Abstract
The present-day patients have complex diseases that are responsible for the great increase of medical interventions, overcrowding in emergency departments and access to the wards, increased waiting times and length of stay, difficult discharge, increased readmission rate and finally increased mortality. By breaking the steps of the patients pathways it allows us to simplify the problems and to face the individual aspects of the complexity related to the management of patients in the hospital. One solution that has been growing in popularity is the rapid intensive observation of the patients in acute hospital setting within Internal Medicine wards. This model has been otherwise defined with different terminology, but the most widely used name is Acute Medical Unit (AMU). We describe the model of an AMU within an Internal Medicine department as proposed and adopted in Anglo-Saxon countries, the methods of clinical approach and the practical organisation of the units in close collaboration with the ED ward. Finally we report our experience at an Internal Medicine department in Padova and the initial results obtained during the first 4 months of the project. Our approach of intensive rapid observation of intermediate risk patients admitted from the ED led to a significant reduction in the duration of hospitalization, without increasing readmission rate after discharge and fatality rate. Factors significantly associated to a short hospital stay were a preserved function and a lower number of previous admissions to the hospital. Several gray zones in the realisation and management of the project were identified and the possible solutions are still matter of discussion and debate.
Similar content being viewed by others
Complexity in medicine
Patients and hospitals are complex systems. Doctors and managers understand bits and pieces of the world around them but when it comes to real life, things often happen in ways that they could not have predicted [1–4]. Many scientists have experienced the same phenomenon in their research and realised that the knowledge of parts of a system often does not provide a clear view of the overall scenario. The term “complex system” means that the parts of a system are linked in ways that creates a whole, with properties above and beyond those of the individual parts [5]. Although our knowledge is starting and is grounded on the understanding of the single parts of the reality and on how each part works in isolation of other parts, this does not help to understand how the whole system works together. Knowing and working with complex systems goes against traditional science practice, defined as reductionism [5]. Holistic approach means bringing the pieces of the puzzle together, in order to understand how the whole system works. The science of the complex systems has to be considered as in a continuous swing and wondering from breaking things down into smaller and smaller components, as the subatomic physics, and understand interactions between components of the different systems, in a more global vision.
Today’s patients are complex systems, meaning that any reality, either normal or modified by intrinsic or extrinsic factors exhibits matter of complexity. Indeed in the last few decades a growing population of patients has been assuming specific connotations of complexity, as they suffer from multiple stable or unstable chronic diseases, are often, although not always, advanced in age [6], are taking several drugs, are frail, less autonomous, are living alone, often assisted by a foreigner caregiver, with scarce emphatic relationship, being their relatives remote or absent. These features linked together have originated a new biotype, a clinical entity not described in the textbooks of medicine. Geriatricians have described several methods of multidimensional system evaluation of this new biotype, with specific attention to frailty and disability. However their methodology is yet lacking of an adequate clinical approach and rapid stabilization of organ decompensation [7]. Multimorbidity, frailty and disability are responsible for increased request of medical interventions both in and out of the hospital, as in outpatient clinics and in territory services, with a continuous raising of the cost of care. Moreover these pathologies cause the inexorable rise in the numbers of patients presenting to hospital emergency departments, with consequent overcrowding, inefficacy of care delivery and increased risk of medical error and complications. The new biotype is responsible for the increased length of stay in the hospital, that may be longer than necessary, difficult discharge, increased use of hospital resources, reduced patient relatives and staff satisfaction, increased waiting times and access block in the emergency department, increased readmission rates and finally increased mortality [8–11]. The complexity of the aforementioned situation is related not only to the epidemiological and organizational aspects of modern medicine, but also to the specific problems related to the doctor and nurse work that reflect an inadequate care and cure of the patients, due to partial competences and expertise in the multimorbidity approach, inadequate and excessive use of drugs, a prevalent highly specialized education and culture, with an exaggerated use of technologic resources in the diagnostic approach and therapeutic interventions. Internal Medicine and Geriatric departments wards are the main theatres of the manifolds aspects of the complexity of the patients and of the hospitals.
By breaking the steps of the patient pathways, hospitals and schools of medicine need to consider structural reform for optimizing evaluation, treatment and subsequent transfer of care to patients admitted to the hospital with acute problems, in order to (1) reduce inpatient admission if possible, (2) reduce the length of stay, (3) adopt a more rational methodological and clinical problem-based approach, (4) discharge patient to the most suitable post acute care setting [12].
In the last decade these problems have been largely debated in internal medical journals all over the world and the key words that can be extrapolated from the published papers are: “acute access block, overcrowding, length of stay, inefficiencies in service delivery, complex elderly, low patient satisfaction”, and in addition “the need of a clinical revolution, a new model of care, whole of hospital response, change in clinical culture within hospitals, flexibility, new style of physician”, etc. [11, 13–20].
One solution that is growing in popularity is the rapid intensive observation of the patients within acute hospitals in Internal Medicine wards, with their rapid discharge. This activity has been otherwise defined with different terminology and synonymous names, including Acute Medical Units (AMU), Acute Medical Care (AMC), Acute Medical Assessment Unit (AMAU), Medical Assessment and Planning Units (MAPU), Acute Medical Wards (AMW), Acute Planning Units (APU), Rapid Assessment Medical Units (RAMU), Early Assessment Medical Units (EAMU), Intermediate Care Units (ICU), Rapid Intensive Observation (RIO), Urgency Medicine (UM) [13, 21, 22].
The model of Acute Medical Care in Internal Medicine
The Acute Medical Unit is characterized by a rapid medical observation and evaluation of acute patients with subsequent stabilization and rapid discharge. A recent systematic review has defined the unit as: “designated hospital wards specifically staffed and equipped to receive medical inpatient presenting with acute medical illness from emergency department and/or the community for expedited multidisciplinary and medical specialist assessment, care and treatment for up to a designated period (typically between 24 and 72 h) prior to discharge or transfer to medical wards” [13]. Promising new models of hospital care for assessing and managing patients presenting to the emergency department with acute medical conditions have been systematically adopted in the last decade in UK, Australia and New Zealand, although some differences have been emphasized between the British and Australian systems for managing emergency medical patients [23]. In the United States the system of intermediate units has been introduced over two decades ago with the goal of increasing the availability of intensive care beds and reducing or eliminating intensive care admissions for patients at low risk for serious morbidity or mortality conditions [21, 22, 24].
All the proposed units are aimed at going beyond the functionality of a traditional medical ward, where the progression of the patient journey may be dependent on a single morning visit of the structured physician and the diagnostic and therapeutic working plan is diluted over the days or weeks, also in relation to the multimorbidity and difficulty to discharge. Medical assessment in the AMU is immediately performed at patient admission by structured physicians with several years of experience in Internal Medicine and with an interest in acute general medicine [13, 25]. Thereafter the patient is supervised by the same consultant, performing at least two daily rounds. Clinical assessment and diagnostic pathways are carried out with the active participation of postgraduate students of the Internal Medicine and of the Emergency and Urgency Specialties, whose presence and control of clinical parameters of patients are warranted during the entire day. Obviously the structure and operational policy and medical organization of individual units varies locally, in relation to administrative, medical and nurse resources. Some units have developed standardized diagnostic and therapeutic regimens or protocols, with prioritized access to diagnostic services, mainly radiology and cardiovascular. All acutely ill patients are potentially eligible for AMU entry, with the exception of those with marked clinical instability, immediate specialized needs (such as Acute Coronary Unit, Stroke Unit, Dialysis), and those presentating for social or residential care, or with severe behavioural disturbance. A recent survey conducted in Australia and New Zealand in 32 hospitals where the AMU has been activated in the last 2 years suggests that, despite some variation in staffing and procedures, AMU seems to be well established and a promising mean for decreasing ED access block [16]. In the USA the Society of Critical Care Medicine has proposed guidelines on admission and discharge for Adult Intermediate Units [21]. These units are specifically designated to admit patients not requiring intensive care, but needing more intensive care than that provided in a general ward. These patients may require frequent monitoring of vital signs and/or nursing interventions, but usually do not require invasive monitoring. Intermediate care areas can be represented as multipurpose progressive care units, conducted by Internal Medicine doctors, or as a single-organ subspecialty divisions such as cardiac, surgical or neurologic units or chronic ventilator respiratory care units. The intermediate care unit concept has been suggested as a strategy that promotes grater flexibility in patient triage, increases accessibility to limited intensive care and provides a cost effective alternative to critical care unit admission, particularly for patient with a low or intermediate risk, but potential for major complications and who have been admitted for routine monitoring [21].
Although the assumptions of the validity of AMU are clear and undisputed, the evidence on the efficacy remains limited, and no controlled trials have been reported to date, as recently claimed by Scott et al. [13]. The authors underlined that “to date there has been no formal investigation of the effect of AMUs on the quality of life in regards to the disease specific process of care indicators, hospital costs and resources related to actual budgetary expenditures or on continuity of care and communication involving referring general practitioners or other community-based health professionals” [13]. Similar considerations have been made earlier by NIH researchers, in relation to the activation of intermediate care in USA. They claimed that clear-cut demonstration of therapeutic efficacy of intermediate care, namely mortality and morbidity, is a much more difficult task, as physicians and patients are reluctant to participate in studies that randomize patients to intermediate units versus hospital floors. Indeed the study available is an evaluation of case fatality rates after the introduction of the intermediate care unit [22]. Nevertheless, the conclusion of the aforementioned systematic review [13] was for a benefit of the Acute Medical Unit model in terms of reduced in hospitalization and increased direct discharge rates, improved efficiency of hospital resources and greater patient satisfaction. From this analysis it also emerges that on average 70% of patients presenting to the ED with acute medical illness will be eligible for admission to AMU and that between 20 to 50% of these patients will be dischargeable within 48 h. Recent investigations have identified several factors predicting a hospital stay up to 3 days among older patients, such as preserved function (measured using the modified Barthel Index), absence of delirium, as well as of infection, anaemia, gastrointestinal disorders and stroke. These individuals are more likely to have a short length of stay and therefore more suitable for admission to the AMU [26].
Methods and organisation
We became interested in the rapid evaluation of acute patients admitted from emergency department to our Internal Medicine unit in the light of several positive factors. First, our interest in complexity in Internal Medicine patients, in consideration of the clinical discipline that, by definition, evaluates the patient in his/her globality and not by singular organs or systems. Second, the problem of the method in Internal Medicine, that is the rational use of the clinical thinking in the evaluation of the patient itself in order to select the best medical decision to obtain the most probable diagnosis and apply the best treatment. Third, the presence of a postgraduate specialty course in Emergency and Urgency Medicine and Fourth, an active collaboration with the Department of Emergency Medicine that is under the hospital administration, but has established experience in teaching emergency medicine in all the Veneto Region and has an intensive collaboration with academic medicine and undergraduate and postgraduate medical and surgical courses for students and fellows.
Our main aims were to improve the management of the patients admitted from the ED and to optimize the clinical approach to the patient affected by acute illness. These two goals imply a better admission organization and an improvement of the clinical and methodological evaluation of the patient in his/her acute symptoms.
The clinical approach used was the same that has been used facing the patient in general and Internal Medicine contest [27, 28], that is the problem-based solving approach, with an early identification of the main problem of the patient, formulation of one or more hypothesis to try the best solution of the problem and thereafter to exclude or to confirm the hypothesis, by means of diagnostic tests selected on the basis of their sensitivity and specificity. The methodology used in ED was the same as that of Internal Medicine ward [29], the main difference being the limited time of the emergency physician (EP). Time constraints occur because of the severity and acuity of the illness and also because of the ever-present worry that someone else will need the physician’s attention [30]. The second challenge for emergency physicians is that they need to quickly assess and make therapeutic decisions on the basis of limited information. The main concern of the EP is not necessarily the diagnosis, but a process of thinking aimed at ruling out or ruling in serious pathology that could be life threatening. The classical model of history taking, followed by a physical examination and then diagnostic testing must often be compressed and conducted simultaneously when time is limited and the patient’s life is threatened. If this is the method of the EP, the same method should be used in the ward when a stabilized patient presents an emergency. In these situations the first and the most important question to answer is: Is the patient about to die ? that means that the patient is dying or moribund, or that he can or could die. Thus patient’s presentation is prioritized to one of the following [30]:
-
1.
Emergent, critical unstable patient, who is dying. This indicate an emergency; the patient has symptoms consistent with a life-threatening illness or injury, with a high probability of death if immediate intervention is not begun.
-
2.
Urgent, critical stable patient, who can die. Patient has symptoms of illness or injury that may progress in severity if a rapid diagnosis is not done or excluded and if treatment is not begun quickly.
-
3.
Non urgent, not critical patient. Patient has symptoms that have a low or very low probability of progression towards a more serious condition.
Thus the physician has to be guided by the symptom of a life-threatening emergency and not by the immediate search of a specific disease entity, and has to anticipate impending life-threatening emergencies in the apparently stable patient. This process may be immediate or may require time. The process is immediate when the vital signs are compromised, requiring as mandatory an immediate lifesaving intervention. The process is also immediate if the main symptom of the patient, supported by sensitive and specific laboratory tests, guides to a life threatening condition. In these cases the Bayesan method is relevant: the pre test probability becomes higher than the treatment threshold, or lower than the test threshold after application of the most sensitive or specific test, able to rule in or rule out the hypothetical disease. For example, in pulmonary embolism these figures were suggested in a treatment threshold of 85% and in a test threshold of 5% [31]. However the process could be not so immediate, in the case of stable although critical patients, that is with patients that are apparently well, but have symptoms (e.g. chest pain) that may progress in severity (e.g. acute coronary syndrome). These patients are classified as patients with an intermediate risk of serious illness. What is the best decision for this category of patients? They cannot be discharged, being the risk of serious disease still present; they cannot be admitted to the general or specific intensive care ward, since this would be an improper admission, nor they can be admitted to a general Internal Medicine ward, because the admission is not adequate for a patient that could become suddenly unstable. This kind of patients need a prolonged observation in a dedicated unit; the best place for them is the Acute Medical Unit, also known as Intermediate Care Unit or Rapid Intensive Observation (RIO) Unit, for a period of time that in general does not exceed 72 h, that is a period of time sufficiently long to allow progression of a possible acute disease and sufficiently short to improve the process of admission and discharge of the patients. The principal aims of the prolonged observation are to exclude severe diseases, to stabilize the patient and to program further clinical and laboratory evaluations in order to better define the presence of other diseases and the appropriate treatment.
It is noteworthy that the Italian Ministry of Health have recently published a document where care systems of prolonged observation are indicated as mandatory in Emergency Department and in Internal Medicine wards [32]. The systems are indicated as Short Intensive Observation, where patients are observed for a period of less than 24 h in the contest of ED, and subsequently discharged or admitted in a second system named Urgency Medicine, that is similar to AMU or to RIO Unit, located in an Internal Medicine contest. Patients are observed during a period of 72 h, and evaluated for exclusion of life-threatening diseases, mainly applying the method of Bayes: when needed, further diagnostic tests will be performed after discharge.
Our experience of Acute Medical Unit in Internal Medicine
The aim of our project was to manage some acute clinical problems during a short-term hospitalization (72 h). To this end, we first identified some clinical problems, each representing the chief complaint experienced by the patients admitted to ED. These problems are not immediately resolved by the physicians and require a period of further observation, being the patients at intermediate risk of evolution to severe pathology. This further observation period of the patients could be done in a RIO stay, made in an AMU, after their discharge from the ED.
Inclusion criteria in the RIO Unit
The medical problems, defined in agreement with the Emergency Department Physicians, after extensive revision of the literature and practical considerations, were the following: (1) low-intermediate risk chest pain based on TIMI score; (2) heart failure (NYHA class II and III); (3) stable supra-ventricular arrhythmias; (4) syncope; (5) deep vein thrombosis at high risk for pulmonary embolism; (6) bronchial asthma; (7) allergies; (8) neoplastic and non-neoplastic pain; (9) acute inflammatory states; (10) acute hypo and hyperglycemia; (11) vertebral fragility fractures; (12) abdominal pain; (13) electrolyte disorders and dehydration; (14) mental confusion.
For each category, a diagnostic flow-chart was defined, specifying the tests that had to be performed in the ED before the patients were sent to our unit. An important aspect of the active collaboration with the ED physicians was the immediate discussion of each clinical case, made generally by phone, before admitting the patient to the RIO Unit.
Organization of the RIO unit
Based on an estimation of the expected number of patients accessing the ED with the aforementioned clinical problems, we dedicated 18 out of 45 beds of our Internal Medicine Unit (Clinica Medica 1) to the RIO care and the remaining 27 beds to regular care Internal Medicine patients. The organization of the two sections was separate as far as medical and nurse staff. The dedicated staff was responsible for:
-
1.
Defining specific diagnostic and therapeutic protocols for the identified clinical acute conditions based on current international guide-lines.
-
2.
Implementing diagnostic procedures to be performed in the unit, including echocardiography, ECG Holter, Stress test, 24 h blood pressure monitoring, thoracic and abdominal ultrasound, angiologic echo color doppler.
-
3.
Defining fast access to cardiology, radiology and endoscopy services.
-
4.
Designing a specific electronic chart record.
-
5.
Establishing a database of data collection for outcome analysis.
Methods of clinical approach
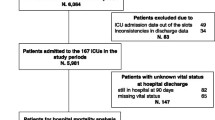
The acute patient that, after the triage process in the ED, has been considered eligible, was admitted in our RIO Unit for the rapid intensive observation (Fig. 1). During hospital stay, the patient is immediately evaluated for his main clinical problem and the degree of clinical and functional instability is defined. Life-threatening conditions are excluded by clinical examination, laboratory and instrumental tests, according to the methodology previously described. After clinical stabilization, the patient undergoes the diagnostic and therapeutic procedure, based on established protocols. In addition, the presence and severity of associated diseases are considered by means of the CIRS Comorbidity and Severity Scores. Upon resolution of the acute medical problem the patient is discharged within 72 h; when this is not possible (i.e. clinical instability or indication for immediate invasive diagnostic and therapeutic procedures), the patient remains admitted and transferred to the Internal Medicine Unit (Fig. 2).
Results
During the first 4 months of the project (February 1st–May 31st 2011), 259 RIO patients (130 M and 129 F) were admitted in our unit. Mean age was 63 ± 16 years. The clinical problems leading to admission are summarized in Table 1. As showed, the majority of patients were admitted for chest pain (42%); interestingly, 13% of the patients were admitted for “other” causes, suggesting that, once the doctor is in the mind-frame of a rapid evaluation and a short hospitalization (i.e. RIO), additional clinical conditions could be considered and managed within a RIO model.
The overall mean duration of hospital stay was 4.1 ± 3.4 days; 65% of the patients fulfilled the criteria for RIO patients and were discharged within 72 h, with a mean hospital stay of 2.4 ± 0.7 days. In the remaining 35% of the patients, who required more than 72 h of hospital stay (RIO-failures), the mean duration of hospitalization was 7.4 ± 4.1 days. Patients discharged within 72 h were younger, had a higher Barthel Index at admission and a significantly lower CIRS Severity Score. Furthermore, the number of previous admissions and of current medications was lower in these patients as compared with RIO-failures. One patient died during hospitalization in the RIO-failure group. The number of re-admissions during this short-term period of observation was similar in the two groups (Table 2).
The likelihood of becoming a RIO-failure patient was significantly affected by the Barthel Index and the CIRS Severity Score at admission, after adjusting for age, gender, CIRS Comorbidity Score, number of previous admissions and medications (Table 3).
Conclusions
The results presented in this report are obviously preliminary. A great effort and time was devoted to the discussion of the project first of all with the direction of the hospital and thereafter with the colleagues of the ED who are in charge of evaluating all the patients admitted to the hospital of Padova. After agreeing on the adequacy, quality and reliability of the project, as well as of its clear potential benefit in terms of cost, we had the approval by the direction of the hospital and obtained some limited resources in terms of nursing staff and technical devices. After approval of the project, we had several meetings with our colleagues in the Internal Medicine Division and with residents and fellows, as well as with nurse staff in order to establish a dedicated medical and nurse team, to define the diagnostic and therapeutic protocols for the different clinical problems of the RIO patients and to discuss on the required change in the attitude towards this short hospitalization patients.
Our initial experience and results can be considered positive and there is general satisfaction both of the medical and nursing staff and of the general direction of the hospital. The approach of RIO has significantly reduced length of stay, is not associated with increased readmission after discharge, nor with an increased fatality rate. All the medical and care staff express their satisfaction to be involved in this new experience. The clinical approach to the patient has been gradually improved, with a better definition of the problems and a careful selection of diagnostic tests and prescription of essential drugs. Doctors and nurses become gradually more and more responsible in their decision making and conscious of the relevance of the project. As reported elsewhere [26], a preserved function and a lower number of previous admissions were factors significantly associated to a short stay.
Several grey zones still remain and need to be solved or improved. The clinical features of patients observed in ED and eligible for RIO Unit need to be better defined. A more extensive data collection will help for a better definition of comorbidity and for understanding the role of cluster of diseases in the resolution of the acute episode of illness. A better comprehensive geriatric assessment is needed to improve outcomes for frail older people. Finally a more efficient interaction with the general practitioner and with the services of the territory has been programmed. We strongly believe that an increased education of doctors and nurses and an improved organisation of the rotating shifts will reduce operating procedures delay and medical and assistance errors towards an improved a more rational approach to the patient with acute clinical problems.
References
Plsek PE, Greenhalgh T (2001) Complexity science: the challenge of complexity in health care. BMJ 323:625–628
Wilson T, Holt T, Greenhalgh T (2001) Complexity science: complexity and clinical care. BMJ 323:685–688
Morton AP (2011) Hospital safety and complexity. BMJ 342:514
Federoff HJ, Gostin LO (2009) Evolving from reductionism to holism: is there a future for systems medicine? JAMA 302(9):994–996
Mazzocchi F (2008) Complexity in biology. EMBO 9:10–14
Gore FM, Bloem PJN, Patton GC et al (2011) Global burden of disease in young people aged 10–24 years: a systematic analysis. Lancet 377:2093–2102
Diederichs C, Berger K, Bartels DB (2011) The measurement of multiple chronic disease. A systematic review on existing multimorbidity indices. J Gerontol A Biol Sci Med Sci 66(3):301–311
Centre for Clinical Practice at NICE (UK) (2007) Acutely Ill patients in hospital: Recognition of and response to acute illness in adults in hospital. London National Institute for Health and Clinical Excellence (UK) (http://www.nice.org.uk)
Royal College of Physicians (2007) Acute medical care. The right person, in the right setting—first time. Report of the acute medicine task force. London RCP
Guttman A, Schull MJ, Vermeulen MJ, Stukel TA (2011) Association between waiting times and short term mortality and hospital admission after departure from emergency department: population based cohort study from Ontario, Canada. BMJ 342:d2983
Walters EH, Dawson DJ (2009) Whole-of-hospital response to admission access block: the need for a clinical revolution. Med J Aust 191(10):561–563
Plsek PE, Wilson T (2001) Complexity, leadership, and management in healthcare organisations. BMJ 323:746–749
Scott I, Vaughan L, Bell D (2009) Effectiveness of acute medical units in hospitals: a systematic review. Int J Qual Health Care 21:397–407
Fatovich DM, Hughes G, McCarthy SM (2009) Access block: it’s all about available beds. Med J Aust 190(7):362–374
Mitra B, Cameron PA, De Villiers Smit P (2010) Whole-of-hospital response to admission access block: the need for a clinical revolution. Med J Aust 192(6):354–356
McNeill GBS, Brand C, Clark K et al (2011) Optimizing care for acute medical patients: the Australasian medical assessment unit survey. Intern Med J 41:19–26
Stott DJ, Langhorne P, Knight PV (2008) Multidisciplinary care for elderly people in the community. Lancet 371:699–700
Brillman J, Mathers-Dunbar L, Graff L et al (1995) Management of observation units. Ann Emerg Med 25:823–830
Hillman K (1999) The changing role of acute-care hospitals. Med J Aust 170:325–328
Epstein M, Barmania N, Robini J, Harbord M (2007) Reforming the acute phase of the inpatient journey. Clin Med 7(4):343–347
Nasraway SA, Cohen IL, Dennis RC et al (1998) Guidelines on admission and discharge for adult intermediate care units. Crit Care Med 26(3):607–610
Charlson ME, Sax FL (1988) Intermediate care. How do we know it works? Arch Intern Med 148:1270–1271
Jenkins PF, Barton LL, McNeill GBS (2010) Contrasts in acute medicine: a comparison of the British and Australian systems for managing emergency medical patients. Med J Aust 193(4):227–228
Franklin CM, Rackow EC, Mamdani B et al (1988) Decreases in mortality on a large urban medical service by facilitating access to critical care. Arch Intern Med 148:1403–1405
Hampton JR, Gray A (1998) The future of general medicine: lessons from an admissions ward. J R Coll Physicians Lond 32(1):39–43
Basic D, Khoo A (2009) Admission variables predicting short lengths of stay of acutely unwell older patients: relevance to emergency and medical short-stay units. Aust Health Rev 33(3):502–512
Bowen JL (2006) Educational strategies to promote clinical diagnostic reasoning. N Engl J Med 355:2217–2225
Heneghan C, Glasziou P, Thompson M et al (2004) Diagnostic strategies used in primary care. BMJ 338:b946
Realdi G, Previato L, Vitturi N (2008) Selection of diagnostic tests for clinical decision making and translation to a problem oriented medical record. Clin Chim Acta 393:37–43
Jones TR (2008) Approach to the emergency department patient. In: Stone CK, Humphries RL (eds) Current diagnosis and treatment: emergency medicine, 6th edn edn. McGraw-Hill, New York, pp 1–4
Roy PM, Colombet I, Durieux P et al (2005) Systematic review and meta-analysis of strategies for the diagnosis of suspected pulmonary embolism. BMJ 331:259–263
Ministero della Salute (2010) Documento commissione Urgenza-Emergenza. http://www.salute.gov.it/imgs/C_17_pubblicazioni_856_ulterioriallegati_ulterioreallegato_0_alleg.pdf
Acknowledgments
The authors want to thank Doctor Adriano Cestrone, General Director of the “Azienda Ospedaliera” of Padova Hospital and Doctors Giampietro Rupolo and Carla Destro, Scientific Directors of the “Azienda Ospedaliera” of Padova for their significant support and Mrs Annarosa Barbato, nurse coordinator of Clinical Medical 1 Unit and of the Acute Medical Unit of the Department of Internal Medicine for her relevant collaboration.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Realdi, G., Giannini, S., Fioretto, P. et al. Diagnostic pathways of the complex patients: rapid intensive observation in an Acute Medical Unit. Intern Emerg Med 6 (Suppl 1), 85 (2011). https://doi.org/10.1007/s11739-011-0681-9
Published:
DOI: https://doi.org/10.1007/s11739-011-0681-9