Abstract
Haemoglobin A1c (HbA1c) is a marker of glycaemic control in type 2 diabetes mellitus (T2DM). Increased waist circumference (WC) is known to be associated with T2DM. Therefore, we investigated the relationship of WC with HbA1c and explored its optimal cutoff for identifying prediabetes and diabetes risk. This study included 2339 participants between 18 and 84 years of age [mean (SD) age, 43.5 (11.9) years] with valid data on WC, HbA1c and related variables in the Shenzhen–Hong Kong United Network on Cardiovascular Disease study. Participants on anti-diabetic medications were excluded. Multiple linear regression was used to investigate the relationship between HbA1c and WC. Cutoff values of WC indicating an HbA1c level of 5.7% and 6.5% were also assessed using optimal binning. There was a significant linear relationship between WC and HbA1c in the overall population (B = 0.261, P < 0.001), men (B = 0.206, P < 0.001) and women (B = 0.311, P < 0.001). After adjustment for smoking, alcohol consumption, physical activity, hypertension, hypercholesterolaemia and age, the association remained significant in the overall population (B = 0.201, P < 0.001), men (B = 0.186, P < 0.001) and women (B = 0.182, P < 0.001). The optimal cutoff values of WC indicating an HbA1c level of 5.7% and 6.5% was 83 cm (entropy = 0.943) and 85 cm (entropy = 0.365) in men, and 78 cm (entropy = 0.922) and 86 cm (entropy = 0.256) in women. The linear relationship between WC and HbA1c in this study suggests that addressing central obesity issue is beneficial to people with T2DM or at risk of T2DM. WC cutoff values of 85 cm for men and 86 cm for women are appropriate for recommendation to undergo diabetes screening.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity is associated with increased risk of multiple diseases such as type 2 diabetes mellitus (T2DM), hypertension and cardiovascular disease, resulting in premature death. According to the latest national survey, more than half of Chinese adults are either overweight or obese, which have become a severe public health concern [1]. It suggested that overweight and obesity would increase the risk of major non-communicable diseases and premature mortality in the general population [1].
Haemoglobin A1c (HbA1c) can reflect average blood glucose level over the past 4 months because the average lifespan of erythrocytes is approximately 120 days. As HbA1c represents a weighted mean of glucose levels, it is used as an indicator of glycaemic control in patients with diabetes.
Waist circumference (WC) is a simple measure of central obesity, which is the cornerstone of the metabolic syndrome and an important risk factor for diabetes [2, 3]. Although glucose monitoring tools, like glucose monitoring meters and blood tests, are minimally invasive, WC is a more timesaving and less expensive screening tool. Therefore, WC may serve as an additional measure beyond blood glucose measurement for identifying prediabetic and diabetic risk. Central obesity has been shown to be associated with fasting plasma glucose (FPG) in Mediterranean, African and US populations [4,5,6]. An African study suggested that WC could predict incident dysglycaemia and T2DM in Black African men and women [5]. WC was associated with FPG in a US study [6]. Whether waist circumference (WC) is associated with HbA1c in Chinese has not been much investigated. Therefore, we aim to study the relationship between waist circumference and HbA1c in a Chinese population.
Materials and methods
Database and study population
The Shenzhen–Hong Kong United Network on Cardiovascular Disease is a population-based survey that began in December 2020. A total of 2339 participants from different communities in Shenzhen enrolled in the first batch of the survey at the end of 2020. The study was reviewed and approved by the institutional review board of Peking University Shenzhen Hospital and the University of Hong Kong. The survey comprises three parts—interview, physical examination and laboratory tests. Data on demographic characteristics, lifestyle factors, dietary habits, medical history and medication usage were obtained using a standard questionnaire during interview. All interviewers, physical examiners and phlebotomists completed training sessions to understand the standard methods and protocol of this survey and master the usage of the survey tools before conducting the survey. All participants voluntarily participated in this research and gave informed consent.
In the present study, participants who had valid data were included for investigating the association of WC with HbA1c and FPG. In all of them, valid data on WC, HbA1c, FPG, smoking, alcohol consumption, physical activity, blood pressure (BP), and hypercholesterolemia were available. Subjects who were on anti-diabetic medications were excluded from the study.
Measurements and definitions
WC was measured in the horizontal plane midway between the lowest rib and the iliac crest using inelastic tape at the end of normal expiration. Central obesity was defined according to the WC cut-offs for Asian adults (WC ≥ 90 cm for male, WC ≥ 80 cm for female). BMI was calculated as the weight in kilograms divided by the square of height in meters (kg/m2). Smoking was defined as smoking any tobacco product, either daily or occasionally or having smoking history. Participants were categorised as drinkers if they reported that they drank any type of alcohol beverage at least once a week or had a history of alcohol drinking. Alcohol beverages included beer, liquor, wine and other alcohol beverages. Participants who had at least 30 min of moderate to high-intensive physical activity on 3 or more days a week were classified as physically active. Blood pressure was measured up to three times in the right arm using a mercury sphygmomanometer after at least 15 min of rest. Hypertension was defined as a previous diagnosis of hypertension by a doctor or another health professional, average blood pressure ≥ 140/90 mmHg, or taking medication for hypertension. Definition of hypercholesterolaemia was previous diagnosis of a doctor or other health professional, total serum cholesterol ≥ 200 mg/dL, or taking medication for hypercholesterolaemia. Blood samples were obtained to measure levels of FPG and HbA1c after fasting for 8 hours. Diabetes was defined by previous diagnosis from a doctor or other health professional, FPG ≥ 7.0 mmol/L, HbA1c ≥ 6.5% or taking medication for diabetes.
Statistical analysis
Statistical analysis was carried out using SPSS Version 27 (IBM Corporation, Armonk, New York). Chi-squared test was used to analyse the baseline characteristics of participants. The FPG or HbA1c in different WC groups in different age groups (18–39 years, 40–59 years and 60–84 years) [7] in men and women were analysed using t test. Linear regression was used to evaluate the relationship of WC with FPG and HbA1c in men and women. Confounding factors such as age, hypercholesterolemia, hypertension, alcohol consumption, smoke and physical activity were included in the regression models. Further, we used optimal binning to find the cutoff values of WC indicating HbA1c of 5.7% and 6.5%. P ≤ 0.05 was considered significant .
Results
A total of 2202 participants (951 men and 1251 women) aged 18–84 years were included in the analysis. In the sensitivity analysis, 152 participants with diabetes were excluded (Supplementary figure 1). In the overall population, 42% of participants had central obesity. The mean WC was 82.1 ± 10.2 cm.
Table 1 shows the general characteristics of the participants with respect to HbA1c. The mean WC of participants with HbA1c ≥ 6.5% was 89.9 ± 9.0 cm while the mean WC of participants with HbA1c < 6.5% was 81.7 ± 9.9 cm (P < 0.001). Participants with HbA1c ≥ 6.5% were older and had higher BMI (P < 0.001). Furthermore, participants with HbA1c ≥ 6.5% were more likely to be men (P = 0.018), had hypercholesterolaemia and hypertension (P < 0.001). However, there were no significant associations of HbA1c with smoking, alcohol consumption and physical activity.
Tables 2 and 3 show the difference in mean FPG or HbA1c in participants with and without central obesity. In men, mean HbA1c statistically differed between normal (WC < 90 cm) and central obese (WC ≥ 90 cm) subjects in the 18–39 age group (P < 0.001) and in the 40–59 age group (P = 0.017) but not in the 60–84 age group (P = 0.209). The differences were also found in women aged 18–39 years (P < 0.001), 40–59 years (P < 0.001) but not aged 60–84 years (P = 0.195). In addition, a difference in FPG level was found in male participants with and without central obesity in the 18–39 age group (P < 0.001) while a difference was found in women in the 18–39 age group (P = 0.025) and 40–59 age group (P < 0.001).
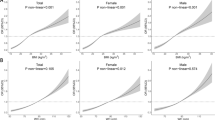
Figure 1 shows the linear relationship between WC and HbA1c in men and women. HbA1c was gradually increased with WC groups in men from 5.5% to 6.0% and women from 5.4% to 5.9%. Table 4 shows the linear regression analysis for the association between WC and HbA1c. In the linear regression model, WC was associated with HbA1c before adjustment in the overall population (B = 0.261, P < 0.001), in men (B = 0.206, P < 0.001) and women (B = 0.311, P < 0.001). After adjustment for smoking, alcohol consumption, physical activity, hypertension, hypercholesterolaemia and age, the association remained significant (overall: B = 0.201, P < 0.001; men: B = 0.186, P < 0.001; women: B = 0.182, P < 0.001).
Table 5 shows the optimal cutoff values of WC indicating HbA1c in men and women. In men, the optimal cutoff values of WC indicating an HbA1c of 5.7–6.5% was 83 cm (entropy: 0.943) and 85 cm (entropy: 0.365). In women, the optimal cutoff values of WC indicating an HbA1c of 5.7–6.5% was 78 cm (entropy: 0.922) and 86 cm (entropy: 0.256).
The linear regression analysis for the relationship between WC and FPG is shown in supplementary table 1. In the linear regression model, WC was associated with FPG before adjustment in the overall population (B = 0.221, P < 0.001), in men (B = 0.175, P < 0.001) and women (B = 0.259, P < 0.001). After adjustment for smoking, alcohol consumption, physical activity, hypertension, hypercholesterolaemia and age, the association remained significant (overall: B = 0.194, P < 0.001; men: B = 0.170, P < 0.001; women: B = 0.166, P < 0.001). WC was consistently associated with FPG after further adjusting for sex in the overall population (B = 0.182, P < 0.001).
In the sensitivity analysis (supplementary table 2), we excluded all diabetic patients to investigate the association of waist circumference with HbA1c in non-diabetic men and women. There was an association between WC and HbA1c before adjustment in the overall population (B = 0.230, P < 0.001), in men (B = 0.179, P < 0.001) and women (B = 0.270, P < 0.001). After adjusting for smoking, alcohol consumption, physical activity, hypertension, hypercholesterolaemia and age, the association was attenuated but still significant (overall: B = 0.162, P < 0.001; men: B = 0.141, P < 0.001; women: B = 0.158, P < 0.001). WC was consistently associated with FPG after adjusting for sex in overall population (B = 0.162, P < 0.001).
Discussion
The main finding of this study is that there was a significant linear relationship of WC with HbA1c and FPG in Chinese aged 18–84 in the general population. The association was significant in both men and women after adjusting for smoking, alcohol consumption, physical activity, hypertension, hypercholesterolaemia and age.
Our study reveals a new and convenient way for people in general and diabetic patients to roughly know their HbA1c by measuring their WC. Frequent testing of FPG and HbA1c in non-diabetic persons causes inconvenience and discomfort. Measuring WC could be a supplementary method for regular use at home to prompt diet and lifestyle modification. In addition, our study is a community-based study. Shenzhen is a city of migrants and, therefore, the study population is representative of the general population in China, at least in terms of genetic background.
Previous studies in different Chinese populations have shown that WC, which is an index of central obesity, is significantly associated with T2DM. A longitudinal study in northern China involving 10,419 participants aged 20–80 years in 2008–2012 showed that WC and its changes were associated with the risk of T2DM. In Cox proportional hazard regression models, WC was found to be a risk factor predictive of T2DM, with an area under the receiver operating characteristic curve of 0.624, which was significantly greater than that for BMI. Moreover, the study found that every 2 kg weight gain or 3 cm WC increase conferred a 1.53-fold or 1.37-fold risk of developing diabetes, respectively [8]. In the Jackson Heart Study in the US that involved 2450 participants and a mean follow-up duration of 8 years, higher levels of HbA1c within the normal range were associated with incident diabetes (HR = 7.51, 95% CI 2.66–21.25) [9]. A large prospective study including 12,403 incident T2DM cases from eight European countries with 3.99 million person-years of follow-up reached the same conclusion, that WC was an independent risk factor for T2DM. The study further indicated that the association was stronger in women (HR = 31.8; 95% CI 25.2–40.2) than in men (HR = 22.0; 95% CI 14.3–33.8), which suggested that it is important to measure WC in women for risk stratification [10]. To date, most studies focused on the association between WC and diabetes but not on the association between WC and HbA1c. Our study highlights the significant association between WC and HbA1c in the general population.
Age differences in the association of WC with HbA1c were shown in our study. WC was significantly associated with HbA1c in the 18–39 age group in both men and women but the association was attenuated in the 40–59 age group and the 60–84 age group. Body adiposity changes with age, resulting in an increase in abdominal fat [11]. The changes of body composition with age may affect both WC and HbA1c. There are studies suggesting that obesity is a major driver in the development of T2DM in youth. A prospective study from the China Kadoorie Biobank that included 512,891 adult subjects aged 35–74 years demonstrated a significant association of central adiposity in early adulthood with incident T2DM after 9.2 years of follow-up [12]. A nationwide study of over one million Israelis aged 16–19 years showed that those with severe obesity had a higher risk of diabetes in the following decades [13]. Among severely obese boys and girls, the mean age of diabetes onset was 27.8 and 25.9 years, while the corresponding ages in the normal BMI reference group were 30.4 and 29.0 years [13]. These findings mean that central obesity increases diabetes risk as early as in adolescence rather than in old age. The measurement of WC allows early prediction of diabetes risk, and allows amelioration of that risk through lifestyle modification.
This study suggests that the optimal WC cutoff point indicating prediabetic risk for male and female are 83 cm and 78 cm whereas the optimal WC cutoff point indicating diabetic risk for male and female are 85–86 cm, respectively. The WC cutoff point indicating diabetic risk for female is higher than that for male. It may be relevant to recall that Japanese WC cut-offs identifying metabolic syndrome for men and women are 85–90 cm, which are equivalent to 100 cm2 of visceral fat. This discrepancy is due to the higher amount of subcutaneous fat in women for a given level of visceral adiposity [14]. T2DM is known to be more strongly associated with WC than BMI. As WC is an easy measurement for the general population, the optimal cutoff of WC for screening diabetes is of practical as well as reference value [15]. However, optimal WC cutoff points indicating prediabetic and diabetic risk are not much investigated. Moreover, the Chinese population is changing in terms of demographics, living standards and lifestyle, such that cutoff values based on previous data may no longer be applicable. Our study not only fills a void but also yields new optimal WC cutoff values based on up-to-date data on a Chinese population that is relatively young and affluent, and would, therefore, be predictive of future trends in China.
The limitation of our study is that the sensitivity and specificity for WC to identify diabetics is not high. However, WC is convenient for patients to measure at home and can be repeatedly measured over a long period of time. It can serve as an additional measure beyond blood glucose measurement at home between clinic visits.
Conclusions
Our study suggests that there is a significant linear relationship between WC and HbA1c. Addressing central obesity issue is of great importance in people at diabetic risk or suffering from diabetes. WC cutoff values of 85 cm for men and 86 cm for women are appropriate for recommendation to undergo diabetes screening.
Data availability
The datasets analysed in the current study available from the corresponding author on reasonable request.
References
Pan XF, Wang L, Pan A (2021) Epidemiology and determinants of obesity in China. Lancet Diabetes Endocrinol 9(6):373–392
Cheung BM, Wat N, Man Y, Tam S, Thomas GN, Leung GM et al (2007) Development of diabetes in Chinese with the metabolic syndrome: a 6-year prospective study. Diabetes Care 30(6):1430–1436
Cheung BM, Wat N, Tam S, Thomas GN, Leung GM, Cheng CH et al (2008) Components of the metabolic syndrome predictive of its development: a 6-year longitudinal study in Hong Kong Chinese. Clin Endocrinol 68(5):730–737
Baena-Díez JM, Elosua R, Cano JF, Masiá R, Sala J, Marrugat J et al (2009) Waist circumference and impaired fasting glucose screening in a Mediterranean population. Diabetes Res Clin Pract 86(2):e12–e14
Goedecke JH, Nguyen KA, Kufe C, Masemola M, Chikowore T, Mendham AE et al (2022) Waist circumference thresholds predicting incident dysglycemia and type 2 diabetes in Black African men and women. Diabetes Obes Metab 24(5):918–927
Firouzi SA, Tucker LA, LeCheminant JD, Bailey BW (2018) Sagittal abdominal diameter, waist circumference, and BMI as predictors of multiple measures of glucose metabolism: an NHANES investigation of US adults. J Diabetes Res 2018:3604108
Zhang Y, Moran AE (2017) Trends in the prevalence, awareness, treatment, and control of hypertension among young adults in the United States, 1999 to 2014. Hypertension (Dallas, Tex: 1979) 70(4):736–742
Fan Y, Wang R, Li D, Meng Z, Zhang Q, Shen Y et al (2020) Waist circumference and its changes are more strongly associated with the risk of type 2 diabetes than body mass index and changes in body weight in Chinese adults. J Nutr 150(5):1259–1265
Edwards MK, Addoh O, Sng E, Ikuta T, Carithers T, Bertoni AG et al (2017) Physical activity, body mass index and waist circumference change, and normal-range glycated hemoglobin on incident diabetes: Jackson heart study. Postgrad Med 129(8):842–848
Langenberg C, Sharp SJ, Schulze MB, Rolandsson O, Overvad K, Forouhi NG et al (2012) Long-term risk of incident type 2 diabetes and measures of overall and regional obesity: the EPIC-InterAct case-cohort study. PLoS Med 9(6):e1001230
Zong G, Zhang Z, Yang Q, Wu H, Hu FB, Sun Q (2016) Total and regional adiposity measured by dual-energy X-ray absorptiometry and mortality in NHANES 1999–2006. Obesity (Silver Spring, Md) 24(11):2414–2421
Bragg F, Tang K, Guo Y, Iona A, Du H, Holmes MV et al (2018) Associations of general and central adiposity with incident diabetes in Chinese men and women. Diabetes Care 41(3):494–502
Twig G, Zucker I, Afek A, Tali CY, Bendor CD, Derazne E et al (2020) Adolescent obesity and early-onset type 2 diabetes. Diabetes Care 43(7):1487–1495
Nishimura R, Nakagami T, Tominaga M, Yoshiike N, Tajima N (2007) Prevalence of metabolic syndrome and optimal waist circumference cut-off values in Japan. Diabetes Res Clin Pract 78(1):77–84
Hou X, Chen S, Hu G, Chen P, Wu J, Ma X et al (2019) Stronger associations of waist circumference and waist-to-height ratio with diabetes than BMI in Chinese adults. Diabetes Res Clin Pract 147:9-18
Funding
This work was financially supported by Hong Kong Innovation and Technology Fund, Guangdong-Hong Kong Technology Cooperation Funding Scheme (TCFS) from Hong Kong Innovation and Technology Commission (GHP/138/18SZ) and Grant of Shenzhen-Hong Kong Innovation Circle from Shenzhen Science and Technology Innovation Committee (SGLH20180629094602262).
Author information
Authors and Affiliations
Contributions
SL and JW collected the data. BMYC and CL planned the study. JZ and CL analysed the data. JZ performed the literature search and wrote the paper. All authors made critical revisions to the paper. All authors have contributed significantly to the manuscript to be published.
Corresponding authors
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Ethical approval
The study was reviewed and approved by the institutional review board of Peking University Shenzhen Hospital and the University of Hong Kong.
Informed consent
All participants voluntarily participated in this research and gave informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhen, J., Liu, S., Zhao, G. et al. Association of waist circumference with haemoglobin A1c and its optimal cutoff for identifying prediabetes and diabetes risk in the Chinese population. Intern Emerg Med 17, 2039–2044 (2022). https://doi.org/10.1007/s11739-022-03072-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-022-03072-z