12,13]. Also in the field of arrhythmias and cardiac pacing, a dramatic reduction was reported in the number of patients admitted for arrhythmia problems, including AF [14]. However, no reports are available on the temporal trends of the impact of the COVID-19 pandemic concerning activities related to arrhythmia management taking into account all the subsequent waves that characterized the pandemic in Italy. The Italian Association of Arrhythmology and Cardiac Pacing (AIAC) launched a survey among its members to specifically report on the situation of cardiac care for arrhythmia during the five waves that characterized the COVID-19 pandemic in Italy between March 2020 and February 2022 [15].
Methods
From March 11 to June 8, 2022, a survey endorsed by the Italian Association of Arrhythmology and Cardiac Pacing (AIAC) was published on the official AIAC website (http://aiac.it/). The survey was open to physicians operating in all Italian arrhythmia centers. Participation in the survey was voluntary. The questionnaire could only be completed by one physician per center.
The questionnaire consisted of 19 questions: five of them focused on the characteristics of the participating centers (i.e., involvement of the centers and of the physicians in the management of suspected and confirmed patients with COVID-19, volume of annual cardiac implantable electronic devices, CIEDs, implantations, and ablation procedures); ten of them focused on the impact of the first five waves of COVID-19 pandemic on the number of CIEDs implantations and ablation procedures performed in both elective and emergency settings, on the number of cases of acute pharmacological and non-pharmacological treatment of atrial fibrillation (AF) in emergency setting, on the number of elective direct-current cardioversion (DCC), and on the number of elective evaluations of patients with syncope; 2 of them focused on the impact of COVID-19 pandemic on the management of remote monitoring (RM) of CIEDs; the remaining two were focused on the impact of the first five pandemic waves on the organizational aspects of CIED replacement procedures. Fifteen of the 19 questions were multiple-choice questions (see online Supplementary material for details).
RM it is a method of remote CIEDs interrogation from the patient's residence alternative to the traditional outpatient visits. This technology provides access to complete information on device settings and status, battery and lead parameters, as well as on arrhythmic burden and electrical therapies delivered. Some patient’s physiological parameters can also be monitored. This remote interrogation can be used for scheduled and unscheduled technical and patient monitoring and follow-up. This information can result in alerts that may require a response from the cardiologist or allied professional.
The first five waves of the COVID-19 pandemic were defined as follows: first wave, from March to May 2020; second wave, from October 2020 to January 2021; third wave, from February to May 2021; fourth wave, from June to October 2021; fifth wave, from November 2021 to February 2022 (Fig. 1) [15].
The first five waves of the COVID-19 pandemic as observed in Italy. *Data from Italian Civil Protection Department [15]
Statistical analysis
Descriptive statistics were reported as means and standard deviations for normally distributed continuous variables. Continuous variables with skewed distribution were reported as medians and 25–75th percentiles. Student’s t-test or the Mann–Whitney U test or the analysis of variance was used to compare continuous variables between groups. Categorical variables were reported as percentages and compared using the χ2 test or Fisher’s exact test, as appropriate. Two-tailed P-values < 0.05 were considered statistically significant.
Results
Participating centers
A total of 127 physicians operating in as many Italian arrhythmia centers took part in the survey. A complete list of participating centers is reported in Acknowledgements. The centers which participated in the survey accounted for 34.1% of all 372 arrhythmia centers operating in Italy in 2019 [16]. The participating centers displayed a wide geographical distribution: a mean of four centers per region (range: 0–19; interquartile range: 2–11) responded. In nine regions, there were five or more participating centers. The response rate was similar in Northern, Central, and Southern Italy (34.0%, 31.4%, and 36.3% of all operating centers, respectively, P = 0.761).
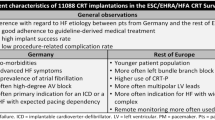
Many participating centers (26.8%) had two operators, 7.1% had only one operator, and 8.7% had more than six operators involved in cardiac electrophysiology and arrhythmia management (Fig. 2, panel A). The rate of participating centers located in hospitals that were designated to treat patients affected by COVID-19 (in some or all the wards) in at least one of the first five waves of the pandemic, and in all the first five waves was 72.4 and 51.2%, respectively. Sixty-six participating centers (52.0%) reported that during the COVID-19 pandemic at least one operator (median: 1; range: 1–6) was directly involved in the management of patients with COVID-19 (for full-time or partial-time management of these patients, including direct patient evaluation during consultations). Passing from the first to the fifth waves of the pandemic, the rate of participating centers with at least one operator, and with > 50% of the operators directly involved in the management of patients with COVID-19 decreased from 45.7 to 25.2%, and from 30.7 to 18.1%, respectively (Fig. 2, panel B).
Number of operators per center (A); rate of centers with at least one operator and with > 50% of operators directly involved in the management of patients with COVID-19 during the first five waves of COVID-19 pandemic (B); the number of CIEDs implantations (C) and of elective ablations (D) performed per year at the participating centers. CIEDs: cardiac implantable electronic devices
The majority of participating centers (54.3%) had implanted from 201 to 500 CIEDs during 2019; 24.3% had implanted from 101 to 200 CIEDs, and the remaining 21.4% < 100 or > 500 (Fig. 2, panel C). In 40.9% of centers, < 50 ablation procedures had been performed during 2019; 26.8% had been performed from 101 to 200 ablation procedures; 32.3% had been performed > 200 ablation procedures (Fig. 2, panel D).
Impact of the first five waves of the COVID-19 pandemic on the activity of participating centers
Procedures performed in an elective setting The vast majority of participating centers (94.5%) reported a significant reduction in the number of elective CIEDs implantations during the first five pandemic waves compared to the same periods of 2019. For elective PM implantations, the greatest reduction was observed during the first wave (median reduction reported of 40%). In the subsequent second and third waves, the extent of the decline gradually decreased (median reduction of 10%), and in the fourth and fifth waves, the majority of participating centers (56.7 and 64.6%, respectively) reported no significant variations compared to the same period of 2019 (Fig. 3, panel A). A similar pattern was observed for implantable cardioverter-defibrillator (ICD) implantations for primary prevention (Fig. 3, panel B), and for cardiac resynchronization therapy (CRT) device implantations (Fig. 3, panel C). The number of ICD implantations for secondary prevention had undergone a lower reduction than ICD implantations for primary prevention: a median reduction of 10% in the first and second waves, no significant variations compared to 2019 for the majority of participating centers during the third, fourth, and fifth waves (54.3, 60.6, and 66.9%, respectively) (Fig. 4, panel A).
Variations in the number of elective PM implantations (A), ICD implantations for primary prevention (B), CRT device implantations (C), and elective ablation procedures (D) during the first five waves of the COVID-19 pandemic compared to the same periods of 2019. The box and whiskers graphs show median, 25th and 75th percentiles, and extreme values. *P < 0.05 compared to CIEDs implantations in emergency setting (see Fig. 4). §P < 0.05 compared to ablations performed in emergency setting (see Fig. 4). ANOVA, analysis of variance; CIED, cardiac implantable electronic device; CRT, cardiac resynchronization therapy; ICD, implantable cardioverter-defibrillator; PM, pacemaker
Variations in the number of ICD implantations for secondary prevention (A), CIEDs implantations in the emergency setting (B), ablation performed in the emergency setting (C), and cases requiring acute treatment of AF in the emergency setting (D) during the first five waves of COVID-19 pandemic compared to the same periods of 2019. The box and whiskers graphs show median, 25th and 75th percentiles, and extreme values. *P < 0.05 compared to elective PM implantations (see Fig. 3). §P < 0.05 compared to elective ablation procedures (see Fig. 3). AF, atrial fibrillation; ANOVA, analysis of variance; CIED, cardiac implantable electronic device; ICD, implantable cardioverter-defibrillator; PM, pacemaker
Participating centers also reported a large reduction in the number of elective ablations during the first wave (median reported reduction of 70%), whereas most of them (60.6%) reported no significant variations during the fifth wave compared to the same period of 2019 (Fig. 3, panel D).
Procedures performed in the emergency setting The majority of participating centers (70.1%) reported a significant reduction in the number of CIED implantations procedures performed in the emergency setting (including temporary and definitive PM implantations for severe, life-threatening bradyarrhythmias) during the first five waves of the COVID-19 pandemic compared to the same periods of 2019. Specifically, a median reduction of 10% was reported during the first wave, whereas no significant variations during the following four waves were reported by the majority of participating centers (51.2, 53.5, 62.2, and 64.4%, respectively) (Fig. 4, panel B).
Similarly, the majority of participating centers (66.1%) reported a significant reduction in the number of ablation procedures performed in the emergency setting (including urgent ablation of an electrical storm, refractory ventricular or supraventricular tachycardias) during the first five pandemic waves compared to the same periods of 2019. Also for these procedures, a median reduction of 10% was reported during the first wave, whereas no significant variations during the following four waves were reported by the majority of participating centers (50.4, 56.7, 59.1, and 60.6%, respectively) (Fig. 4, panel C).
Changes in the number of procedures reported by participating centers during each of the five pandemic waves compared to the same periods in 2019 are reported in detail in Supplementary Table.
The temporal trend in the variations in the number of elective and emergency procedures did not show significant differences between the centers located in hospitals designated to treat COVID-19 patients in all the first five waves of the pandemic (n = 65) compared to the other centers (n = 62) (see Supplementary Figure). Similarly, no significant differences in the temporal trend of centers with an high rate (> 20%) of operators directly involved in the management of COVID-19 patients (n = 63) compared to the other centers (n = 64) was observed.
The COVID-19 pandemic impacted also the total cases of acute pharmacological and non-pharmacological treatment of AF in the emergency setting (including pharmacological rate or rhythm control, and urgent electrical cardioversion). Specifically, a median reduction of 40% was reported during the first wave, with a gradual return to the number of cases treated before the pandemic in subsequent waves (Fig. 4, panel D).
Based on the reported procedure volumes, we estimated that during the first five pandemic waves in the 127 centers that participated in the survey, globally about 9,900 fewer CIEDs had been implanted and about 6,400 fewer ablations had been performed (in both elective and emergency settings) compared to the same periods of 2019.
Other procedures The vast majority of participating centers (94.5%) reported a significant reduction in the number of elective DCC of persistent AF/atrial flutter performed under day-case admission. The greatest reduction was observed during the first wave (median reduction reported of 70%). In the subsequent waves, the extent of the decline gradually decreased. However, at the end of the analyzed period, the number of elective DCC did not return to pre-pandemic values (median reduction of 10%, Fig. 5, panel A).
Variations in the number of elective direct-current cardioversions of persistent AF/atrial flutter performed under day-case admission (A), elective evaluations of patients with syncope (B), new CIED patients enrolled in the remote monitoring program (C) during the first five waves of COVID-19 pandemic compared to the same periods of 2019. The box and whiskers graphs show median, 25th and 75th percentiles, and extreme values. AF, atrial fibrillation; ANOVA, analysis of variance; CIED, cardiac implantable electronic device
The vast majority of participating centers (92.1%) reported a significant reduction in the number of elective evaluations of patients with syncope who required diagnostic procedures during the pandemic. The greatest reduction was observed during the first wave (median reduction of 40%) with a gradual return to pre-pandemic values in subsequent waves (Fig. 5, panel B).
RM of CIEDs All participating centers declared to use RM for follow-up of the CIED patients. COVID-19 pandemic resulted in a significant increase in the use of RM in most participating centers (57.5%). The maximum increase in the number of new CIED patients enrolled in the RM program compared to the same period of 2019 was reported during the first wave (median increase of 40%); during the second wave, a slight increase was reported (median 10%). During the fourth and fifth waves, no significant changes were observed compared to the same periods of 2019 (Fig. 5, panel C).
Discussion
The present survey provides important and novel information that depicts a more comprehensive picture of the impact of the COVID-19 pandemic with the temporal perspective of all the five different waves that characterized the diffusion of the Sars-Cov-2 infection in Italy [15]. First of all, the survey, which involved an important proportion of Italian centers, deeply involved in the provision of care in the field of electrophysiology and pacing showed that many physicians traditionally dedicated to arrhythmias and pacing were directly involved in the management of patients affected by COVID-19 (for full-time or partial-time management of these patients, including direct patient evaluation during consultations). Moreover, this organizational derangement was not confined to the first wave, but continued with a progressive decline, with an important contribution to the care of COVID-19 patients even in the fifth wave.
An important impact of COVID-19 outbreak on cardiac care provision has been reported for the first wave of COVID-19 in various countries [17], but our study expands the evidence of the profound alterations of in-hospital cardiology practice, that involved both staff physicians [14, 18] and fellows in training [19] and that unfortunately was counteracted by a wide range of re-arrangements of health care organization. This survey shows for the first time that the marked reduction in elective procedures of pacemaker, ICD and CRT implants, as well as cardiac ablations, observed immediately after the COVID-19 outbreak, during the first wave [14], more pronounced in Italy as compared to other countries such as Germany [20], had a slow recovery over time and levels of operational activity similar to the same periods in 2019 were actually achieved only during the third or fourth waves, and for elective ablations only during the fifth wave. Although the nature of our study, in the form of a survey addressed to physicians, does not allow to explain such temporal trend, it is possible to hypothesize that it was due to multiple reasons, including the limited propensity of patients to be admitted for both elective procedures and emergencies in hospitals with a large number of beds dedicated to patients affected by COVID-19 [21, 22], as well as the re-organization of care with reduced availability of beds and operators for usual care, particularly in public hospitals [23, 24].
However, it is reassuring to realize that for emergency procedures related to ICD implants for secondary prevention, PM, CRT implantations and urgent ablations, after a 10% reduction of activity during the first wave, the return to the same levels of activity of the pre-pandemic period of occurred in most cases at the time of the second wave, even though with some variability. In other words, the dramatic impact that the first wave of COVID-19 created, in terms of reduced access and efficiency of interventions for cardiac acute events and emergencies, such as cardiac arrests, acute coronary syndromes and bradyarrhythmias [11, 12, 14, 25,26,27] had a period of major disruption during the first and second waves, with the volumes of activities for emergencies restored at the end of the year 2020. It is noteworthy that several patients affected by COVID-19 presented with cardiac arrhythmias or syncope and required pacing or other electrophysiological interventions [28,29,30,31,32,33,34,35].
A field where the COVID-19 pandemic exerted a particularly negative influence is the care of patients with AF. Indeed, both acute care for AF in emergency and elective DCC for achieving rhythm control had not only a marked reduction in the first wave but also a prolonged reduction as compared with the reference of the pre-pandemic period. The mid-term and long-term consequences of this lack of adequate care for AF management implied that the strong recommendations to institute oral anticoagulation in patients at risk of stroke and to apply a rhythm-control strategy when indicated [36, 37] could not be followed, with dramatic consequences on outcomes and specifically on stroke events, as reported in one country analysis related to Denmark [38].
The trend in cardiology activities for elective evaluations of syncope observed during the five waves of COVID-19 showed a pattern quite similar to the trend of AF management, supporting the concept that the diagnostic pathways for important cardiovascular diseases and events were profoundly altered during the pandemic, with consequences that will completely emerge only in the following years [39,40,41,42]. Indeed, the delay in recovery of the full volume of activities for elective procedures observed in this survey could have resulted in a series of risky consequences, including the worsening of patient clinical status, the need for urgent interventions, or the evolution to more severe, even life-threatening, conditions. Finally, we should be able to assess in the next months if the most appropriate target is the level of activities in the year 2019 or an over-reaction due to the increased need for procedures/interventions is needed.
It is noteworthy that an important and proactive consequence of the derangement in care provision caused by the COVID-19 pandemic was the input for widespread implementation of telemedicine, to overcome the difficulties in providing care for chronic diseases through the conventional approach based on in-person visits and checks. The easily achievable implementation of telemedicine during the pandemic was the RM of CIEDs. As known, implanted devices offer the possibility of RM of devices and in many CIEDs also of some variables related to cardiac status and heart failure [43,44,45,46,47]. The results of this survey confirm that during the lockdown period of COVID-19 in Italy there has been a global increase in the use of RM of CIEDs [48], although with a substantial amount of within centers variability, as shown by the observation that the percentage change in the number of new CIED patients enrolled in the RM program ranged from − 20 to + 70% (see Fig. 5, panel C). This technology allowed to safely check thousands of patients with CIEDs, as well as to document a wide range of consequences and reactions to the lockdown [45, 49,50,51]. The complete implementation of RM as a standard of care for the follow-up of CIED patients is currently challenged by many factors including the lack of appropriate reimbursement across Europe [52] and many Italian regions. It appears that in consideration of the reliability of RM concerning the safety of the transmissions and proven ability to anticipate detection of CIED malfunctions, the implementation of RM as a standard of care for CIED follow-up should be fostered, even beyond the emergency of COVID-19 outbreak [48]. Indeed, the number of new patients followed with RM in Italy sharply increased during the first wave, but then the rate of increase in the adoption of RM declined.
Beyond RM of CIEDs, telemedicine with digital, non-implanted devices has a great potential to be useful in several settings [53,54,55,56,57,58] and during COVID-19 there was a trend to fuel the implementation of these tools also in arrhythmia detection and management [59,60,61], even if lack of digital literacy, of frequent occurrence among elderly patients [62], may be an important barrier. Our survey suggests that the care of AF patients could benefit from digital tools/wearables and remote connection, especially in problematic situations, such as the pandemic, even if the organization and preparedness of physicians remain a matter of debate [56, 63].
Study limitations
Overall 127 out of 372 arrhythmia centers operating in Italy took part in the survey (34.1% of the Italian centers) and our findings should be interpreted with caution, as they did not provide an accurate measurement, but simply an estimate of the impact of the first waves of COVID-19 pandemic on the activities of all Italian arrhythmia centers. However, it is noteworthy that the characteristics of the centers that took part in the survey (geographical distribution, number of operators, volume and types of procedures performed) seem to be representative of the current Italian scenario [64,65,66]. In addition, the reduction in cases managed for acute AF during the first wave, as assessed by this survey, is consistent with the actual data derived from the National Registry in Denmark [38].
The volume of activities and procedures of every specific center was self-reported and not objectively defined; however, this is a method that allows a rapid feedback and was chosen for having a general view of COVID-19 pandemic in Italy.
In the questionnaire, participating centers were not asked to report in detail the absolute number of procedures performed during 2019. They were asked to report the percentage change in the number of procedures performed during each of the five pandemic waves compared to the same periods of 2019. Consequently, it was not possible to perform a statistical comparison between the number of procedures performed during the five pandemic waves and the same periods of 2019. This is in line with the characteristics of our study, which is actually a survey.
Since this survey did not collect data on patient's outcome, it was not possible to assess the impact of the reduction in the treatment of arrhythmias caused by the COVID-19 pandemic on the survival and the quality of life of patients, which actually depend on the complex interaction of many factors [50].
Fifteen of the 19 questions of the questionnaire were multiple-choice questions. This type of questionnaire is time-efficient, and responses are easy to code and interpret. On the other hand, the surveys based on multiple-choice questions have some limitations. Respondents are required to choose a response that may not exactly reflect their answer but is conditioned by a pre-conceived simplest of answers to depict the experiences, beliefs, and activities of respondents.
Conclusions
In conclusion, in this nationwide survey involving one-third of the centers involved in cardiac electrophysiology and arrhythmia management in Italy, the dramatic and profound derangement that occurred during the first wave of the COVID-19 pandemic, and that involved all the activities related to cardiac care for arrhythmias (CIED implants, management of AF, including ablations, and evaluation of patients with syncope) was followed by a progressive return to the volume of activities of the pre-pandemic periods. However, different temporal dynamics and some centres' heterogeneity characterized the specific recovery of full activities, especially concerning elective cardioversions for AF and elective evaluation of patients with syncope. The innovative approaches based on telemedicine were largely applied, using RM in patients with CIEDs during the first wave, but full implementation is needed with dedicated pathways and adequate organization.
References
Di Liberto IA, Pilato G, Geraci S, Milazzo D, Vaccaro G, Buccheri S, Caramanno G (2020) Impact on hospital admission of ST-elevation myocardial infarction patients during coronavirus disease 2019 pandemic in an Italian Hospital. J Cardiovasc Med (Hagerstown) 21:722–724
Zuin M, Bilato C, Zuliani G, Roncon L (2020) Italian Vò municipality cohort and COVID-19 epidemiology: The “Framingham” study of the 21st century. Eur J Intern Med 81:95–96
Task Force for the management of COVID-19 of the European Society of Cardiology (2022) European Society of Cardiology guidance for the diagnosis and management of cardiovascular disease during the COVID-19 pandemic: part 1-epidemiology, pathophysiology, and diagnosis. Eur Heart J 43:1033–1058
Zuin M, Rigatelli G, Zuliani G, Bilato C, Zonzin P, Roncon L (2020) Incidence and mortality risk in coronavirus disease 2019 patients complicated by acute cardiac injury: systematic review and meta-analysis. J Cardiovasc Med (Hagerstown) 21:759–764
Romeo F, Calcaterra G, Barilla F, Mehta JL (2020) Coronavirus disease 2019 infection and the cardiovascular system. J Cardiovasc Med (Hagerstown) 21:403–405
Task Force for the management of COVID-19 of the European Society of Cardiology (2022) ESC guidance for the diagnosis and management of cardiovascular disease during the COVID-19 pandemic: part 2-care pathways, treatment, and follow-up. Eur Heart J 43:1059–1103
Ramadan MS, Bertolino L, Marrazzo T, Florio MT, Durante-Mangoni E, The Monaldi Hospital Cardiovascular Infection Study Group (2021) Cardiac complications during the active phase of COVID-19: review of the current evidence. Intern Emerg Med 16:2051–2061
Campanile A, Verdecchia P, Ravera A, Coiro S, Mattei C, Scavelli F, Bearzot L, Cutolo A, Centola M, Carugo S, De Rosa S, Guerra F, Marini M, Perna GP, Indolfi C, Cavallini C (2021) Intensive cardiac care unit admission trends during the COVID-19 outbreak in Italy: a multi-center study. Intern Emerg Med 16:2077–2086
Venturelli A, Vitolo M, Albini A, Boriani G (2021) How did COVID-19 affect medical and cardiology journals? A pandemic in literature. J Cardiovasc Med (Hagerstown) 22:840–847
Vitolo M, Venturelli A, Valenti AC, Boriani G (2022) Impact of COVID-19 in emergency medicine literature: a bibliometric analysis. Intern Emerg Med 17:1229–1233
De Rosa S, Spaccarotella C, Basso C, Calabrò MP, Curcio A, Filardi PP, Mancone M, Mercuro G, Muscoli S, Nodari S, Pedrinelli R, Sinagra G, Indolfi C, Società Italiana di Cardiologia and the CCU Academy investigators group (2020) Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur Heart J 41:2083–2088
Campo G, Fortuna D, Berti E, De Palma R, Pasquale GD, Galvani M, Navazio A, Piovaccari G, Rubboli A, Guardigli G, Galiè N, Boriani G, Tondi S, Ardissino D, Piepoli M, Banchelli F, Santarelli A, Casella G, AMI-Co investigators (2021) In- and out-of-hospital mortality for myocardial infarction during the first wave of the COVID-19 pandemic in Emilia-Romagna, Italy: a population-based observational study. Lancet Reg Health Eur 3:100055
Flori M, Marinucci L, Gabrielli G, Baiocco E, Accardi R, Scalone G, Grossi P, Guerra F (2021) Reduction of acute coronary syndromes during coronavirus disease 2019 global pandemic: data from the Marche region of Italy. J Cardiovasc Med (Hagerstown) 22:350–356
Boriani G, Palmisano P, Guerra F, Bertini M, Zanotto G, Lavalle C, Notarstefano P, Accogli M, Bisignani G, Forleo GB, Landolina M, D'Onofrio A, Ricci R, De Ponti R, AIAC Ricerca Network Investigators (2020) Impact of COVID-19 pandemic on the clinical activities related to arrhythmias and electrophysiology in Italy: results of a survey promoted by AIAC (Italian Association of Arrhythmology and Cardiac Pacing). Intern Emerg Med 15:1445–1456
Data from Italian Civil Protection Department. https://opendatadpc.maps.arcgis.com/apps/dashboards/b0c68bce2cce478eaac82fe38d4138b1. Accessed 23 June 2022
Censimento delle strutture aritmologiche italiane AIAC 2019. https://aiac.it/attivita/censimenti/. Accessed 23 June 2022
Yasmin F, Shujauddin SM, Naeem A, Jabeen A, Shah SMI, Ochani RK, Mohiuddin O, Khan AA, Jalees S, Razzack AA, Salman S, Khan SAK, Mustafa A, Lak HM (2021) Exploring the impact of the COVID-19 pandemic on provision of cardiology services: a scoping review. Rev Cardiovasc Med 22:83–95
Bollmann A, Hohenstein S, Meier-Hellmann A, Kuhlen R, Hindricks G (2020) Emergency hospital admissions and interventional treatments for heart failure and cardiac arrhythmias in Germany during the Covid-19 outbreak: insights from the German-wide Helios hospital network. Eur Heart J Qual Care Clin Outcomes 6:221–222
Strangio A, Leo I, Spaccarotella CAM, Barillà F, Basso C, Calabrò MP, Curcio A, Filardi PP, Mancone M, Mercuro G, Muscoli S, Nodari S, Pedrinelli R, Romeo F, Sinagra G, Indolfi C (2021) Effects of the COVID-19 pandemic on the formation of fellows in training in cardiology. J Cardiovasc Med (Hagerstown) 22:711–715
Schwab JO, Wiese J, Hauser T (2022) The influence of the 2020 COVID-19 pandemic on the implantation rates of cardiac implantable electronic devices in Germany: changes between 2020 Q1–Q3 and 2019 Q1–Q3. Eur Heart J Qual Care Clin Outcomes 8:104–112
Ben-Haim G, Zabatani A, Orion D, Leshem E, Irony A, Katorza E (2021) The Pandemic’s impacts on patients without Covid-19 on multidisciplinary aspects in emergency medicine care. Intern Emerg Med 16:2261–2268
Morello F, Bima P, Ferreri E, Chiarlo M, Balzaretti P, Tirabassi G, Petitti P, Aprà F, Vallino D, Carbone G, Pivetta EE, Lupia E (2021) After the first wave and beyond lockdown: long-lasting changes in emergency department visit number, characteristics, diagnoses, and hospital admissions. Intern Emerg Med 16:1683–1690
Mazzone A, Mumoli N (2020) Reorganizing Italian Internal Medicine wards for COVID 19. Eur J Intern Med 77:143
Rubin GA, Biviano A, Dizon J, Yarmohammadi H, Ehlert F, Saluja D, Rubin DA, Morrow JP, Waase M, Berman J, Kushnir A, Abrams MP, Garan H, Wan EY (2020) Performance of electrophysiology procedures at an academic medical center amidst the 2020 coronavirus (COVID-19) pandemic. J Cardiovasc Electrophysiol 31:1249–1254
Fileti L, Vecchio S, Moretti C, Reggi A, Aquilina M, Balducelli M, Santarelli A, Grosseto D, Piovaccari G, Rubboli A (2020) Impact of the COVID-19 pandemic on coronary invasive procedures at two Italian high-volume referral centers. J Cardiovasc Med (Hagerstown) 21:869–873
Legutko J, Niewiara Ł, Bartuś S, Dobrzycki S, Gąsior M, Gierlotka M, Kochman J, Lesiak M, Matysek J, Ochała A, Pawłowski T, Gil R, Witkowski A (2020) Decline in the number of coronary angiography and percutaneous coronary intervention procedures in patients with acute myocardial infarction in Poland during the coronavirus disease 2019 pandemic. Kardiol Pol 78:574–576
Russo V, Pafundi PC, Rapacciuolo A, de Divitiis M, Volpicelli M, Ruocco A, Rago A, Uran C, Nappi F, Attena E, Chianese R, Esposito F, Del Giorno G, D’Andrea A, Ducceschi V, Russo G, Ammendola E, Carbone A, Covino G, Manzo G, Montella GM, Nigro G, D’Onofrio A (2021) Cardiac pacing procedures during coronavirus disease 2019 lockdown in Southern Italy: insights from Campania Region. J Cardiovasc Med (Hagerstown) 22:857–859
Coromilas EJ, Kochav S, Goldenthal I, Biviano A, Garan H, Goldbarg S, Kim JH, Yeo I, Tracy C, Ayanian S, Akar J, Singh A, Jain S, Zimerman L, Pimentel M, Osswald S, Twerenbold R, Schaerli N, Crotti L, Fabbri D, Parati G, Li Y, Atienza F, Zatarain E, Tse G, Leung KSK, Guevara-Valdivia ME, Rivera-Santiago CA, Soejima K, De Filippo P, Ferrari P, Malanchini G, Kanagaratnam P, Khawaja S, Mikhail GW, Scanavacca M, Abrahão Hajjar L, Rizerio B, Sacilotto L, Mollazadeh R, Eslami M, Laleh Far V, Mattioli AV, Boriani G, Migliore F, Cipriani A, Donato F, Compagnucci P, Casella M, Dello Russo A, Coromilas J, Aboyme A, O’Brien CG, Rodriguez F, Wang PJ, Naniwadekar A, Moey M, Kow CS, Cheah WK, Auricchio A, Conte G, Hwang J, Han S, Lazzerini PE, Franchi F, Santoro A, Capecchi PL, Joglar JA, Rosenblatt AG, Zardini M, Bricoli S, Bonura R, Echarte-Morales J, Benito-González T, Minguito-Carazo C, Fernández-Vázquez F, Wan EY (2021) Worldwide Survey of COVID-19-Associated Arrhythmias. Circ Arrhythm Electrophysiol 14:e009458
Tovia-Brodie O, Rav Acha M, Belhassen B, Gasperetti A, Schiavone M, Forleo GB, Guevara-Valdivia ME, Ruiz DV, Lellouche N, Hamon D, Castagno D, Bellettini M, De Ferrari GM, Laredo M, Carvès JB, Ignatiuk B, Pasquetto G, De Filippo P, Malanchini G, Pavri BB, Raphael C, Rivetti L, Mantovan R, Chinitz J, Harding M, Boriani G, Casali E, Wan EY, Biviano A, Macias C, Havranek S, Lazzerini PE, Canu AM, Zardini M, Conte G, Cano Ó, Casella M, Rudic B, Omelchenko A, Mathuria N, Upadhyay GA, Danon A, Schwartz AL, Maury P, Nakahara S, Goldenberg G, Schaerli N, Bereza S, Auricchio A, Glikson M, Michowitz Y (2022) Implantation of cardiac electronic devices in active COVID-19 patients: Results from an international survey. Heart Rhythm 19:206–216
Denegri A, Pezzuto G, D’Arienzo M, Morelli M, Savorani F, Cappello CG, Luciani A, Boriani G (2021) Clinical and electrocardiographic characteristics at admission of COVID-19/SARS-CoV2 pneumonia infection. Intern Emerg Med 16:1451–1456
Inciardi RM, Adamo M, Lupi L, Cani DS, Di Pasquale M, Tomasoni D, Italia L, Zaccone G, Tedino C, Fabbricatore D, Curnis A, Faggiano P, Gorga E, Lombardi CM, Milesi G, Vizzardi E, Volpini M, Nodari S, Specchia C, Maroldi R, Bezzi M, Metra M (2020) Characteristics and outcomes of patients hospitalized for COVID-19 and cardiac disease in Northern Italy. Eur Heart J 41(19):1821–1829
Lip GYH, Genaidy A, Tran G, Marroquin P, Estes C (2021) Incident atrial fibrillation and its risk prediction in patients developing COVID-19: a machine learning based algorithm approach. Eur J Intern Med 91:53–58
Angeli F, Spanevello A, De Ponti R, Visca D, Marazzato J, Palmiotto G, Feci D, Reboldi G, Fabbri LM, Verdecchia P (2020) Electrocardiographic features of patients with COVID-19 pneumonia. Eur J Intern Med 78:101–106
Ghio S, Baldi E, Vicentini A, Lenti MV, Di Sabatino A, Di Matteo A, Zuccaro V, Piloni D, Corsico A, Gnecchi M, Speciale F, Sabena A, Oltrona Visconti L, Perlini S, San Matteo COVID Cardiac Injury Task Force (2020) Cardiac involvement at presentation in patients hospitalized with COVID-19 and their outcome in a tertiary referral hospital in Northern Italy. Intern Emerg Med 15:1457–1465
Ceriani E, Marceca A, Lanfranchi A, De Vita S, Schiavon R, Casella F, Torzillo D, Del Medico M, Ruggiero D, Barosi A, Cogliati C (2021) Early echocardiographic findings in patients hospitalized for COVID-19 pneumonia: a prospective, single center study. Intern Emerg Med 16:2173–2180
Hindricks G, Potpara T, Dagres N, Arbelo E, Bax JJ, Blomström-Lundqvist C, Boriani G, Castella M, Dan GA, Dilaveris PE, Fauchier L, Filippatos G, Kalman JM, La Meir M, Lane DA, Lebeau JP, Lettino M, Lip GYH, Pinto FJ, Thomas GN, Valgimigli M, Van Gelder IC, Van Putte BP, Watkins CL; ESC Scientific Document Group (2021) 2020 ESC guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J 42:373–498
Boriani G, Vitolo M, Lane DA, Potpara TS, Lip GY (2021) Beyond the 2020 guidelines on atrial fibrillation of the European society of cardiology. Eur J Intern Med 86:1–11
Holt A, Gislason GH, Schou M, Zareini B, Biering-Sørensen T, Phelps M, Kragholm K, Andersson C, Fosbøl EL, Hansen ML, Gerds TA, Køber L, Torp-Pedersen C, Lamberts M (2020) New-onset atrial fibrillation: incidence, characteristics, and related events following a national COVID-19 lockdown of 5.6 million people. Eur Heart J 41:3072–3079
Task Force for the management of COVID-19 of the European Society of Cardiology (2022) European Society of Cardiology guidance for the diagnosis and management of cardiovascular disease during the COVID-19 pandemic: part 1-epidemiology, pathophysiology, and diagnosis. Eur Heart J 43:1154–1156
Task Force for the management of COVID-19 of the European Society of Cardiology (2022) ESC guidance for the diagnosis and management of cardiovascular disease during the COVID-19 pandemic: part 2-care pathways, treatment, and follow-up. Int J Environ Res Public Health 18:9194
Henry TD, Kereiakes DJ (2022) The direct and indirect effects of the COVID-19 pandemic on cardiovascular disease throughout the world. Eur Heart J 43:1154–1156
Russo V, Boggian G, Bolognesi MG, Carretta DM, Cencetti S, De Laura D, Hrovatin E, Pastori P, Tomaselli C, Parente E, Rafanelli M, Ungar A, On Behalf Of Covid-Gimsi Study Group (2021) The impact of COVID-19 outbreak on syncope units activities in Italy: a report from the Italian Multidisciplinary Working Group on Syncope (GIMSI). Int J Environ Res Public Health 18:9194
Boriani G, Diemberger I, Martignani C, Biffi M, Valzania C, Bertini M, Domenichini G, Saporito D, Ziacchi M, Branzi A (2008) Telecardiology and remote monitoring of implanted electrical devices: the potential for fresh clinical care perspectives. J Gen Intern Med 23(Suppl 1):73–77
Imberti JF, Tosetti A, Mei DA, Maisano A, Boriani G (2021) Remote monitoring and telemedicine in heart failure: implementation and benefits. Curr Cardiol Rep 23:55
Diemberger I, Vicentini A, Cattafi G, Ziacchi M, Iacopino S, Morani G, Pisanò E, Molon G, Giovannini T, Dello Russo A, Boriani G, Bertaglia E, Biffi M, Bongiorni MG, Rordorf R, Zucchelli G (2021) The impact of COVID-19 pandemic and lockdown restrictions on cardiac implantable device recipients with remote monitoring. J Clin Med 10:5626
Boriani G, Da Costa A, Quesada A, Ricci RP, Favale S, Boscolo G, Clementy N, Amori V, Mangoni di S Stefano L, Burri H, MORE-CARE Study Investigators (2017) Effects of remote monitoring on clinical outcomes and use of healthcare resources in heart failure patients with biventricular defibrillators: results of the MORE-CARE multicentre randomized controlled trial. Eur J Heart Fail 19:416–425
Maines M, Tomasi G, Moggio P, Peruzza F, Catanzariti D, Angheben C, Simoncelli M, Degiampietro M, Piffer L, Valsecchi S, Del Greco M (2020) Implementation of remote follow-up of cardiac implantable electronic devices in clinical practice: organizational implications and resource consumption. J Cardiovasc Med (Hagerstown) 21:648–653
Maines M, Palmisano P, Del Greco M, Melissano D, De Bonis S, Baccillieri S, Zanotto G, D’Onofrio A, Ricci RP, De Ponti R, Boriani G (2021) Impact of COVID-19 pandemic on remote monitoring of cardiac implantable electronic devices in Italy: results of a survey promoted by AIAC (Italian Association of Arrhythmology and Cardiac Pacing). J Clin Med 10:4086
O’Shea CJ, Thomas G, Middeldorp ME, Harper C, Elliott AD, Ray N, Lau DH, Campbell K, Sanders P (2021) Ventricular arrhythmia burden during the coronavirus disease 2019 (COVID-19) pandemic. Eur Heart J 42:520–528
Boriani G, Vitolo M (2021) COVID-19 pandemic: complex interactions with the arrhythmic profile and the clinical course of patients with cardiovascular disease. Eur Heart J 42(5):529–532
Bontempi L, Aboelhassan M, Cerini M, Salghetti F, Fabbricatore D, Maiolo V, Freda L, Giacopelli D, Curnis A (2021) Could Home Monitoring parameters provide information about the impact of the pandemic period on CIED patients? A comparison between 2019 and 2020. J Cardiovasc Med (Hagerstown) 22(7):606–608
Boriani G, Burri H, Svennberg E, Imberti JF, Merino JL, Leclercq C (2022) Current status of reimbursement practices for remote monitoring of cardiac implantable electrical devices across Europe euac118. https://doi.org/10.1093/europace/euac118(Online ahead of print)
Bonini N, Vitolo M, Imberti JF, Proietti M, Romiti GF, Boriani G, Paaske Johnsen S, Guo Y, Lip GYH (2022) Mobile health technology in atrial fibrillation. Expert Rev Med Dev 19:327–340
Svennberg E, Tjong F, Goette A, Akoum N, Di Biase L, Bordachar P, Boriani G, Burri H, Conte G, Deharo JC, Deneke T, Drossart I, Duncker D, Han JK, Heidbuchel H, Jais P, de Oliviera Figueiredo MJ, Linz D, Lip GYH, Malaczynska-Rajpold K, Márquez M, Ploem C, Soejima K, Stiles MK, Wierda E, Vernooy K, Leclercq C, Meyer C, Pisani C, Pak HN, Gupta D, Pürerfellner H, Crijns HJGM, Chavez EA, Willems S, Waldmann V, Dekker L, Wan E, Kavoor P, Turagam MK, Sinner M (2022) How to use digital devices to detect and manage arrhythmias: an EHRA practical guide. Europace 24:979–1005
Guo Y, Guo J, Shi X, Yao Y, Sun Y, Xia Y, Yu B, Liu T, Chen Y, Lip GYH, mAF-App II Trial investigators (2020) Mobile health technology-supported atrial fibrillation screening and integrated care: a report from the mAFA-II trial long-term extension cohort. Eur J Intern Med 82:105–111
Freedman B, Camm J, Calkins H, Healey JS, Rosenqvist M, Wang J, Albert CM, Anderson CS, Antoniou S, Benjamin EJ, Boriani G, Brachmann J, Brandes A, Chao TF, Conen D, Engdahl J, Fauchier L, Fitzmaurice DA, Friberg L, Gersh BJ, Gladstone DJ, Glotzer TV, Gwynne K, Hankey GJ, Harbison J, Hillis GS, Hills MT, Kamel H, Kirchhof P, Kowey PR, Krieger D, Lee VWY, Levin LÅ, Lip GYH, Lobban T, Lowres N, Mairesse GH, Martinez C, Neubeck L, Orchard J, Piccini JP, Poppe K, Potpara TS, Puererfellner H, Rienstra M, Sandhu RK, Schnabel RB, Siu CW, Steinhubl S, Svendsen JH, Svennberg E, Themistoclakis S, Tieleman RG, Turakhia MP, Tveit A, Uittenbogaart SB, Van Gelder IC, Verma A, Wachter R, Yan BP, AF-Screen Collaborators (2017) Screening for atrial fibrillation: a report of the AF-SCREEN international collaboration. Circulation 135:1851–1867
Boriani G, Palmisano P, Malavasi VL, Fantecchi E, Vitolo M, Bonini N, Imberti JF, Valenti AC, Schnabel RB, Freedman B (2021) Clinical factors associated with atrial fibrillation detection on single-time point screening using a hand-held single-lead ECG device. J Clin Med 10(4):729
Sgreccia D, Mauro E, Vitolo M, Manicardi M, Valenti AC, Imberti JF, Ziacchi M, Boriani G (2022) Implantable cardioverter defibrillators and devices for cardiac resynchronization therapy: what perspective for patients’ apps combined with remote monitoring? Expert Rev Med Devices 19:155–160
Mattioli AV, Cossarizza A, Boriani G (2020) COVID-19 pandemic: usefulness of telemedicine in management of arrhythmias in elderly people. J Geriatr Cardiol 17:593–596
Rigante D (2021) Telemedicine and the risk of overshadowing children with Kawasaki disease in a worldwide coronavirus pandemic climate. Intern Emerg Med 16:2027–2028
Garattini L, Badinella Martini M, Mannucci PM (2021) Improving primary care in Europe beyond COVID-19: from telemedicine to organizational reforms. Intern Emerg Med 16:255–258
Boriani G, Maisano A, Bonini N, Albini A, Imberti JF, Venturelli A, Menozzi M, Ziveri V, Morgante V, Camaioni G, Passiatore M, De Mitri G, Nanni G, Girolami D, Fontanesi R, Siena V, Sgreccia D, Malavasi VL, Valenti AC, Vitolo M (2021) Digital literacy as a potential barrier to implementation of cardiology tele-visits after COVID-19 pandemic: the INFO-COVID survey. J Geriatr Cardiol 18:739–747
Boriani G, Schnabel RB, Healey JS, Lopes RD, Verbiest-van Gurp N, Lobban T, Camm JA, Freedman B (2020) Consumer-led screening for atrial fibrillation using consumer-facing wearables, devices and apps: A survey of health care professionals by AF-SCREEN international collaboration. Eur J Intern Med 82:97–104
Proclemer A, Zecchin M, Zanotto G, Gregori D, D’Onofrio A, Ricci RP, De Ponti R (2022) Registro Italiano Pacemaker e Defibrillatori – Associazione Italiana di Aritmologia e Cardiostimolazione – Report 2020 [The Pacemaker and Implantable Cardioverter-Defibrillator Registry of the Italian Association of Arrhythmology and Cardiac Pacing-Report 2020]. G Ital Cardiol (Rome) 23:309–313
Stabile G, Guerra F, Tola G, Bertaglia E, Palmisano P, Berisso MZ, Soldati E, Bisignani G, Forleo GB, Zanotto G, Landolina M, Boriani G, D’Onofrio A, De Ponti R, Registro RRP, Ablazioni I (2019) Associazione Italiana di Aritmologia e Cardiostimolazione [2019 Catheter Ablation Registry of the Italian Association of Arrhythmology and Cardiac Pacing]. G Ital Cardiol (Rome) 2021(22):1034–1037
Stabile G, Bertaglia E, Guerra F, Palmisano P, Zoni Berisso M, Soldati E, Bisignani G, Forleo GB, Zanotto G, Landolina M, Boriani G, D'Onofrio A, De Ponti R, Ricci RP, Associazione Italiana di Aritmologia e Cardiostimolazione (AIAC) (2021) Organization and procedures in contemporary catheter ablation centres: data from the 2018 Italian Catheter Ablation Registry. J Cardiovasc Med (Hagerstown) 22:631–636
Acknowledgements
We acknowledge the AIAC Ricerca Investigators who participated in this survey: Abruzzo: Luise R, Ospedale San Salvatore, L'Aquila; Calabria: De Bonis S, Ospedale Civile Ferrari, Castrovillari; Pangallo A, Grande Ospedale Metropolitano di Reggio Calabria, Reggio Calabria; Talarico A, SC Cardiologia. PO Annunziata, Cosenza; Maglia G, Aspromonte V, Azienda Ospedaliera Pugliese-Ciaccio, Catanzaro; Campania: Nigro G, Università degli Studi della Campania L. Vanvitelli - AORN dei Colli - Ospedale Monaldi, Napoli; Bianchi V, AORN dei Colli - Ospedale Monaldi, Napoli; Rapacciuolo A, AOU Federico II, Napoli; Ammendola E, Ospedale Monaldi, Napoli; Solimene F, Stabile G, Clinica Montevergine, Mercogliano (Avellino); Emilia Romagna: Biffi M, Ziacchi M, Policlinico S.Orsola Malpighi, Bologna; Saporito D, Ospedale Infermi - ASL Romagna, Rimini; Casali E, Turco V, Malavasi VL, Vitolo M, Imberti JF, Policlinico di Modena, Modena; Bertini M, Arcispedale S. Anna, Ferrara; Zardini M, Placci A, AOU Parma, Parma; Quartieri F, Bottoni N, Aricispedale Santa Maria Nuova, Reggio Emilia; Carinci V, Barbato G, Ospedale Maggiore - AUSL Città di Bologna, Bologna; De Maria E, Borghi A, Ospedale B Ramazzini, Carpi, Modena; Bronzetti G, Cardiologia Pediatrica, IRCSS Azienda Ospedaliera Universitaria di Bologna; Tomasi C, Ospedale S Maria delle Croci, AUSL della Romagna, Ravenna; Boggian G, Ospedale di Bentivoglio, Bologna; Virzì S, Sassone B, Ospedale S.S. Annunziata, Cento (Ferrara); Corzani A, Sabbatani P, Ospedale Bufalini, Cesena; Pastori P, Ospedale di Fidenza, Fidenza (Parma); Lazio: Ciccaglioni A, Policlinico Universitario Umberto I, Roma; Adamo F, Scaccia A, Spampinato A, Villa Tiberia Hospital, Roma; Patruno N, Ospedale dei Castelli, Ariccia (Roma); Biscione F, Ospedale Santo Spirito, Roma; Cinti C, CdC S. Anna Policlinico Città di Pomezia, Pomezia (Roma); Pignalberi C, PO San Filippo Neri, Roma; Calò L, Policlinico Casilino, Roma; Tancredi M, Di Belardino N, Ospedali riuniti Anzio-Nettuno, Anzio (Latina); Ricciardi D, Policlinico Campus Bio-Medico, Roma; Cauti F, Rossi P, Aritmologia San Giovanni Calibita Fatebenefratelli Isola Tiberina Roma, Roma; Cardinale M, Azienda Ospedaliera San Giovanni Addolorata, Roma; Ansalone G, Ospedale Madre Giuseppina Vannini, Istituto Figlie di San Camillo, Roma; Narducci ML, Pelargonio G, Policlinico Gemelli, Roma; Silvetti M, Drago F, Ospedale Pediatrico Bambino Gesù, Palidoro (Roma); Santini L, Ospedale GB Grassi, Asl Roma 3, Roma; Liguria: Pentimalli F, Ospedale San Paolo, Savona; Lombardia: Pepi P, ASST-Mantova "Carlo Poma", Mantova; Caravati F, Ospedale di Circolo e Fondazione Macchi, Varese; Taravelli E, Ospedale Maggiore Crema, Crema; Belotti G, UOS Elettrofisiologia, Treviglio (Bergamo); Rordorf R, IRCCS Policlinico S.Matteo, Pavia; Mazzone P, Della Bella P, Ospedale San Raffaele di Milano; Rossi S, Canevese LF, Ospedale di Saronno - ASST Valle Olona; Cilloni S, Ospedale Predabissi, Vizzolo Predabissi (Milano); Doni LA, ASST Sette Laghi P.O.U. Ospedale di Circolo e Fondazione Macchi, Varese; Vergara P, Baroni M, Perna E, ASST Grande Ospedale Metropolitano Niguarda, Milano; Gardini A, Istituto Clinico S. Anna, Brescia; Negro R, ASST PAVIA Ospedale civile di Vigevano, Vigevano; Perego GB, Istituto Auxologico Italiano IRCCS Ospedale San Luca, Milano; Curnis A, Arabia G, Spedali Civili di Brescia, Brescia; Marche: Dello Russo A, Azienda Ospedaliera universitaria Ospedali Riuniti Ancona, Ancona; Marchese P, ASUR-Area vasta 5; Piemonte: Dell'Era G, AOU Maggiore della Carità, Novara; Occhetta E, AO Sant'Andrea, Vercelli; Pizzetti F, Santo Spirito, Casale Monferrato; Amellone C, Giammaria M, Cardiologia Ospedale Maria Vittoria, Torino; Devecchi C, P.O. SS. Pietro e Paolo Borgosesia, Vercelli; Coppolino A, Ospedale SS Annunziata, Savigliano; Tommasi S, Ospedale San Biagio, Domodossola; Anselmino M, Ospedale Molinette, Torino; Puglia: Coluccia G, Guido A, Azienda Ospedaliera "Card. Giovann Panico", Tricase; Rillo M, Palamà Z, CDC Villa Verde, Taranto; Luzzi G, Ospedale SS Annunziata, Taranto; Pellegrino PL, Policlinico Riuniti di Foggia, Foggia; Grimaldi M, Ospedale Miulli, Acquaviva delle Fonti (Bari); Grandinetti G, Mater Dei, Bari; Vilei E, Ospedale "Veris Delli Ponti", Scorrano (Lecce); Potenza D, Ospedale Casa Sollievo della Sofferenza, San Giovanni Rotondo (Foggia); Scicchitano P, P.O. "F. Perinei", Altamura (Bari); Favale S, Santobuono VE, Azienda Ospedaliero Universitaria Policlinico di Bari, Bari; Sai R, Ospedale Sacro Cuore di Gesù, Gallipoli (Lecce); Melissano D, Ospedale Francesco Ferrari, Casarano, Lecce; Candida TR, Bonfantino VM, P.O. Di Venere UTIC-Cardiologia, Bari; Di Canda D, Anthea Hospital, Bari; Gianfrancesco D, Ospedale Bonomo Andria, Andria; Carretta D, U.O. Cardiologia Ospedaliera A.O.U. Consorziale Policlinico di Bari; Pisanò ECL, Ospedale "Vito Fazzi" ASL Lecce, Lecce; Medico A, Ospedale Perrino, Brindisi; Giaccari R, Ospedale Dario Camberlingo, Francavilla Fontana (Brindisi); Sardegna: Aste R, Murgia C, Ospedale Sirai Carbonia; Nissardi V, Clinica Cardiologica-UTIC - Policlinico "D. Casula", Monserrato, Cagliari; Sanna GD, Azienda Ospedaliero - Universitaria di Sassari, Sassari; Sicilia: Firetto G, Crea P, AOU G. Martino, Messina; Ciotta E, Ospedale di Sciacca, Sciacca; Sgarito G, ARNAS Civico, Palermo; Caramanno G, PO San Giovanni di Dio, Agrigento; Ciaramitaro G, Policlinco P. Giaccone, Palermo; Faraci A, Policlinico di Palermo, Palermo; Fasheri A, O.S.A. Abate, Trapani; Di Gregorio L, Clinica Orestano, Palermo; Campsi G, Ospedale Giovanni Paolo II, Ragusa; Muscio G, Ospedale Umberto I, Siracura; Giannola G, Fondazione Istituto G. Giglio, Cefalù; Toscana: Padeletti M, Ospedale del Mugello, Borgo san Lorenzo (Firenze); Del Rosso A, Ospedale San Giuseppe, Empoli; Notarstefano P, Nesti M, PO San Donato, Arezzo; Miracapillo G, Ospedale Misericordia, Grosseto; Giovannini T, Ospedale S. Stefano, Prato; Pieragnoli P, Ospedale Careggi, Firenze; Trentino Alto Adige: Rauhe W, Ospedale Regionale di Bolzano, Bolzano; Marini M, Guarracini F, Ospedale S. Chiara, Trento; Umbria: Ridarelli M, Presidio Ospedaliero Gubbio, Gualdo Tadino; Fedeli F, Ospedale Città di Castello - USL Umbria 1, Città di Castello; Mazza A, Ospedale S. Maria della Stella, Orvieto; Zingarini G, Ospedale S. Maria della Misericordia, Perugia; Andreoli C, Ospedale S.G. Battista, Foligno; Carreras G, Azienda Ospedaliera Santa Maria di Terni, Terni; Veneto: Zorzi A, Ospedale Fra Castoro, San Bonifacio (Verona); Zanotto G, Ospedale "Mater Salutis", Legnago (Verona); Rossillo A, Ospedale San Bortolo, Vicenza; Ignatuk B, Ospedali Riuniti Padova Sud, Monselice; Zerbo F, Ospedale Civile di Mirano, Mirano (Venezia); Molon G, IRCCS S. Cuore Don Calabria - Negrar (Verona); Fantinel M, Ospedale di Feltre, Feltre; Zanon F, Marcantoni L, Ospedale Santa Maria della Misericordia, Rovigo; Zadro M, ASL 3 Bassano Del Grappa; Bevilacqua M, Ospedale della Navicella di Chioggia, Chioggia.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
G Boriani: small speaker fees from Bayer, Boston, Boehringer Ingelheim, and Daiichi-Sankyo. F Guerra: small speaker fees from Bayer, Bristol-Meyers-Squibb, Boston, Boehringer-Ingelheim, Daiichi-Sankyo, and Zoll. M Bertini: small speaker fees from Boston Scientific, Abbott, Boehringer Ingelheim, and Bayer. M Landolina: modest speaker fees from Bayer, Boehringer Ingelheim, Boston Scientific, LivaNova, Medtronic, and Pfizer. RP Ricci: small speaker fees by Boston e Biotronik; advisory board modest fees by Dompé. R De Ponti: lecture fees from Biosense Webster and Biotronik. P Palmisano: small speaker fees from Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, Medtronic. Novartis and personal fees from Proctorship agreement with Abbott, Medtronic, Biotronik, and Boston Scientific. No conflicts of interest were reported by the other authors.
Human and animal rights
The study procedures were in accordance with the ethical standards of the latest Helsinki declaration.
Informed consent
All the participants provided written consent for their participation in this survey at the time of online data collection. Due to the anonymous and voluntary nature of the study, no identifying information about participants was mandatory for inclusion.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The list of collaborators of AIAC Ricerca Network Investigators is reported in the Acknowledgements.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Boriani, G., Guerra, F., De Ponti, R. et al. Five waves of COVID-19 pandemic in Italy: results of a national survey evaluating the impact on activities related to arrhythmias, pacing, and electrophysiology promoted by AIAC (Italian Association of Arrhythmology and Cardiac Pacing). Intern Emerg Med 18, 137–149 (2023). https://doi.org/10.1007/s11739-022-03140-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-022-03140-4