Abstract
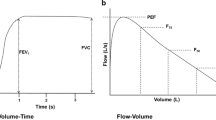
Single breath counting (SBC) is the measurement of how far an individual can count in cadence with a metronome set at 2 beats per second in a normal speaking voice following a maximal effort inhalation. Previous work has demonstrated that it correlates well with standard measures of pulmonary function. The objective of this study is to derive a “normogram” of healthy children showing the expected SBC value as a function of easily measured physiologic parameters (age, gender, height, and weight). This was a prospective observational study of a convenience sample of healthy children presenting for well-child checks or non-respiratory complaints at a large tertiary care center. Correlation was determined by the Pearson’s product correlation coefficient (r) and r 2 determined as a measure of shared variance. Multiple regression analysis was performed on demographic data to determine a best linear fit with calculation of the coefficient of determination (R 2). A total of 105 children served as the basis for analysis; 54 (51.4 %) were male and average age was 9.7 (median 10, range 3–15) years. For both males and females, height correlated most strongly with SBC score (r = 0.730 and 0.725, respectively). In both genders, height alone accounted for more than 50 % of the observed variance in the results (r 2 = 0.533 and 0.526, respectively). Breath counting, an easy to perform test that appears to correlate well with standard measures of pulmonary function and shows promise for measuring asthma severity in children. We present an equation for predicting normal results (a “normogram”).


Similar content being viewed by others
References
Ali S, O’Connell C, Kass L, Graff G (2011) Single breath counting: a pilot study of a novel technique for measuring pulmonary function in children. Am J Emerg Med 29(1):33–36
Enright PL, Lebowitz MD, Cockroft DW (1994) Physiologic measures: pulmonary function tests: asthma outcome. Am J Respir Crit Care Med 149:9–18
Klein RB, Fritz GK, Yeung A, McQuaid EL, Mansell A (1995) Spirometric patterns in childhood asthma: peak flow compared with other indices. Pediatr Pulmonol 20:372–379
National Asthma Education and Prevention Program Expert Panel Report 2 (1997) Guidelines for the diagnosis and management of asthma. National Asthma Education Program, Office of Prevention, Education, and Control, National Heart, Lung and Blood Institute, National Institutes of Health, Bethesda, Publication no. 97-4051
Miller MR, Crapo R, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, Enright P, van der Grinten CP, Gustafsson P, Jensen R, Johnson DC, MacIntyre N, McKay R, Navajas D, Pedersen OF, Pellegrino R, Viegi G, Wanger J, ATS/ERS Task Force (2005) General considerations for lung function testing. Eur Respir J 26(1):1–2
Li TCJ (1995) Home peak expiratory flow rate monitoring in patients with asthma. Mayo Clin Proc 70:649–656
Sly PD, Cahill P, Willet K, Burton P (1994) Accuracy of mini peak flow meters in indicating changes in lung function in children with asthma. Br Med J 308:572–574
Nemr E, Ben Y, Laura H, Martha E, Shahid S (2000) Can peak expiratory flow predict airflow obstruction in children with asthma? Pediatrics 105:354–358
Saetta M, Thienne G, Crescioli S, Fabbri LM (1989) Fatal asthma in a young patient with severe bronchial hyperresponsiveness but stable peak flow records. Eur Respir J 2:1008–1012
Ferguson AC (1988) Persisting airway obstruction in asymptomatic children with asthma with normal peak expiratory flow rates. J Allergy Clin Immunol 82:19–22
Bartfield JM, Ushkow BS, Rosen JM, Dylong K (1994) Single breath counting in the assessment of pulmonary function. Ann Emerg Med 24:256–259
Ushkow BS, Bartfield JM, Reicho PR, Raccio-Robak N (1998) Single-breath counting for the assessment of bronchospastic patients in the ED. Am J of Emerg Med 16:100–101
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Statement of human and animal rights
This study was approved by our Institutional Review Board.
Informed consent
Informed consent or assent was obtained from all subjects.
Rights and permissions
About this article
Cite this article
Kass, L.E., Putnam, K. Single breath counting for the evaluation of pediatric respiratory function: derivation of a “normogram”. Intern Emerg Med 11, 225–228 (2016). https://doi.org/10.1007/s11739-015-1316-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-015-1316-3