Abstract
The relationship between albumin corrected anion gap (ACAG) and mortality in acute kidney injury (AKI) patients who received continuous renal replacement therapy (CRRT) has not been investigated in any previous studies. This study aimed to investigate the relationship between ACAG at CRRT initiation and all-cause mortality among these patients in the intensive care unit (ICU). Patients diagnosed with AKI and treated with CRRT in the ICU from the Medical Information Mart for Intensive Care-IV version 1.0 (MIMIC IV) database and Huzhou Central Hospital were retrospectively enrolled. Participants were divided into two groups: the normal ACAG group (12–20 mmol/L) and high ACAG group (> 20 mmol/L). The Kaplan–Meier method and log-rank test were used to compare the survival rate between the two groups. Restricted cubic spine (RCS) and Cox proportional-hazards models were utilized to analyze the relationship between ACAG at CRRT initiation and ICU all-cause mortality of these patients. A total of 708 patients met the inclusion criteria in the study. The all-cause mortality of these patients during ICU hospitalization was 41.95%. Patients in the high ACAG group exhibited significantly higher ICU all-cause mortality rate than patients in the normal ACAG group (all P < 0.001). The Kaplan–Meier survival curves showed that the normal ACAG group had a higher ICU cumulative survival rate than the high ACAG group (log-rank test, χ12 = 13.620, χ22 = 12.460, both P < 0.001). In the multivariate COX regression analyses, patients with higher ACAG (> 20 mmol/L) levels at the time of CRRT initiation in the MIMIC IV database and Huzhou Central Hospital were significantly correlated with ICU all-cause mortality after adjusting multiple potential confounding factors with hazard ratios of 2.852 (95% CI 1.718–4.734) and 2.637(95% CI 1.584–4.389), respectively. In critically AKI patients who undergo CRRT, higher ACAG (> 20 mmol/L) level at the initiation of CRRT was significantly correlated with ICU all-cause mortality. Therefore, clinicians should pay more attention to those patients with a higher ACAG value.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute kidney injury (AKI), characterized by a rapid weakening of kidney function, is a complex clinical disorder that carries a high societal, economic, and personal burden worldwide [1, 2]. Moreover, AKI is one of the most common reasons for an intensive care unit (ICU) admission and affects 33–66% of adult critically ill patients [3].
Generally, continuous renal replacement therapy (CRRT) is one of the most common interventions for AKI patients provided by intensivists in the ICU setting [4]. Even with medical advances, the mortality rate of AKI patients remains high, and there is currently no specific treatment that can reverse the progression of this disease [5]. Besides, critically ill patients with AKI who require CRRT have a high mortality rate [6]. Given the severity of AKI patients who need CRRT, it is necessary and important to have a way to predict the prognosis for these patients.
Acid–base disorders, especially for metabolic acidosis, are recognized as a frequent problem for critically ill patients and are associated with morbidity and mortality [7]. Generally, anion gap (AG), an indicator that reflects the unmeasured anion concentration, is applied to detect and evaluate the presence and severity of metabolic acidosis. However, because the albumin molecule carries a net negative charge, an increase or decrease in its concentration can affect the result of AG [8]. Hypoproteinemia, indeed, is very common in critically ill patients. Moreover, previous studies reported that hypoalbuminemia at the initiation of CRRT [9], as well as the dynamic changes of albumin during CRRT [10], are important risk factors for poor prognosis in AKI patients. Therefore, the formula of calculating the albumin corrected anion gap (ACAG) is described by Figge J et al. in 1998 to correct the AG for fluctuations in the albumin concentration [11, 12]. Prior studies have shown an association between elevated ACAG levels and poor outcomes of critically ill patients, such as sepsis [13] and cardiopulmonary arrest [14] etc.
To our knowledge, however, there have been no reports concerning the correlation between ACAG level and their prognosis in AKI patients who requires CRRT. We therefore initiated this study to determine whether there is an association between ACAG levels at the initiation of CRRT treatment and mortality among these patients.
Materials and methods
Source of data
The Medical Information Mart for Intensive Care-IV (MIMIC-IV, version 1.0) database is an openly accessible critical care database, and it provided the data with pre-existing institutional review board approval. This database contained data of 76,540 ICU admissions between 2008 and 2019 at the Beth Israel Deaconess Medical Center in Boston. One author was approved to exploit data from this database after completed the online course and examination (ZL, certification number: 36142713). Besides, Huzhou Central Hospital is a 1500-bed urban teaching hospital with an ICU census of around 900 annually, and the other part of our dataset were collected from the electronic hospitalization databases of this hospital. Our study was conducted according to the Declaration of Helsinki and approved by the Ethics Committee of Huzhou Central Hospital (Approval no: 202203021-01). Owing to the retrospective nature of this study, patient’s consent was not required. This study was a retrospective observational study, and it is reported based on the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.
Study population
Adult patients diagnosed with AKI and treated with CRRT in the ICU from the MIMIC-IV database (America, from 2008 to 2019) and Huzhou Central Hospital (China, from July 2019 to March 2022) were retrospectively enrolled. Patients were included if they fulfilled the Kidney Disease: Improving Global Outcomes (KDIGO) criteria for AKI in the first 7 day of their ICU admission. The AKI severity stage was also determined by the KDIGO guideline. If the patients had multiple ICU stay records, we only took the first ICU admissions. The exclusion criteria were the following: (1) age < 18 years, (2) end-stage renal disease, (3) discharged within 24 h after being admitted to ICU, (4) patients with missing data or inadequate information (such as AG, albumin, etc.).
Study variables
Structured query language with PostgreSQL 10.13 was used for acquiring the data from the MIMIC-IV database. For each patient, we collected the demographics, clinical characteristics, comorbidities at the time of ICU admission, and laboratory values were collected at the time of CRRT initiation (detailed information is given in Table 1).
The normal reference value of AG in the MIMIC-IV database and the data from our hospital ranged from 8.00 to 20.00 mmol/l and 8.00 to 16.00 mmol/l, respectively. The ACAG was calculated with the following formula: AG (mmol/l) = (sodium + potassium)− (chloride + bicarbonate); ACAG = AG + {4.4-[albumin(g/dl)]}×2.5. The participants were divided into the survival group and the death group based on their survival during the ICU stay. Further, the study population was split into 2 groups based on their ACAG level using criteria from previous literature [15]: the normal ACAG group (ACAG 12–20 mmol/L) and high ACAG group (ACAG > 20 mmol/L). The primary endpoint was ICU all-cause mortality.
Statistical analysis
Continuous data were expressed as mean ± standard deviation (SD) for normal distributions or median (interquartile range, IQR) for skewed distributions. Categorical data were described as numbers (%). The data were analyzed with one-sample t test, Wilcoxon rank-sum test or Chi-squared test as appropriate. Variables with a P value < 0.20 in the univariate analysis were included in the multivariate regression analysis. Kaplan–Meier curve was established to visualize differences in survival and was compared using the log-rank test. Restricted cubic spine (RCS) was utilized to calculate the correlation between ACAG and the risk of ICU all-cause mortality. Simultaneously, the association of ACAG with ICU all-cause mortality was determined using Cox proportional-hazards models and presented as hazard ratio (HR) with 95% confidence interval (CI). Stata 14.0 software and R language were used for all analyses. A two-sided P valueless than 0.05 was regarded as statistically significant.
Results
Study population
The flowchart of included study population was displayed in Fig. 1. During the study period, a total of 452 and 256 eligible patients were ultimately enrolled from the MIMIC-IV database and Huzhou Central Hospital, respectively. The average age of patients from the MIMIC-IV database and our hospital were 59.69 ± 15.26 years and 66.74 ± 16.01 years. In both study populations, the SOFA score, anion gap, ACAG, and the incidence rate of cardiac arrest in the non-survivors group were significantly higher than those in the survivors group, while the serum creatinine level and length of ICU stay in the survivor group were higher than those in the non-survivors group (all P < 0.05). The baseline characteristics of the patients included are listed in Table 1.
ACAG and all-cause mortality
As indicated in Table 2, the all-cause mortality rate during ICU hospitalization of the study population from the MIMIC IV database and our hospital is 44.25 and 37.89%, respectively. For the whole study population, the mortality rate of the high ACAG group (49.14%) is significantly higher than that of the normal ACAG group (21.31%, χ2 = 43.163, P < 0.001). Meanwhile, similar results are reported in both the subgroup of patients from the MIMIC IV database and our hospital (all P < 0.001).
Kaplan–Meier survival curve analysis
In the Kaplan–Meier survival curves, as noted in Fig. 2, ICU cumulative survival rate is high for the normal ACAG group compared to the high ACAG group (log-rank test, χ12 = 13.620, χ22 = 12.460, both P < 0.001).
Higher ACAG was significantly associated with ICU all-cause mortality
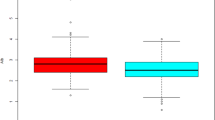
As noted in Fig. 3, a linear relationship is observed between ACAG at CRRT initiation and ICU all-cause mortality in the MIMIC IV database = 1.380, P = 0.709), while the relationship in our hospital is nonlinear (χ2 = 9.640, P = 0.022).
For patients from the MIMIC IV database, the HR (95% CI) of ICU all-cause mortality for the high ACAG group compared to the normal ACAG group is 2.474 (1.504–4.069). The HR (95% CI) of ICU all-cause mortality for the high ACAG group compared to the normal ACAG group is 2.288 (1.416–3.696,) for patients from Huzhou Central Hospital. Based on the multivariate Cox proportional hazard analyses, an elevated ACAG at CRRT initiation (> 20 mmol/L) is an independent predictor for ICU all-cause mortality after adjusting for potential confounders (Table 3).
Discussion
The current study found that patients in the high ACAG group exhibited a higher ICU all-cause mortality rate than the normal ACAG group. Simultaneously, the Kaplan–Meier survival curves showed that ICU cumulative survival rate is high for the normal ACAG group compared to the high ACAG group. The results of the RCS were different, which might be a result of the differences in race of patients, sample sizes, and normal reference range of AG, etc. Furthermore, compared with participants with normal ACAG levels, those with high ACAG levels (> 20 mmol/L) in the MIMIC-IV database and in our hospital denoted a 1.85-fold and 1.64-fold increased risk of ICU all-cause mortality, respectively. Hence, clinicians ought to pay more attention to those patients with ACAG more than 20 mmol/L because of the poor prognosis associated with high ACAG levels.
It is universally acknowledged that acid–base homeostasis is the basis of life, and several organ systems including brain, lungs, kidney, and liver are involved in the regulation of acid–base balance [16, 17]. Indeed, the kidneys play a central role in maintaining electrolyte homeostasis and acid–base balance [18]. AKI is a common and severe complication in patients hospitalized in the ICU [19], characterized by an increase in SCr levels and impairment of kidney functions such as fluid, electrolyte, and acid–base balance [20]. Moreover, metabolic acidosis is one of the most common complications in AKI patients [21]. Accumulating evidence suggested that metabolic acidosis is associated with an increased risk of chronic kidney disease progression [22, 23], as acidosis can reduce renal blood flow and increase the release of inflammatory mediator [24]. However, studies on the relationship between metabolic acidosis and the progression of kidney dysfunction during AKI are scarce. One experimental study [25] demonstrated that metabolic acidosis exacerbates renal injury through the high expression of NF-κB in an ischemia/reperfusion-induced AKI model. Besides, previously published articles indicated that the indicators of metabolic acid–base status, such as AG, base excess, and lactate, etc., can serve as potential prognostic predictors for AKI patients.
Metabolic acidosis is one of the most common complications of patients hospitalized in ICU, and high AG metabolic acidosis is one subcategory of metabolic acidosis [26, 27]. In a prospective study [28], plasma AG was measured in 500 critically ill patients, and the authors concluded that an elevated AG level on ICU admission was associated with higher mortality and longer length of stay in the ICU. In addition, several other studies have also explored the relationships between metabolic acidosis and clinical outcomes of AKI patients. Cheng Y et al. [29] found a U-shaped association between base excess value measured at the ICU admission and 30 day all-cause mortality in critically AKI patients, and both lower (≤ − 3 mEq/L)and higher (≥ 9 mEq/L) base excess would increase the risk of 30 day all-cause mortality. One latest study by Uusalo and colleagues [30] acknowledged that for perioperative AKI patients requiring CRRT, blood lactate at ICU admission and CRRT initiation were both independently associated with mortality.
ACAG, which is combined serum albumin and AG, can be used to distinguish acidosis caused by acid load or base deficit, which correspond to two pathological states of human body-hypoalbuminemia and metabolic acidosis [31]. Also, as mentioned previously, ACAG value is a more accurate predictor for metabolic acidosis for critically ill patient because of their hypoalbuminemia. Recently, one study has reported that low serum albumin before the initiation of CRRT is an independent predictor of mortality of AKI patients who underwent CRRT [9]. It’s worth noting that the incidence of hypoalbuminemia (albumin < 3.5 g/dL) is as high as 80.23% (568/708) in the overall patient population in our study. Cheng and colleagues observed a nonlinear association between AG measured at ICU admission and 30 day all-cause mortality, and high-AG levels (≥ 14 mmol/L) at the time of ICU admission are independently associated with 30, 90 and 365 day all-cause mortality in patients with AKI [32]. However, studies regarding the relationship between ACAG and mortality in patients undergoing CRRT for AKI have not been reported before. Consequently, we carried out this study and found that ACAG at the initiation of CRRT treatment is an independent risk factor that can predict the ICU all-cause mortality of these patients.
The current study has several strengths. First, this study is the first to explore the relationship between ACAG and mortality in patients undergoing CRRT for AKI. Second, the data in this study are collected from two distinct sources: one subtset of data is from a well-established registry of MIMIC-IV database with high data quality from America, and the other subset comes from a Chinese teaching hospital. Data from both subsets generate positive results that are consistent with each other based our analysis. In conclusion, our findings demonstrate elevated ACAG at CRRT initiation is associated with mortality of AKI patients treated with CRRT.
However, there were several limitations of our study. First, this study is a retrospective study, therefore, inherent biases cannot be ignored because of the retrospective nature. Second, due to the absence of data regarding out-of-hospital mortality in the MIMIC-IV (v1.0) database and Huzhou Central Hospital, we are unable to evaluate the relationship between ACAG and prognosis after discharge in AKI patients undergoing CRRT. Third, the current study explored the relationship between the ACAG and mortality based on a single ACAG measurement. Consequently, further study is warranted to investigate the relationship between the dynamic changes of ACAG and mortality of these patients.
In conclusion, the current evidence suggested that a higher ACAG level (> 20 mmol/L) at the initiation of CRRT treatment is associated with ICU all-cause mortality in critically AKI patients who undergo CRRT, and ACAG can serve as an early indicator of adverse outcomes for these patients. Nonetheless, additional studies, especially a rigorously designed prospective study, are required to evaluate and verify this finding.
Data availability
Not applicable.
Abbreviations
- ACAG:
-
Albumin corrected anion gap
- AG:
-
Anion gap
- RCS:
-
Restricted cubic spine
- AKI:
-
Acute kidney injury
- CRRT:
-
Continuous renal replacement therapy
- CI:
-
Confidence interval
- HR:
-
Hazard ratio
- ICU:
-
Intensive care unit
- IQR:
-
Interquartile range
- KDIGO:
-
Kidney Disease Improving Global Outcomes
- MIMIC:
-
Medical Information Mart for Intensive Care
- Scr:
-
Serum creatinine
- SD:
-
Standard deviation
References
Saito R, Hirayama A, Akiba A, Kamei Y, Kato Y, Ikeda S, Kwan B, Pu M, Natarajan L, Shinjo H et al (2021) Urinary metabolome analyses of patients with acute kidney injury using capillary electrophoresis-mass spectrometry. Metabolites 11(10):671
Annamalai C, Seth R, Viswanathan P (2021) Ferrotoxicity and Its amelioration by calcitriol in cultured renal cells. Anal Cell Pathol 2021:6634429
Hoste EAJ, Kellum JA, Selby NM, Zarbock A, Palevsky PM, Bagshaw SM, Goldstein SL, Cerda J, Chawla LS (2018) Global epidemiology and outcomes of acute kidney injury. Nat Rev Nephrol 14(10):607–625
Verma S, Palevsky PM (2021) Prescribing continuous kidney replacement therapy in acute kidney injury: a narrative review. Kidney med 3(5):827–836
An JN, Kim SG, Song YR (2021) When and why to start continuous renal replacement therapy in critically ill patients with acute kidney injury. Kidney Res Clin Pract 40(4):566–577
Shawwa K, Kompotiatis P, Bobart SA, Mara KC, Wiley BM, Jentzer JC, Kashani KB (2021) New-onset atrial fibrillation in patients with acute kidney injury on continuous renal replacement therapy. J Crit Care 62:157–163
Schricker S, Schanz M, Alscher MD, Kimmel M (2020) Metabolic acidosis : diagnosis and treatment. Medizinische Klinik Intensivmedizin und Notfallmedizin 115(4):275–280
Pratumvinit B, Lam L, Kongruttanachok N, Hemthong C, Kost GJ, Kamkang P, Reesukumal K (2020) Anion gap reference intervals show instrument dependence and weak correlation with albumin levels. Clin Chim Acta 500:172–179
Lv J, Wang H, Sun B, Gao Y, Zhang Z, Pei H (2021) Serum albumin before crrt was associated with the 28 and 90 day mortality of critically ill patients with acute kidney injury and treated with continuous renal replacement therapy. Front Nutr 8:717918
Rhee H, Jang GS, Kim S, Lee W, Jeon H, Kim DW, Ye BM, Kim HJ, Kim MJ, Kim SR et al (2022) Worsening or improving hypoalbuminemia during continuous renal replacement therapy is predictive of patient outcome: a single-center retrospective study. J Intensive Care 10(1):25
Figge J, Bellomo R, Egi M (2018) Quantitative relationships among plasma lactate, inorganic phosphorus, albumin, unmeasured anions and the anion gap in lactic acidosis. J Crit Care 44:101–110
Figge J, Jabor A, Kazda A, Fencl V (1998) Anion gap and hypoalbuminemia. Crit Care Med 26(11):1807–1810
Hu T, Zhang Z, Jiang Y (2021) Albumin corrected anion gap for predicting in-hospital mortality among intensive care patients with sepsis: A retrospective propensity score matching analysis. Clin Chim Acta 521:272–277
Hagiwara S, Oshima K, Furukawa K, Nakamura T, Ohyama Y, Tamura J (2013) The significance of albumin corrected anion gap in patients with cardiopulmonary arrest. Ann Thorac Cardiovasc Surg 19(4):283–288
He X, Liao X, Xie Z, Jiang C, Kang Y (2017) Albumin corrected anion gap is an independent risk factor for long-term mortality of patients with sepsis. Zhonghua wei zhong bing ji jiu yi xue 29(2):117–121
Berend K, Duits AJ (2019) The role of the clinical laboratory in diagnosing acid-base disorders. Crit Rev Clin Lab Sci 56(3):147–169
Seifter JL, Chang HY (2017) Disorders of acid-base balance: new perspectives. Kidney Dis 2(4):170–186
Dhondup T, Qian Q (2017) Electrolyte and acid-base disorders in chronic kidney disease and end-stage kidney failure. Blood Purif 43(1–3):179–188
Orieux A, Boyer A, Dewitte A, Combe C, Rubin S (2022) Acute kidney injury in intensive care unit: a review. Nephrologie Therapeutique 18(1):7–20
Albeladi FI (2021) Essence core: fluid management in acute kidney injury. Saudi J Kidney Dis Transpl 32(1):9–18
Thongprayoon C, Qureshi F, Petnak T, Cheungpasitporn W, Chewcharat A, Cato LD, Boonpheng B, Bathini T, Hansrivijit P, Vallabhajosyula S et al (2020) Impact of acute kidney injury on outcomes of hospitalizations for heat stroke in the United States. Diseases 8(3):28
Hu J, Wang Y, Geng X, Chen R, Xu X, Zhang X, Lin J, Teng J, Ding X (2017) Metabolic acidosis as a risk factor for the development of acute kidney injury and hospital mortality. Exp Ther Med 13(5):2362–2374
Kim HJ, Ryu H, Kang E, Kang M, Han M, Song SH, Lee J, Jung JY, Lee KB, Sung S et al (2021) Metabolic acidosis is an independent risk factor of renal progression in Korean chronic kidney disease patients: the KNOW-CKD study results. Front Med (Lausanne) 8:707588
Chowdhury AH, Cox EF, Francis ST, Lobo DN (2012) A randomized, controlled, double-blind crossover study on the effects of 2-L infusions of 0.9%saline and plasma-lyte(R) 148 on renal blood flow velocity and renal cortical tissue perfusion in healthy volunteers. Ann Surg 256(1):18–24
Magalhaes PA, de Brito TS, Freire RS, da Silva MT, dos Santos AA, Vale ML, de Menezes DB, Martins AM, Liborio AB (2016) Metabolic acidosis aggravates experimental acute kidney injury. Life Sci 146:58–65
Ghauri SK, Javaeed A, Mustafa KJ, Podlasek A, Khan AS (2019) Bicarbonate therapy for critically ill patients with metabolic acidosis: a systematic review. Cureus 11(3):e4297
Sajan A, Horowitz J, Murakami N, McFarlane IM (2019) Recurrent anion gap metabolic acidosis. Am J Med Case Rep 7(9):200–202
Dafal A, Kumar S, Agrawal S, Acharya S, Nirmal A (2021) admission anion gap metabolic acidosis and its impact on patients in medical intensive care unit. J Lab Physician 13(2):107–111
Cheng Y, Zhang Y, Tu B, Qin Y, Cheng X, Qi R, Guo W, Li D, Wu S, Zhu R et al (2021) Association between base excess and mortality among patients in ICU with acute kidney injury. Front Med 8:779627
Uusalo P, Hellman T, Jarvisalo MJ (2021) Mortality and associated risk factors in perioperative acute kidney injury treated with continuous renal replacement therapy. Perioper Med 10(1):57
Jung B, Martinez M, Claessens YE, Darmon M, Klouche K, Lautrette A, Levraut J, Maury E, Oberlin M, Terzi N et al (2019) Diagnosis and management of metabolic acidosis: guidelines from a French expert panel. Ann Intensiv Care 9(1):92
Cheng B, Li D, Gong Y, Ying B, Wang B (2020) Serum anion gap predicts all-cause mortality in critically Ill patients with acute kidney injury: analysis of the MIMIC-III database. Dis Markers 2020:6501272
Funding
This study was funded by the Key Research and Development Plan of Zhejiang province (2019C03024), Provincial and ministerial joint construction of key projects of Zhejiang Medical and Health Science and Technology Plan (WKJ-ZJ-1811) and Traditional Chinese Medicine Science and Technology Plan Project of Zhejiang Province (2019ZA017).
Author information
Authors and Affiliations
Contributions
YXH and ZL conceived and designed the study. ZL was responsible for the data collection, management, statistical analyses and manuscript. XB and JXW were involved in drafting and revising the article. YXH read and revised this manuscript from a professional standpoint. All authors approved the final version and the decision to submit for publication.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Human and animal rights statement and informed consent
The study was approved by the Institutional Review Board of Huzhou Central Hospital (approval number: 202203021-01) with a waiver of informed consent because of the anonymous nature of this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhong, L., Xie, B., Ji, XW. et al. The association between albumin corrected anion gap and ICU mortality in acute kidney injury patients requiring continuous renal replacement therapy. Intern Emerg Med 17, 2315–2322 (2022). https://doi.org/10.1007/s11739-022-03093-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-022-03093-8