Abstract
One of the most helpful strategies to deal with ongoing coronavirus pandemics is to use some prudence when treating patients infected with SARS-CoV-2. We aimed to evaluate the clinical, demographic, and laboratory parameters that might have predictive value for in-hospital mortality and the need for intensive care and build a model based on them. This study was a prospective, observational, single-center study including non-critical patients admitted to COVID-19 wards. Besides classical clinic-demographic features, basic laboratory parameters obtained on admission were tested, and then new models for each outcome were developed built on the most significant variables. Receiver operating characteristics (ROC) analyses were performed by calculating each model’s probability. A total of 368 non-critical hospitalized patients were recruited, the need for ICU care was observed in 70 patients (19%). The total number of patients who died in either ICU or wards was 39 (10.6%). The first two models (based on clinical features and demographics) were developed to predict ICU and death, respectively; older age, male sex, active cancer, and low baseline saturation were noted to be independent predictors. The area under the curve values of the first two models were noted 0.878 and 0.882 (p < .001; confidence interval [CI] 95% [0.837–0.919], p < .001; CI 95% [0.844–0.922]). Following two models, the third and fourth were based on laboratory parameters with clinic-demographic features. Initial lower sodium and lower albumin levels were determined as independent factors in predicting the need for ICU care; higher blood urea nitrogen and lower albumin were independent factors in predicting in-hospital mortality. The area under the curve values of the third and fourth model was noted 0.938 and 0.929, respectively (p < .001; CI 95% [0.912–0.965], p < .001; CI 95% [0.895–962]). By integrating the widely available blood tests results with simple clinic demographic data, non-critical patients can be stratified according to their risk level. Such stratification is essential to filter the patients’ non-critical underlying diseases and conditions that can obfuscate the physician’s predictive capacity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Coronavirus disease 2019 (COVID-19) has already affected millions of people. Most patients with COVID-19 are asymptomatic or experience mild illness; however, some patients rapidly progress to a critical stage of the disease. The proportion of hospitalized patients who develop acute respiratory distress syndrome (ARDS) during the course of the disease is between 16 and 29% [1,2,3]. The fatality rate has been documented to be 40.5% in critically ill COVID-19 patients, similar to ARDS [4]. However, the fatality rate remains obscure among those hospitalized but not admitted as severe or critical since considerable variation has occurred from time to time, institute to institute and country to country. Nevertheless, the case fatality rate of hospitalized COVID-19 patients can be assumed to be between 4.3 and 15% [2, 5, 6].
Previous reports defined an array of prognostic factors for predicting the disease course. Older age, male sex, and pre-existing medical conditions are also associated with increased mortality [7, 8]. Besides these classical features, numerous investigations have been carried out to reveal factors associated with the severity. Various studies have gathered evidence on impaired interferon response, serum levels of cytokines, and the effect of concentrations of trace elements [9,10,11]. But a significant focus on inpatient management should be on ensuring a feasible, sustainable, and reliable risk categorization that can be adjusted to various non-critical cases. Recent studies have reported some nomograms and scoring systems; however, they did not satisfy the need for practical and reliable tools [12,13,14,15,16].
This study aimed to describe the clinical features and outcomes of a medium-scaled population consisting of non-critical cases and investigate all independent factors associated with in-hospital mortality and the need for intensive care. The second aim was to develop a model for a prediction tool that will lead to more proper and faster triage of these non-critical patients.
Patients and methods
Study design and participants
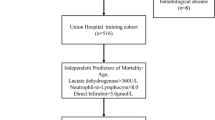
This prospective, observational, single-center study was conducted in a cohort of laboratory-confirmed COVID-19 patients hospitalized in a tertiary university hospital, Ankara, Turkey, between 15 June 2020 and 15 October 2020. The period was chosen with intention since the admission criteria before July were highly subjective. Even asymptomatic patients were hospitalized due to the ambiguity and lack of knowledge of the disease (Fig. 1).
All adult patients with suspected symptoms of COVID-19 presented to the emergency room, or COVID-19 outpatient clinics at our hospital were tested with a nasopharyngeal swab for virus identification by SARS-CoV-2 real-time reverse transcription-polymerase chain reaction (RT-PCR). Consultant physicians managed the medical treatment and decisions of admission, discharge, and intensive care unit (ICU) transfer regarding the relevant national guidelines and regulations. As this was an observational study, there was no intervention in the patient’s medical management and decisions.
Data collection
All patients or their official guardians signed the written informed consent to participate in the study. The medical registry was built according to the ethical principles and the medical data anonymization process details. The complete blindness of the caring physicians or nurses to the researchers was explained to the patients and their official guardians.
The demographics (age, gender, travel history), medical history (concurrent medical illnesses, contact history with COVID-19, detailed medication history), and symptoms were obtained directly from the patients or their first-degree relatives on admission. Concurrent medical conditions included a detailed list of the diseases (Supplementary File 1). Vital signs were recorded from the electronic database since primary caring physicians and nurses were not involved in the study. The blood tests included in routine admission protocol were recorded and not intervened by data collecting researchers.
The patients were tracked until discharge, transfer to the ICU, or death in the wards. The primary endpoint was the need for intensive care or death in the wards. The secondary endpoint was in-hospital mortality.
Clinical assessment
Judgment of the severity of COVID-19 pneumonia and subsequent stratification was made according to WHO Clinical Management Guideline: COVID-19 Clinical management [17]. Symptomatic patients meeting the case definition for COVID-19 without evidence of viral pneumonia or hypoxia were classified as mild. Patients with clinical signs of pneumonia (fever, cough, dyspnea, fast breathing) but no signs of severe pneumonia, including SpO2 ≥ 90% on room air, were classified as moderate. Patients with clinical signs of pneumonia (fever, cough, dyspnea, fast breathing) plus one of the following: respiratory rate > 30 breaths/min; respiratory distress; or SpO2 < 90% on room air were classified as severe disease. Critically ill patients requiring intensive care at the time of admission were excluded. The ICU admission criteria of our hospital were adapted according to national regulations.
Supportive and antiviral therapy was provided to all eligible patients soon after admission, and each individual was assessed by infectious disease specialists at the bedside upon admission and then daily. Favipiravir was the only approved and commercially available antiviral drug for COVID-19 treatment in Turkey [18]. Antibiotics were only administered to clinically suspected cases for bacterial co-infection, and the treating physician made the decision along with infectious disease specialists.
Statistical analysis
Patients were stratified into two groups based on the ICU requirement or death before ICU transfer (discharged without ICU requirement vs. either deceased before ICU transfer or transferred to ICU) and the survival outcome (discharged vs. deceased in the hospital).
Continuous variables were given as median ± interquartile range, as many variables were not distributed normally. Categorical variables were summarized as counts and percentages. The Chi-squared test (χ2 test) or Fisher’s exact test was used for categorical variables, and the Mann–Whitney U test was used for continuous ones.
After the descriptive analysis of the data, univariate logistic regression analyses were performed, any variable having a significant univariate test at some arbitrary level was selected as a candidate for the multivariate analysis, based on the Wald test from logistic regression and a p-value cut-off point of 0.2. Through using the ‘backward stepwise’ method, four multivariate logistic regression models (mv-model) were developed to identify predictors for each endpoint (need for ICU care and in-hospital mortality); mv-model ICU-1 and ICU-2 were developed to predict ICU transfer. The mv-model SUR-1 and SUR-2 were developed to predict in-hospital mortality. Interactions were also tested by adding interaction-term into models. The probability of the event occurring versus the model parameters (the data where \({y}_{i} \in \left\{-\mathrm{1,1}\right\}\) and \({x}^{(i)} \in {\mathbb{R}}^{n}\)) was calculated through the formula below;
The probability of each model (\(p\in \left\{0 , 1\right\}\)) was tested with receiver operating characteristic curves (ROC) with the area under the curve (AUC) statistics.
All analyses were conducted using the IBM SPSS Software version 22.0 (SPSS Inc., Chicago, IL) licensed to the institution where the study was carried on. Two-sided significance testing was performed, and p values < 0.05 were considered significant.
Results
Demographics and clinical data
We recorded 849 adult patients (≥ 18 years old) hospitalized in COVID-19 wards during the specified period (Fig. 1). After excluding patients who had inadequate radiological data (n = 122), inadequate or conflicting clinical data (n = 78), a history of readmission (n = 79), were hospitalized less than a day (n = 56), initially admitted to the intensive-care unit (n = 23) or did not have PCR confirmation (n = 99) and patients who did not want to be a participant to our cohort (n = 24), a total of 368 patients were recruited into our study. Among these, six patients (1.6%) were deceased before ICU transfer. Nevertheless, they met the admission criteria for ICU and they were also included in the group of patients requiring ICU care.
Three hundred twenty-eight (89.1%) patients were treated with the recommended dosage of favipiravir; those who were not eligible for the treatment with favipiravir were only observed with supportive therapy except for six patients (1.6%) who received remdesivir in the scope of a clinical trial.
Our cohort had a slightly female dominance (total n = 197; 53.5%) and a median age of 57 years (IQR 31). The most common comorbidities were arterial hypertension (AH) (n = 140, 38%) and diabetes mellitus (DM) (n = 89, 24.2%). As can be seen from Table 1, 64 patients were transferred to ICU, six patients died before ICU transfer, so the need for ICU care was observed/assumed in 70 patients (19%). The total number of patients who died in either ICU or wards was 39 (10.6%).
With regards to endpoints (need for intensive care and mortality), patients who experienced any of these events were significantly older (ICU group vs. non-ICU group: 68 vs. 52 years, p < 0.001, non-survivors vs. survivors: 68 vs. 53 years, p < 0.001) and predominantly male (ICU group vs. non-ICU group: 27.5% versus 11.7%; p < 0.001, non-survivors vs. survivors: 16.5% versus 5.6%; p = 0.001), compared to those who did not (Table 1).
Patients who required intensive care had a higher prevalence of AH (p < 0.001), coronary artery disease (CAD) (p = 0.001), congestive heart failure (CHF) (p = 0.002), active cancer (p = 0.002) and higher median CCI (p < 0.001) than the non-ICU group. Smoking was not different between the ICU group and the non-ICU group. Prevalences of certain comorbidities were also higher among the deceased patients (Table 1). Smoking habits did seem to be different among groups in regard to mortality outcomes. The difference comes mainly from ex-smokers (p = 0.002, Bonferroni correction was made for each 2 × 2 cross-table). The known epidemiological link was higher in patients who did not require intensive care (p < 0.001); however, it was not statistically significant between survivors and non-survivors (p = 0.241).
Among patients who required intensive care, the history of using diuretics, beta-blockers, anti-platelet therapy were significantly higher than the patients who were discharged without any event (Table 1). In patients who did not survive, the history of being treated by RAS blockers, diuretics, beta-blockers, and anti-platelet therapy was significantly higher than the patients who survived.
The need for oxygen support upon admission and baseline low saturation (< 90%) were significantly higher in ICU and non-survivor groups. The median duration between the onset of symptoms and PCR confirmation was 2 (IQR 3.25) days, and admission was 3 (IQR 3) days. The median length of stay in the wards was 5 (IQR 4) days. These intervals were not different between groups.
Laboratory parameters
Patients who required intensive care had significantly lower hemoglobin levels, lymphocyte, thrombocyte counts, but higher neutrophil counts (Table 2). Similar pattern was observed among those who didn’t survive; however, neutrophil counts were not different between survivors and non-survivors. Blood urea nitrogen (BUN), uric acid, AST, GGT, lactate dehydrogenase (LDH), ferritin, C-reactive protein (CRP), brain natriuretic peptide, erythrocyte sedimentation rate, procalcitonin, Il-6, fibrinogen, INR, d-dimer levels were significantly higher, and LDL, sodium, albumin levels were significantly lower in patients who required intensive care. A similar pattern was observed in the non-survivor group; however, HDL was also significantly lower, ESR and fibrinogen were not significantly different. Cardiac-specific enzymes were significantly higher in groups representing poor outcome in both endpoints.
Vital signs and symptomatology
Symptoms, vital signs, and the comparison of the proportions between groups are shown in Table 3. The most common two symptoms were fever (61.4%) and non-productive cough (54.6%). There were no statistically significant differences between groups regarding these symptoms. Sputum production was observed significantly higher in the ICU group than the non-ICU group (p = 0.039). The proportion of dyspnea was noted to be lower in the survivor group than non-survivors (p = 0.04). In contrast, sore throat and headache were recorded as significantly lower in the ICU group.
The vital signs were similar in both groups with both outcomes, besides baseline saturation on room air were significantly lower in groups who experienced the endpoints than those who did not.
Logistic regression models
The univariate binary logistic regression analysis for each variable for each endpoint is shown in Supplementary Table 1. Several demographic, clinical and laboratory parameters including; sex, smoking history, CCI score, the severity of the disease, medication history, requiring oxygen support on admission and baseline low O2 saturation on room air, sputum, higher neutrophil count, acute phase reactants, ferritin, LDH, GGT, AST, uric acid, d-dimer, cardiac enzyme levels and lower thrombocyte count, lymphocyte count, hemoglobin, sodium and albumin, LDL levels were recorded as significant predictors for ICU need. Having a lower HDL, in addition to LDL, was also a significant predictor for in-hospital mortality.
Four models were developed for different purposes (Table 4). The first two models (MV model ICU-1 and SUR-1; based on same variables) were developed to predict ICU need, built on clinical variables and demographics, without laboratory parameters. The third and fourth models (MV model ICU-2 and SUR-2) were based on clinical data and demographics plus laboratory parameters. In the multivariate model ICU-1; age, male sex, active cancer, baseline saturation on room air lower than 90% were noted to be significant independent predictors. The probability of the model was tested with ROC analysis, and the AUC value was noted to be 0.878 (Fig. 2). The same parameters were also modelled for predicting mortality (MV model SUR-1), found to be independent and significant. The latter was also tested with ROC analysis and AUC value was 0.882 (Fig. 2).
Third model and fourth model (named model-ICU-2 and model-SUR-2, respectively) were developed by investigating significant blood parameters and clinic-demographic data. In model-ICU-2, older age, male sex, need for supplemental oxygen during the first 48 hours after admission, lower sodium and albumin level were significant and independent predictors for ICU need. Having a lymphocyte count lower than 800 was not independently significant but contributed to the model. The probability of the model was tested with ROC analysis and AUC value was 0.938. In model-SUR-2, older age, gender, active cancer, higher BUN, and lower albumin levels were noted to be significant independent predictors; however, hypertension was not found to be significant but has contributed to the model positively. AUC value of the model-SUR-2 was 0.929 (Fig. 2).
Discussion
In this study, we tested the extent to which clinical, demographic, and routine laboratory parameters predicted the poor outcomes, represented as the need for intensive care and in-hospital mortality in a group of patients being treated for non-critical COVID-19 pneumonia in wards. According to these new models, besides older age and male sex, independent predictors for ICU requirement were the need for oxygen support upon admission, and lower sodium and albumin levels. On the other hand, independent predictors for in-hospital mortality included confounding active cancer, the need for oxygen support, lower albumin, and higher blood urea nitrogen levels.
Previous studies have reported descriptive, predictive, and prognostic models based on many parameters from routine blood tests, radiological findings, medical history, and symptoms [11, 19, 20]. The best-known scoring systems include ISARIC-4c score, COVID-GRAM score, and quick COVID-19 Severity Index (qCSI) [13, 21, 22]. NEWS score, which was validated for adult patients to predict unanticipated ICU admission or death was also tested and modified for COVID-19 patients [23]. These scores were also compared in one large-scale study [24]. However, none of those developments have been capable of slowing down global efforts to search for a practical prediction tool yet.
Active cancer is the most powerful predictive factor for poor outcomes among comorbidities, which is also consistent with the COVID-gram critical illness Risk Score [13]. Upon admission, the need for oxygen support upon admission was an independent and powerful factor for poor outcomes in both endpoints. Recently introduced models also emphasized the predictive factor for baseline oxygen saturation and the need for supplemental oxygen [21, 25]. Low oxygen saturation may reflect the extent of the alveoli-capillary unit destruction, as some patients might not always respond to non-pressurized nasal oxygen support since damaged areas of the lung could cause shunting of non-oxygenated blood from right-to-left, and result in ventilation-perfusion (V/P) mismatch [26, 27]. Extended thrombosis in aerated regions may also be responsible for V/P mismatch and can be found with right-to-left shunts [27, 28].
Among our findings, increased troponin level was not a significant independent predictor; however, the addition of the serum troponin level to the multivariate model increased the strength of the prediction ability. The interaction between the virus and the cardiovascular system has been complex, ranging from microvascular thrombosis to inflammatory myocarditis [29, 30]. The most interesting point is that even mild increases in troponin levels without overt signs or clues of a myocardial injury can be predictive of poor outcomes [31].
Another finding which needs to be highlighted was the difference in the predictors between the two models (ICU and mortality). Significant factors predicting the need for intensive care were more likely to be laboratory parameters. In contrast, parameters predicting in-hospital mortality were more likely to be pre-existing illnesses, including active cancer and arterial hypertension. This difference reflects the fact that some ICU admission might have been influenced by laboratory findings (such as; uremia, high ferritin, hyponatremia, low fibrinogen, etc.). Nevertheless, higher blood urea nitrogen and lower albumin levels on admission were also independent factors for in-hospital mortality. Low albumin can be an indicator of a couple of ongoing processes. First of all, a patient presented with lower albumin levels might have poor nutritional status. One study showed that elderly patients are more likely to be malnourished and have lower serum albumin levels on admission [32]. Lower serum albumin level is also associated with increased catabolism, decreased hepatic albumin synthesis, and increased capillary permeability [33]. All these conditions can be associated with poor prognosis in patients regardless of disease state and the predictive value of low serum albumin was appreciated by recent studies [34,35,36,37]. In the present study, the linear association of lower serum albumin levels and poor prognosis in COVID-19 patients (both ICU transfer and in-hospital mortality) has been very well demonstrated and may potentially increase the foresight capability of physicians.
Mortality seems to be predicted by increased BUN levels, as well, and this finding is consistent with COVID-19 literature [38,39,40]. Some of the easy-to-use nomograms include serum BUN levels [15, 41]. As being one of the most validated scoring systems, the ISARIC-4C tool also includes serum BUN level [21]. Serum BUN level may not be the best surrogate marker of kidney dysfunction but is almost always found to be increased in case of poor perfusion of the kidneys, mild-to-profound dehydration, increased catabolic processes, and can be potentially an early warning parameter for clinical deterioration.
Our work has several limitations. First of all, this was a single-center study. Secondly, the lack of validation makes the model questionable, even though six different prediction tools based on mentioned models are being reviewed under the internal validation process. The third limitation, participants weren’t vaccinated at the study time and joined our cohort before variants arose. Therefore the risk factors and the models described during this study have not been tested on subjects outside of these particular circumstances.
Conclusion
Even though some overt prognostic factors exist, the severity and progression of the disease remain somewhat unpredictable. Patients who are not elders, co-morbid, or critical upon admission are also highly susceptible to misjudgment. So, we demonstrate the impact of independent predictive factors which can be easily obtained and may lead to clinicians attending to high-risk patients on the proposed model more intensively.
References
Cheng S, Wu D, Li J et al (2020) Risk factors for the critical illness in SARS-CoV-2 infection: a multicenter retrospective cohort study. Respir Res 21(1):277
Huang C, Wang Y, Li X et al (2020) Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395(10223):497–506
Wang D, Hu B, Hu C et al (2020) Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA 323(11):1061–1069
Macedo A, Gonçalves N, Febra C (2021) COVID-19 fatality rates in hospitalized patients: systematic review and meta-analysis. Ann Epidemiol 57:14–21
Wang C, Horby PW, Hayden FG, Gao GF (2020) A novel coronavirus outbreak of global health concern. Lancet 395(10223):470–473
Li LQ, Huang T, Wang YQ et al (2020) COVID-19 patients’ clinical characteristics, discharge rate, and fatality rate of meta-analysis. J Med Virol 92(6):577–583
Weiss P, Murdoch DR (2020) Clinical course and mortality risk of severe COVID-19. Lancet 395(10229):1014–1015
Zhou F, Yu T, Du R et al (2020) Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 395(10229):1054–1062
Hadjadj J, Yatim N, Barnabei L et al (2020) Impaired type I interferon activity and inflammatory responses in severe COVID-19 patients. Science (New York, NY) 369(6504):718–724
Han H, Ma Q, Li C et al (2020) Profiling serum cytokines in COVID-19 patients reveals IL-6 and IL-10 are disease severity predictors. Emerg Microbes Infect 9(1):1123–1130
Heller RA, Sun Q, Hackler J et al (2021) Prediction of survival odds in COVID-19 by zinc, age and selenoprotein P as composite biomarker. Redox Biol 38:101764
Cummings BC, Ansari S, Motyka JR et al (2021) Predicting intensive care transfers and other unforeseen events: analytic model validation study and comparison to existing methods. JMIR Med Inform 9(4):e25066
Moreno-Pérez Ó, Andrés M, León-Ramirez JM et al (2021) The COVID-GRAM tool for patients hospitalized with COVID-19 in Europe. JAMA Intern Med. https://doi.org/10.1001/jamainternmed.2021.0491
Safdari R, Rezayi S, Saeedi S et al (2021) Using data mining techniques to fight and control epidemics: a scoping review. Health Technol. https://doi.org/10.1007/s12553-021-00553-7
Cheng A, Hu L, Wang Y et al (2020) Diagnostic performance of initial blood urea nitrogen combined with d-dimer levels for predicting in-hospital mortality in COVID-19 patients. Int J Antimicrob Agents 56(3):106110
Yao Z, Zheng X, Zheng Z et al (2021) Construction and validation of a machine learning-based nomogram: a tool to predict the risk of getting severe coronavirus disease 2019 (COVID-19). Immun Inflamm Dis 9(2):595–607
World Health Organization. COVID-19 Clinical Management: Living Guidance 2021 [January 25, 2021]. Available from: https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2021-1.
T.C. Sağlık Bakanlığı. COVID-19 Tedavi 2020 [updated July 2, 2020]. Available from: https://covid19.saglik.gov.tr/TR-66299/covid-19-tedavi.html.
Velavan TP, Meyer CG (2020) Mild versus severe COVID-19: laboratory markers. Int J Infect Dis 95:304–307
Xie J, Wang Q, Xu Y et al (2021) Clinical characteristics, laboratory abnormalities and CT findings of COVID-19 patients and risk factors of severe disease: a systematic review and meta-analysis. Ann Palliat Med 10(2):1928–1949
Knight SR, Ho A, Pius R et al (2020) Risk stratification of patients admitted to hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: development and validation of the 4C Mortality Score. BMJ (Clinical research ed) 370:m3339
Rodriguez-Nava G, Yanez-Bello MA, Trelles-Garcia DP et al (2021) Performance of the quick COVID-19 severity index and the Brescia-COVID respiratory severity scale in hospitalized patients with COVID-19 in a community hospital setting. Int J Infect Dis 102:571–576
Volff M, Tonon D, Bourenne J et al (2020) No added value of the modified NEWS score to predict clinical deterioration in COVID-19 patients. Anaesth Crit Care Pain Med 39(5):577–578
Cheng F-Y, Joshi H, Tandon P et al (2020) Using machine learning to predict ICU transfer in hospitalized COVID-19 patients. J Clin Med 9(6):1668
Puah SH, Young BE, Chia PY et al (2021) Clinical features and predictors of severity in COVID-19 patients with critical illness in Singapore. Sci Rep 11(1):7477
Lang M, Som A, Mendoza DP et al (2020) Hypoxaemia related to COVID-19: vascular and perfusion abnormalities on dual-energy CT. Lancet Infect Dis 20(12):1365–1366
Santamarina MG, Boisier D, Contreras R et al (2020) COVID-19: a hypothesis regarding the ventilation-perfusion mismatch. BioMed Central. https://doi.org/10.1186/s13054-020-03125-9
Busana M, Giosa L, Cressoni M et al (2021) The impact of ventilation–perfusion inequality in COVID-19: a computational model. J Appl Physiol 130(3):865–876
Bavishi C, Bonow RO, Trivedi V et al (2020) Special article—acute myocardial injury in patients hospitalized with COVID-19 infection: a review. Prog Cardiovasc Dis 63(5):682–689
Hu H, Ma F, Wei X, Fang Y (2021) Coronavirus fulminant myocarditis treated with glucocorticoid and human immunoglobulin. Eur Heart J 42(2):206
Hui H, Zhang Y, Yang X et al (2020) Clinical and radiographic features of cardiac injury in patients with 2019 novel coronavirus pneumonia. MedRxiv. 5:372
Li T, Zhang Y, Gong C et al (2020) Prevalence of malnutrition and analysis of related factors in elderly patients with COVID-19 in Wuhan, China. Eur J Clin Nutr 74(6):871–875
Soeters PB, Wolfe RR, Shenkin A (2019) Hypoalbuminemia: pathogenesis and clinical significance. J Parenter Enter Nutr 43(2):181–193
de la Rica R, Borges M, Aranda M et al (2020) Low albumin levels are associated with poorer outcomes in a case series of COVID-19 patients in Spain: a retrospective cohort study. Microorganisms 8(8):1106
Paliogiannis P, Mangoni AA, Cangemi M et al (2021) Serum albumin concentrations are associated with disease severity and outcomes in coronavirus 19 disease (COVID-19): a systematic review and meta-analysis. Clin Exp Med. https://doi.org/10.1007/s10238-021-00686-z
Aziz M, Fatima R, Lee-Smith W, Assaly R (2020) The association of low serum albumin level with severe COVID-19: a systematic review and meta-analysis. Critical care (London, England) 24(1):255
Huang J, Cheng A, Kumar R et al (2020) Hypoalbuminemia predicts the outcome of COVID-19 independent of age and co-morbidity. J Med Virol 92(10):2152–2158
Gao S, Jiang F, Jin W et al (2020) Risk factors influencing the prognosis of elderly patients infected with COVID-19: a clinical retrospective study in Wuhan, China. Aging (Albany NY) 12(13):12504–12516
Li Z, Wu M, Yao J et al (2020) Caution on kidney dysfunctions of COVID-19 patients. medRxiv. 12:48
Cheng Y, Luo R, Wang K et al (2020) Kidney impairment is associated with in-hospital death of COVID-19 patients. medRxiv. 69:752
Liu Q, Wang Y, Zhao X et al (2021) Diagnostic performance of a blood urea nitrogen to creatinine ratio-based nomogram for predicting in-hospital mortality in COVID-19 patients. Risk Manag Healthc Policy 14:117–128
Acknowledgements
We would like to thank Banu Çakır, MD, and Mithat Temizer, MD, for technical support and sharing wisdom. This study was not funded by any institution and was carried out by the endless efforts of the study team. We also would like to thank Isaac Bochay Drum, a native speaker from Illinois, United States of America, for checking grammar and correcting spells.
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
NÇB and GSG conceptualized and designed the study, THŞ, BÖ, HO, and LÖ collected the data, OAU, MDT and MÖ analysed the data, text was written by MÖ. All authors reviewed and approved the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Authors have no competing interests to declare.
Financial interests
The authors declare they have no financial interests.
Ethical Approval
This study was conducted in accordance with principles defined in the Declaration of Helsinki and International Conference on Harmonization Good Clinical Practice guidelines, and approved by the relevant institutional ethics committee (31.03.2020, GO 20/354, 2020/07-33).
Human and animal rights statement
This article does not contain any studies with animals performed by any of the authors.
Consent to participate
Informed consent was obtained from each participating patient at the Hacettepe University, Ankara.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Başaran, N.Ç., Özdede, M., Uyaroğlu, O.A. et al. Independent predictors of in-hospital mortality and the need for intensive care in hospitalized non-critical COVID-19 patients: a prospective cohort study. Intern Emerg Med 17, 1413–1424 (2022). https://doi.org/10.1007/s11739-022-02962-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-022-02962-6