Abstract
The objectives of this study were to evaluate current robotic surgery training methodologies for ACGME-accredited obstetrics and gynecology (OB/GYN) residency programs, better understand current resident perspectives, and explore potential areas for improvement within resident education. A cross-sectional study was done of ACGME-accredited OB/GYN residents in the 2023–2024 academic year. The study was done on a national setting via web-based survey. 75 surveys were included. The study was conducted via a 33-question survey study using a mixture of multiple choice, multiple answer, and Likert scale questions. Participants noted that 98.7% of their institutions perform robotic surgery and 90.7% have access to robotic console trainers. Outside of the operating room, slightly more than half of participants (57.3%) have formalized robotics training curriculums. A variety of training modalities were noted to be utilized by residents with the most helpful being hands-on training (67.7%) followed by dual-assist console (45.6%). The least helpful was noted to be online modules (58.7%). Most residents either strongly agree (45.3%) or agree (36.0%) that standardized robotics curriculums should be implemented for all OB/GYN residency programs. The largest barriers to completion of this training were noted to be attending comfort with resident participation in the case (74.0%), personal time (58.9%), and availability or access to trainers (42.5%). A formalized and standardized robotic training curriculum should be considered for OB/GYN residents with a multi-modal model utilizing a combination of training modalities as well as dedicated didactic hours.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Robotic-assisted surgery (RAS) allows for surgeons to operate in a minimally invasive approach while having increased dexterity and range of motion due to ability to articulate wrist and hand motions [1]. Other reported advantages to robotic surgery include improved ergonomics, elimination of tremor, and improved visualization [2]. Over 11 million robotic surgeries have been performed worldwide with over 7500 platforms installed for use as of 2023 [3].
To be able to perform robotic surgeries proper training is required, but current guidelines for credentialing and privileges vary across institutions and hospitals [2]. Current guidelines exist from commercial robotics companies; however, there are no standardized curriculums for robotic training during obstetrics and gynecology residency (OB/GYN) despite the robust use of robotics systems. The American College of Obstetricians and Gynecologists (ACOG) and Society of General Surgeons (SGS) both recommend that those training requirements to include a didactic educational program as well as hands-on training which would include bedside assisting and sitting on the console [2].
To evaluate resident perspectives on robotics training, a nationwide survey of OB/GYN residents was done in 2015–2016 which found that 35% of participants did not have access to any robotics training and the greatest barriers to education were time and proper equipment [4]. Compared to a similar prior 2011 survey, there was an increase in completion of robotics training programs in 65% of those interviewed vs 16% [5]. Since then there has been a push to implement a more formalized curriculum for robotic-assisted surgery within OB/GYN residency [5]. It is known that there has been a substantial increase in the number of robotic-assisted surgeries since 2015. However, it is not well studied how resident surgical training curriculums and perspective have changed over the years with this continued rise.
The motivation of this study is to evaluate if ACGME-accredited OB/GYN residency programs have evolved with the changing landscape of gynecologic surgery. The objectives of this study were to evaluate current robotic surgery training methodologies for ACGME-accredited OB/GYN residency programs, better understand current resident perspectives, and explore potential areas for improvement within resident education.
Methods
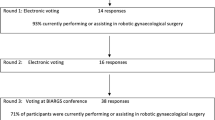
This study was an IRB-approved multi-institutional survey of ACGME-accredited OB/GYN residents enrolled in the 2023–2024 academic year. A 33-question survey study was created with a mixture of multiple choice, multiple answer, and Likert scale questions to evaluate resident access, education, and outlooks on robotic surgery training during residency. The survey was developed utilizing templates from similar prior studies. The survey was distributed via Survey Monkey platform using their anonymous collection platform. There are currently 292 OB/GYN programs in the United States. The survey was sent via email to all accredited OB/GYN program coordinators to then forward to their residents for completion. No incentives were offered for completion. At the beginning of the survey, a brief description regarding the survey was provided. The participant then had the option to continue with the survey as a means of consent to the survey. Alternatively, participants could exit and choose not to complete the survey. Respondents could review and change their responses before the final submission. Responses were collected over the course of 4 months during which time email reminders were sent periodically to program coordinators to forward to their residents. Responses were automatically collected into the survey website which was password protected. Data were downloaded onto secure password protected computers. Exclusion criteria included those who have already completed a prior surgical residency prior to OB/GYN and any OB/GYN faculty other than residents. Given that participants are residents within ACGME-accredited programs, participants were assumed to be over the age of 18 and able to read English. Results were analyzed primarily in a descriptive manner with a percentage breakdown per response.
Results
Demographics
There were 75 surveys completed. Although the number of OB/GYN residents nationally can be determined, this is not reflective of the true sample size. The true sample size is unknown given due to the method of distribution. It is unable to be determined how many residents received the survey due to the nature of the anonymity of the survey. Surveys with missing data were not excluded due to the nature of the survey questions and possibility of certain questions being inapplicable to the participant. The number of participants is reported for each question. Most of the participants were white (67.6%), female (91.9%) and between age 26 and 30 (64.0%). Majority were post-graduate year (PGY) 4 (40.0%) or PGY3 (32.0%) from an academic institution (74.7%). Geographically, most participants attended programs in the Northeast (52.0%) followed by Southeast (18.7%) and West (14.7%) (Table 1).
Robotics surgical exposure
Most institutions (98.7%) perform robotic surgeries with most residents getting involved in cases at the PGY1 (45.3%) or PGY2 (46.7%) level. Involvement via bedside assistance for most participants started at as a PGY1 (45.3%) or PGY2 (40.0%). Most residents can sit on the robotic console during surgery (93.3%) which primarily starts as a PGY3 (46.7%) or PGY2 (32%). However, most residents have never been the primary surgeon (60%), defined by completion of at least half the case. The rotations during which most residents were exposed to robotic surgery included gynecologic oncology (94.6%) followed by benign gynecology (83.8%) and urogynecology/female pelvic medicine and reconstructive surgery (66.2%) (Table 2).
Robotics simulation and education
Outside of the operating room, slightly more than half of participants (57.3%) have formalized robotics training curriculums. Required didactics training taught by faculty is noted to be nonexistent or minimal at 0 h (56.7%) or 1–2 h (20.9%). In terms of simulation training, most residents noted access to a robotic console trainer (90.7%), while less residents noted to have easy access to training simulators as a whole (72.0%). Completion of virtual reality simulation modules is not required as part of robotic training for most residents (62.5%). Those who did complete the modules noted spending between 3-5 h (36.4%) or 6–10 h (25%) completing them (Table 3; Fig. 1).
A variety of training modalities were noted to be utilized by residents for robotic surgery training including online modules (85.9%), dual-assist console (70.4%), virtual reality simulation (46.5%), hands-on training (87.3%), animal/cadaver labs (18.3%), formal didactics (36.6%), dry laboratory (11.3%), live case observation (64.8%), laparoscopic training (64.8%), and other (1.41%). The training modality written in under other was E-MIGS. Of these utilized modalities, the methods that residents found most helpful were hands-on training (67.7%) followed by dual-assist console (45.6%). The least helpful was noted to be online modules (58.7%).
At the time of the survey, most residents were not robotic certified (90.7%) but were planning to achieve certification by the time of graduation (79.7%). The largest barriers to completion of this training were noted to be attending comfort with resident participation in the case (74.0%), personal time (58.9%), and availability or access to trainers (42.5%).
Resident perspectives and future directions
From a resident perspective, most agree (33.3%) or strongly agree (54.7%) that robotics training is an important part of residency training and do not believe that a rise in robotics cases detract from resident learning (53.3%). There is a wide variation in confidence of future skills with most residents agreeing (27.0%) or strongly agreeing (17.6%) that they feel confident performing robotic surgery based on their training, while another large subset either strongly disagreed (20.3%) or disagreed (16.2%) with that statement (Figs. 2, 3).
For future careers paths, most strongly agree (44.0%) or agree (24%) that they will be using robotic surgery in future clinical practice. The distribution of future career paths was about half generalists (50.7%) and the other a mixture of various subspecialties including gynecologic oncology (12.0%), family planning (10.7%), and maternal fetal medicine (9.3%) (Fig. 3).
Importantly, most residents either strongly agree (45.3%) or agree (36.0%) that standardized robotics curriculums should be implemented for all OB/GYN residency programs. Another subset felt neutral (16.0%) regarding that statement and only a small minority disagreed (2.7%).
Discussion
In 2014, the number of robotic-assisted surgeries (RAS) was over 570,000 in the Unites States alone [4]. In 2020, this number was 876,000 despite decrease in elective cases due to COVID-19 [6]. Furthermore, an analysis by Michigan Surgical Quality Collaborative registry showed a rise between 2012 and 2018 of 1.8% to 15.1% for robotic cases [7].
The FDA approved RAS for gynecologic surgery in 2005 with rapid growth of use since then [2]. Although commonly used for general surgery procedures, according to Intuitive Surgical 2021 report, gynecology was the second largest surgical subspecialty using robotic systems in the United States [8]. A parallel increase has been seen with a rise in robotic hysterectomies with a decline in abdominal, laparoscopic, and vaginal hysterectomies [8]. Numbers have also risen within subspecialities of gynecology such as gynecologic oncology with a rise in minimally invasive staging procedures for uterine cancer after the LAP2 trial illustrated it as a feasible and safe alternative to open surgical staging [9].
Over the years, similar surveys to this have been performed to assess resident perspectives on robotic surgery training, education, and curriculums. These studies showed an increase in access to robotic consoles at training institutions from 58% to 98.9% between 2011 and 2014 [4]. This number has remained consistent in this survey with 98.7% of institutions performing robotic surgery and 90.7% having access to robotic console trainers.
Similar to prior studies, time was a major barrier to completion of robotics training for 58.9% of respondents. Interestingly, an even larger barrier for 74.0% of residents was noted to be attending comfort with resident participation in robotic surgeries. This is further demonstrated in that residents have participated in both bedside assisting and sitting on the console; however, 60% have never been primary surgeon, meaning completing at least half the case. This barrier may reflect the curriculum residents are receiving with robotics. Only 57.3% of residents are receiving any sort of formalized curriculum, which may translate to attending lack of comfort with allowing residents as primary surgeon. Based on our survey, this firsthand training was found to be most helpful in training.
After the 2015 study, there was a push for creation of standardized curriculums for robotic surgery within OB/GYN residency [5]. Potential standardized and certified training pathways are being explored on a global level through utilization of web-based training, simulation, on-site training, and mentorship [10]. A U.K.-based survey study further illustrated OB/GYN trainee interest in receiving formal education for first assist and console role [11]. The study utilized a Delphi technique with four rounds of questions to illustrate that it is possible to come to a consensus on the core curriculum for this training [11].
In terms of future directions, approximately 80% of OB/GYN residents in our study are aiming to become robot certified and 68% are planning to continue use of robotics in future clinical practice. In addition to the absence of standardized training programs, robotics certification itself also varies by institution with a lack of criteria and benchmarks based on ACGME requirements [2]. Although other areas of surgery within gynecology such as vaginal surgery or laparoscopy do not have standardized curriculums nationally, there are a certain number required for graduation creating some level of standardization nationally. Current requirements for laparoscopic cases for graduation from OB/GYN residency include 60 laparoscopy cases, 15 of which are hysterectomies, but none of which are required to be robotic cases [12].
Furthermore, hospital requirements for privileges with robotic surgery post-graduation also vary greatly. The American Associated of Gynecologic Laparoscopists have suggested guidelines regarding privileging including pre-requisites such as performing a minimum of 20 robotic cases per year [13]. The premise is that the surgeon must have the judgment and training to complete the procedure safely as intended and institutions require previous case logs as primary surgeon as well as proctoring based on medical staff bylaws to perform robotic surgery. If most OB/GYN residents are aiming to use robotics in their future practice, the required training and experience is needed to obtain privileges as an attending surgeon.
Our survey study illustrates this need for a formalized curriculum and benchmarks for robotic surgery in OB/GYN residency, limitations of this study include the low response rate. Additionally, given the method of distribution, we cannot determined how many residents received the survey to complete. However, the distribution of geographic locations and years of residents indicate that it was distributed nationally and across post-graduate levels. Future survey studies may benefit from using a larger scale platform, for example through the American College of Obstetrics and Gynecology, or incentivization for survey completion. Another limitation for consideration is that the topic of robotic surgery may appeal to residents based on interest in the field, which may create a bias in those who complete the survey. However, based on the responses received, most residents think there should be a standardized curriculum implemented, even if there is a variation of interest in robotic surgery itself.
In 2015, 42.5% of residents had said that they strongly agree or agree with the statement that they would use robotics in their future practice [4]. This is compared to 68.0% in our survey, illustrating a parallel between rising rates of robotic gynecologic surgery and resident plans for future practice in robotic surgery. For this reason, a formalized and standardized robotic training curriculum that allows trainees to obtain the necessary cases and primary surgeon experience is necessary for OB/GYN residency training. This would allow residents to gain necessary skills in a timely manner and competency for future careers in robotic gynecologic surgery.
Data availability
No datasets were generated or analysed during the current study.
References
Chopra H et al (2022) Robotics in surgery: Current trends. Ann Med Surg (Lond) 81:104375
American College of, O. and T.S.O.G.S. Gynecologists’ Committee on Gynecologic Practice (2020) Robot-assisted surgery for noncancerous gynecologic conditions: ACOG COMMITTEE OPINION, Number 810. Obstet Gynecol 136(3): e22–e30
Marchegiani F et al (2023) New Robotic platforms in general surgery: what’s the current clinical scenario? Medicina (Kaunas) 59(7):1264
Vetter MH et al (2018) Time to consider integration of a formal robotic-assisted surgical training program into obstetrics/gynecology residency curricula. J Robot Surg 12(3):517–521
Moglia A (2018) Integration of a formal robotic-assisted surgical training program into obstetrics/gynecology residency curricula. J Robot Surg 12(4):753–754
Rizzo KR et al (2023) Status of robotic assisted surgery (RAS) and the effects of Coronavirus (COVID-19) on RAS in the Department of Defense (DoD). J Robot Surg 17(2):413–417
McCartney J (2023) Robotic surgery is here to stay— and so are surgeons. 108
Levin G et al (2023) Robotic surgery in obstetrics and gynecology: a bibliometric study. J Robot Surg 17(5):2387–2397
Walker JL et al (2009) Laparoscopy compared with laparotomy for comprehensive surgical staging of uterine cancer: Gynecologic Oncology Group Study LAP2. J Clin Oncol 27(32):5331–5336
Moawad G, Rahman S, Saridogan E (2022) The case for standardising robotic curriculum globally. Facts Views Vis Obgyn 14(2):99–102
Ismail A et al (2020) The development of a robotic gynaecological surgery training curriculum and results of a delphi study. BMC Med Educ 20(1):66
Education, A.C.F.G.M. (2022) Case log information: obstetrics and gynecology
Worldwide A.A.M.I.G (2014) Guidelines for privileging for robotic-assisted gynecologic laparoscopy. J Minim Invasive Gynecol 21(2):157–167
Funding
None.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation and analysis were done by Anusha Adkoli. Data collection was performed by Anusha Adkoli and Samantha Eng. The first draft of the manuscript was written by Anusha Adkoli. All authors commented on previous versions of the manuscript and all authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Informed consent
Informed consent was obtained for all participants.
IRB approval
This study was approved by Rutgers Robert Wood Johnson IRB on 8/7/23 (Approval No. Pro2023000876).
Prior presentation
Has not been presented prior.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Adkoli, A., Eng, S. & Stephenson, R. Need for formalized robotic training and curriculum in obstetrics and gynecology residency: an examination of current resident outlooks and perspectives. J Robotic Surg 18, 218 (2024). https://doi.org/10.1007/s11701-024-01985-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11701-024-01985-9